Abstract
Background: Poor childhood nutritional status has lifetime effects and food insecurity is associated with dietary practices that can impair nutritional status.
Objectives: We assessed concurrent and subsequent associations between food insecurity and height-for-age z scores (HAZs) and body mass index–for-age z scores (BMI-Zs); evaluated associations with transitory and chronic food insecurity; and tested whether dietary diversity mediates associations between food insecurity and nutritional status.
Methods: We used data from the Young Lives younger cohort composed of children in Ethiopia (n = 1757), India (n = 1825), Peru (n = 1844), and Vietnam (n = 1828) recruited in 2002 (round 1) at ∼1 y old, with subsequent data collection at 5 y in 2006 (round 2) and 8 y in 2009 (round 3).
Results: Children from food-insecure households had significantly lower HAZs in all countries at 5 y (Ethiopia, −0.33; India, −0.53; Peru, −0.31; and Vietnam, −0.68 HAZ; all P < 0.001), although results were attenuated after controlling for potential confounders (Ethiopia, −0.21; India, −0.32; Peru, −0.14; and Vietnam, −0.27 HAZ; P < 0.01). Age 5 y food insecurity predicted the age 8 y HAZ, but did not add predictive power beyond HAZ at age 5 y in Ethiopia, India, or Peru. Age 5 y food insecurity predicted the age 8 y BMI-Z even after controlling for the 5 y BMI-Z, although associations were not significant after the inclusion of additional confounding variables (Ethiopia, P = 0.12; India, P = 0.29; Peru, P = 0.16; and Vietnam, P = 0.51). Chronically food-insecure households had significantly lower HAZs than households that were consistently food-secure, although BMI-Zs did not differ by chronic food-insecurity status. Dietary diversity mediated 18.8–30.5% of the association between food security and anthropometry in Vietnam, but mediated to a lesser degree (8.4–19.3%) in other countries.
Conclusions: In 4 countries, food insecurity at 5 y of age was associated with both HAZ and BMI-Z at age 8 y, although the association was attenuated after adjusting for other household factors and anthropometry at age 5 y, and remained significant only for the HAZ in Vietnam.
Keywords: household food security, child growth, weight gain, dietary diversity, longitudinal cohort study
Introduction
Approximately 171 million children under 5 y of age are stunted (1, 2). Poor childhood nutritional status is associated with impaired growth and cognition, lower lifetime educational achievement and earnings, and lower birth weight in the next generation (3–12). Assessing food insecurity, a concept that reflects constrained food availability, accessibility, and utilization (13), is one approach to identifying households at risk of poor nutritional status. In some, but not all studies, food insecurity is associated with decreased dietary intake (14–16), poor child feeding practices (17), and suboptimal health outcomes (18–20) in low- and middle-income countries (15, 21). Although food insecurity is associated with underweight and/or stunting among infants and young children in Bangladesh (17, 22), Brazil (18), Colombia (19, 21), Pakistan (23), Vietnam (22), and Ethiopia (22), food insecurity is not associated with risk of wasting in Colombia (19) or child stunting in Colombia (21) and Nepal (15). Most studies use cross-sectional data, although we identified 2 exceptions (17, 24). Additionally, studies employ different food-insecurity measures, including short- (15) and full-length (22) versions of the Household Food Insecurity Access Scale (HFIAS),13 the USDA Household Food Security Module (HFSM) (23), and locally developed measures (17, 19). It is not clear whether results are inconsistent because populations differ, instruments used to measure food insecurity differ, or associations reflect only short-term fluctuations.
The vast majority of previous studies have been cross-sectional, and do not tell a consistent story about the associations between food insecurity and chronic malnutrition [height-for-age z score (HAZ)] or thinness or wasting [body mass index–for-age z score (BMI-Z) or weight-for-height z score]. One challenge in investigating these associations is that food-security tools are often used to capture food insecurity at specific time points, which can represent differing underlying experiences, including patterns of a single acute episode of food insecurity (pattern 1), intermittent food insecurity (pattern 2), and chronic food insecurity (pattern 3). We expect that food insecurity could have highly significant associations with concurrent thinness and fewer associations with subsequent thinness if households are experiencing pattern 1. However, if households are experiencing patterns 2 or 3, longer-term associations between food security and thinness might also be observed. Because the HAZ captures chronic nutrition, we would expect stronger associations between food insecurity and future HAZs, although durations of household food insecurity would seem relevant.
The primary objectives of these analyses were to assess concurrent and subsequent associations between food insecurity and HAZ and BMI-Z; to consider associations with transitory and chronic food insecurity; and to test whether dietary diversity mediates associations between food insecurity and nutritional status. The older child ages (5 y and 8 y), past the age of peak growth velocity, provide an opportunity to investigate influences on height and thinness in this age group, particularly in light of recent interest in catch-up growth after the 1000 d window (25–27).
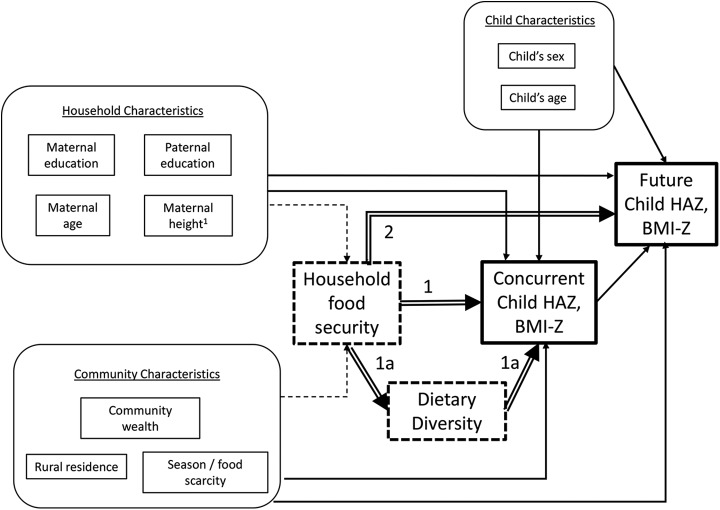
The conceptual framework guiding this research is found in Figure 1. This posits that community and household characteristics are associated with food insecurity and that food insecurity in turn is associated with children’s concurrent and future nutritional status. Community, household, and child factors are posited to influence anthropometry independent of associations between food insecurity and nutritional status.
FIGURE 1.
