Abstract
Study Design Narrative review.
Objective To elucidate the current concepts in diagnosis and treatment of traumatic spondylolisthesis of the axis.
Methods Literature review using PubMed, Google Scholar, and Cochrane databases.
Results The traumatic spondylolisthesis of the axis accounts to 5% of all cervical spine injuries and is defined by a bilateral separation of the C2 vertebral body from the neural arch. The precise location of the fracture line may vary widely. For understanding the pathobiomechanics, the involvement of the C2–C3 disk is essential. Although its synonym “hangman's fracture” suggests an extension moment as primary injury mechanism, flexion moments are also proven to cause such fracture morphology. The axial force vector (distraction versus compression) is thought to have a significant effect on the neurologic involvement. The most widely accepted classifications, according to Effendi and modified by Levine, regard the displacement of the C2 vertebral body and possible locking of the facet joints. For decisions on conservative versus surgical therapy, a definitive statement about the stability is essential. The stability is determined by involvement of the C2–C3 disk and longitudinal ligaments, which frequently cannot be assessed by X-ray or computed tomography alone. The assessment of this soft tissue injury therefore requires additional imaging either by magnetic resonance imaging to display the disk and longitudinal ligaments or dynamic fluoroscopy to assess functional behavior of the C2–C3 motion segment. If stability is proven, an immobilization of the cervical spine in a semirigid cervical collar is sufficient. Unstable lesions require surgical stabilization. The standard procedure is an anterior C2–C3 diskectomy and fusion, because of the lower morbidity of the anterior approach and the motion preservation between C1 and C2. In rare cases (irreducible locked facet joints, the necessity of decompression of the vertebral artery, contraindication for anterior approach), a posterior approach is sometimes necessary. Isolated direct screw osteosynthesis is of little value, because it only makes sense in cases with an intact C2–C3 disk, which is usually regarded as stable and therefore might be treated conservatively.
Conclusions Overall, the clinical evidence regarding traumatic spondylolisthesis of the axis is very low and mainly based on small case series, expert opinion, laboratory findings, and theoretical considerations.
Keywords: spinal trauma, cervical spine, traumatic spondylolisthesis of the axis, hangman's fracture, axis, review, Effendi, surgery
Introduction
The upper cervical spine consists of a unique anatomy and biomechanics resulting in specific injury patterns not observed in the subaxial spine. One particular type of injury is the traumatic spondylolisthesis of the axis, also known as the “hangman's fracture.” This review covers the unique characteristics of the traumatic spondylolisthesis of the axis, historical context of the injury, current classifications, and recommended treatments based on the most current literature.
Historical Overview and Pathogenesis
The “Hangman's Fracture”
In the late 19th century, researchers discovered that the submental positioning of the gallows knot leads to a safer and more humane execution than the suboccipital or subaural positioning.1 Anatomical studies revealed fractures of the neck to be the major difference between these techniques. Although other types of cervical injury, such as dissociation between the fifth and sixth cervical vertebrae or skull base fractures, were found in the hangees, Wood-Jones proposed a dissociation of the neural arch of the axis vertebra (remaining connected to the subaxial spine) and the vertebral body of C2 as the major type of injury in hanging.2
During his examinations on cervical spine injuries in traffic accidents, Schneider remembered this injury mechanism and his group named the frequently occurring fracture type through the pars interarticularis of the axis “hangman's fracture.”3 Although later studies showed that this special fracture morphology only accounts for ∼10% of the injuries observed in judicial hanging,4 this striking term is still frequently used to describe a bilateral isthmus fracture of the axis.
Typical Injury Mechanisms and Pathobiomechanics
Traumatic spondylolisthesis of the axis refers to the common locus of failure in the pars interarticularis of the neural arch, the separation from the C2 vertebral body, and the subsequent slippage of the C2 over the C3 vertebral body in an anterior direction. To understand the pathobiomechanics of this injury, it is crucial to pay attention to the osseous and to the soft tissue component of the lesion.
A hyperextension or hyperflexion mechanism on the head will tilt backward (or forward) the upper cervical structures including the odontoid peg and the body of the axis. The articular processes cannot follow this motion due to the underlying facet joints, which are held in position by the body's weight. This movement induces a bending moment to the vertebral body and the pedicle of the axis, causing failure at the weakest part of the bone, which is the interarticular portion of the neural arch.5
Depending on the additional force vector along the longitudinal axis, the injury mechanism can be a hyperextension-distraction injury (likely in “judicial hanging”) or a hyperextension-compression injury, which is observed for example in traffic accidents when passengers' foreheads hit against the windshield. The distraction-type injury may cause a complete disruption of all the ligamentous structures, which will generate severe instability and usually fatal neurologic damage to the spinal cord at the C2 level.
The compression-type injury might be associated with multiple fractures of the adjacent spinous processes or vertebral body fractures in the lower cervical spine.6 7 The exact course of the fracture line shows a great variability, with fracture lines running through the isthmus itself, the facet joint surface, as well through the vertebral body.6 An asymmetrical fracture configuration is frequently seen, which will conceal the fracture in conventional lateral X-ray, impeding a quick diagnosis.
If the posterior wall of the C2 vertebral body keeps partially connected to the neural arch, it might dislocate posteriorly and compromise the myelon. This so-called atypical traumatic spondylolisthesis of the axis is a rare condition where neurologic damage is observed.
The most important soft tissue component of the traumatic spondylolisthesis of the axis is the disruption of the longitudinal ligaments and the disk at the C2–C3 level. The posterior longitudinal ligament is always injured in the rare hyperflexion type of injury,8 whereas its role in the hyperextension type of injury is controversial.6 A hyperflexion mechanism will cause a traumatic spondylolisthesis of the axis, if the major translational component is directed more than 60 degrees upward from the horizontal plane.9
Depending on the amount of impact, further prevertebral soft tissues might be injured: lacerations of the longus colli muscle with the adjacent sympathetic nerve fibers might cause Horner syndrome. A strain to the pharyngeal and esophageal muscle tube may lead to dysphagia. Even tracheal ruptures are described in the literature.7 The course of the vertebral artery in the transversal foramina puts this vessel under the danger of injury with potentially fatal consequences. In traumatic spondylolisthesis of the axis, the rate of radiographically detected vertebral artery injury (VAI) is found to be as high as 27%.10 Risk factors for VAI include fracture extending to the transverse foramen, fractures having greater angulation, age, male sex, and comminuted fracture.10
Epidemiology
The traumatic spondylolisthesis of the axis accounts for ∼5% of all cervical spine fractures and ∼20% of all axis fractures and is the second most common fracture type of the axis after the odontoid fracture.11
Diagnostics
During the diagnostic process, three main goals are pursued:
To be aware that patients with a suspicious trauma mechanism and/or complaints may have this type of fracture
To answer the question or whether the lesion is unstable or not
In case of an unstable lesion (which is generally an indication for surgical therapy), to decide on the surgical strategy, in particular whether to choose an anterior or posterior approach
Suspicious Signs and Symptoms
As outlined in the biomechanics section of this article, any trauma mechanism that combines an extension or flexion moment on the head with an axial distraction or compression component may raise suspicion of a traumatic spondylolisthesis of the axis. Besides judicial or suicidal hanging, typical injury mechanisms are falls combined with hitting an obstacle with the forehead or the chin. Motor vehicle accidents are likely to cause such an injury as well, either by hitting the windshield or the dashboard with the head. Mindful examination of the car wreck at the accident site can provide helpful information for the treating physician.
