Abstract
BACKGROUND:
Advice has been associated with increased adherence to recommended infant care practices, and may represent a modifiable factor to promote infant health.
METHODS:
A stratified, 2-stage, clustered design, with oversampling of black and Hispanic mothers, was used to survey a nationally representative sample of 1031 mothers of infants aged 2 to 6 months. Survey questions assessed advice received from doctors, birth hospital nurses, family, and media regarding immunization, breastfeeding, sleep position, sleep location, and pacifier use. Weighted frequencies of no advice and advice consistent with recommendations were calculated to obtain prevalence estimates. Multivariable logistic regression analyses were performed to assess factors associated with receipt of recommendation consistent advice.
RESULTS:
Although doctors were the most prevalent source of reported advice, ∼20% of mothers reported no doctor advice for breastfeeding or sleep position, and more than 50% reported no advice regarding sleep location or pacifier use. Reported advice from nurses was generally similar to doctors. The prevalence of any advice from family or media was 20% to 56% for nearly all care practices, and advice given was often inconsistent with recommendations. The only factors that were consistently associated with receipt of recommendation consistent advice were race/ethnicity and parity; black and Hispanic mothers and first-time mothers were more likely to report recommendation consistent advice.
CONCLUSIONS:
Mothers commonly report receiving either no advice or recommendation inconsistent advice from each of the 4 sources we studied. By identifying care practices with low prevalence of recommendation consistent advice from potentially important advisors, our findings highlight opportunities for future intervention.
What’s Known on This Subject:
Parental adherence to recommended infant care practices (eg, breastfeeding; safe sleep) is below targeted goals. Adherence to practice recommendations increases when parents receive appropriate advice from multiple sources such as family and physicians.
What This Study Adds:
Using a nationally representative sample, this study explores the advice mothers receive about safe sleep, immunization, breastfeeding, and pacifier use; the findings suggest infant care practices about which mothers receive little or inappropriate advice, suggesting possible targets for intervention.
A variety of infant care practices are known to impact health outcomes. Medical and public health advocacy groups such as the American Academy of Pediatrics have therefore issued guidelines and recommendations to promote evidence-based practices for immunization,1,2 breastfeeding,3,4 and safe sleep behaviors.5 Although studies have revealed associations between recommendations and maternal infant care practice choices,6–8 adherence to these practices remain below targeted goals.9–13
Advice received by mothers from potentially influential sources such as medical professionals, family, and the media represents a potentially important modifiable factor that may influence mothers’ choices about infant care practices.13–19 However, relatively little is known about the frequency with which mothers receive such advice and the extent to which advice given is consistent with evidence-based guidelines.
The Study of Attitudes and Factors Effecting Infant Care Practices (SAFE) was designed to obtain nationally representative data related to mothers’ choices regarding recommended safe sleep and other infant care practices. Factors surveyed included advice received from a variety of potentially influential sources, and the extent to which the advice was consistent with current recommendations. The scope of advice sources and infant care practice behaviors captured in this nationally representative, cross-sectional survey conducted in 2011–2012, provides a unique opportunity to better understand the quantity and quality of advice reported by mothers across the United States for important infant care practices.
The specific objectives of this report are as follows: (1) to determine whether mothers report receiving advice from doctors, birth hospital nurses, family, and the media about immunization, breastfeeding, sleep position, sleep location, and pacifier use; (2) describe the extent to which the advice they report receiving is consistent with current recommendations; and (3) assess the association between maternal sociodemographic factors and maternal report of receiving recommendation consistent advice.
Methods
The SAFE study used a stratified 2-stage, clustered design to obtain a nationally representative sample of mothers of infants aged 2 to 6 months, with oversampling of Hispanic and non-Hispanic (NH) black mothers. The first stage sampled 32 intrapartum hospitals with at least 100 births reported in the past year, using the 2010 American Hospital Association annual survey of hospitals. Among the 32 hospitals initially selected, 69% agreed to participate; sampling procedures were used to identify replacement hospitals within the same stratum to complete the full sample of 32 hospitals. Institutional review board approval was obtained at all participating institutions.
Sampled hospitals were assigned targets for sampling and enrollment of Hispanic, NH-black, and NH-other race mothers so that ∼1000 completed follow-up surveys were obtained from mothers of infants aged 2 to 6 months, including at least 250 surveys each from Hispanic and NH-black mothers. Mothers were enrolled between January 2011 and February 2013.
