Abstract
BACKGROUND:
Differences in antibiotic knowledge and attitudes between parents of Medicaid-insured and commercially insured children have been previously reported. It is unknown whether understanding has improved and whether previously identified differences persist.
METHODS:
A total of 1500 Massachusetts parents with a child <6 years old insured by a Medicaid managed care or commercial health plan were surveyed in spring 2013. We examined antibiotic-related knowledge and attitudes by using χ2 tests. Multivariable modeling was used to assess current sociodemographic predictors of knowledge and evaluate changes in predictors from a similar survey in 2000.
RESULTS:
Medicaid-insured parents in 2013 (n = 345) were younger, were less likely to be white, and had less education than those commercially insured (n = 353), P < .01. Fewer Medicaid-insured parents answered questions correctly except for one related to bronchitis, for which there was no difference (15% Medicaid vs 16% commercial, P < .66). More parents understood that green nasal discharge did not require antibiotics in 2013 compared with 2000, but this increase was smaller among Medicaid-insured (32% vs 22% P = .02) than commercially insured (49% vs 23%, P < .01) parents. Medicaid-insured parents were more likely to request unnecessary antibiotics in 2013 (P < .01). Multivariable models for predictors of knowledge or attitudes demonstrated complex relationships between insurance status and sociodemographic variables.
CONCLUSIONS:
Misconceptions about antibiotic use persist and continue to be more prevalent among parents of Medicaid-insured children. Improvement in understanding has been more pronounced in more advantaged populations. Tailored efforts for socioeconomically disadvantaged populations remain warranted to decrease parental drivers of unnecessary antibiotic prescribing.
What’s Known on This Subject:
Attitudes and knowledge about appropriate management of common childhood illnesses may lead parents to mistakenly believe antibiotics are needed. Differences existed in antibiotic knowledge and attitudes between parents of Medicaid- and commercially insured children and according to other sociodemographic variables.
What This Study Adds:
Despite efforts to decrease unnecessary antibiotic use, misconceptions about antibiotic use persist and continue to be more prevalent among parents of Medicaid-insured children. Tailored efforts for socioeconomically disadvantaged populations remain warranted to decrease parental drivers of unnecessary antibiotic prescribing.
Efforts to reduce antibiotic misuse and overuse are necessary to curb additional increases in antibiotic resistance.1–4 The United States saw decreases in antibiotic use for children during the last 2 decades, likely because of combined benefits of new professional guidelines, educational campaigns for patients and professionals, and introduction of new vaccines.3–5 Although recent studies demonstrate that antibiotic use has decreased and perhaps leveled off, additional reductions in use and improvements in antibiotic selection are believed possible.6–8
Among the factors contributing to pediatric prescribing, parental attitudes and knowledge about common childhood illnesses may lead parents to mistakenly believe antibiotics are needed,9–17 particularly for respiratory tract infections, the most common indication for antibiotics among young children.6,8,16,18 Examples include the belief that antibiotics are needed to treat green nasal discharge, cough illnesses or bronchitis, and common colds or influenza.16,18–25 Providers, in turn, may respond to their perception of parental expectations by prescribing unnecessary antibiotics.26,27 In previous studies, parental knowledge and expectation for antibiotics have been associated with parental age, race or ethnicity, and educational attainment, among other factors.12,19,20,23,26 Data stratified by insurance type, Medicaid versus commercial,19,20 as a proxy for sociodemographic factors, have shown similar associations. With significant attention placed on educating the public about appropriate antibiotic use, it is plausible that misconceptions among parents have decreased over time. It is important to understand whether these changes, if they occurred, were similar across patients of varying insurance status and sociodemographic factors.
Therefore, we sought to examine current knowledge and attitudes about antibiotic use among parents of young children from diverse sociodemographic backgrounds, assess predictors of particular misconceptions, and compare current knowledge and attitudes with those found in a similar survey conducted in 2000.