The examiner has to search for any signs of impact at the mental or submental region (extension-distraction), such as lacerations, bruises, or mandibular fractures. An extension-compression mechanism is likely with signs of impact at the frontal or parietal region, which can present with skin lacerations, frontal skull fractures, or intracerebral hematoma. A flexion injury may reveal itself with injury signs at the parieto-occipital region.
If still conscious, patients usually report severe neck pain. Due to the separation of the vertebral body and neural arch with normally consecutive widening rather than compression of the spinal canal, the rate of neurologic injury is reported to be low. In the original publication of Effendi and colleagues, they reported ∼13% of patients showing a temporary neurologic deficit (excluding TBI), with changing probability dependent on the injury grading (I: 11%; II: 19%; III: 11%).12 The rate of permanent neurologic deficit is 3% in their study. Type III lesions showed no recovery at all, whereas all type I lesions recovered. Francis and colleagues reported a 6.5% temporary and a 2% permanent neurologic deficit, and Levine and Edward's study counted up to 25% of patients with a neurologic deficit, regardless whether temporary or permanent.13 14
Due to the high rate of VAI, it is important to look for typical vertebrobasilar symptoms like vertigo, ataxia, or drop attacks. Other specific clinical and radiographic criteria have been developed, including severe angulation or a fracture line running into the transverse foramen.10 15 Nevertheless, the neurologic symptoms due to VAI often develop delayed over an interval of hours or even days after the primary injury.16 17 18 Early radiologic detection might trigger early treatment and prevent significant morbidity and mortality.
Classification
Multiple classification systems describe the fractures of the interarticular portion of the axis. The three most widely accepted are the classification according to Effendi et al, its modification according to Levine and Edward, and the classification according to Francis and colleagues.12 13 14 Especially in the German-speaking countries, the Josten classification is also quite common.19 The major drawback of all mentioned classification systems is the lack of a functional component (e.g., assessment of stability), although this topic is directly related to the decision-making process regarding treatment.
Effendi Classification and Modification by Levine and Edwards
The Effendi classification is based on radiographic signs in the lateral view.12 Levine has published his classification system, based on the previous work of Effendi, in 1985.14 Both take into account the amount of displacement and angulation of the C2-vertebral body against the C3 vertebral body as well as the position of the C2–C3 facet joint (Figs 1, 2, 3, 4 and Table 1).
Fig. 1.

A nondisplaced fracture is classified as “Effendi/Levine I.” (Image from Kandziora et al27 with permission from Springer Images.)
Fig. 2.
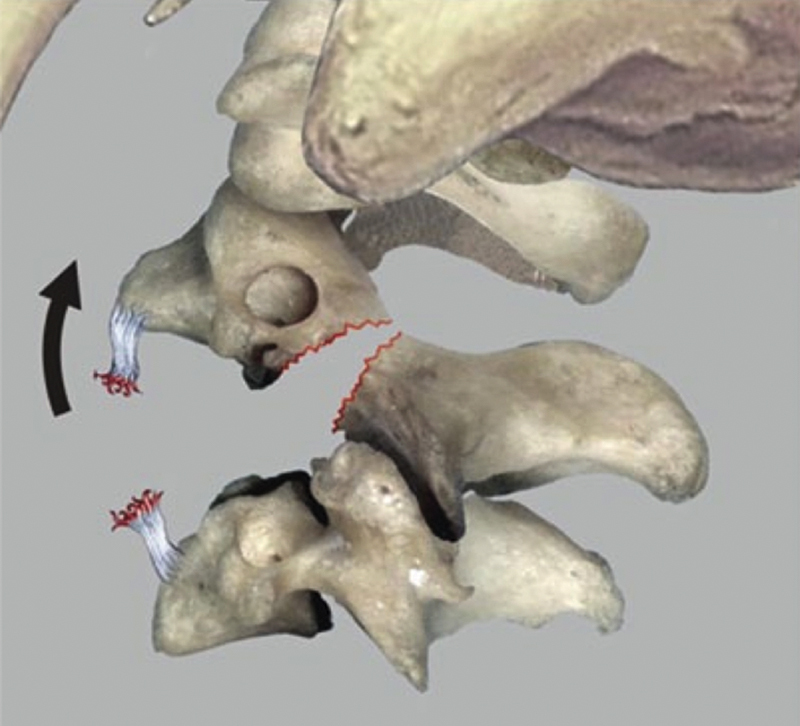
A fracture with an angulated and translated vertebral body is classified as “Effendi/Levine II.” (Image from Kandziora et al27 with permission from Springer Images.)
Fig. 3.
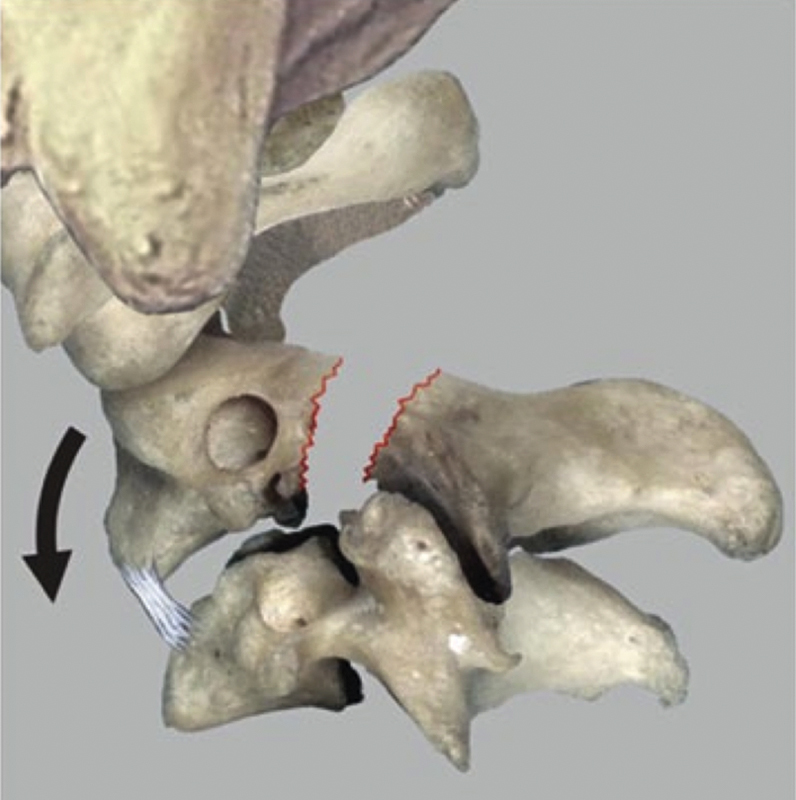
A fracture with an angulated, but not translated vertebral body is classified as “Effendi/Levine IIa.” (Image from Kandziora et al27 with permission from Springer Images.)
Fig. 4.

A fracture with uni- or bilaterally locked facet joints is classified as “Effendi/Levine III.” (Image adapted from Kandziora et al27 with permission from Springer Images.)
Table 1. Effendi12 and Levine/Edwards14 classification.
| Type | Levine/Edwards | Effendi |
|---|---|---|
| I | Hairline fracture, no angulation, dislocation < 3 mm | “Isolated hairline fractures of the ring of the axis with minimal displacement of the body of C2. The fracture may involve any part of the ring of the axis and may extend anteriorly into the body of C2. The fracture line is then oblique, involving usually one or rarely both postero-inferior corners of the body. The disk space below the axis is normal and stable.” (p. 321) |
| II | Significant angulation, dislocation > 3 mm | “Displacement of the anterior fragment, with an abnormal disk below the axis. The body of the axis may be displaced in extension, flexion or obvious forward listhesis.” (p. 321) |
| IIa | Significant angulation, no translation (“hinging” of the ALL) | – |
| III | Uni- or bilaterally locked facet joint | “Displacement of the anterior fragment with the body of the axis in the flexed position; but in addition the facet joints at C2–3 are dislocated and locked. A type II lesion must be suspected when the body of the axis is in a position of flexion; it has not been seen when it is in a position of extension or of forward listhesis.” (p. 321) |
Abbreviation: ALL, anterior longitudinal ligament.