Mothers were eligible for the study if they spoke English or Spanish, lived in the United States, and would be providing care for their infant by 2 to 4 months after delivery. At the time of enrollment, mothers providing written informed consent completed a short initial interview to collect demographic information including the following: mother’s age, education and income level; pregnancy and delivery history including infant gender and birth weight and mother’s parity; and contact information for follow-up from Boston University study staff. Mothers were eligible to complete the survey once their infant was >60 days old. Mothers received reminders to complete the survey a few days before the infants’ 60th day of age and then approximately weekly thereafter until completion of the survey or the infants’ 180th day of age. After the infant reached 180 days of age, mothers received no additional reminders, but were still permitted to complete the survey. Eleven mothers completed the survey after the infants’ 180th day of age, with the oldest infant being 227 days of age at the time the survey was completed.
Measures
The follow-up survey included questions about advice received from 4 different sources: doctors, nurses at the hospital where the infant was born, family, and the media, and regarding 5 infant care practices: immunization, breastfeeding, sleep position, sleep location, and pacifier use. All measures were self-reported.
Receipt of Advice
To determine if mothers recalled receiving advice about the different infant care practices from each of the 4 sources, mothers were asked a true/false question as to whether “[Source] has given me advice about [practice]”; for example, “My baby’s doctor has given me advice about where my baby should sleep,” or “My family has given me advice about breastfeeding.” If the mother answered “false,” then she was categorized as receiving “no advice” for that practice from that source. If she answered true, a follow-up question was asked to determine the nature of the advice relative to current recommendations (see below).
Advice Consistency With Recommendations
To categorize advice received as either consistent or not consistent with recommendations, mothers were asked to agree or disagree on a 7-point Likert scale (ranging from 1 = strongly disagree to 7 = strongly agree) with whether “[Source] thinks I should [practice]”; for example, “My family thinks I should get my baby all of the recommended baby shots (vaccinations).” For immunization, breastfeeding, and pacifier use, categorization was based on the response to a single question about each behavior, and responses of 5 to 7 were categorized as “consistent with recommendations.”
For sleep position, the same question stem was asked for each of 3 sleep positions: back, side, or stomach; for example, “The nurses at the hospital where my baby was born think that I should place my baby to sleep on the side.” In keeping with the most recent safe sleep guidelines,5 recommendation consistent advice for sleep position was categorized as a response of 5 to 7 for back sleep only (ie, responses indicating source recommendation of back sleep and any other sleep position were considered not consistent with recommendations).
For sleep location, the question stem was repeated for each of 4 sleep locations: infant’s own bed/own room, infant’s own bed/parents’ room, shared bed for part of night, or shared bed for whole night. Similar to sleep position, advice for sleep location was determined to be consistent with recommendations if a 5 to 7 response was given for room-sharing without bed-sharing only.
Statistical Analysis
All analyses accounted for the stratified 2-stage cluster sample design for both parameter estimates and SEs by using SAS (SAS Institute, Inc, Cary, NC) procedures for complex survey designs. Data were weighted to account for sampling probabilities and dropout, and to reflect the national joint distribution of maternal age and race/ethnicity. As a check on the representativeness of our sample, weighted demographics were compared with the national demographics of mothers delivering in 2011/2012 by using National Center for Health Statistics data.20
Weighted frequencies of no advice and advice consistent or not consistent with recommendations were calculated to obtain prevalence estimates for receipt of advice and consistency of advice with published recommendations. Multivariable logistic regression analyses were performed to assess the association between maternal or infant factors and the likelihood of reporting having received advice consistent with recommendations. The no advice and “received advice not consistent with recommendations” groups were pooled in these logistic regressions to create a binary outcome of receipt of recommendation consistent advice or not. Variables included in the model, selected a priori based on documented associations from previous literature, included maternal age, race/ethnicity, education level, parity, and income, US region of residence, and infant gender, birth weight, and infant age at the time of interview. We elected not to perform analyses for report of pacifier advice because we thought these were unlikely to be informative given the low prevalence of reported advice for pacifier use.
Weighting and analyses were conducted with SAS 9.3 software by using procedures for analyzing complex survey design data; α for all tests was set at 0.05.