Conceptual framework of household food security and child anthropometry. Boxes with dashed borders represent the independent variables that were tested in the models. Thick-bordered boxes are the dependent variables. Child characteristics were included in age- and sex-adjusted models. Household, community, and child characteristics were included in fully adjusted models. Double arrows represent the associations that were explored: food security and concurrent anthropometry (1); dietary diversity as a mediator of concurrent anthropometry (1a); and food security and future anthropometry (2). 1Paternal height also influences child anthropometry; however, paternal height was lacking for many children across the 4 countries and it was not included in this analysis. BMI-Z, body mass index–for age z score; HAZ, height-for-age z score.
We had 4 key hypotheses. First, we hypothesized that children from households that experienced current food insecurity were more likely than children from food-secure households to have lower concurrent and subsequent HAZs and BMI-Zs. Second, we hypothesized that adjusting for initial anthropometry and various individual, household, and community characteristics would attenuate but not render these associations nonsignificant. Third, we hypothesized that children from chronically food-insecure households (at both 5 y and 8 y) would have lower HAZs and BMI-Zs than children from intermittently food-insecure households (at either 5 y or 8 y). Fourth, we hypothesized that associations between food security and child anthropometry were partially mediated by dietary diversity.
Methods
Study design and participants
This study used data from the Young Lives (YL) younger cohort, a cohort study of ∼8000 children in Ethiopia, India, Peru, and Vietnam. The YL study team recruited ∼2000 children aged ∼1 y from each country in 2002 (round 1) with subsequent data collection at age 5 y (round 2; Ethiopia, October 2006–January 2007; India, January–July 2007; Peru, October 2006–August 2007; and Vietnam, December 2006–April 2007) and age 8 y (round 3; Ethiopia, October 2009–January 2010; India, August 2009–March 2010; Peru, July 2009–January 2010; and Vietnam, September 2009–January 2010). Children’s ages at each round ranged from 6 to 18 mo (round 1), 4.5 to 5.5 y (round 2), and 7.5 to 8.5 y (round 3). The YL team used multistage sampling designs with the first stage consisting of a selection of 20 sentinel sites. Sampling was pro-poor; for example, in Ethiopia, the most food-insecure areas were the sampling universe. In Peru, the richest 5% of districts were excluded from the sample. Although poor clusters were moderately oversampled, the final samples provided diverse representation of social, geographic, and demographic groups. The sample in India consisted only of households from Andhra Pradesh (since split into Andhra Pradesh and Telangana), whereas the 3 other countries used nationwide samples. The YL team randomly selected ∼100 households with children aged 6–18 mo in each cluster. Additional study methods are described elsewhere (28), and are provided at http://www.younglives.org.uk (29). From age 1 y to age 8 y, the YL cohort lost between 1.5% and 5.7% of the age 1 y sample to attrition (Ethiopia, 114/1999; India, 81/2011; Peru, 106/2052; and Vietnam, 36/2000). From the complete age 8 y dataset, children were excluded for this analysis if they were missing the dependent variables, anthropometry at 5 y (2006) or 8 y (2009) (Ethiopia, 128/1885; India, 105/1930; Peru, 102/1946; and Vietnam 136/1964).
Ethical review
The University of Oxford Ethics Committee and the Peruvian Nutritional Research Institute institutional review board approved YL study protocols. Approval for these analyses was obtained from the University of Pennsylvania and Boston University. Written parental consent was obtained at each round, and verbal child assent was obtained in round 3.
Study indicators
Child anthropometry.
Height was measured with the use of locally made stadiometers with standing plates and moveable head boards accurate to 1 mm. HAZ was calculated with the use of WHO 2006 standards for children 0–59 mo (30) and WHO 2007 standards for older children (31). Weight was measured with the use of calibrated digital balances (Soehnle) with 100 g precision. BMI-Zs also were calculated with the use of WHO growth curves. All anthropometrists were trained and used techniques according to WHO guidelines (32, 33). Birth dates were taken from children’s health cards when available, and mothers’ reports otherwise.
Dietary diversity.
YL collected information on consumption of 11 food groups at age 5 y and 15 food groups at age 8 y. Food groups were combined into the following 7 categories at age 5 y: 1) starches (cereals, roots, and tubers), 2) meat (meat and fish), 3) eggs, 4) legumes and nuts, 5) dairy, 6) fruit and vegetables, and 7) fats and oils. At age 8 y, vitamin A–rich fruits and vegetables were added as an additional food category. Because there is no standard dietary diversity tool for children of this age, after reviewing food groupings used by other researchers (34, 35), we chose to aggregate the questions at age 5 y to 7 food groups; with the addition of questions about vitamin A–rich foods at age 8 y, we aggregated the questions at age 8 y into 8 food groups. We assessed individual dietary diversity by asking the caregiver what food items each child had eaten the previous day, and then summing the number of food groups reported.
Food insecurity.
Different questions were used to capture food insecurity across rounds. At both rounds, respondents were asked about food insecurity in the previous 12 mo. For age 5 y, YL adapted questions from the HFSM (36) with the use of formative research to create a YL adaptation (37) focused on quantitative indicators of food insecurity (food shortage, fewer meals, and smaller portions). At age 8 y, YL used the HFIAS (38), which includes additional domains such as, “In the past 12 mo, did you ever worry that your household would run out of food?” and “Were you or any household member not able to eat the kinds of foods you want because of lack of money?” At age 5 y, caregivers were asked whether households experienced various aspects of food insecurity, whereas at age 8 y, respondents were asked to quantify how frequently this occurred (rarely, sometimes, always or nearly always). We coded the age 8 y responses with the use of the HFIAS coding algorithm; households classified as moderately or severely food-insecure were considered food-insecure. After comparing the specific questions (Table 1), we determined that positive responses at age 5 y to any of the food-security questions except eating less-preferred foods captured households that had to limit food quantity, which is most comparable to HFIAS moderate and severe food-insecurity at age 8 y. Thus, households at age 5 y responding positively to any food-insecurity questions other than eating less-preferred foods were considered food-insecure. Chronic food-insecurity was assessed by comparing food-insecurity status at ages 5 y and 8 y; households that were food-insecure at both ages were considered chronically food-insecure. Households that were food-secure at both times were classified as food-secure, and households that were food-insecure at one but not both time points were classified as transitorily food-insecure.
TABLE 1.