Methods
Setting and Design
In spring 2013, we conducted a mailed survey of parents with children <6 years old. Recipients were 600 randomly selected members of 1 commercial health plan and 900 randomly selected members of 1 Medicaid managed care plan living in Boston, Cambridge, and 16 other Massachusetts communities whose antibiotic use and resistance patterns had been studied previously.19,28–31 One additional survey mailing was sent to nonresponders. In 2000, surveys were mailed to 2666 randomly sampled families located in only the 16 communities outside Boston and Cambridge. This sample was drawn from a non–managed care Medicaid system, and commercially insured families were drawn from 2 insurance plans (one of which was resampled in 2013). Methods for the 2000 survey were previously published.20 Both studies were approved by the institutional review board of Harvard Pilgrim Health Care.
Survey Instrument
The 2013 survey included selected items from the 2000 survey.19,20 Domains included knowledge of common childhood infections and antibiotic indications, attitudes toward antibiotic use, health care use, and demographics. In the knowledge domain, 10 questions focused on the role of antibiotics for specific childhood infections and on the difference between viral and bacterial infections. Respondents were asked to indicate how often antibiotics were needed (always/almost always, sometimes, never or almost never, don’t know) for 7 questions. Other questions asked whether colds were caused by viruses or bacteria, whether antibiotics were helpful in treating bacterial or viral infections, and, on a 5-point Likert scale, whether a child with a cold would be sicker without antibiotics. We considered responses correct if they reflected recommendations of the Centers for Disease Control and Prevention, Infectious Disease Society of America, and American Academy of Pediatrics and were consistent with published studies.4,19,20,32–34
Additional items were designed to identify parents who expressed strong expectations for receiving antibiotics when hypothetical situations were presented, suggesting they might be dissatisfied if antibiotics were not prescribed. In 2013, we also included new questions about awareness of antibiotic side effects and resistance, methicillin-resistant Staphylococcus aureus, and treatment options for influenza. Finally, we explored the extent of trust families place in specific channels of health information, including physicians’ offices, public health entities, pharmacies, child care or schools, advertisements, news stories on TV, radio, and newspapers, and social media sites. The survey was written in English, and all questions used a seventh-grade Flesch–Kincaid reading level35 but included some medical language when assessing understanding of medical terminology (eg, virus, bacteria, and antibiotics).
2013 Analysis
We compared 2013 demographic characteristics, child care attendance, and trust domains between commercially insured and Medicaid-insured respondents by using χ2 tests. We compared utilization rates by using Poisson regression. We calculated the percentages of correct responses to each of the knowledge questions and affirmative responses to the antibiotic expectation questions between insurance types and compared them using χ2 tests.
We selected 3 knowledge questions for additional analysis because they assessed misconceptions highlighted in previous studies as potentially important drivers of antibiotic overuse: “How often are antibiotics needed for colds or flu?” “How often are antibiotics needed for deep cough or bronchitis?” and “How often are antibiotics needed for runny nose or green nasal discharge?”19,20 Because insurance (public vs commercial) likely serves as a proxy for other sociodemographic variables more directly related to knowledge, we also looked at individual sociodemographic predictors: parent age, race or ethnicity, education, child age (<2 years old or ≥2 years old), and child care participation, for each of these 3 knowledge questions. All outcomes were dichotomized, and predictors were assessed in bivariate logistic regression and a multivariable mixed effects regression model that accounted for clustering by community.
We characterized an affirmative answer to ≥1 antibiotic expectation question as reflecting a proclivity to request or expect antibiotics. The analysis of predictors of a proclivity to request antibiotics used similar bivariate and multivariable models as those for knowledge predictors.