Although the Effendi classification is rather imprecise in setting the borders between the type I and II lesions (“minimal displacement” and “normal disk space” versus “displacement” and “abnormal disk”), Levine and Edwards do quantify the cut edge between the two types at least for anteroposterior translation (3 mm), but neither do that for angulation (“no angulation” versus “significant angulation”).
A locked C2–C3 facet joint constitutes a type III lesion in both classification systems.
Although these classifications systems have been developed ∼30 years ago, before the computed tomography (CT) and magnetic resonance imaging (MRI) era, they still are widely used in the everyday clinical setting.
Francis Classification (Table 2)
Table 2. Francis classification.
| Francis grade | Displacement | Angulation (degrees) |
|---|---|---|
| I | <3.5 mm | <11 |
| II | <3.5 mm | >11 |
| III | >3.5 mm <0.5 vertebral width |
>11 |
| IV | >3.5 mm >0.5 vertebral width |
>11 |
| V | Any disk disruption |
The Francis classification, also published in 1981, takes into account the amount of displacement and angulation as well as any disk disruption.13
Josten Classification
The Josten classification takes in to account the presence of a lesion of the anterior longitudinal ligament and/or the disk or any facet joint locking (Table 3).19 Although the original publication does not mention how these lesions are to be determined, it is the first classification that specifically addressed the soft tissue injury, which is regarded as the major determinant for therapeutic decision making.
Table 3. Josten classification.
| Type | Characteristics | Treatment |
|---|---|---|
| 1 | Intact ALL, intact disk | Halo |
| 2 | ALL intact, ruptured disk | Halo |
| 3 | ALL and disk ruptured | Anterior C2–C3 fusion |
| 4 | Posterior dislocated and fixated facet joint | Open posterior procedure necessary |
Abbreviation: ALL, anterior longitudinal ligament.
Imaging
Conventional Radiography
Conventional lateral X-ray is part of the standard imaging of trauma patients in most health care systems. The grossly displaced Effendi II and III fractures are usually easily visible on these pictures.
Nevertheless, the false-negative rate to detect a cervical spine fracture on a plain X-ray is estimated to be as high as 40%.20 In the special case of a spondylolisthesis of the axis, this concern is valid especially for undisplaced or spontaneously reduced fractures. If the fracture lines at the left and right isthmus are not symmetrical, which is quite common, they will be concealed by the intact bone of the opposite side.
Congenital spondylolysis of the axis is a rare but considerable radiologic differential diagnosis. Smooth, clearly defined bone edges, a strictly symmetric configuration of the pars defect, dysplastic facets, ossification centers within the pars defect, or lack of a prevertebral hematoma should raise the suspicion of a congenital spondylolysis.21
Computed Tomography
In any unclear diagnosis in conventional X-ray, a CT scan is the next step. The CT is better in detecting fracture lines, especially if these are asymmetric or run into the vertebral body. Small bone fragments at the edges of the vertebral body may indicate a bony avulsion of the anterior or posterior longitudinal ligament, which is a clear indicator for instability.
Another advantage of the CT scan is its ability to display the transverse foramen. A suspected distraction or compression of the vertebral artery in the transverse foramen should lead to a CT angiography (CTA).
The accuracy of CTA has improved dramatically during the past decade.22 Nevertheless, the reported sensitivity varies considerably across the studies dealing with this topic.23 In a recent meta-analysis, the sensitivity was calculated to a value of around 80%, if >16-slice scanners were used and neuroradiologist evaluation was performed. The specificity was calculated to be ∼97%.23
Magnetic Resonance Imaging
In the absence of clear indicators of instability in X-ray or CT, a definitive verification of stability is essential to prevent undesirable outcomes with conservative treatment.
In MRI, the focus lies on the assessment of the integrity of the longitudinal ligaments as well the intervertebral disk at the C2–C3 level. A prevertebral hematoma is an indirect indicator, which might help in diagnosing this type of injury.
Assessment of Stability
After having identified the fracture, the most critical step is the decision on the grade of instability. It is mainly determined by the grade of discoligamentous injury at the C2–C3 level.
All widespread classification schemes (Effendi, Levine, Francis) claim to provide a statement about the stability. The criticism of the mentioned classification schemes is that they are based on static radiographs, which do not take into account the functional impairment or soft tissue injury.24
The previously mentioned classification schemes mostly depend on the angulation and translation between the C2 and C3 vertebral body. The international Spine Trauma Study Group has formulated some rules for assessing these values from standard imaging.1 25
To measure the angulation between C2 and C3, the reliability of end plate measures is greater than the posterior wall measurement method.2 26 For translation measurements, plain X-ray provides a more reliable diagnosis than CT.3 26 In severe cases, some indicators that prove instability appear even on conventional radiographs, indicating the need for surgical therapy. Conversely, it is not possible to rule out instability using conventional X-rays alone. The authors therefore recommend a more differentiated diagnostic algorithm, which includes the use of MRI and/or functional imaging under fluoroscopic control.
Treatment Options
A commonly accepted algorithm for decision on conservative or operative treatment does not exist, yet. The indication for surgery usually depends on the estimated amount of instability. Estimating the grade of instability is therefore a critical step in the decision making. Several suggestions have been made to address this problem. In a recent review, the authors have proposed an algorithm that takes assessment of stability into account.27
Nonoperative Treatment
In the most recent review on the management of hangman's fractures by Li et al,28 about three quarters (74%) of all hangman's fractures were treated conservatively. Depending on the Effendi/Levine grade, conservative treatment was performed mainly in Effendi/Levine I and II injuries, whereas Effendi/Levine IIa and III-type injuries were treated operatively. Nonoperative treatment consists of semirigid immobilization using a cervical orthosis for 6 to 12 weeks.29
Halo Vest or Halo Traction
With modern surgical procedures, we see the indication for putting a patient into the halo fixator only in situations where an operative treatment is not possible (due to the general status of the patient) or as a bridging measure until surgery is possible. Halo traction is contraindicated in all hyperextension-traction injuries. The stabilizing effect of the halo vest is definitely lower than that of an internal osteosynthesis.30 31 Complication rates vary from 0 to 100%, depending on the definition of a complication.32 Pin loosening is observed in at least 25%, infections occur in ∼10%, and an overall failure rate of up to 85% of cases is described.32 Additionally, the acceptance rate due to severe patient discomfort (39%) is low.
In selected cases, halo traction can be used for a closed reduction of a locked facet joint (Effendi III) to prepare for an anterior surgical procedure.
Operative Treatment
In unstable lesions, operative treatment is recommended, because nonoperative treatment has a high rate of treatment failure in these cases. Li et al found a 50% pseudarthrosis rate with conservative treatment in Levine IIa and III cases.28 The review of Li et al did not address a secondary neurologic deficit or a poor functional outcome (pain/stiffness), which have a huge impact on patients' quality of life. Koller and Kathrein24 therefore estimated the need for surgical therapy to be higher than the 26% of the cases in the review by Li et al.28
There are several different surgical strategies, with their own advantages and disadvantages. They are described next and are summarized in Table 4.