Proportion of households reporting food insecurity in the 12 mo before interview, Young Lives younger cohort1
| Ethiopia (n = 1757) | India (n = 1825) | Peru (n = 1844) | Vietnam (n = 1828) | |
| Age 5 y | ||||
| Categorical: Food-insecure household2 | 34.5 | 8.7 | 22.7 | 9.6 |
| Household had food shortages | 34.5 | 8.7 | 22.7 | 9.6 |
| Eat less-preferred foods | 10.6 | 2.8 | 18.2 | 5.3 |
| Limit portion sizes | 31.4 | 4.2 | 14.6 | 5.5 |
| Skip meals | 26.7 | 3.4 | 4.7 | 1.4 |
| Skip eating for a whole day | 6.7 | 1.0 | 0.8 | 0.1 |
| Borrow food or money for food | 17.1 | 4.7 | 15.7 | 6.2 |
| Individuals forfeit meals for others | 17.4 | 0.2 | 5.9 | 3.0 |
| Age 8 y3 | ||||
| Categorical: Food-insecure household4 | 54.3 | 27.6 | 30.6 | 31.2 |
| Worried that household would run out of food | 66.7 | 26.1 | 69.0 | 61.3 |
| Not able to eat the foods you want | 83.6 | 69.2 | 63.7 | 66.5 |
| Eat a limited range of foods | 75.1 | 32.3 | 43.6 | 59.1 |
| Eat food you did not want to eat | 15.0 | 28.5 | 20.4 | 26.2 |
| Eat less than you wanted | 63.0 | 14.4 | 30.3 | 15.7 |
| Reduce number of meals eaten per day | 44.2 | 7.4 | 14.8 | 7.7 |
| No food to eat | 8.8 | 3.7 | 6.3 | 4.8 |
| Go to bed hungry | 5.7 | 2.6 | 4.0 | 1.4 |
| Not eat for a whole day and night | 2.1 | 1.8 | 1.7 | 0.1 |
| Persistent food insecurity, ages 5 y and 8 y | ||||
| Food secure at both time points | 34.5 | 67.5 | 55.9 | 64.3 |
| Food insecure at age 5 y only | 11.2 | 4.9 | 13.6 | 4.5 |
| Food insecure at age 8 y only | 31.0 | 23.8 | 21.5 | 26.0 |
| Food insecure at both time points | 23.3 | 3.8 | 9.1 | 5.1 |
Values are percentages representing the proportion of households experiencing each condition. For questions about reducing meals or forfeiting meals for others, values represent anyone in the household reducing meals or forfeiting meals for others. HFIAS, Household Food Insecurity Access Scale.
At age 5 y, households were categorized as food insecure if the household responded positively to any of the food insecurity questions other than eating less-preferred foods.
At age 8 y, households are included in the prevalence of a particular experience if they reported any frequency of that condition (i.e., rarely, sometimes, always, or nearly always) and are only excluded if they reported never experiencing that condition.
At age 8 y, households were categorized as food insecure if the household was considered moderately or severely food insecure based on the HFIAS coding algorithm. HFIAS categorizes households as moderately or severely food insecure if someone in the household had to eat a limited variety of foods or foods they really did not want to eat sometimes or often, or if someone in the household had smaller or fewer meals, went to sleep at night hungry, or went 24 h without eating, or if there was no food in the house.
Control variables.
Other measures included community wealth [measured by indexes of asset ownership, housing quality, and service access for other YL households in the same communities (39, 40)], monetary value of all household expenditures in the preceding 2 wk (household consumption), whether interviewed in a food-scarce month, maternal ages, maternal heights, maternal schooling, paternal schooling, and child ages and sex. In an analysis of associations of age 5 y food security with age 8 y anthropometry, we controlled for age 5 y anthropometry to isolate associations of food security with growth at age 8 y that were not acting through growth at age 5 y.
Statistical analyses
We used Stata (version 12.0, 2011) for all analyses. We employed multiple imputation methods with 15 replications (41) with the use of the ice command to impute the following missing covariates: maternal height (n = 279), maternal age (n = 64), rural residence at age 5 y (n = 3), rural residence at age 8 y (n = 3), interviewed in a scarce month at age 5 y (n = 87), interviewed in a scarce month at age 8 y (n = 108), community wealth (n = 2), and food security at age 8 y (n = 12). We used multivariable regressions for HAZ and BMI-Z to examine associations between food insecurity and nutritional status. Results were considered statistically significant at P < 0.05.
Dietary diversity mediation.
We assessed dietary diversity mediation in 2 stages. First, we assessed whether the 3 Baron and Kenny criteria (42) were met: 1) food insecurity was a significant predictor of anthropometric measures, 2) dietary diversity was significantly associated with food insecurity, and 3) when dietary diversity and food insecurity were both included in models predicting anthropometric measures, dietary diversity was significant and the food-insecurity coefficient was smaller than when dietary diversity was not included. Second, when these criteria were met, we assessed mediation levels and calculated P values for Sobel–Goodman tests of mediation.
Results
Household food-insecurity experiences at age 5 y.
The percentages of households experiencing food insecurity ranged from 8.7% (India) to 34.5% (Ethiopia) (Table 1). Ethiopian households were most likely to report that someone had skipped meals for an entire day (6.7%) compared with ≤1% of households in the other countries. More households in each country experienced food shortage, eating less-preferred foods, and smaller portion sizes than skipping meals for an entire day. Borrowing food or money were more common coping mechanisms in Ethiopia (17.1%) and Peru (15.7%) than in India and Vietnam. Forfeiting meals so another person could eat was most common in Ethiopia (17.4%), and 75% of Ethiopian households that reported someone forfeiting meals also reported individuals going without food for an entire day (data not shown).
Household food insecurity at age 8 y.
Because somewhat different food-insecurity measures were used at ages 5 y and 8 y, definitive comparisons between the 2 rounds were not possible. At age 8 y, over 60% of households in Ethiopia, Peru, and Vietnam worried about running out of food, compared with 26.1% of households in India (Table 1). Few households in any of the 4 countries reported that someone had not eaten for a whole day and night. Households experiencing moderate or severe food insecurity ranged from 27.6% (India) to 54.3% (Ethiopia). Eating limited ranges of foods, eating less than wanted, and reducing the number of meals were more common than going to bed hungry or not eating for 24 h. Households that were food-secure at both ages ranged from 34.5% (Ethiopia) to 67.5% (India).
Characteristics of food-insecure households.