Analysis of Change From 2000 to 2013
We compared responses from the current 2013 survey with the knowledge and attitudes measured by the same items in 2000.20 For this analysis, we excluded respondents from Boston and Cambridge from the 2013 data, limiting respondents to the 16 communities studied in 2000. The total numbers of parent respondents in the 16 communities were 1051 and 353 in 2000 and 2013, respectively,20 with different proportional representation of the individual communities. Therefore, to assess change in responses to specific items over time, we weighted the fraction of respondents from each community, within commercial or Medicaid insurance type, in 2000 to that of the 2013 survey. Using χ2 tests, we compared community-weighted Medicaid-insured respondents in 2000 with Medicaid-insured respondents in 2013 for changes in knowledge and attitudes toward antibiotics. We did the same for the community-weighted sample of commercially insured respondents. A multivariable model controlled for possible confounders and included interaction terms to assess whether particular demographic variables were associated with a differential change in responses over time. All analyses were conducted in SAS 9.4 (SAS Institute, Inc, Cary, NC).36
Results
2013 Survey
Of the 1500 surveys mailed, 707 (47%) completed surveys were returned. Response rates were higher among commercially insured versus Medicaid-insured respondents (n = 354, 59% vs n = 353, 40%). We eliminated 9 respondents who were not parents (1 commercial and 8 Medicaid-insured). Nearly all respondents were mothers, and the groups did not differ by child age or gender (Table 1). The proportion of commercially insured children in child care was higher (68% vs 54%, P < .01) and parents of Medicaid-insured children were more likely to be ≤30 years old, to be nonwhite, and to have less than a college education (P < .01).
TABLE 1.
Demographics for the 2013 Survey and Comparison of Demographics Between 2000 and 2013 Samples
| 18 Communities (Including Boston and Cambridge) | 16 Communities,a Commercial Insurance, Unweighted | 16 Communities,b Medicaid Insurance, Unweighted | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 2013 | 2000 | 2013 | 2000 | 2013 | |||||
| Commercial | Medicaid | P | Commercial | Commercial | P | Medicaid | Medicaid | P | |
| Response rate | 59% | 40% | 54% | 61% | 32% | 39% | |||
| No. parent surveys | 353 | 345 | 776 | 189 | 275 | 164 | |||
| Respondent = mother | 304 (86) | 333 (97) | <.01 | 689 (89) | 167 (88) | NS | 265 (96) | 157 (96) | NS |
| Age (y) | <.01 | NS | NS | ||||||
| <20 | 1 (0) | 15 (4) | 2 (0) | 1 (1) | 22 (8) | 8 (5) | |||
| 21–30 | 53 (15) | 190 (55) | 176 (23) | 35 (19) | 134 (49) | 92 (56) | |||
| 31–40 | 226 (64) | 112 (33) | 486 (63) | 115 (61) | 96 (35) | 53 (33) | |||
| 41–50 | 70 (20) | 26 (8) | 106 (14) | 37 (20) | 20 (7) | 10 (6) | |||
| 50+ | 3 (1) | 1 (0) | 5 (1) | 1 (1) | 3 (1) | 0 (0) | |||
| Ethnicity | |||||||||
| Latino or Hispanicc | 38 (11) | 127 (37) | <.01 | NA | c | NA | c | ||
| Race | <.01 | <.01 | <.01 | ||||||
| White | 282 (80) | 167 (48) | 684 (91) | 148 (79) | 207 (81) | 70 (43) | |||
| Latino or Hispanic | NA | NA | 16 (2) | 19 (10) | 14 (5) | 44 (27) | |||
| African American | 20 (6) | 90 (26) | 4 (1) | 1 (1) | 9 (4) | 20 (12) | |||
| Asian | 19 (5) | 18 (5) | 27 (4) | 8 (4) | 2 (1) | 10 (6) | |||
| Otherd | 32 (9) | 70 (20) | 24 (4) | 12 (6) | 24 (9) | 20 (12) | |||
| Education | <.01 | NS | <.05 | ||||||
| College graduate | 261 (74) | 42 (12) | 506 (66) | 136 (72) | 59 (22) | 18 (11) | |||
| High school graduate or some college | 89 (25) | 262 (77) | 257 (33) | 51 (27) | 183 (67) | 129 (80) | |||
| Less than high school | 3 (1) | 36 (11) | 9 (1) | 2 (1) | 31 (11) | 15 (9) | |||
| Female child (yes) | 184 (52) | 158 (46) | NS | 364 (47) | 98 (52) | NS | 133 (49) | 83 (52) | NS |
| Day care (yes) | 239 (68) | 186 (54) | <.01 | 509 (66) | 125 (66) | NS | 165 (61) | 76 (46) | <.01 |
| Child age | NS | NS | NS | ||||||
| 0–<12 mo | 52 (15) | 40 (12) | 62 (8) | 26 (14) | 33 (12) | 18 (11) | |||
| 12–<24 mo | 60 (17) | 44 (13) | 118 (16) | 35 (19) | 40 (15) | 25 (15) | |||
| 24–<48 mo | 119 (34) | 115 (34) | 272 (36) | 57 (30) | 91 (34) | 55 (34) | |||
| 48–<60 mo | 71 (20) | 88 (26) | 155 (21) | 42 (22) | 44 (16) | 43 (26) | |||
| 60–<72 mo | 48 (14) | 56 (16) | 147 (19) | 28 (15) | 59 (22) | 22 (13) | |||
NA, not applicable; NS, nonsignificant.