Table 4. Summary of different surgical strategies and their advantages and disadvantages.
| Anterior plate and interbody graft | Posterior C2–C3 | Posterior C1–C2–C3 | Posterior C2 (Judet) | |
|---|---|---|---|---|
| Approach morbidity | Low | Moderate | Moderate | Moderate |
| Disk pathology is addressed | + | − | − | − |
| Anterior decompression | + | − | − | − |
| Posterior decompression | − | + | + | + |
| Reduction of angulation | + | ? | +++ | ? |
| Reduction facet luxation | − | + | + | + |
| Direct fracture fixation | − | + | + | + |
| Stabilized segments | 1 | 1 | 2 | 0 |
| Fused segments | 1 | 1 | 1–2 | 0 |
Anterior Approach
Because the C2–C3 disk injury is the major determinant of instability, the surgical treatment should involve the C2–C3 motion segment in any unstable traumatic spondylolisthesis of the axis. Due to lesser access morbidity, the standard anterior approaches are commonly preferred over difficult approaches such as the transoral or retropharyngeal approaches (Fig. 5).10 33
Fig. 5.
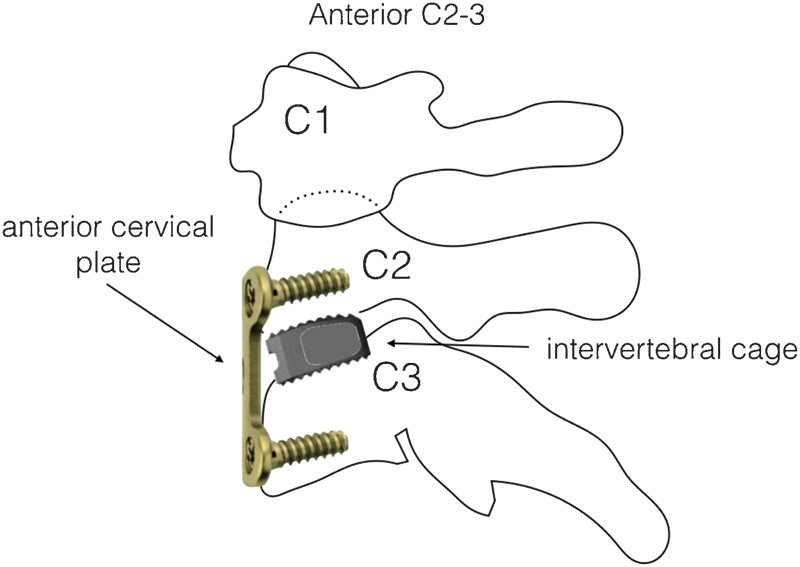
The anterior interbody fusion and stabilization of the C2–C3 segment is the preferred option for an unstable traumatic spondylolisthesis of the axis when there is no necessity for a posterior approach, such as irreducible locked facet joints.
Biomechanical studies show a high stability for both the anterior plating plus intervertebral graft and the posterior screw and rod constructs. A slight but significant advantage for the posterior constructs was observed, however.34 35 But this biomechanical difference has to be weighed against the higher access morbidity of the posterior approach and the functional impairment of atlantocervical fixation in case of impossible pedicle screw placement in C2.
In the rare condition of an intraspinally dislocated C2–C3 disk, spinal cord decompression is possible via an anterior approach only.
Due to the lesser access morbidity, direct access to the main pathology, and nearly biomechanical equivalence, anterior C2–C3 intervertebral fusion and plating is regarded as the standard operation for an unstable traumatic spondylolisthesis of the axis.
Transoral Approach
Anterior C2–C3 fusion is also possible via a transoral approach.36
Because there are excellent alternative approaches and the transoral approach is associated with a significant infection rate, it cannot be recommended as a routine procedure.
Posterior Approach
The posterior approach for treatment of traumatic spondylolisthesis of the axis is necessary in the following conditions:
Locked facet joints or severely displaced, irreducible fractures with impossible closed reduction
Necessity to decompress the vertebral artery
Concomitant fractures of the atlas, which require surgical stabilization
Any contraindication against anterior surgery (e.g., severe scarring due to a prior operation or an impossible approach due to high rigidity of the spine)
Posterior Stabilization and/or Fusion
Because the major instability is at the C2–C3 motion segment, a C2–C3 stabilization is always necessary (Figs. 6, 7, and 8). However, prior to surgery, the number of included levels has to be determined based on the individual fracture morphology. Depending on the anticipated C2 screw purchase, one has to consider to include C1 into the instrumentation, which will cause a severe loss of rotational and flexion/extension capability. This concern might be avoided by a temporary C1 inclusion into the instrumentation to achieve optimal reduction followed by an early implant removal with evidence of a consolidated C2–C3 fusion. However, regaining rotational ability after several months of temporary atlantoaxial fixation is still controversial.
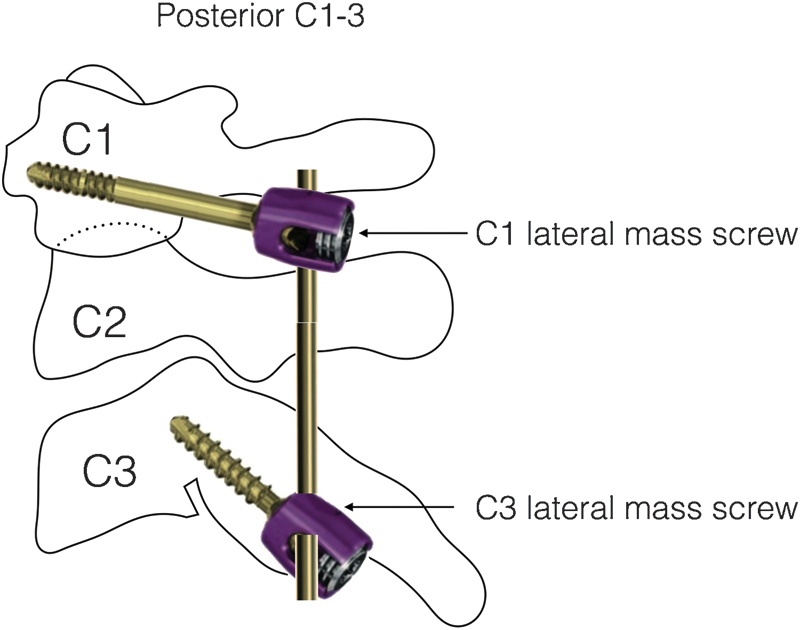
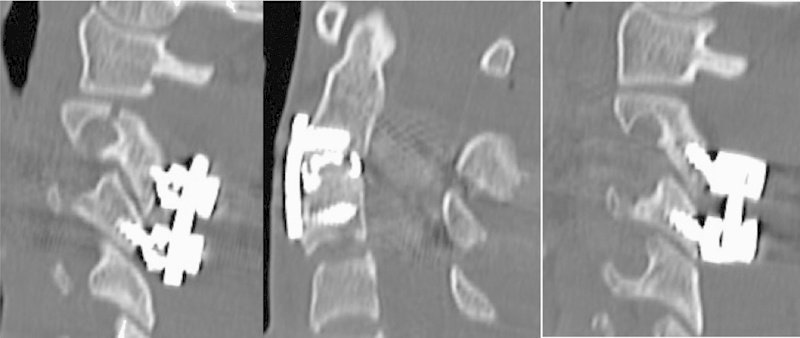
Fig. 6.