In all 4 countries at both ages 5 y and 8 y, food insecurity was significantly negatively associated with community wealth, household consumption, and parental schooling attainment (Supplemental Tables 1 and 2). At age 5 y, maternal ages were significantly higher in food-insecure households in Ethiopia and India than in food-secure households, whereas at age 8 y, maternal ages were not associated with food insecurity in any country. Mothers in food-insecure households were significantly shorter except in India at age 8 y and Ethiopia at both ages 5 y and 8 y. In Ethiopia, a significantly higher proportion of households that experienced food insecurity were interviewed in months that community leaders described as “food scarce,” although this was not true in the other countries. Children’s age and sex were not significantly different for food-insecure households in any country with the exception of children’s ages in Vietnam at age 5 y. Food insecurity had significant negative associations with dietary diversity scores in all countries.
At age 5 y, children from food-secure households in all countries had significantly higher HAZs (Supplemental Table 1). At age 8 y, children from food-secure households in all countries except Ethiopia had significantly higher HAZs than children from food-insecure households (Supplemental Table 2). Mean HAZs increased from age 5 y to age 8 y among both food-secure and food-insecure households in all countries. BMI-Zs did not differ for children from food-secure and food-insecure households at age 5 y, but were significantly higher for Peruvian and Vietnamese children from food-secure households at age 8 y. Mean BMI-Zs decreased from age 5 y to age 8 y among both food-secure and food-insecure households in all countries.
Food insecurity and concurrent anthropometry.
For all countries, in models adjusted for children’s ages and sex only, food insecurity at age 5 y was significantly associated with concurrent HAZ, but not associated with BMI-Z (Table 2). In fully adjusted models, associations with HAZ remained significant in all countries. At age 8 y, food insecurity was significantly associated with HAZ in age- and sex-adjusted models except for in Ethiopia. At age 8 y, food insecurity was significantly associated with BMI-Z in age- and sex-adjusted models in Peru and Vietnam. In fully adjusted models at age 8 y, food insecurity was significantly associated with HAZ and BMI-Z only in Vietnam. We found significant interactions between country and food-insecurity status in pooled estimates, so we have not presented pooled results.
TABLE 2.
Cross-sectional association of food insecurity and child anthropometry at ages 5 y and 8 y, Young Lives younger cohort1
| Ethiopia (n = 1757) |
India (n = 1825) |
Peru (n = 1844) |
Vietnam (n = 1828) |
|||||
| Dependent variable | Age and sex-adjusted | Fully adjusted2 | Age and sex-adjusted | Fully adjusted2 | Age and sex-adjusted | Fully adjusted2 | Age and sex-adjusted | Fully adjusted2 |
| Age 5 y | ||||||||
| HAZ | −0.33*** (−0.48, −0.19) | −0.21** (−0.35, −0.07) | −0.53***(−0.69, −0.38) | −0.32*** (−0.47, −0.17) | −0.31*** (−0.45, −0.18) | −0.14** (−0.24, −0.03) | −0.68*** (−0.98, −0.39) | −0.27** (−0.43, −0.10) |
| BMI-Z | −0.02 (−0.19, 0.15) | −0.02 (−0.20, 0.16) | −0.02 (−0.19, 0.14) | −0.01 (−0.18, 0.15) | −0.07 (−0.16, 0.02) | −0.06 (−0.15, 0.04) | −0.15 (−0.40, 0.10) | −0.13* (−0.26, −0.002) |
| Age 8 y | ||||||||
| HAZ | −0.06 (−0.16, 0.03) | −0.05 (−0.13, 0.03) | −0.21* (−0.34, −0.09) | −0.05 (−0.16, 0.06) | −0.27*** (−0.35, −0.17) | −0.07 (−0.14, 0.01) | −0.40*** (−0.57, −0.23) | −0.17* (−0.26, −0.09) |
| BMI-Z | −0.07 (−0.17, 0.03) | −0.05 (−0.16, 0.05) | −0.03 (−0.15, 0.10) | 0.06 (−0.05, 0.18) | −0.19* (−0.30, −0.07) | −0.09 (−0.18, 0.01) | −0.34** (−0.57, −0.11) | −0.20* (−0.32, −0.08) |
Values are z scores (95% CIs) and represent the difference in anthropometry between children from food-insecure households and children from food-secure households. *P < 0.05; **P < 0.01; ***P < 0.001. BMI-Z, body mass index–for-age z score; HAZ, height-for-age z score.
Adjusted for rural residence, community wealth, whether the household was interviewed in a food-scarce month, maternal age, maternal height, maternal education, paternal education, and child age and sex.
Food insecurity and subsequent anthropometry.
Before adjusting for HAZ at age 5 y, food insecurity at age 5 y was significantly associated with HAZ at age 8 y in all countries (Table 3). After adjusting for HAZ at age 5 y, food insecurity at age 5 y was associated with HAZ at age 8 y in India, Peru, and Vietnam; those associations remained significant after adjusting for additional confounders in Vietnam. Similarly, food insecurity at age 5 y was significantly associated with BMI-Z at age 8 y in all countries except Ethiopia before adjusting for BMI-Z at age 5 y. After adjusting for other confounders, these associations were no longer significant. Food insecurity at age 5 y was significantly associated with BMI-Z at age 8 y in all countries after adjusting for BMI-Z at age 5 y, although these associations were no longer significant after adjusting for additional confounders. Interaction terms between food-security status and HAZ and BMI-Z at age 5 y were not significant (estimates not shown).
TABLE 3.