We excluded parent respondents from Boston and Cambridge from the 2013 data, limiting respondents to the 16 communities studied in 2000.
To assess change in responses to specific items over time, we weighted the fraction of respondents from each community, within commercial or Medicaid insurance type, in 2000 to that of the 2013 survey.
Data on race and ethnicity were collected in different categories in the 2 study years. For the multivariable modeling and comparison across years, Latino or Hispanic ethnicity in 2013 was recoded as a category of race. A global P value for all categories is reported.
The Other category includes Native American, Alaska Native, and those who answered multiple categories for race.
The average number of reported antibiotic courses over the past year was <1 among both Medicaid-insured and commercially insured children (P = .27). Few parents reported giving their child an antibiotic without talking to a physician first (3% vs 5%, commercial vs Medicaid, P = .29). Similarly, very few reported requesting any specific antibiotic during a clinical encounter (2% vs 4%, commercial vs Medicaid, P = .18). Medicaid-insured parents generally expressed more concern for side effects from antibiotics compared with those commercially insured (Table 1). More commercially insured parents had heard of methicillin-resistant Staphylococcus aureus compared with those insured by Medicaid (59% vs 36%, P < .01). Approximately three-quarters of parents reported that their child received the influenza vaccine for the current season, with no difference by insurance type (P = .35). Commercially insured parents were more aware of a prescription medicine to treat influenza than Medicaid-insured parents (33% vs 13%, P < .01).
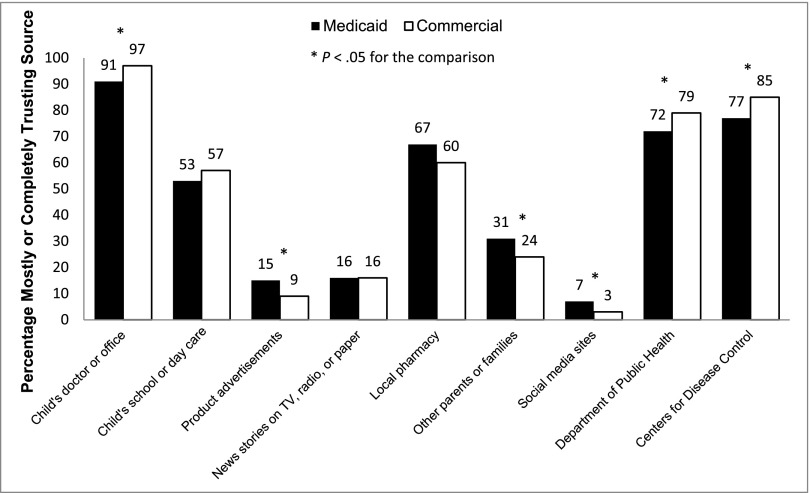
Parents expressed high levels of trust in their physician to provide advice on prevention of coughs, colds, and the flu (Fig 1). Other sources of information trusted by parents included the local department of public health and the Centers for Disease Control and Prevention, followed by pharmacists and child care or schools. Parents were less likely to trust advertisements and social media sites or online forums. Differences in trust between commercially insured and Medicaid-insured respondents were observed (Fig 1).
FIGURE 1.
Parental trust in sources of information for prevention of coughs, colds, and flu, 2013.