Results
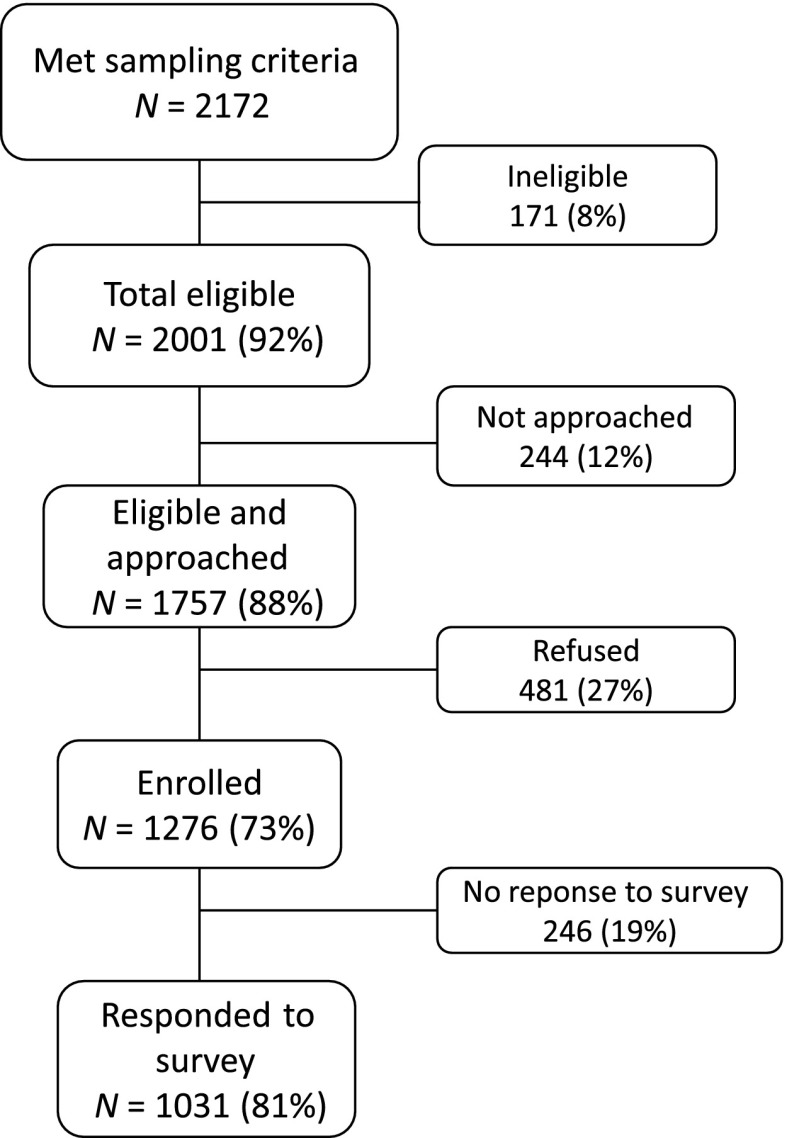
Among 2172 mothers who met sampling criteria, 2001 (92%) were eligible (Fig 1). Of those eligible mothers, 1757 (88%) were approached and of those approached 1276 (73%) were enrolled. When eligible mothers were not approached, the reason was generally related to staff availability or other logistical issues. Mothers who were not approached did not differ from those who were approached with regards to either maternal age or maternal race/ethnicity, which were the only data available for these mothers. The follow-up survey was completed by 1031 mothers (81% of those enrolled). The targeted oversample of at least 25% black and 25% Hispanic mothers was achieved (Table 1). After weighting and adjustment for cluster sampling, our sample demographic closely matched 2011/2012 National Center for Health Statistics data.20
FIGURE 1.
Enrollment and follow-up.
TABLE 1.
