Abstract
Study Design Case report.
Objective To analyze the surgical difficulties in restoring global spinal stability and to describe an effective surgical option for tuberculosis with extensive destruction of the lumbosacral spine. Advanced tuberculosis with destruction of the lumbosacral spine can result in a kyphosis or hypolordosis, leading to back pain, spinal instability, and neurological deficits. The conventional treatment goals of lumbosacral tuberculosis are to correct and prevent a lumbar kyphosis, treat or prevent a neurological deficit, and restore global spinal stability. Instrumentation at the lumbosacral junction is technically demanding due to the complex local anatomy, the unique biomechanics, and the difficult fixation in the surrounding diseased bone.
Methods We report a 21-year-old woman with tuberculosis from L1 to S2 with back pain and spinal instability. The radiographs showed a kyphosis of the lumbar spine. The magnetic resonance imaging and computed tomography scans revealed extensive destruction of the lumbar and lumbosacral spine. Spinopelvic stabilization combined with anterior debridement and reconstruction with free fibular strut graft was performed.
Results The radiographs at follow-up showed a good correction of the kyphosis and excellent graft incorporation and fusion.
Conclusions Anterior column reconstruction with a fibular strut graft helps restore and maintain the vertebral height. Posterior stabilization with spinopelvic fixation can be an effective surgical option for reconstructing the spine in extensive lumbosacral tuberculosis with sacral body destruction, requiring long fusions to the sacrum. It augments spinal stability, prevents graft-related complications, and accelerates the graft incorporation and fusion, thereby permitting early mobilization and rehabilitation. In spinal tuberculosis, antitubercular therapy may have to be prolonged in cases with large disease load, based on the clinicoradiographic and laboratory parameters.
Keywords: tuberculosis, lumbosacral junction, spinopelvic stabilization, fibular graft, spinal stability
Introduction
Tuberculosis of the lumbosacral junction is rare (2 to 3% of vertebral column tuberculosis).1 2 The treatment goals of spinal tuberculosis are to cure the disease and prevent spinal deformity, instability, and neurodeficit. The early stages of lumbosacral tuberculous spondylitis can be treated successfully with chemotherapy alone. Advanced tuberculosis with extensive destruction of the lumbosacral region and loss of a normal lumbar lordosis and lumbosacral biomechanics requires surgical management. The conventional treatment goals of lumbosacral tuberculosis are to restore or preserve a normal lumbosacral angle and global spinal stability. The management principles of tuberculosis of the lumbar spine and lumbosacral junction are entirely different when dealing with disease of either of these regions individually. Extensive disease involving both the lumbar spine and the lumbosacral junction (a unique transition zone) has not been previously described in the literature. The goals and principles of management have not been clearly defined for such extensive disease. The instrumentation at the lumbosacral junction is technically demanding due to the complex local anatomy, the unique biomechanics, and the difficult fixation in the surrounding diseased bone. We discuss the difficulties encountered during the surgical management of a 21-year-old woman with extensive tuberculosis of the L1 to S2 vertebrae, and we describe an effective surgical option.
Case Report
A 21-year-old woman presented with pain in the lower back for 6 months' duration in March 2008. The patient was diagnosed with pulmonary tuberculosis 3 months previously, and first-line antitubercular drugs were started empirically. Initially, the pain was bearable. After 3 months, she started experiencing severe pain in her lower back, radiating to both her lower limbs. She was unable to sit and had difficulty standing, walking, and performing her activities of daily living. She was completely bedridden with fever, malaise, loss of weight, and weakness of both her lower limbs for a month before presenting to us. The physical examination revealed a loss of the normal lumbar lordosis, tenderness over the lumbosacral spine, a bilateral sensory blunting below L1, grade 4 muscle strength in the lower limbs, and a normal cystorectal sphincter function.
The lateral radiographs showed a kyphosis of the lumbar spine. The magnetic resonance imaging (Fig. 1) and computed tomography (CT) scans (Fig. 2A, B) showed extensive bony destruction from the L1 to S2 vertebrae, with a prevertebral and epidural abscess compressing the neural elements.
Fig. 1.

T2-weighted magnetic resonance sagittal image showing tuberculous involvement from L1 to upper sacral vertebral bodies with prevertebral, presacral, and epidural abscess with neural compression.