Medicaid-insured parents were less likely than those with commercial insurance to answer knowledge questions correctly for nearly all questions (Table 2). For example, “How often are antibiotics needed for colds or flu?” was answered correctly by a greater proportion of commercially insured parents (78% vs 44%, P < .01), as was the question about antibiotics for green nasal discharge (53% vs 38%, P < .01). Only a small minority answered the item about deep cough or bronchitis correctly, with no difference between commercially insured and Medicaid-insured parents (16% vs 15%, P = .66). Parents with commercial insurance were less likely to endorse that they would rather give their child an antibiotic that may not be needed rather than wait to see whether an illness resolved (6% vs 21%, Medicaid P < .01), with similar patterns for other antibiotic expectation questions (Table 2).
TABLE 2.
2013 Responses for Antibiotic Knowledge and Attitude Questions, by Insurance Type
| Acceptable Response | Commercial Insurance, n (%) | Medicaid Insurance, n (%) | P | |
|---|---|---|---|---|
| Knowledge | ||||
| 1. How often are antibiotics needed for sore throat? | Sometimes or almost never | 321 (93) | 255 (78) | <.01 |
| 2. How often are antibiotics needed for colds or flu?a | Almost never | 268 (78) | 143 (44) | <.01 |
| 3. How often are antibiotics needed for ear infection? | Almost always or sometimes | 321 (91) | 285 (85) | .01 |
| 4. How often are antibiotics needed for runny nose or green nasal discharge?a | Almost never | 181 (53) | 124 (38) | <.01 |
| 5. How often are antibiotics needed for deep cough or bronchitis?a | Almost never | 56 (16) | 49 (15) | .66 |
| 6. How often are antibiotics needed for middle ear fluid? | Sometimes or almost never | 194 (56) | 144 (44) | <.01 |
| 7. How often are antibiotics needed for strep throat? | Almost always | 290 (84) | 203 (62) | <.01 |
| 8. Are most colds caused by bacteria or viruses? | Viruses | 294 (83) | 202 (59) | <.01 |
| 9. Are antibiotics helpful in treating bacterial, viral, or both? | Bacterial | 252 (71) | 112 (33) | <.01 |
| 10. If my child does not receive an antibiotic for a cold, he or she will be sick for a longer time. | Disagree or strongly disagree | 259 (74) | 174 (52) | <.01 |
| Tendency to expect antibiotics | ||||
| 1. I will take my child to another doctor if I expect an antibiotic and don’t receive one.a | Strongly agree or agree | 32 (9) | 77 (23) | <.01 |
| 2. If I expect an antibiotic, I am less satisfied if I don’t receive one.a | Strongly agree or agree | 49 (14) | 81 (24) | <.01 |
| 3. I would rather give my child antibiotic than wait and see if he or she needed it.a | Strongly agree or agree | 22 (6) | 69 (21) | <.01 |
| High concern for antibiotic use | ||||
| 1. Decided not to give an antibiotic when it was prescribed | Yes | 15 (4) | 9 (3) | .24 |
| 2. Concerned for allergic reaction | Very concerned | 30 (9) | 59 (17) | <.01 |
| 3. Concerned for diarrhea or other side effects from antibiotics | Very concerned | 27 (8) | 52 (15) | <.01 |
| 4. Concerned for the development of antibiotic resistance in your child | Very concerned | 68 (19) | 68 (20) | .73 |
| 5. Concerned for the development of antibiotic resistance in community | Very concerned | 44 (13) | 54 (16) | .18 |
| 6. Concerned that antibiotics will affect your child’s natural ability to fight infection | Very concerned | 56 (16) | 73 (22) | .05 |
Explored in bivariate and multivariable modeling.