Food insecurity at age 5 y in relation to anthropometry at age 8 y, Young Lives younger cohort, by country1
| Ethiopia (n = 1757) |
India (n = 1825) |
Peru (n = 1844) |
Vietnam (n = 1828) |
|||||
| Age and sex-adjusted | Fully adjusted2 | Age and sex-adjusted | Fully adjusted2 | Age and sex-adjusted | Fully adjusted2 | Age and sex-adjusted | Fully adjusted2 | |
| Age 8 y HAZ | ||||||||
| Food insecure at age 5 y | −0.28*** (-0.40, −0.16) | −0.17** (−0.29, −0.05) | −0.58*** (−0.73, −0.44) | −0.34*** (−0.48, −0.20) | −0.31*** (−0.45, −0.17) | −0.15* (−0.27, −0.03) | −0.71*** (−1.03, −0.39) | −0.31*** (−0.48, −0.14) |
| Food insecure at age 5 y3 | −0.05 (−0.14, 0.05) | −0.03 (−0.12, 0.06) | −0.15** (−0.25, −0.05) | −0.09 (−0.20, 0.01) | −0.06* (−0.12, −0.005) | −0.04 (−0.10, 0.02) | −0.12* (−0.21, −0.03) | −0.09* (−0.17, −0.01) |
| Age 5 y HAZ4 | 0.70*** (0.64, 0.76) | 0.68*** (0.62, 0.75) | 0.82*** (0.78, 0.86) | 0.77*** (0.73, 0.82) | 0.79*** (0.76, 0.82) | 0.74*** (0.70, 0.79) | 0.87*** (0.82, 0.92) | 0.84* (0.78, 0.90) |
| Age 8 y BMI-Z | ||||||||
| Food insecure at age 5 y | −0.14 (−0.28, 0.01) | −0.07 (−0.18, 0.04) | −0.19* (−0.35, −0.04) | −0.08 (−0.23, 0.07) | −0.16* (−0.28, −0.04) | −0.10 (−0.21, 0.02) | −0.31** (−0.54, −0.08) | −0.15 (−0.32, 0.02) |
| Food insecure at age 5 y3 | −0.13* (−0.24, −0.01) | −0.06 (−0.14, 0.03) | −0.18** (−0.31, −0.05) | −0.07 (−0.19, 0.06) | −0.11**(−0.20, −0.03) | −0.06 (−0.14, 0.02) | −0.19* (−0.34, 0.00) | −0.05 (−0.20, 0.10) |
| Age 5y BMI-Z4 | 0.46*** (0.40, 0.51) | 0.46*** (0.41, 0.50) | 0.68*** (0.60, 0.75) | 0.67*** (0.60, 0.74) | 0.69*** (0.63, 0.76) | 0.67*** (0.61, 0.74) | 0.84*** (0.79, 0.90) | 0.80*** (0.76, 0.85) |
Values are z scores (95% CIs) and represent the difference in anthropometry at age 8 y between children who were from food-insecure households at age 5 y and children from food-secure households at age 5 y. *P < 0.05; **P < 0.01; ***P < 0.001. BMI-Z, body mass index-for-age z score; HAZ, height-for-age z score.
Adjusted for rural residence, community wealth, whether the household was interviewed in a food-scarce month, maternal age, maternal height, maternal education, paternal education, and child age and sex.
Includes age 5 y anthropometry and food security status.
Values represent the change in age 8 y z scores with a 1 z change in age 5 y z scores.
Chronic food insecurity and anthropometry at age 8 y.
Across all countries, households that were food-insecure at both ages 5 y and 8 y had children with significantly lower HAZs than households that were food-secure at both ages (Figure 2A). No such effect was apparent for BMI-Z (Figure 2B). Children from households that were food secure at age 5 y but not at age 8 y had lower mean HAZs than children who were food-secure at age 8 y and not at age 5 y for all countries except Peru. The same pattern held for BMI-Zs only in India.
FIGURE 2.
Anthropometric measures at age 8 y in the Young Lives younger cohort, by persistence of food insecurity and country. Mean HAZ (A) and BMI-Z (B), adjusted for age and sex, by experience of food security at ages 5 y and 8 y. Values are means ± 95% CIs. Sample size: Ethiopia, n = 1757; India, n = 1825; Peru, n = 1844; and Vietnam, n = 1828. Bars within a country with different letters are significantly different, P < 0.05. BMI-Z, body mass index–for-age z score; HAZ, height-for-age z score.
Dietary diversity.
Children in food-insecure households had less diverse diets than children in food-secure households, at both ages 5 y and 8 y (Supplemental Tables 1 and 2), although the food groups consumed varied among countries and across rounds (Supplemental Table 3). Animal-source foods, such as meat, eggs, and dairy products, were less commonly eaten among food-insecure households in all countries, and the differences were almost always significant. Dietary diversity was consistent with more of the association between food insecurity and anthropometry in Vietnam, and less in India (Table 4). In Vietnam, dietary diversity mediated 30.5% and 22.7% of the variation in HAZ associated with food insecurity at ages 5 y and age 8 y, respectively. As previously shown (Table 3), BMI-Z was not significantly associated with food insecurity at age 5 y, and was significantly associated with food insecurity at age 8 y only for Vietnam.
TABLE 4.
Proportion of association between food security and anthropometry mediated by dietary diversity, Young Lives younger cohort1
| Ethiopia | India | Peru | Vietnam | |
| Age 5 y anthropometry | ||||
| HAZ | 10.1* | 8.4*** | 19.3*** | 30.5*** |
| BMI-Z | a,c | a,c | a,c | a |
| Age 8 y anthropometry | ||||
| HAZ | a | c | 14.5*** | 22.7*** |
| BMI-Z | a | a,c | c | 18.8*** |
Values are percentages and are the proportion of change in regression coefficient for FS as a predictor of anthropometry with and without DD in the model. Mediation was determined by modeling FS as a predictor of anthropometry, FS as a predictor of DD, and DD + FS as a predictor of anthropometry. Letters indicate which of the 3 Baron and Kenny assumptions underlying the S-G test were not met. The Baron and Kenny assumptions include the following: FS was a significant predictor of anthropometry (a), FS was a significant predictor of DD (b), and DD was a significant predictor of anthropometry when FS was also in the model (c). If these assumption are met, the S-G test assesses the change in coefficient for FS with and without DD in the model. *P < 0.05; **P < 0.01; ***P < 0.001. BMI-Z, body mass index–for-age z score; DD, dietary diversity; FS, food security; HAZ, height-for-age z score; S-G, Sobel–Goodman.
Discussion
In this large, prospective multicountry study, we found significant associations between household food insecurity and concurrent HAZ and BMI-Z in all countries, although results were attenuated after controlling for potential confounders. Household food insecurity at age 5 y was significantly associated with HAZ and BMI-Z at age 8 y, but those associations were attenuated after controlling for age 5 y HAZ or BMI-Z and other covariates. Specifically, age 5 y food insecurity was associated with decreases of 0.15–0.34 in age 8 y HAZ. However, after adjusting for age 5 y HAZ, the effect was reduced to decreases of 0.03–0.09 in age 8 y HAZ. Age 5 y food insecurity also predicted age 8 y BMI-Z in all countries, even after controlling for age 5 y BMI-Z, although the associations were not significant after inclusion of additional confounding variables. Households that were chronically food-insecure had significantly lower HAZs than households that were consistently food-secure. Children from households that were food-secure at age 5 y but not at age 8 y had lower mean HAZs than children who were food-secure at age 8 y and not at age 5 y for all countries except Peru. BMI-Z did not differ by chronic food-insecurity status. Dietary diversity mediated almost one-third of the associations between food security and anthropometry in Vietnam, but mediated lesser amounts in the other countries. Although food security was associated with subsequent anthropometry, the associations were attenuated and sometimes no longer significant after adjusting for other household factors and previous child anthropometry. This suggests that other household and individual factors were also important predictors, and food-insecurity measures did not always capture sufficient additional information to address the determinants of child anthropometry.