Weighted Demographic Characteristics of Study Population
| N (%) | Weighted, % | US Vital Statistics (2011/2012)20 | |
|---|---|---|---|
| Maternal age, y | |||
| 14–19 | 81 (7.9) | 7.6 | 8.1 |
| 20–29 | 569 (55.2) | 52.9 | 51.8 |
| ≥30 | 381 (37.0) | 39.5 | 40.1 |
| Maternal education | |||
| < High school | 152 (14.8) | 14.1 | 17.8 |
| High school/high school equivalent | 240 (23.3) | 22.0 | 25.1 |
| Some college | 315 (30.6) | 27.3 | 28.8 |
| ≥ College degree | 323 (31.4) | 36.6 | 28.3 |
| Parity | |||
| 1 | 389 (37.8) | 37.1 | 39.8 |
| ≥2 | 641 (62.2) | 62.9 | 59.6 |
| Maternal race/ethnicity | |||
| White | 407 (39.5) | 53.8 | 54.1 |
| Black | 252 (24.4) | 12.6 | 14.7 |
| Hispanic | 300 (29.1) | 26.8 | 23.1 |
| Other | 72 (7.1) | 6.9 | 7.3 |
| Income | |||
| <$20 000 | 397 (38.5) | 31.7 | NA |
| $20 000–$49 999 | 274 (26.6) | 27.2 | NA |
| ≥$50 000 | 184 (17.9) | 21.1 | NA |
| Unknown | 175 (17.0) | 20.1 | NA |
| Region | |||
| Northeast | 193 (18.7) | 22.3 | 16.2 |
| Midwest | 158 (15.3) | 13.6 | 21.1 |
| South | 409 (39.7) | 40.0 | 38.1 |
| West | 271 (26.3) | 24.2 | 24.6 |
| Infant age, wk | |||
| 8–11 | 543 (52.6) | 55.2 | a |
| 12–15 | 230 (22.3) | 21.9 | a |
| 16–19 | 121 (11.7) | 10.8 | a |
| ≥20 | 138 (13.4) | 12.1 | a |
| Infant gender | |||
| Girl | 498 (48.2) | 47.7 | 48.8 |
| Boy | 534 (51.7) | 52.3 | 51.2 |
| Infant birth weight, g | |||
| <2500 | 56 (5.5) | 5.0 | 8.0 |
| ≥2500 | 970 (94.5) | 95.0 | 91.9 |
NA, not available.
US Vital Statistics Data not applicable to infant age at time of survey response.
Advice Received
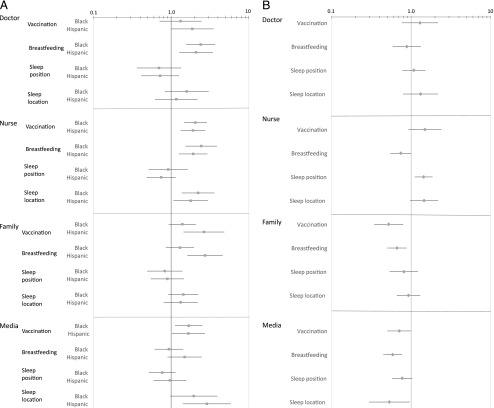
Figure 2 illustrates the extent to which mothers reported receiving advice from a given source for each infant care practice, and the proportion of advice received that was consistent with current American Academy of Pediatrics recommendations.
FIGURE 2.
Prevalence estimates of advice received by source of advice and infant care practice.
Doctors were reported as most often providing advice. However, substantial percentages of mothers reported no advice from doctors; ∼20% of mothers reported no advice from doctors for breastfeeding and sleep position, and >50% reported no advice about sleep location or pacifier use. In addition, although advice from doctors was often consistent with recommendations, as much as 10% to 15% of reported advice was not consistent with recommendations for breastfeeding and pacifier use, and >25% was not consistent with recommendations for sleep position or location.
Generally, when advice was not consistent with recommendations, it was because the mother reported doctor support for both the behavior that was consistent and at least 1 behavior that was not consistent with recommendations; for example, of the 25.7% of mothers reporting sleep position advice from doctors not consistent with recommendations, 85% of those (ie, 22% of all mothers) reported advice in support of back sleep and at least 1 other position, usually side sleep. For sleep location, of the 28.7% of mothers reporting doctor advice not consistent with recommendations, 66% (ie, 19% of all mothers) reported advice for the recommended practice of infant’s own bed/parents’ room and another location.
Report of advice from birth hospital nurses was generally similar to that reported from doctors, except that a lower percentage of mothers reported receiving advice from nurses about immunizations.