Fig. 2.
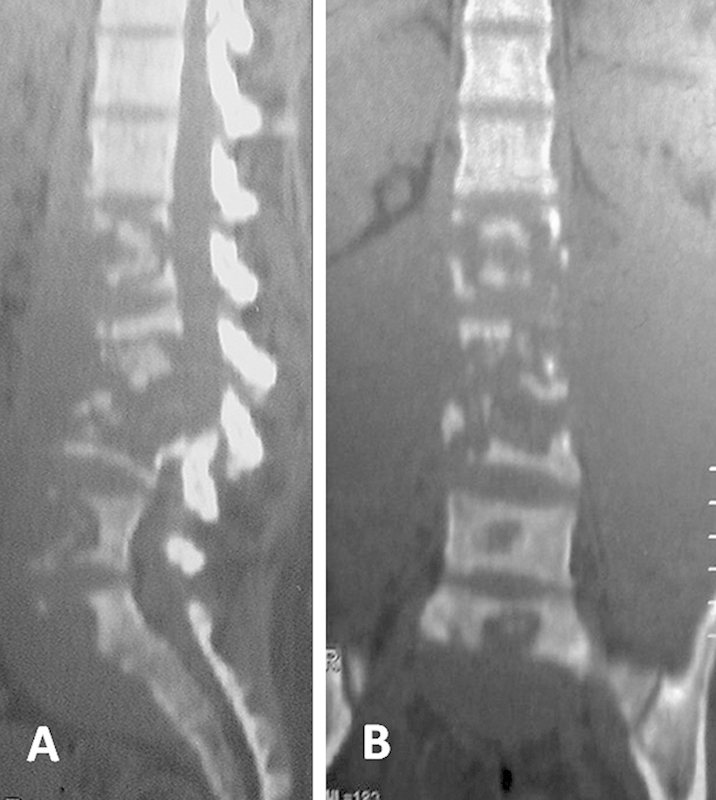
Sagittal (A) and coronal (B) computed tomographic scans showing extensive vertebral body destruction from L1 to upper sacral vertebrae.
The condition of the diseased bones at surgery was such that the partially destroyed L1, L5, and S1 vertebrae and the grossly destroyed L2, L3, and L4 vertebrae could not hold any screws at all. Therefore, a spinopelvic fixation was done through the posterior approach. The pedicular screws were inserted bilaterally at the T10, T11, and T12 levels. As the body of the S1 was destroyed (Fig. 3), the pedicle screws were inserted bilaterally into the undestroyed ala along with additional screws in the iliac wings (Fig. 4A). Screws were not deployed in S2 for biomechanical reasons. A bone graft was not used during the first posterior surgery. The general health of the patient was so poor that we waited 4 weeks for her condition to improve before proceeding to the second stage of surgery. In the second surgery, an anterior debridement with drainage of the abscess was performed through a transperitoneal approach, and reconstruction with a free fibular strut autograft of 12.6-cm length extending from the D12 to the inferior end plate of the L5 was done (Fig. 4B). The undestroyed residual lower end plate of the L5 vertebra was used to seat the lower end of the fibular graft. It was difficult to mobilize the vessels during surgery due to the extensive adhesions to the surrounding structures. A vascular surgeon assisted in the exposure of the diseased area. Further details on the patient's disease process are given in Table 1.
Fig. 3.
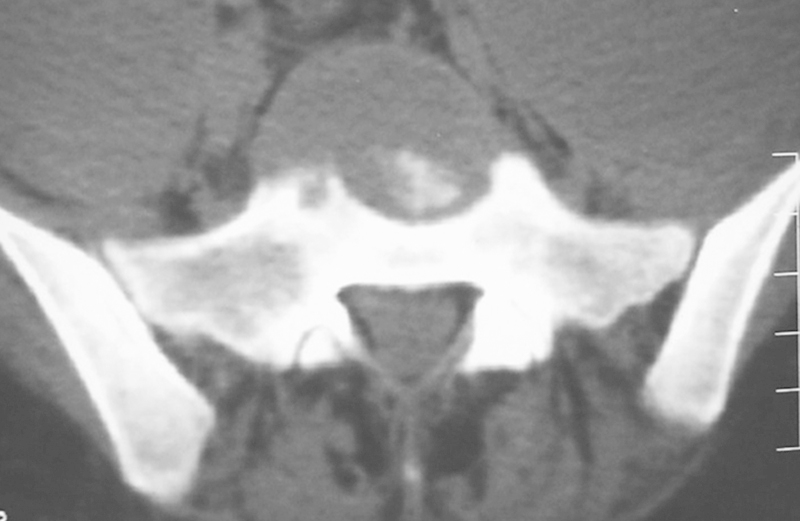
Axial computed tomographic scan showing destruction of S1 vertebral body.