A number of studies have found cross-sectional associations between anthropometry and food security even after adjusting for such variables as maternal age, maternal and paternal schooling, urban/rural setting, household size, income, household ownership, and wealth indexes (17–19, 21–23, 43). For example, a recent 8-country study found that a 10-point increase in the 27-item HFIAS was associated with a 0.20 SD decrease in HAZ (43). Other studies have reported no or more-nuanced results for associations between anthropometry and food security. One recent study reported no association between food insecurity and child underweight, stunting, or anemia in Nepal (15); another found associations between food insecurity and underweight but not stunting in Colombia (21); and another found associations between food insecurity and BMI-Z or weight-for height z score in Brazil (44). Interestingly, in our study, BMI-Z was not associated with food security in any of the 4 countries in cross-sectional analysis at age 5 y, and only in Peru and Vietnam at age 8 y. This finding is consistent with results reported by Kac et al. (44) who reported no significant associations between BMI-Z and food security in Brazilian children after adjusting for confounders. Stunting may contribute to the ability of children from food-insecure households to maintain a BMI that is comparable to that of food-secure children.
Although growth in the age group considered has been less well studied, a recent commentary (25) highlighted evidence that children do recover HAZ, both after age 5 y and during puberty. Previous analysis of the YL younger cohort found that all 4 countries experienced decreases in HAZ between age 1 y and age 5 y; between age 5 y and age 8 y, all 4 countries experienced some increase in HAZ (27). Regardless, there is variability in individual changes in HAZ around that mean, with some children experiencing larger increases, and some experiencing decreases. In a different population, Lundeen et al. (26) noted that increases in HAZ are compatible with continued absolute increases in height deficits; thus, increases in HAZ should be interpreted cautiously.
Only in Vietnam was food security at age 5 y a significant predictor of HAZ at age 8 y after adjusting for covariates and anthropometry at age 5 y. In the other 3 countries, HAZ at age 5 y and additional confounding variables attenuated the effect of household food insecurity on anthropometry at age 8 y. Interestingly, we also found that children who were food-secure at age 5 y and insecure at age 8 y had lower mean HAZs than children who were food-insecure at age 5 y and food-secure at age 8 y, suggesting that the proximity in time to the experience of food insecurity may be important for HAZ, or, alternatively, that there is a greater effect on HAZ from food insecurity at age 8 y than at age 5 y. These results raise additional questions about the meaning of food security. The observed associations may represent a programming effect whereby early food insecurity “programs” limits to future anthropometric growth.
There is limited research about the predictive power of food security at one time point and subsequent anthropometry, particularly with the age group studied herein, although we did identify 2 previous longitudinal studies in different age groups. In rural Bangladesh, Saha et al. (17) demonstrated significantly better trajectories for weight-for-age z score and length-for-age z score among children ages 1–24 mo from food-secure households when compared with mild, moderate, and severely food-insecure households; in Ethiopia, Belachew et al. (24) reported slightly more catch-up growth in adolescent girls ages 13–17 y from food-insecure households. The Bangladesh study followed infants from birth to 24 mo of age and used a local food-security scale based on questions about frequency of food purchases, borrowing or lending money for food, and access to adequate meals and snacks (17). In that study, household food security was associated with greater attained weight and length indexes, and lower proportions of underweight and stunting at 24 mo (17). In Ethiopia, researchers examined the growth of adolescents ages 13–17 y over a 2 y period (24); experiences of food insecurity were measured with the use of 4 of the 18 questions in the HFSM (36) and the coping strategies index (45). Girls who reported food insecurity at baseline were 0.87 cm shorter at baseline than food-secure girls (P < 0.001). However, food-insecure girls exhibited a slightly greater increase in height than food-secure girls during the follow-up period (0.38 cm per year; P = 0.066). Boys’ mean height at baseline and follow-up did not differ by food-security status. The study in Ethiopia found that after adjusting for baseline HAZ, food security was a significant predictor of HAZ at follow-up for girls, but not for boys (24).
Understanding potential pathways between food insecurity and nutritional status is important, but food security is a complex construct that includes availability, access, and utilization (13), and all food-security measures are simplified approaches to capturing the experience. One of the proposed pathways by which food security affects growth is through dietary diversity, with food-secure households consuming a greater variety of foods (22). We found that dietary diversity mediated some of the associations of the food-security measures with anthropometry, particularly in Vietnam. This is in contrast to a recent study in Bangladesh, Ethiopia, and Vietnam, in which dietary diversity did not mediate associations of food security with anthropometry (22). That study focused on younger children, ages 6–60 mo, whereas our analysis focused on slightly older children, ages 5 y and 8 y, and the different results may be due to different roles for dietary diversity and other mediators of child growth, such as child illnesses or maternal depression at different ages (22).
Our study has several limitations. The YL dataset characterizes household food security at 2 ages, 3 y apart, and no information is available about the intervening years; thus, it is not clear whether our characterization of food insecurity represents the usual household situation or more temporary conditions. Because food insecurity was measured at the household level, not the child level, the impact of household food insecurity on the child may have varied across households (18). The questions about food insecurity differed across rounds so the food-insecurity classifications are slightly different and might not have captured identical household conditions. Both food security and dietary diversity are simplified constructs attempting to capture complex dietary and socioeconomic conditions. There is potential for misclassification in both the dietary diversity and food-security scales, which could attenuate the observed associations. Analysis was based on complete cases, which excluded 9.4% of households that completed surveys at ages 5 y and 8 y. This analysis did not incorporate other household and community variables that might also affect growth, such as water, sanitation, hygiene, and infections.