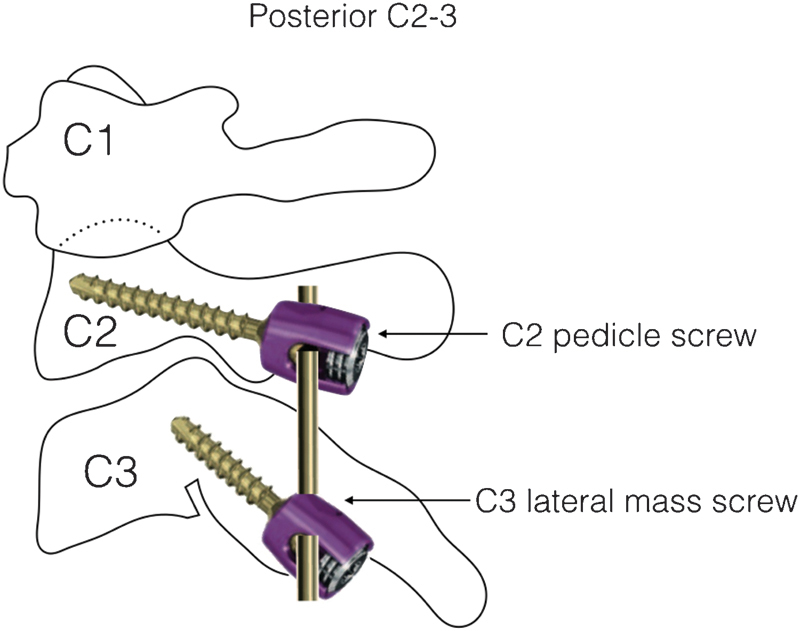
If a posterior approach is necessary (e.g., locked facet joints), posterior C2–C3 stabilization with pedicle screws in C2 and lateral mass screws in C3 is the treatment of choice.
Fig. 7.
If the C2 vertebral body cannot be stabilized sufficiently by posterior C2 pedicle screws (due to severe fragmentation, poor bone stock, intervening vertebral artery, etc.), C1 instrumentation can serve as a salvage option.
Fig. 8.
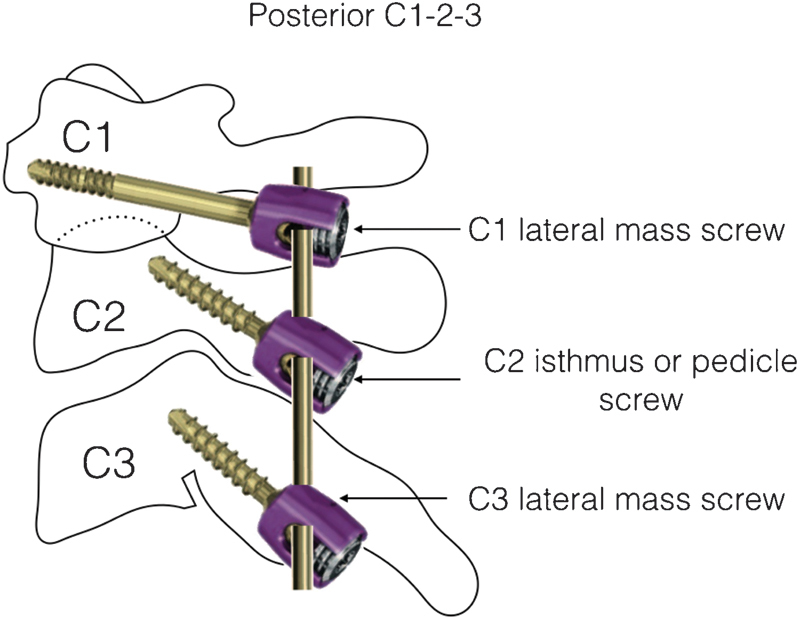
It also possible to include C2 and C1 into the construct to further enhance stability in cases of severe instability. The C2 screws might either be placed transpedicular or into the isthmus.
Direct Screw Osteosynthesis (Leconte/Judet)
Leconte was the first to describe the direct screw osteosynthesis of C2-isthmic fractures in 1964.37 It took until 1984 before the first clinical case series of this technique was published by Borne et al.38 These publications recommended a 20-degree ascending and 20-degree converging screw trajectory for optimal placement (Fig. 9). Recent publications emphasize that such rules of thumb are not feasible in this region due to the high anatomical variations and therefore recommend a preoperative trajectory planning for each patient individually based on CT imaging.39 To ensure the correct placement intraoperatively, either a navigation system should be used or direct visualization of the medial border of the C2 pedicle should be achieved.40 The use of a navigation system also facilitates a percutaneous direct osteosynthesis of the C2 pars, which has been proposed by several authors.41 42 43 44 45
Fig. 9.
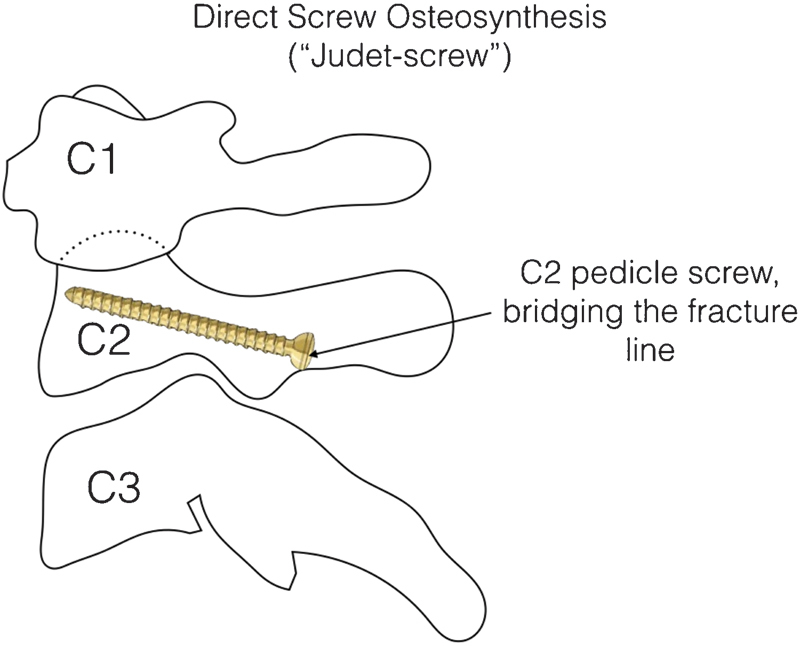
The direct screw osteosynthesis (or “Judet screw”) uses a lag screw effect to bridge and compress the fracture line. Because it does not stabilize the C2–C3 motion segment, it is only effective in stable lesions without any discoligamentous injury at this level (Effendi/Levine type I). Because these injuries show good results with conservative therapy, the authors see no indication for this type of surgery.
A variant of the direct screw osteosynthesis uses bicortical screws and an internal fixator construct with the rod connecting the left and right pedicle screw, which will cause an anterior directed reduction force onto the posterior arch.14 46
Nevertheless, because the isolated direct screw osteosynthesis does not address the C2–C3 instability, in the authors' opinion it is only suitable for type I injuries or maybe type II injuries, which usually also show good results after conservative treatment.
We therefore see the indication of “Judet screw placement” only as a part of a longer internal fixator construct, to adjunct C2–body reposition, when a posterior approach is indicated for other reasons.
Case Example: Posterior-Anterior-Posterior Procedure in a Bilaterally Locked Effendi III Lesion
Although representing an unconventional treatment strategy, the following case is illustrative to discuss the principles in the treatment of traumatic spondylolisthesis of the axis (Figs. 10 to 15).
Fig. 10.
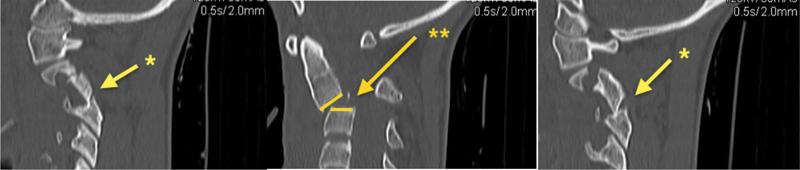
Initial trauma scan of a 28-year-old motor vehicle accident victim. The sagittal reconstructions show a bilaterally locked facet joint C2–C3, which classifies this injury as Effendi/Levine III. *Bilaterally locked facet joints C2–C3. **Severe angulation (40 degrees) and translation C2–C3.