Family was reported as a source of advice roughly 30% to 60% of the time, with variable consistency with recommendations. Of family advice reported, more than 20% of advice about breastfeeding, and roughly two-thirds of advice about sleep position, sleep location, and pacifier use was not consistent with recommendations. Media was reported as a source of advice less than half of the time, with the exception of ∼70% of mothers reporting advice about breastfeeding from the media. This advice was frequently not consistent with recommendations; almost 20% of reported breastfeeding advice from the media was not consistent with recommendations. Also noteworthy was that >25% of mothers reporting receipt of media advice about vaccination indicated that the advice was not consistent with recommendations. Similar to health care providers, when advice from family or media was not consistent with recommendations, it was generally because mothers reported advice in support of both the behavior that was consistent and at least 1 behavior that was not consistent with recommendations. However, it was notable that, of the 32.5% of mothers reporting family sleep position advice not consistent with recommendations, 51% (ie, 17% of all mothers) reported advice in support of prone sleep, either with or without another position, and 30% (ie, 10% of all mothers) reported family advice that did not include any support for back sleep.
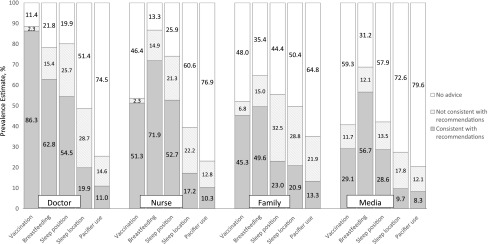
Factors Associated With Receipt of Recommendation Consistent Advice
Figure 3 A and B reveal results of multivariable logistic regression to examine maternal factors associated with the report of receiving advice consistent with recommendations. The only factors that consistently were associated with whether mothers reported receiving recommendation consistent advice were race/ethnicity (Fig 3A) and parity (Fig 3B). In these figures, an odds ratio of >1 (to the right) indicates increased likelihood of reporting receipt of recommendation consistent advice compared with the reference group (white mothers [Fig 3A] and primiparous mothers [Fig 3B]).
FIGURE 3.
A, Adjusted odds ratio (95% CI) of receiving recommendation consistent advice for black and Hispanic versus white mothers (reference) by infant care practice and source. The small squares represent adjusted odds ratio point estimates and bars represent 95% CIs. An adjusted odds ratio of >1 (to the right of the 1.0 line) indicates increased likelihood of reporting receipt of recommendation consistent advice compared with the reference group of white mothers. Variables adjusted for in the model include maternal age, education level, parity, and income, US region of residence and infant gender, birth weight, and infant age at the time of interview. B, Adjusted odds ratio (95% CI) of receiving recommendation consistent advice for multiparous versus primiparous mothers (reference) by infant care practice and source. The small squares represent adjusted odds ratio point estimates and bars represent 95% CIs. An odds ratio of >1 (to the right of the 1.0 line) indicates increased likelihood of reporting receipt of recommendation consistent advice compared with the reference group of primiparous mothers. Variables adjusted for in the model include maternal age, race/ethnicity, education level, and income, US region of residence and infant gender, birth weight, and infant age at the time of interview.
No consistent noteworthy associations were observed for the other potential factors assessed including the following: region, maternal age, education, and income; and infant age, gender, and birth weight.
Race/Ethnicity
In general, black and Hispanic mothers were more likely than white mothers to report receiving recommendation consistent advice. Although not all reached statistical significance, point estimates were consistently greater than 1 for the odds of black versus white and Hispanic versus white mothers reporting recommendation consistent advice from all sources for vaccination, breastfeeding, and sleep location. Sleep position was the only behavior for which point estimates were consistently below 1.0; however, none of these reached statistical significance. For the other 3 behaviors, the most consistent and strongest differences were for advice from hospital nurses, with Hispanic and black mothers each having roughly twice the odds of reporting recommendation consistent advice from nurses compared with white mothers; for Hispanic mothers, the adjusted odds ranged from 1.8 (95% confidence interval [CI]: 1.3–2.1) to 1.9 (95% CI: 1.7–2.6); and for black mothers, the range was 2.1 (95% CI: 1.5–2.9) to 2.4 (95% CI: 1.5–4.0).
Parity
Compared with first time mothers, multiparous mothers had consistently lower odds of reporting recommendation consistent advice from family and media for all behaviors, with a range of 0.52 (95% CI: 0.3–0.8) to 0.93 (95% CI: 0.7–1.3). By contrast, the report of advice from health care providers did not generally differ between primiparous and multiparous mothers.