It is important that future studies compare different food-insecurity measures to assess whether they capture the same underlying construct and to determine whether food-insecurity classifications are comparable across instruments. In addition, longitudinal studies are needed to better understand trajectories in anthropometry. Most of what we know about the association between food insecurity and nutritional status is based on cross-sectional data. Until future studies assess the predictive power of the underlying constructs, the prognostic power of food-insecurity measures is not yet clear. Furthermore, household measures of food insecurity are, as their name indicates, aggregate indicators. The food insecurity of individual household members is not captured by such measures. Research on the food insecurity of various household members would add to our understanding of how the age, sex, and position of individuals within households influence their experience of food insecurity.
Governments, nongovernmental organizations, and other institutions working to improve the nutritional status of school-age children should consider several measures of nutritional well-being, and collection of data on anthropometry and food-insecurity status with the use of one of the accepted measures would be beneficial. Program planners and implementers should be cautioned about using food-insecurity measures to identify children who are currently at risk. The HAZ improvements demonstrated in all 4 countries from age 5 y to age 8 y emphasizes the possible importance of nutritional programs for this age group. As shown in previous analysis (46, 47), school-based meal programs in particular may be of value in improving HAZ recovery in countries with moderate and high amounts of stunting.
Acknowledgments
The Young Lives Determinants and Consequences of Child Growth Project team includes, in addition to the coauthors of this paper: Andreas Georgiadis, Santiago Cueto, Le Thuc Duc, Javier Escobal, Subha Mani, and Whitney Schott.
DLH, KAD, BTC, LCF, ADS, TW, MEP, and JRB designed the research questions and analysis; TW and MEP supervised and implemented the data collection; DLH and BTC performed the statistical analysis; DLH, KAD, BTC, and JRB wrote the paper; and DLH, KAD, BTC, and JRB had primary responsibility for the final content. All authors read and approved the final manuscript.
Footnotes
Abbreviations used: BMI-Z, body mass index–for-age z score; HAZ, height-for-age z score; HFIAS, Household Food Insecurity Access Scale; HFSM, Household Food Security Module; YL, Young Lives.
References
- 1.de Onis M, Blossner M, Borghi E. Prevalence and trends of stunting among pre-school children, 1990–2020. Public Health Nutr 2012;15:142–8. [DOI] [PubMed] [Google Scholar]
- 2.UNICEF [Internet]. New York [updated 2014; cited 2014 Apr 5]. Available from: http://www.childinfo.org/malnutrition_nutritional_status.php.
- 3.Adair LS, Fall CHD, Osmond C, Stein AD, Martorell R, Ramirez-Zea M, Sachdev HS, Dahly DL, Bas I, Norris SA, et al. Associations of linear growth and relative weight gain during early life with adult health and human capital in countries of low and middle income: findings from five birth cohort studies. Lancet 2013;382:525–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crookston BT, Schott W, Cueto S, Dearden KA, Engle P, Georgiadis A, Lundeen EA, Penny ME, Stein AD, Behrman JR. Postinfancy growth, schooling, and cognitive achievement: Young Lives. Am J Clin Nutr 2013;98:1555–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haas JD, Martinez EJ, Murdoch S, Conlisk E, Rivera JA, Martorell R. Nutritional supplementation during the preschool years and physical work capacity in adolescent and young adult Guatemalans. J Nutr 1995; 125(4, Suppl)1078S–89S. [DOI] [PubMed] [Google Scholar]
- 6.Hoddinott J, Behrman JR, Maluccio JA, Melgar P, Quisumbing AR, Ramirez-Zea M, Stein AD, Yount KM, Martorell R. Adult consequences of growth failure in early childhood. Am J Clin Nutr 2013;98:1170–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stein AD, Wang M, Martorell R, Norris SA, Adair LS, Bas I, Sachdev HS, Bhargava SK, Fall CH, Gigante DP, et al. Growth patterns in early childhood and final attained stature: data from five birth cohorts from low- and middle-income countries. Am J Hum Biol 2010;22:353–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Victora CG, Adair L, Fall C, Hallal PC, Martorell R, Richter L, Sachdev HS. Maternal, Child Undernutrition Study G. Maternal and child undernutrition: consequences for adult health and human capital. Lancet 2008;371:340–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maluccio JA, Hoddinott J, Behrman JR, Quisumbing A, Martorell R, Stein A. The impact of nutrition during early childhood on education among Guatemalan adults. Econ J 2009;119:734–63. [Google Scholar]
- 10.Deverewx S, Hoddinott J. Improving Food Needs Assessment Methodologies: A ‘Viewpoint’ paper for Food Policy. Mimeo.
- 11.Hoddinott J, Maluccio JA, Behrman JR, Flores R, Martorell R. Effect of a nutrition intervention during early childhood on economic productivity in Guatemalan adults. Lancet 2008;371:411–6. [DOI] [PubMed] [Google Scholar]
- 12.Behrman JR, Calderon MC, Preston SH, Hoddinott J, Martorell R, Stein AD. Nutritional supplementation in girls influences the growth of their children: prospective study in Guatemala. Am J Clin Nutr 2009;90:1372–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jones AD, Ngure FM, Pelto G, Young SL. What are we assessing when we measure food security? A compendium and review of current metrics. Adv Nutr 2013;4:481–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kendall A, Olson CM, Frongillo EA Jr. Relationship of hunger and food insecurity to food availability and consumption. J Am Diet Assoc 1996;96:1019–24, quiz 25–6. [DOI] [PubMed] [Google Scholar]
- 15.Osei A, Pandey P, Spiro D, Nielson J, Shrestha R, Talukder Z, Quinn V, Haselow N. Household food insecurity and nutritional status of children aged 6 to 23 months in Kailali District of Nepal. Food Nutr Bull 2010;31:483–94. [Google Scholar]
- 16.Rosas LG, Harley K, Fernald LC, Guendelman S, Mejia F, Neufeld LM, Eskenazi B. Dietary associations of household food insecurity among children of Mexican descent: results of a binational study. J Am Diet Assoc 2009;109:2001–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saha KK, Frongillo EA, Alam DS, Arifeen SE, Persson LA, Rasmussen KM. Household food security is associated with growth of infants and young children in rural Bangladesh. Public Health Nutr 2009;12:1556–62. [DOI] [PubMed] [Google Scholar]