Fig. 4.
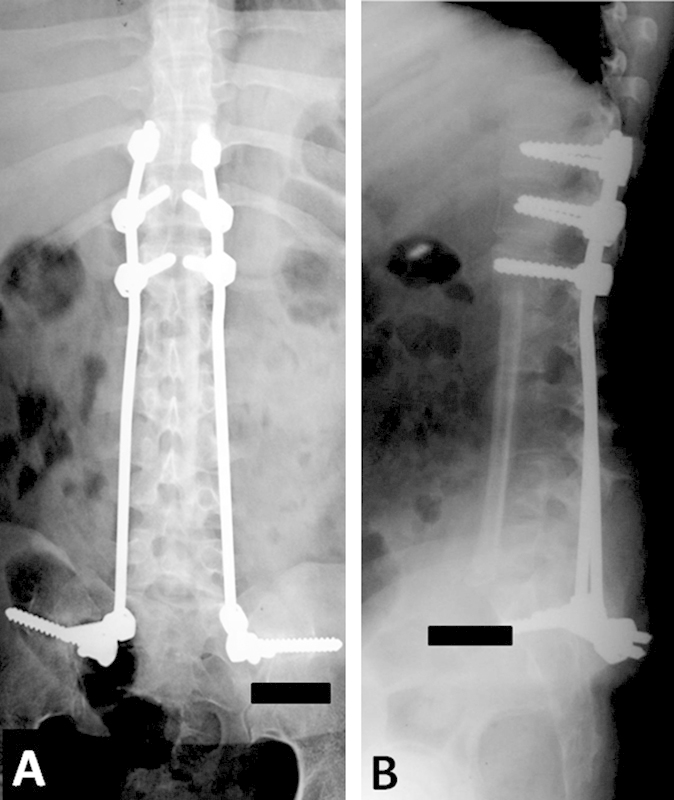
(A) Anteroposterior view of immediate postoperative radiograph. (B) Lateral view of immediate postoperative radiograph showing the anterior column reconstruction with a 12.6-cm-long fibular graft spanning across four disk spaces.
Table 1. Patient data.
| Level of involvement | L1 to S2 |
|---|---|
| Origin of disease | Lung |
| Vertebral body lossa | 4.8 |
| Preoperative angle of kyphosis/lordosis (degrees) | 8 |
| Operation time (both stages combined; min) | 270 |
| Blood loss (mL) | 1,900 |
| Complications | None |
The vertebral body loss was measured on pretreatment anteroposterior and a lateral radiograph similar to the method used by Rajasekaran et al.12 There was major vertebral body loss in this case.
The patient was put on antitubercular treatment [category I, DOTS (directly observed treatment, short-course) regimen] for 12 months along with spinal bracing. She returned to her activities of daily living in 3 months. The lateral radiographs taken at 5-year follow-up (Fig. 5) showed a correction of the kyphosis with a lumbar lordosis of 18 degrees. At 5-year follow-up, her Oswestry Disability Index (ODI) and Scoliosis Research Society (SRS) scores showed a marked improvement compared with her preoperative and early postoperative scores. CT showed excellent incorporation and consolidation of the graft with maintenance of the vertebral column height (Fig. 6). The postoperative standing whole-spine radiographs showed a good coronal alignment and an acceptable sagittal alignment (Fig. 7A, B).
Fig. 5.