In bivariate analyses, parental age >30 years and college or more education were associated with answering the questions about colds and flu, green nasal discharge, and bronchitis correctly. Child care attendance was also associated with a correct response for 2 of the 3 questions (colds or flu and green nasal discharge, P < .05). Race was an inconsistent predictor of knowledge. African American respondents were more likely to know that antibiotics are not needed for bronchitis (odds ratio [OR] 1.87; 95% confidence interval [CI], 1.03–3.38) but less likely to correctly answer that antibiotics were not needed for colds and flu or for green nasal discharge (OR 0.16; 95% CI, 0.09–0.28 and 0.53; 95% CI, 0.31–0.89). When we controlled for other sociodemographic predictors, the effect of insurance was attenuated while other demographic attributes remained significant, including education, race, and parental age. Predictors varied for each model, demonstrating the complex relationships of these factors (Table 3).
TABLE 3.
Multivariable Model for Predictors of a Correct Knowledge Response, 2013
| Effect | Reference Group | Knowledge Question | ||
|---|---|---|---|---|
| How Often Are Antibiotics Needed for Colds or Flu?, OR (CI) | How Often Are Antibiotics Needed for Runny Nose or Green Nasal Discharge?, OR (CI) | How Often Are Antibiotics Needed for Deep Cough or Bronchitis?, OR (CI) | ||
| Insurance (Medicaid) | Commercial | 0.81 (0.51–1.30) | 0.77 (0.50–1.20) | 0.99 (0.54–1.80) |
| Education | ||||
| Less than high school | College | 0.19 (0.08–0.49)a | 0.51 (0.23–1.17) | 0.58 (0.17–1.95) |
| Completed high school | College | 0.43 (0.27–0.68)a | 0.60 (0.39–0.91)a | 0.91 (0.52–1.59) |
| Age >30 y | Age ≤30 y | 2.35 (1.57–3.50)a | 1.11 (0.76–1.64) | 2.13 (1.24–3.68)a |
| Race or ethnicity | ||||
| Hispanic or Latino | White | 0.50 (0.31–0.83)a | 1.39 (0.87–2.21) | 1.51 (0.81–2.80) |
| African American | White | 0.30 (0.16–0.55)a | 0.78 (0.43–1.41) | 2.55 (1.30–5.01)a |
| Other | White | 0.37 (0.21–0.64)a | 0.99 (0.59–1.64) | 1.35 (0.68–2.68) |
| Child age ≥2 y | Age <2 y | 0.96 (0.62–1.49) | 0.77 (0.52–1.12) | 1.07 (0.63–1.80) |
| Child in child care | Yes | 1.70 (1.14–2.53)a | 1.34 (0.94–1.92) | 1.03 (0.64–1.68) |
Statistically significant.
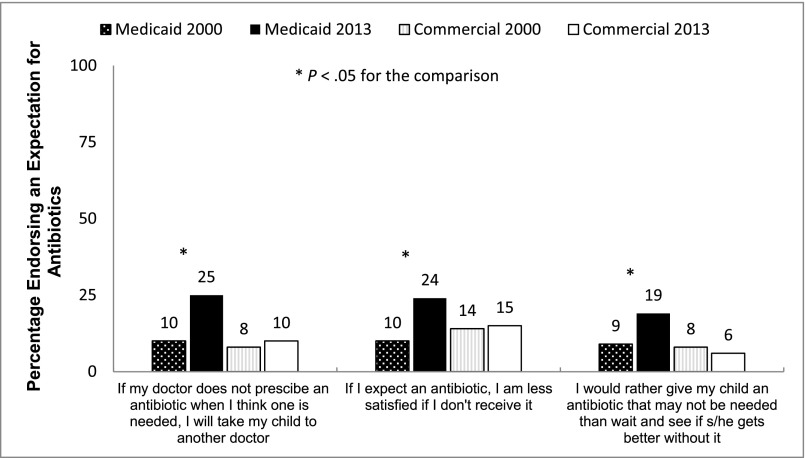
In a multivariable model examining associations with affirmatively answering questions suggesting a proclivity to request antibiotics (Table 4), insurance status was an inconsistent predictor. Parents of Medicaid-insured children were more likely to endorse that they would rather give their child an antibiotic than wait and see (OR 3.73; 95% CI, 1.89–7.36), even after adjustment. No demographic predictors consistently predicted responses to all 3 questions.
TABLE 4.