Fig. 15.
Computed tomography scan showing the final result.
Fig. 11.
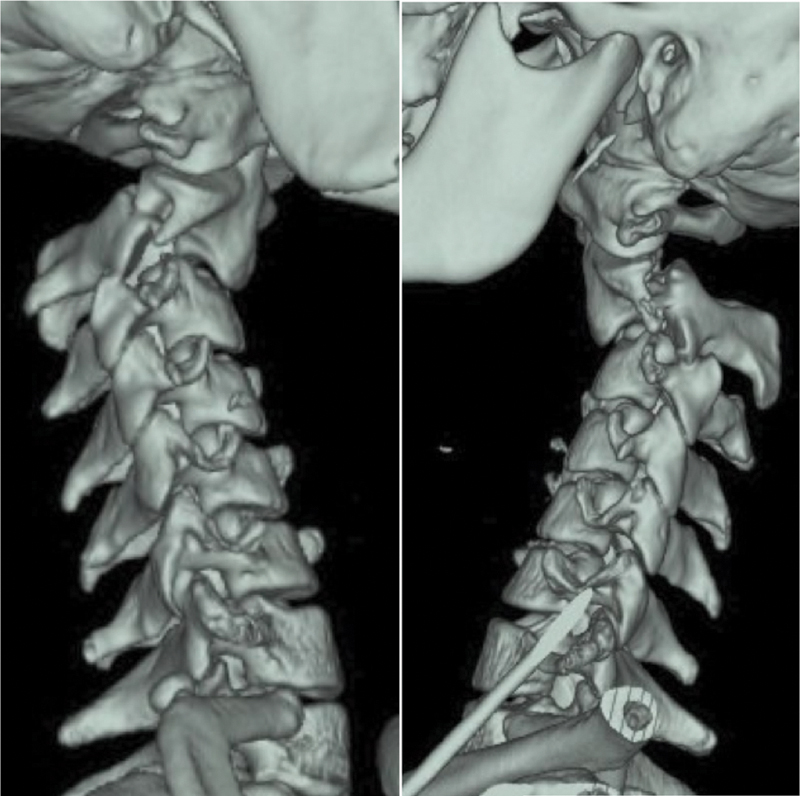
Three-dimensional reconstruction of the initial trauma scan.
Fig. 12.
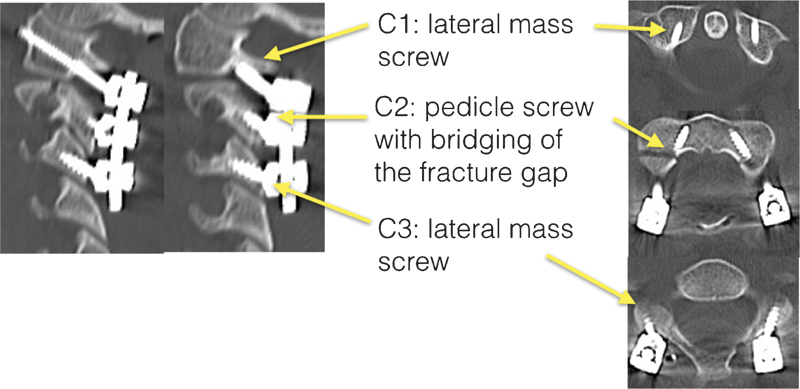
After immediate surgery, the C2–C3 joint is reduced and the fracture gap is bridged. Inclusion of the C1 was performed, because the stability of screw purchase in the C2 vertebral body was doubtful.
Fig. 14.
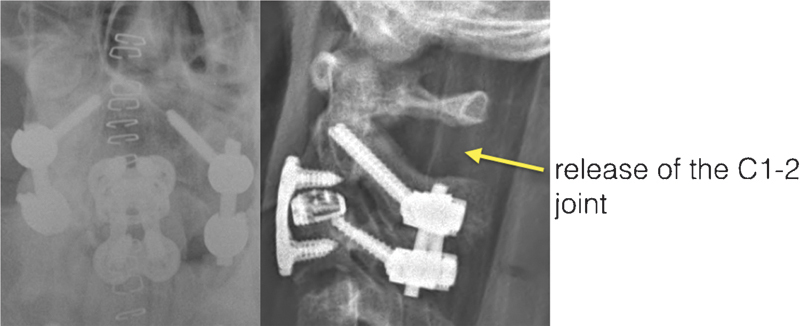
After anterior stabilization, the C2–C3 segment was definitely stable. Therefore, the strongly restricting C1–C2 stabilization could be released again, 3 weeks after the injury.
A 28-year-old man suffered a motor vehicle accident. He was delivered into the emergency room in a conscious state without any neurologic deficit but with severe neck pain and bleeding out of his mouth. His vital signs were normal.
The initial CT trauma scan revealed a traumatic spondylolisthesis of the axis and a mandibular fracture. The vertebral body of the axis was angulated 33 degrees in a kyphotic direction with an anterior translation of more than 5 mm. A fracture line was running into the transverse foramen. The facet joints were locked bilaterally. The injury was classified as Effendi type III.
The transverse foramen fracture and the severe angulation of 33 degrees led to performing a CTA, which showed no signs of VAI.
The severe angulation as well as anterior translation indicated a severe instability due to disruption of the posterior longitudinal ligament and the disk. In addition, there was a high suspicion of a ruptured anterior longitudinal ligament. Therefore, a surgical option was the therapy of choice.
Intraoperative closed reduction of the locked facet joints was not possible, so the persistently locked facet joint forced an open reduction from a posterior approach.
The C2–screw purchase in the anterior vertebral body cortex, which would be necessary to close the fracture in a lag screw technique completely, was not optimal (see Fig. 13, right side), due to moderate bone quality. Additionally high angulation and instability resulted in the intraoperative decision to include C1 temporarily into the construct to achieve optimal reduction.
Fig. 13.
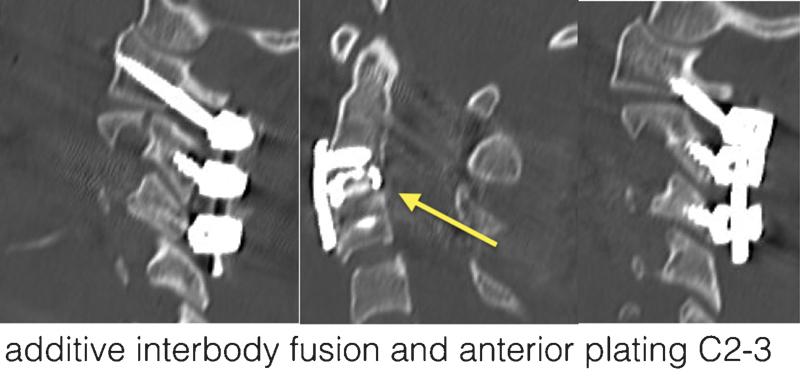
The second surgery addressed the C2–C3 segment and secured stability to this segment. This operation was done 1 week after the injury, using an interbody cage (arrow) and an anterior plate.
A second operation was performed to stabilize C2–C3 from an anterior approach. The additional stability achieved by the anterior intervertebral fusion allowed for a shortening of the posterior instrumentation and release of the atlantoaxial joint complex in a third operation.
There were no complications during the surgeries. The young man had complete recovery and subjectively full range of motion (ROM) was restored.