Discussion
In this nationally representative study of advice for infant care practices, the overall prevalence of mothers of infants reporting that they received advice from doctors, birth hospital nurses, family, or media was 23% to 89% from health care providers, and 20% to 69% for family and the media; and advice received was often not consistent with recommendations. Even for well-accepted recommendations such as supine sleep, breastfeeding, and immunization, up to 45% of mothers reported receiving either no advice or recommendation inconsistent advice from health care professionals. Understanding the prevalence of advice reported by source of advice and the sources of advice that more frequently provide advice that is inconsistent with recommendations may help identify important targets for public health efforts to increase adherence. For health care providers, our findings may suggest a need for increased attention not only to the content of advice delivered, but also to message clarity and delivery. Family and media, meanwhile, appear to represent a particularly untapped resource for advice to mothers of infants.
Previous studies of advice for infant care practices have generally been conducted in specific populations or examined advice for a single infant care practice, particularly sleep position or location. In a 2010 study of predominantly African American mothers enrolled in Supplemental Nutrition Program for Women, Infants, and Children, rates of health care professional advice consistent with recommendations (ie, recommending exclusive supine sleep) were similar to our study findings (56% vs 54.5% of doctors and 46% vs 52.7% of nurses, respectively).14 With respect to physician advice about bed-sharing, the 2013 National Infant Sleep Position study revealed a similarly high prevalence of mothers reporting no receipt of advice from doctors (54% vs 51%)13; we cannot compare specific advice given because we defined recommendation consistent advice for sleep location as advice for room sharing without bed-sharing only, whereas that study assessed physician advice as positive, negative, or neutral toward bed-sharing.
An unexpected finding of our study was that black and Hispanic mothers were more likely than white mothers to report advice consistent with recommendations for all infant care practices except sleep position, despite previous literature revealing white mothers have generally higher rates of adherence with recommendations.12,13,21–23 Perhaps less surprising was that multiparous mothers reported less advice than first time mothers, especially from family and media. In both cases, it may be that certain mothers are perceived by potential advisors as needing less advice, though there is no evidence that some mothers need less advice than others. Differences may also reflect more proactive advice seeking by some mothers, or different perceptions of what constitutes advice, particularly among mothers from different racial or ethnic backgrounds.
It is important to consider that all outcomes in this study were obtained by self-report. We acknowledge that perceived receipt of advice is not the same as actual advice given, and could be impacted by a variety of factors including advice seeking, attitudes toward advice receipt (in general and from a given source), and behavior. Nevertheless, perception seems particularly relevant in the case of advice, where the opportunity for action rests with the advice recipient. We also acknowledge that our sample of 32 hospitals and ∼1000 mothers would not be expected to represent the US population perfectly, though our weighted sample provided demographics well matched to the US population. In addition, these data were collected in 2011–2012; however, we are unaware of subsequent large scale programs likely to have changed the advice patterns identified in this study.
This study was not designed to assess or comment on the merits of existing recommendations, but rather to examine the degree to which mothers of infants report receiving advice, and whether specific maternal factors are associated with receipt of advice consistent with current recommendations. There are a variety of reasons that potential advisors may not give advice or may give advice inconsistent with recommendations. These reasons may include lack of knowledge of the recommendations, a perception of controversy surrounding the recommendations, or actual disagreement with the recommendations. It is possible that some health professionals may choose to avoid controversy or a lengthy conversation about potentially controversial guidelines during a busy, time-pressured practice.
Conclusions
This study provides a comprehensive picture of advice for infant care practices in a nationally representative sample. By identifying care practices with low prevalence of recommendation consistent advice from potentially important advisors, our study provides insights that may be useful to providers, public health professionals, and policy makers that develop and issue recommendations. There is some evidence that a multimodal approach may be most promising in improving the quality and quantity of advice reported by mothers.24 We are currently undertaking an intervention trial at 16 of the SAFE study hospitals to assess a multimodal approach to improving recommendation consistent messaging for infant care practices.