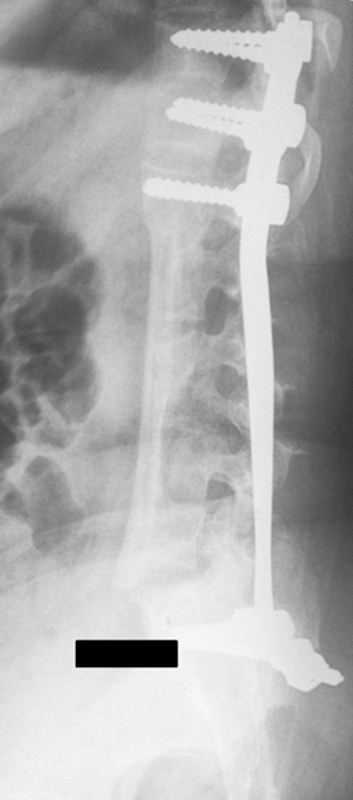
Lateral radiograph of the lumbosacral spine (taken at 61 months) showing excellent graft incorporation and consolidation.
Fig. 6.

Fusion analysis at 61 months postsurgery with multislice multiplanar computed tomography with three-dimensional reconstruction and implant subtraction imaging showing excellent graft consolidation and fusion with no subsidence.
Fig. 7.
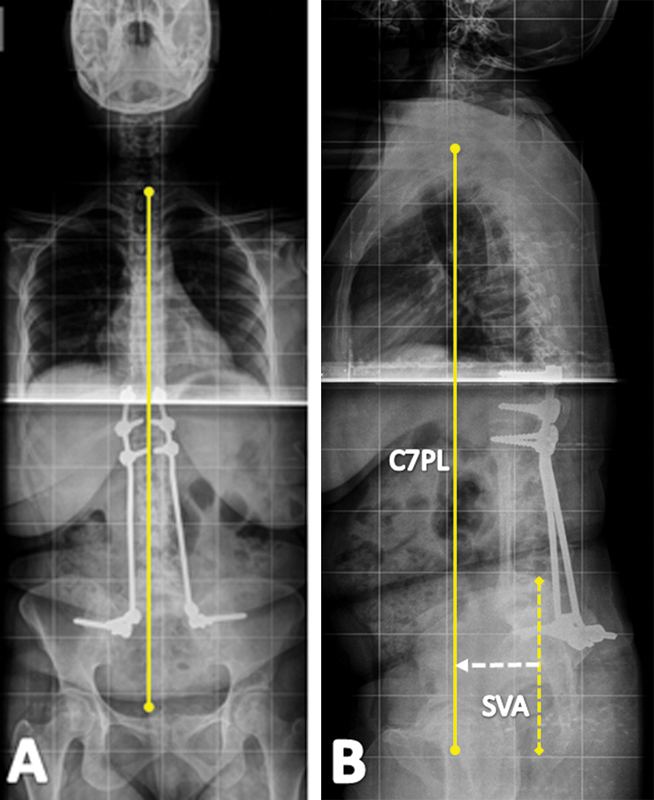
(A) Standing whole-spine anteroposterior radiograph (taken at 61 months) showing the coronal alignment. (B) Standing whole-spine lateral radiograph (taken at 61 months) showing the C7PL (C7 plumb line) and sagittal vertical axis of 34 mm.
Discussion
The treatment of tuberculosis of the lumbosacral junction remains difficult and controversial. There are no detailed studies on the surgical strategies in advanced lumbosacral junctional tuberculosis. Pun et al reported that all cases treated nonoperatively ended up with a kyphosis associated with trunk shortening.1 Advanced tuberculosis with extensive destruction of the lumbosacral spine results in a kyphosis or a hypolordosis, with a higher incidence of back pain and difficulties during childbirth.1
The conventional treatment goals of lumbosacral tuberculosis are to correct and prevent a lumbar kyphosis, decompress the neural elements to correct or prevent a neurological deficit, restore or preserve a normal lumbosacral angle, and maintain the vertebral height and global spinal stability. Anterior debridement and fusion with a strut graft can prevent and lessen a kyphosis, but there is a high incidence of graft-related problems and rehabilitation is slower.1 3 Supportive posterior instrumentation helps withstand the shear forces across the lumbosacral junction, prevents graft slippage, and accelerates the graft incorporation and fusion, allowing early mobilization and rehabilitation.4 5
Instrumentation at the lumbosacral junction is technically demanding due to the complex local anatomy, the unique biomechanics, and the difficult fixation in the surrounding diseased bone. In tuberculosis with extensive destruction of the lumbar spine and lumbosacral junction requiring long fusions to the sacrum, as in this case, a spinopelvic fixation is an effective surgical option. The loss of sacral bone for implant anchoring (Figs. 2A, 3) changes the fixation options available in such cases.6 The S2 pedicle screw remains dorsal to the lumbosacral pivot point of McCord and does not add much to the overall strength of the lumbopelvic fixation construct.7 8 Therefore, a biomechanically stable fixation was achieved with screws in the disease-free sacral ala along with additional screws in the iliac wings bilaterally. Although free fibular grafts spanning more than two disk spaces are known for complications such as graft fractures and failure of graft incorporation,3 at 5-year follow-up the patient showed excellent graft incorporation and fusion with good functional results.