Several key learning points can be drawn from this case:
The mandibular fracture as a typical concomitant injury, indicating the injury mechanism
The involvement of the transverse foramen and the severe angulation, which both carry a great risk for VAI, triggered the evaluation via CTA
The necessity to use a posterior approach when the facet joints cannot be reduced by closed maneuvers
The emphasis on the main pathology at C2–C3
Bilateral C2 Judet type lag screws to close the fracture lines completely are especially used in highly unstable traumatic spondylolisthesis with significant angulation challenge. Temporary inclusion of C1 into the posterior construct and/or the additional anterior procedure to stabilize C2–C3 is always an option to improve stability. Although a C1–C3 posterior stabilization and fusion rarely fails, the significant reduction of ROM following a C1–C2 fusion justified the additional anterior C2–C3 stabilization and posterior C1–C2 implant removal in this 28-year-old man.
Prognosis
It is generally accepted that neurologic damage is a rare condition in traumatic spondylolisthesis of the axis. The information on outcome should therefore focus on pain, cervical motion, and return to work. In a recent literature review and expert opinion survey, the rate of pain-free patients after 1 year was expected to be ∼75%. The same rate was expected to have regained full self-reported ROM after 1 year.47
The off-work duration varied between 9 to 16 weeks. A return to full activity can be expected in ∼40% of the patients, with another 40% being restricted only in high-impact activity such as contact sports.47
Watanabe et al found a fracture line through the inferior facet of C2 to be a major determinant of residual neck pain,48 which supports the drive to surgical therapy of displaced injuries.
Conclusions
A bilateral separation of the neural arch from the vertebral body of the axis is called traumatic spondylolisthesis of the axis or hangman's fracture.
There are several classification systems, of which the Effendi/Levine classification has gained widespread use.
Assessment of the C2–C3 stability is the major determinant regarding conservative or surgical therapy.
To judge stability, MRI or dynamic fluoroscopy is necessary in many cases. Some other specific features do determine the surgical approach in case of indication for surgery.
Surgical options include anterior as well as posterior procedures. All of these aim at restoring stability at the C2–C3 level.
Footnotes
Disclosures Philipp Schleicher, none Matti Scholz, none Andreas Pingel, none Frank Kandziora, none
References
- 1.de Zouche Marshall J J. Judicial executions. BMJ. 1888;2(1449):779–786. doi: 10.1136/bmj.2.1449.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wood-Jones F. The ideal lesion produced by judicial hanging. Lancet. 1913;181(4662):53. [Google Scholar]
- 3.Schneider R C, Livingston K E, Cave A J, Hamilton G. “Hangman's fracture” of the cervical spine. J Neurosurg. 1965;22:141–154. doi: 10.3171/jns.1965.22.2.0141. [DOI] [PubMed] [Google Scholar]
- 4.James R, Nasmyth-Jones R. The occurrence of cervical fractures in victims of judicial hanging. Forensic Sci Int. 1992;54(1):81–91. doi: 10.1016/0379-0738(92)90083-9. [DOI] [PubMed] [Google Scholar]
- 5.White A A, Panjabi M M. Philadelphia, PA: Lippincott Williams & Wilkins; 1990. Clinical Biomechanics of the Spine. [Google Scholar]
- 6.Saternus K S. [The spectrum of hangman's fracture] Aktuelle Traumatol. 1986;16(5):169–175. [PubMed] [Google Scholar]
- 7.Wozasek G E, Strassegger H, Rizzi C. [Fatal hangman's fracture] Unfallchirurg. 1989;92(1):32–36. [PubMed] [Google Scholar]
- 8.Sköld G. Fractures of the axis caused by hanging. Z Rechtsmed. 1978;80(4):329–331. doi: 10.1007/BF02092331. [DOI] [PubMed] [Google Scholar]
- 9.Saternus K S, Paul E. Bruchformen des Dens axis bei ventralflektierender Krafteinleitung. Aktuelle Traumatol. 1986;16(1):28–33. [PubMed] [Google Scholar]
- 10.Ding T, Maltenfort M, Yang H. et al. Correlation of C2 fractures and vertebral artery injury. Spine (Phila Pa 1976) 2010;35(12):E520–E524. doi: 10.1097/BRS.0b013e3181cd98b6. [DOI] [PubMed] [Google Scholar]
- 11.Greene K A, Dickman C A, Marciano F F, Drabier J B, Hadley M N, Sonntag V K. Acute axis fractures. Analysis of management and outcome in 340 consecutive cases. Spine. 1997;22(16):1843–1852. doi: 10.1097/00007632-199708150-00009. [DOI] [PubMed] [Google Scholar]
- 12.Effendi B, Roy D, Cornish B, Dussault R G, Laurin C A. Fractures of the ring of the axis. A classification based on the analysis of 131 cases. J Bone Joint Surg Br. 1981;63-B(3):319–327. doi: 10.1302/0301-620X.63B3.7263741. [DOI] [PubMed] [Google Scholar]
- 13.Francis W R, Fielding J W, Hawkins R J, Pepin J, Hensinger R. Traumatic spondylolisthesis of the axis. J Bone Joint Surg Br. 1981;63-B(3):313–318. doi: 10.1302/0301-620X.63B3.7263740. [DOI] [PubMed] [Google Scholar]
- 14.Levine A M, Edwards C C. The management of traumatic spondylolisthesis of the axis. J Bone Joint Surg Am. 1985;67(2):217–226. [PubMed] [Google Scholar]
- 15.Eastman A L Chason D P Perez C L McAnulty A L Minei J P Computed tomographic angiography for the diagnosis of blunt cervical vascular injury: is it ready for primetime? J Trauma 2006605925–929., discussion 929 [DOI] [PubMed] [Google Scholar]
- 16.Batnitzky S, Price H I, Holden R W, Franken E A Jr. Cervical internal carotid artery injuries due to blunt trauma. AJNR Am J Neuroradiol. 1983;4(3):292–295. [PMC free article] [PubMed] [Google Scholar]
- 17.Fakhry S M, Jaques P F, Proctor H J. Cervical vessel injury after blunt trauma. J Vasc Surg. 1988;8(4):501–508. doi: 10.1067/mva.1988.avs0080501. [DOI] [PubMed] [Google Scholar]
- 18.Ahmad H A, Gerraty R P, Davis S M, Cameron P A. Cervicocerebral artery dissections. J Accid Emerg Med. 1999;16(6):422–424. doi: 10.1136/emj.16.6.422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Josten C. Die traumatische Spondylolisthese des Axis. Orthopade. 1999;28(5):394–400. doi: 10.1007/s001320050364. [DOI] [PubMed] [Google Scholar]
- 20.Lin J T, Lee J L, Lee S T. Evaluation of occult cervical spine fractures on radiographs and CT. Emerg Radiol. 2003;10(3):128–134. doi: 10.1007/s10140-003-0274-7. [DOI] [PubMed] [Google Scholar]
- 21.Mondschein J, Karasick D. Spondylolysis of the axis vertebra: a rare anomaly simulating hangman's fracture. AJR Am J Roentgenol. 1999;172(2):556–557. doi: 10.2214/ajr.172.2.9930829. [DOI] [PubMed] [Google Scholar]