Acknowledegments
The authors want to acknowledge Brenda Cox, PhD for hospital sampling and help with weighting, and Denis Rybin for statistical assistance. We also want to thank the study staff at all 32 of the participating hospitals for their role in data collection and mother enrollment: Baylor University Medical Center, TX; Baystate Medical Center, MA; Ben Taub General Hospital, TX; Bethesda Memorial Hospital, FL; Brookdale Hospital and Medical Center, NY; CamdenClark Medical Center, WV; Delaware County Memorial Hospital, PA; Geisinger Regional Medical Center, PA; Genesys Regional Medical Center, MI; Hamilton Medical Center, GA; Jersey Shore University Medical Center, NJ; Johns Hopkins Hospital and Medical Center, MD; Kaweah Delta Health Care District, CA; Lake Charles Memorial Hospital, LA; Medical Center of Arlington, TX; Moreno Valley Community Hospital, CA; Mount Carmel, OH; Natchitoches Regional Medical Center, LA; Nashville General Hospital, TN; Northcrest Medical Center, TN; Riverside County Regional Medical Center, CA; Riverside Regional Medical Center, VA; Rush-Copley Medical Center, IL; Saint Francis Hospital and Medical Center, CT; Saint Joseph Hospital, CA; Saint Mary’s Health Care, MI; Socorro General Hospital, NM; Sutter Roseville Medical Center, CA; Tacoma General Hospital, WA; Texas Health Presbyterian Hospital Plano, TX; University of California, Davis Medical Center, CA; and Wheaton Franciscan Healthcare, WI.
Glossary
- CI
confidence interval
- NH
non-Hispanic
- SAFE
Study of Attitudes and Factors Effecting Infant Care Practices
Footnotes
Dr Eisenberg led conceptualization and design of the analysis, analyzed and interpreted data, and drafted the initial manuscript; Dr Bair-Merritt contributed to the analysis and interpretation of the data and critically reviewed the manuscript; Dr Colson conceptualized and designed the study, supervised the study, obtained study funding, and critically reviewed the manuscript; Dr Heeren conceptualized and designed the study, analyzed and interpreted data, and critically reviewed the manuscript; Ms Geller contributed to conceptualization and design of the study, supervised acquisition of data, and critically reviewed and revised the manuscript; Dr Corwin conceptualized and designed the study, supervised the study, and critically reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: All phases of this study were supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (grant U10 HD059207). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
COMPANION PAPER: A companion to this article can be found on page e490, online at www.pediatrics.org/cgi/doi/10.1542/peds.2015-1826.
References
- 1.Akinsanya-Beysolow I, Jenkins R, Meissner HC. Advisory Committee on Immunization Practices (ACIP) recommended immunization schedule for persons aged 0 through 18 years–United States, 2013. MMWR Surveill Summ. 2013;62(suppl 1):2–8 [PubMed] [Google Scholar]
- 2.Brady MT, Byington CL, Davies HD, et al. Committee on Infectious Diseases, American Academy of Pediatrics . Recommended childhood and adolescent immunization schedule—United States, 2014. Pediatrics. 2014;133(2):357–363 [DOI] [PubMed] [Google Scholar]
- 3.Eidelman AI, Schanler RJ, Johnston M, et al. Section on Breastfeeding . Breastfeeding and the use of human milk. Pediatrics. 2012;129(3). Available at: www.pediatrics.org/cgi/content/full/129/3/e827 [DOI] [PubMed] [Google Scholar]
- 4.Committee on Health Care for Underserved Women, American College of Obstetricians and Gynecologists . ACOG Committee Opinion No. 361: Breastfeeding: maternal and infant aspects. Obstet Gynecol. 2007;109(2 pt 1):479–480 [DOI] [PubMed] [Google Scholar]
- 5.Moon RY, Task Force on Sudden Infant Death Syndrome . SIDS and other sleep-related infant deaths: expansion of recommendations for a safe infant sleeping environment. Pediatrics. 2011;128(5):1030–1039 [DOI] [PubMed] [Google Scholar]
- 6.Pollack HA, Frohna JG. Infant sleep placement after the back to sleep campaign. Pediatrics. 2002;109(4):608–614 [DOI] [PubMed] [Google Scholar]
- 7.Willinger M, Hoffman HJ, Wu KT, et al. Factors associated with the transition to nonprone sleep positions of infants in the United States: the National Infant Sleep Position Study. JAMA. 1998;280(4):329–335 [DOI] [PubMed] [Google Scholar]