The management principles of tuberculosis of the lumbar spine and the lumbosacral junction are entirely different when dealing with disease of either of these regions individually. Extensive disease involving the whole lumbar spine and the lumbosacral junction (a unique transition zone), as in this case, has not been previously described in the literature. The goals and principles of management have not been clearly defined, and the conventional techniques would not be applicable in this particular case.
In a case with extensive loss of the anterior spinal column and its axial load-bearing function, the stability of the spine depends largely on the integrity of the posterior osteoligamentous complex. The need for reconstruction of the anterior column (using a fibular strut graft) to correct and/or prevent the progression of a lumbar kyphosis cannot be overemphasized.1 3
The restoration of a normal lumbosacral angle may be difficult with surgical reconstruction and fusion spanning across many levels as in this case. Contouring the rods to achieve a lordotic lumbar spine was not done because it might compromise the stability of the anteriorly placed long fibular strut graft, which could slip due to the high axial loads and the shear forces across the graft.
Doing an osteotomy (Smith Peterson osteotomy/pedicle subtraction osteotomy) to restore the normal lumbar lordosis would jeopardize the stability of the spine, which solely rests on the posterior osteoligamentous complex. Furthermore, an osteotomy was not possible because the condition of the diseased bones at surgery was such that the partially destroyed L1, L5, and S1 vertebrae and the grossly destroyed L2, L3, and L4 vertebrae could not hold any screws at all. Hence, we chose a long spinopelvic construct spanning the diseased lumbosacral spine with pedicle screw anchors at the proximal and distal ends.
The standing whole-spine radiographs show that a good coronal alignment and an acceptable sagittal alignment (sagittal vertical axis 34 mm) have been achieved. At 5 years postsurgery, the patient had no pain and was able to do her daily activities without discomfort or increased efforts, as reflected by her improved ODI and SRS scores.
It cannot be denied that proper sagittal alignment is an important factor that determines the outcome of spinal deformity surgeries. Although restoration of the normal lumbar lordosis and an ideal sagittal alignment continue to be the prime goals in treating spinal deformities, there are situations such as in the present case in which the options of achieving the ideal spinopelvic alignment are drastically reduced.9 Although restoration of a normal lumbosacral angle may be difficult with surgical reconstruction and fusion spanning across many levels as in this case, the primary goals of deformity correction and restoration of spinal stability can be achieved as evidenced by the good clinical and functional outcomes.
Therefore, in tuberculosis with the extensive destruction of the lumbar spine and lumbosacral junction, involving multiple vertebral levels, the main goals of surgical reconstruction are to correct and prevent kyphotic deformity, restore global spinal stability, and decompress the neural elements to correct or prevent a neurodeficit.
In cases of spinal tuberculosis with large disease load, the standard DOTS regimen may need to be extended for up to 18 months based on the clinicoradiographic and laboratory parameters. The erythrocyte sedimentation rate and C-reactive protein are reliable parameters evaluating the response to the treatment and the prognosis of spinal tuberculosis.10 11
Conclusion
The treatment of tuberculosis of the lumbosacral region is difficult, and each patient needs individual consideration. In tuberculosis with extensive destruction of the lumbar spine and lumbosacral junction requiring long fusions to the sacrum, spinopelvic stabilization along with free fibular strut graft reconstruction is a safe and effective surgical option for reconstructing the destroyed lumbar spine and the lumbosacral junction. It prevents the progression of a kyphosis and helps to restore and maintain the vertebral height and spinal stability, thereby permitting early mobilization and rehabilitation. It is evident that the goals of an ideal spinopelvic alignment cannot be obtained in all cases. It is important to meticulously analyze and customize the treatment on a patient-specific level. In spinal tuberculosis, the antitubercular therapy may have to be prolonged in cases with large disease load, on the basis of clinicoradiographic and laboratory parameters.