- 22.Paulus E M Fabian T C Savage S A et al. Blunt cerebrovascular injury screening with 64-channel multidetector computed tomography: more slices finally cut it J Trauma Acute Care Surg 2014762279–283., discussion 284–285 [DOI] [PubMed] [Google Scholar]
- 23.Roberts D J, Chaubey V P, Zygun D A. et al. Diagnostic accuracy of computed tomographic angiography for blunt cerebrovascular injury detection in trauma patients: a systematic review and meta-analysis. Ann Surg. 2013;257(4):621–632. doi: 10.1097/SLA.0b013e318288c514. [DOI] [PubMed] [Google Scholar]
- 24.Koller H Kathrein A Letter to the Editor concerning: a systematic review of the management of hangman's fractures by Xin-Feng Li et al. (2006) Eur Spine J 15:257–269 Eur Spine J 20061591415–1418., author reply 1419–1421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bono C M, Vaccaro A R, Fehlings M. et al. Measurement techniques for upper cervical spine injuries: consensus statement of the Spine Trauma Study Group. Spine (Phila Pa 1976) 2007;32(5):593–600. doi: 10.1097/01.brs.0000257345.21075.a7. [DOI] [PubMed] [Google Scholar]
- 26.Bono C M, Schoenfeld A J, Anderson P A. et al. Observer variability of radiographic measurements of C2 (axis) fractures. Spine (Phila Pa 1976) 2010;35(12):1206–1210. doi: 10.1097/BRS.0b013e3181d9bb58. [DOI] [PubMed] [Google Scholar]
- 27.Kandziora F Schnake K Hoffmann R [Injuries to the upper cervical spine. Part 2: osseous injuries] Unfallchirurg 2010113121023–1039., quiz 1040 [DOI] [PubMed] [Google Scholar]
- 28.Li X-F, Dai L-Y, Lu H, Chen X-D. A systematic review of the management of hangman's fractures. Eur Spine J. 2006;15(3):257–269. doi: 10.1007/s00586-005-0918-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Coric D, Wilson J A, Kelly D LJ Jr. Treatment of traumatic spondylolisthesis of the axis with nonrigid immobilization: a review of 64 cases. J Neurosurg. 1996;85(4):550–554. doi: 10.3171/jns.1996.85.4.0550. [DOI] [PubMed] [Google Scholar]
- 30.Anderson P A Budorick T E Easton K B Henley M B Salciccioli G G Failure of halo vest to prevent in vivo motion in patients with injured cervical spines Spine (Phila Pa 1976) 199116(10, Suppl):S501–S505. [DOI] [PubMed] [Google Scholar]
- 31.Ivancic P C, Telles C J. Neck motion due to the halo-vest in prone and supine positions. Spine (Phila Pa 1976) 2010;35(10):E400–E406. doi: 10.1097/BRS.0b013e3181bb4d2c. [DOI] [PubMed] [Google Scholar]
- 32.Shin J J, Kim S J, Kim T H, Shin H S, Hwang Y S, Park S K. Optimal use of the halo-vest orthosis for upper cervical spine injuries. Yonsei Med J. 2010;51(5):648–652. doi: 10.3349/ymj.2010.51.5.648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang Y, Zhang J, Wang X, Chen D, Yuan W. Application of the cervical subaxial anterior approach at C2 in select patients. Orthopedics. 2013;36(5):e554–e560. doi: 10.3928/01477447-20130426-15. [DOI] [PubMed] [Google Scholar]
- 34.Duggal N, Chamberlain R H, Perez-Garza L E, Espinoza-Larios A, Sonntag V KH, Crawford N R. Hangman's fracture: a biomechanical comparison of stabilization techniques. Spine (Phila Pa 1976) 2007;32(2):182–187. doi: 10.1097/01.brs.0000251917.83529.0b. [DOI] [PubMed] [Google Scholar]
- 35.Chittiboina P, Wylen E, Ogden A, Mukherjee D P, Vannemreddy P, Nanda A. Traumatic spondylolisthesis of the axis: a biomechanical comparison of clinically relevant anterior and posterior fusion techniques. J Neurosurg Spine. 2009;11(4):379–387. doi: 10.3171/2009.4.SPINE08516. [DOI] [PubMed] [Google Scholar]
- 36.Wilson A J, Marshall R W, Ewart M. Transoral fusion with internal fixation in a displaced hangman's fracture. Spine (Phila Pa 1976) 1999;24(3):295–298. doi: 10.1097/00007632-199902010-00022. [DOI] [PubMed] [Google Scholar]
- 37.Leconte P. Paris, France: Masson et Cie; 1964. Fracture et luxation des deux premieres vertebres cervicales; pp. 147–166. [Google Scholar]
- 38.Borne G M, Bedou G L, Pinaudeau M. Treatment of pedicular fractures of the axis. A clinical study and screw fixation technique. J Neurosurg. 1984;60(1):88–93. doi: 10.3171/jns.1984.60.1.0088. [DOI] [PubMed] [Google Scholar]
- 39.El Hawary M A. Determining optimal c2 pedicle screw placement and length in patients with axis traumatic spondylolisthesis: a case series. Global Spine J. 2013;3(2):63–68. doi: 10.1055/s-0033-1345035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ebraheim N, Rollins J R Jr, Xu R, Jackson W T. Anatomic consideration of C2 pedicle screw placement. Spine (Phila Pa 1976) 1996;21(6):691–695. doi: 10.1097/00007632-199603150-00005. [DOI] [PubMed] [Google Scholar]
- 41.Rajasekaran S, Tubaki V R, Shetty A P. Results of direct repair of type 2 hangman fracture using Iso-C3D navigation: 20 cases. J Spinal Disord Tech. 2012;25(5):E134–E139. doi: 10.1097/BSD.0b013e31825bcfe9. [DOI] [PubMed] [Google Scholar]
- 42.Rajasekaran S, Vidyadhara S, Shetty A P. Intra-operative Iso-C3D navigation for pedicle screw instrumentation of hangman's fracture: a case report. J Orthop Surg (Hong Kong) 2007;15(1):73–77. doi: 10.1177/230949900701500116. [DOI] [PubMed] [Google Scholar]
- 43.Yoshida G, Kanemura T, Ishikawa Y. Percutaneous pedicle screw fixation of a hangman's fracture using intraoperative, full rotation, three-dimensional image (O-arm)-based navigation: a technical case report. Asian Spine J. 2012;6(3):194–198. doi: 10.4184/asj.2012.6.3.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sugimoto Y, Ito Y, Shimokawa T, Shiozaki Y, Mazaki T. Percutaneous screw fixation for traumatic spondylolisthesis of the axis using iso-C3D fluoroscopy-assisted navigation (case report) Minim Invasive Neurosurg. 2010;53(2):83–85. doi: 10.1055/s-0030-1247503. [DOI] [PubMed] [Google Scholar]
- 45.Wu Y-S, Lin Y, Zhang X-L. et al. Management of hangman's fracture with percutaneous transpedicular screw fixation. Eur Spine J. 2013;22(1):79–86. doi: 10.1007/s00586-012-2578-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dalbayrak S, Yaman O, Yılmaz M. A new technique in the surgical treatment of Hangman's fractures: Neurospinal Academy (NSA) technique. J Craniovertebr Junction Spine. 2013;4(2):59–63. doi: 10.4103/0974-8237.128529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lewkonia P, Dipaola C, Schouten R, Noonan V, Dvorak M, Fisher C. An evidence-based medicine process to determine outcomes after cervical spine trauma: what surgeons should be telling their patients. Spine (Phila Pa 1976) 2012;37(18):E1140–E1147. doi: 10.1097/BRS.0b013e31825b2c10. [DOI] [PubMed] [Google Scholar]
- 48.Watanabe M, Nomura T, Toh E, Sato M, Mochida J. Residual neck pain after traumatic spondylolisthesis of the axis. J Spinal Disord Tech. 2005;18(2):148–151. doi: 10.1097/01.bsd.0000154459.47467.d6. [DOI] [PubMed] [Google Scholar]