- 8.Crocetti M, Dudas R, Krugman S. Parental beliefs and practices regarding early introduction of solid foods to their children. Clin Pediatr (Phila). 2004;43(6):541–547 [DOI] [PubMed] [Google Scholar]
- 9.US Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Healthy People 2020. Washington, DC. Available at: www.healthypeople.gov/2020/topicsobjectives2020/default. Published 2015. Accessed January 30, 2015
- 10.Elam-Evans LD, Yankey D, Singleton JA, Kolasa M, Centers for Disease Control and Prevention (CDC) . National, state, and selected local area vaccination coverage among children aged 19-35 months - United States, 2013. MMWR Morb Mortal Wkly Rep. 2014;63(34):741–748 [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Breastfeeding Report Card United States. 2014. Available at: www.cdc.gov/breastfeeding/data/reportcard.htm. Accessed January 30, 2015
- 12.Colson ER, Rybin D, Smith LA, Colton T, Lister G, Corwin MJ. Trends and factors associated with infant sleeping position: the national infant sleep position study, 1993-2007. Arch Pediatr Adolesc Med. 2009;163(12):1122–1128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Colson ER, Willinger M, Rybin D, et al. Trends and factors associated with infant bed sharing, 1993–2010: the National Infant Sleep Position Study. JAMA Pediatr. 2013;167(11):1032–1037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Von Kohorn I, Corwin MJ, Rybin DV, Heeren TC, Lister G, Colson ER. Influence of prior advice and beliefs of mothers on infant sleep position. Arch Pediatr Adolesc Med. 2010;164(4):363–369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smith LA, Colson ER, Rybin D, et al. Maternal assessment of physician qualification to give advice on AAP-recommended infant sleep practices related to SIDS. Acad Pediatr. 2010;10(6):383–388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lu MC, Lange L, Slusser W, Hamilton J, Halfon N. Provider encouragement of breast-feeding: evidence from a national survey. Obstet Gynecol. 2001;97(2):290–295 [DOI] [PubMed] [Google Scholar]
- 17.Odom EC, Li R, Scanlon KS, Perrine CG, Grummer-Strawn L. Association of family and health care provider opinion on infant feeding with mother’s breastfeeding decision. J Acad Nutr Diet. 2014;114(8):1203–1207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith PJ, Kennedy AM, Wooten K, Gust DA, Pickering LK. Association between health care providers’ influence on parents who have concerns about vaccine safety and vaccination coverage. Pediatrics. 2006;118(5). Available at: www.pediatrics.org/cgi/content/full/118/5/e1287 [DOI] [PubMed] [Google Scholar]
- 19.Zimicki S, Hornik RC, Verzosa CC, et al. Improving vaccination coverage in urban areas through a health communication campaign: the 1990 Philippine experience. Bull World Health Organ. 1994;72(3):409–422 [PMC free article] [PubMed] [Google Scholar]
- 20.United States Department of Health and Human Services (US DHHS). Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS), Division of Vital Statistics, Natality public-use data 2007–2012, on CDC WONDER Online Database, November 2013. Available at: http://wonder.cdc.gov/natality-current.html. Accessed December 10, 2014
- 21.Centers for Disease Control and Prevention (CDC) . Racial and ethnic differences in breastfeeding initiation and duration, by state - National Immunization Survey, United States, 2004-2008. MMWR Morb Mortal Wkly Rep. 2010;59(11):327–334 [PubMed] [Google Scholar]
- 22.Lahr MB, Rosenberg KD, Lapidus JA. Maternal-infant bedsharing: risk factors for bedsharing in a population-based survey of new mothers and implications for SIDS risk reduction. Matern Child Health J. 2007;11(3):277–286 [DOI] [PubMed] [Google Scholar]
- 23.Fu LY, Colson ER, Corwin MJ, Moon RY. Infant sleep location: associated maternal and infant characteristics with sudden infant death syndrome prevention recommendations. J Pediatr. 2008;153(4):503–508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goodstein MH, Bell T, Krugman SD. Improving infant sleep safety through a comprehensive hospital-based program. Clin Pediatr (Phila). 2015;54(3):212–221 [DOI] [PubMed] [Google Scholar]