Acknowledgment
I thank Prof. Devi Meenal, MD (RD), MRCR for her invaluable help, support, and encouragement.
Footnotes
Funding No funding, technical support, or corporate support in any form for research was received for this article from any of the following organizations: National Institutes of Health (NIH); Wellcome Trust; Howard Hughes Medical Institute (HHMI); Research Councils UK (RCUK) and other(s). Disclosures Nalli R. Uvaraj, none Aju Bosco, none Nalli R. Gopinath, none
References
- 1.Pun W K, Chow S P, Luk K DK, Cheng C L, Hsu L CS, Leong J CY. Tuberculosis of the lumbosacral junction. Long-term follow-up of 26 cases. J Bone Joint Surg Br. 1990;72(4):675–678. doi: 10.1302/0301-620X.72B4.2143192. [DOI] [PubMed] [Google Scholar]
- 2.Tuli S M. Severe kyphotic deformity in tuberculosis of the spine. Int Orthop. 1995;19(5):327–331. doi: 10.1007/BF00181121. [DOI] [PubMed] [Google Scholar]
- 3.Hodgson A R, Stock F E. Anterior spinal fusion. A preliminary communication on the radical treatment of Pott's disease and Pott's paraplegia. 1956. Clin Orthop Relat Res. 1994;(300):16–23. [PubMed] [Google Scholar]
- 4.Moon M S, Woo Y K, Lee K S, Ha K Y, Kim S S, Sun D H. Posterior instrumentation and anterior interbody fusion for tuberculous kyphosis of dorsal and lumbar spines. Spine (Phila Pa 1976) 1995;20(17):1910–1916. doi: 10.1097/00007632-199509000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Sundararaj G D, Behera S, Ravi V, Venkatesh K, Cherian V M, Lee V. Role of posterior stabilisation in the management of tuberculosis of the dorsal and lumbar spine. J Bone Joint Surg Br. 2003;85(1):100–106. doi: 10.1302/0301-620x.85b1.13300. [DOI] [PubMed] [Google Scholar]
- 6.Asher M, Lai S M, Burton D, Manna B. Maintenance of trunk deformity correction following posterior instrumentation and arthrodesis for idiopathic scoliosis. Spine (Phila Pa 1976) 2004;29(16):1782–1788. doi: 10.1097/01.brs.0000134568.45154.34. [DOI] [PubMed] [Google Scholar]
- 7.McCord D H Cunningham B W Shono Y Myers J J McAfee P C Biomechanical analysis of lumbosacral fixation Spine (Phila Pa 1976) 199217(8, Suppl):S235–S243. [DOI] [PubMed] [Google Scholar]
- 8.Camp J F, Caudle R, Ashmun R D, Roach J. Immediate complications of Cotrel-Dubousset instrumentation to the sacro-pelvis. A clinical and biomechanical study. Spine (Phila Pa 1976) 1990;15(9):932–941. doi: 10.1097/00007632-199009000-00018. [DOI] [PubMed] [Google Scholar]
- 9.Schwab F, Patel A, Ungar B, Farcy J P, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 2010;35(25):2224–2231. doi: 10.1097/BRS.0b013e3181ee6bd4. [DOI] [PubMed] [Google Scholar]
- 10.Jain A K. Tuberculosis of the spine: a fresh look at an old disease. J Bone Joint Surg Br. 2010;92(7):905–913. doi: 10.1302/0301-620X.92B7.24668. [DOI] [PubMed] [Google Scholar]
- 11.Rasouli M R, Mirkoohi M, Vaccaro A R, Yarandi K K, Rahimi-Movaghar V. Spinal tuberculosis: diagnosis and management. Asian Spine J. 2012;6(4):294–308. doi: 10.4184/asj.2012.6.4.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rajasekaran S, Shanmugasundaram T K, Prabhakar R, Dheenadhayalan J, Shetty A P, Shetty D K. Tuberculous lesions of the lumbosacral region. A 15-year follow-up of patients treated by ambulant chemotherapy. Spine (Phila Pa 1976) 1998;23(10):1163–1167. doi: 10.1097/00007632-199805150-00018. [DOI] [PubMed] [Google Scholar]