- 18.Reis M. Food insecurity and the relationship between household income and children's health and nutrition in Brazil. Health Econ 2012;21:405–27. [DOI] [PubMed] [Google Scholar]
- 19.Hackett M, Melgar-Quinonez H, Alvarez MC. Household food insecurity associated with stunting and underweight among preschool children in Antioquia, Colombia. Revista Panamericana De Salud Publica-Pan American Journal of Public Health 2009;25:506–10. [DOI] [PubMed] [Google Scholar]
- 20.Pilgrim A, Barker M, Jackson A, Ntani G, Crozier S, Inskip H, Godfrey K, Cooper C, Robinson S. Does living in a food insecure household impact on the diets and body composition of young children? Findings from the Southampton Women's Survey. J Epidemiol Community Health 2012;66:e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Isanaka S, Mora-Plazas M, Lopez-Arana S, Baylin A, Villamor E. Food insecurity is highly prevalent and predicts underweight but not overweight in adults and school children from Bogota, Colombia. J Nutr 2007;137:2747–55. [DOI] [PubMed] [Google Scholar]
- 22.Ali D, Saha KK, Nguyen PH, Diressie MT, Ruel MT, Menon P, Rawat R. Household food insecurity is associated with higher child undernutrition in Bangladesh, Ethiopia, and Vietnam, but the effect is not mediated by child dietary diversity. J Nutr 2013;143:2015–21. [DOI] [PubMed] [Google Scholar]
- 23.Baig-Ansari N, Rahbar MH, Bhutta ZA, Badruddin SH. Child's gender and household food insecurity are associated with stunting among young Pakistani children residing in urban squatter settlements. Food Nutr Bull 2006;27:114–27. [DOI] [PubMed] [Google Scholar]
- 24.Belachew T, Lindstrom D, Hadley C, Gebremariam A, Kasahun W, Kolsteren P. Food insecurity and linear growth of adolescents in Jimma Zone, Southwest Ethiopia. Nutr J 2013;12:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prentice AM, Ward KA, Goldberg GR, Jarjou LM, Moore SE, Fulford AJ, Prentice A. Critical windows for nutritional interventions against stunting. Am J Clin Nutr 2013;97:911–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lundeen EA, Stein AD, Adair LS, Behrman JR, Bhargava SK, Dearden KA, Gigante D, Norris SA, Richter LM, Fall CH, et al. Height-for-age z scores increase despite increasing height deficits among children in 5 developing countries. Am J Clin Nutr 2014;100:821–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lundeen EA, Behrman JR, Crookston BT, Dearden KA, Engle P, Georgiadis A, Penny ME, Stein AD, Young Lives D. Consequences of Child Growth Project T. Growth faltering and recovery in children aged 1–8 years in four low- and middle-income countries: Young Lives. Public Health Nutr 2014;17:2131–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barnett I, Ariana P, Petrou S, Penny ME, Duc LT, Galab S, Woldehanna T, Escobal JA, Plugge E, Boyden J. Cohort Profile: The Young Lives Study. Int J Epidemiol 2013;42:701–8. [DOI] [PubMed] [Google Scholar]
- 29.Young Lives [Internet]. Oxford (United Kingdom) [cited 2015 May 8]. Available from: http://www.younglives.org.uk/.
- 30.de Onis M, Martorell R, Garza C, Lartey A, Reference WMG. WHO child growth standards based on length/height, weight and age. Acta Paediatr Suppl 2006;450:76–85. [DOI] [PubMed] [Google Scholar]
- 31.de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 2007;85:660–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.World Health Organization Department of Nutrition for Health and Development. WHO child growth standards: training course on child growth assessment (module b). Geneva: WHO, 2008. [Google Scholar]
- 33.United Nations Department of Technical Co-operation for Development and Statistical Office. How to weigh and measure children: Assessing the nutritional status of young children in household surveys. New York: UN, 1986. [Google Scholar]
- 34.FAO Nutrition and Consumer Protection Division. Guidelines for measuring household and individual dietary diversity. Rome (Italy): FAO, 2007. [Google Scholar]
- 35.Kennedy G, Ballard T, Dop M. Guidelines for measuring household and individual dietary diversity. Rome (Italy): FAO of the UN, 2010. [Google Scholar]
- 36.Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to measuring household food security. Alexandria (VA): Food and Nutrition Service, USDA, 2000. [Google Scholar]
- 37.Vargas S, Penny ME. Measuring food insecurity and hunger in Peru: a qualitative and quantitative analysis of an adapted version of the USDA's Food Insecurity and Hunger Module. Public Health Nutr 2010;13:1488–97. [DOI] [PubMed] [Google Scholar]
- 38.Coates J, Swindale A, Bilinsky P. Household Food Insecurity and Access Scale (HFIAS) for measurement of household food access: Indicator guide (v. 3). In: Project FaNTA, ed. Washington (DC): Academy for Educational Development, 2007. [Google Scholar]
- 39.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data–or tears: an application to educational enrollments in states of India. Demography 2001;38:115–32. [DOI] [PubMed] [Google Scholar]
- 40.Schott WB, Crookston BT, Lundeen EA, Stein AD, Behrman JR. Periods of child growth up to age 8 years in Ethiopia, India, Peru and Vietnam: Key distal household and community factors. Soc Sci Med 2013;97:278–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Allison PD. Missing Data. Thousand Oaks (CA): SAGE Publications, 2001. [Google Scholar]
- 42.Baron RM, Kenny DA. The moderator mediator variable distinction in social psychological-research - conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1986;51:1173–82. [DOI] [PubMed] [Google Scholar]
- 43.Psaki S, Bhutta ZA, Ahmed T, Ahmed S, Bessong P, Islam M, John S, Kosek M, Lima A, Nesamvuni C, et al. Household food access and child malnutrition: results from the eight-country MAL-ED study. Popul Health Metr 2012;10:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kac G, Schlussel MM, Perez-Escamilla R, Velasquez-Melendez G, da Silva AA. Household food insecurity is not associated with BMI for age or weight for height among Brazilian children aged 0–60 months. PLoS ONE 2012;7:e45747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Maxwell D, Watkins B, Wheeler R, Collins G. The coping strategies index: Field methods manual. World Food Programme, CARE, 2003. [Google Scholar]
- 46.Greenhalgh T, Kristjansson E, Robinson V. Realist review to understand the efficacy of school feeding programmes. BMJ 2007;335:858–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kristjansson EA, Robinson V, Petticrew M, MacDonald B, Krasevec J, Janzen L, Greenhalgh T, Wells G, MacGowan J, Farmer A, et al. School feeding for improving the physical and psychosocial health of disadvantaged elementary school children. Cochrane Database Syst Rev 2007;(1):CD004676. [DOI] [PubMed] [Google Scholar]