Multivariable Model for Predictors of a Tendency to Expect Antibiotics, 2013
| Effect | Reference Group | Tendency to Expect Antibiotics | ||
|---|---|---|---|---|
| If I Expect an Antibiotic, I Am Less Satisfied if I Don’t Receive One, OR (CI) | I Would Rather Give My Child Antibiotic Than Wait and See if He or She Needed It, OR (CI) | I Will Take My Child to Another Doctor if I Expect an Antibiotic and Don’t Receive One, OR (CI) | ||
| Insurance (Medicaid) | Commercial | 1.47 (0.85–2.55) | 3.73 (1.89–7.36) | 1.75 (0.96–3.21) |
| Education | ||||
| Less than HS | College | 1.08 (0.63–1.83) | 1.38 (0.72–2.67) | 2.15 (1.15–4.00)a |
| Completed HS | College | 0.64 (0.23–1.77) | 2.51 (0.96–6.60) | 1.79 (0.64–5.04) |
| Age >30 y | Age ≤30 y | 0.86 (0.55–1.36) | 1.83 (1.10–3.06)a | 0.86 (0.53–1.38) |
| Race or ethnicity | ||||
| Hispanic or Latino | White | 1.65 (0.97–2.81) | 1.16 (0.61–2.21) | 1.34 (0.74–2.40) |
| African American | White | 1.12 (0.56–2.22) | 1.06 (0.50–2.25) | 1.15 (0.56–2.36) |
| Other | White | 1.32 (0.71–2.45) | 0.94 (0.43–2.03) | 1.01 (0.50–2.02) |
| Child age ≥2 y | Age <2 y | 1.20 (0.74–1.93) | 1.05 (0.59–1.84) | 0.69 (0.42–1.15) |
| Child in child care | Yes | 0.83 (0.54–1.28) | 0.96 (0.58–1.59) | 1.00 (0.62–1.60) |
Statistically significant.
Change in Knowledge and Attitudes From 2000 to 2013
Response rates in 2000 were 32% for Medicaid-insured and 54% for commercially insured parents,20 compared with 39% for Medicaid-insured and 61% for commercially insured parents in the same communities in 2013. The sample from 2013 included a higher proportion of respondents of racial and ethnic minorities. Fewer respondents completed college and fewer children were in child care in the Medicaid-insured group in 2013 compared with 2000 (Table 1).
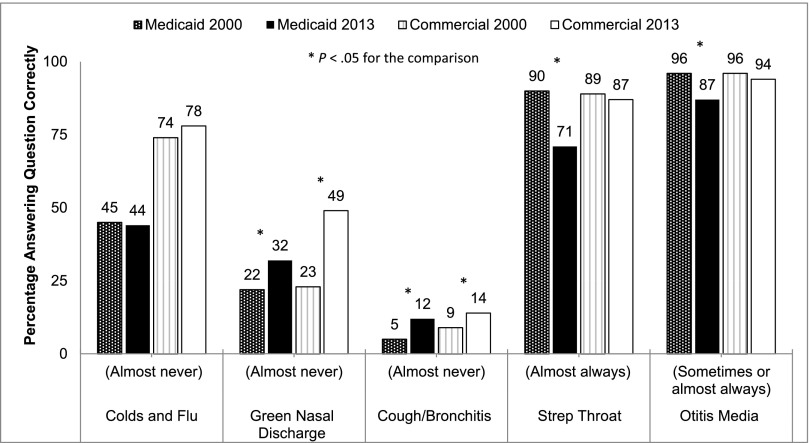
Among commercially insured parents, knowledge remained high (Fig 2, Appendix). Knowledge that green nasal discharge did not require antibiotics improved from 23% in 2000 to 49% among commercially insured respondents (P < .01). This increase was not as great among Medicaid-insured parents (22% in 2000 vs 32% in 2013, P = .02). Among Medicaid-insured parents, the percentage correctly answering the otitis media and strep throat questions actually decreased in 2013. We found very low levels of understanding that antibiotics are rarely needed for bronchitis, with marginal improvements over time in both groups (commercial insurance, 9% in 2000 and 14% in 2013; Medicaid, 5% in 2000 and 12% in 2013; both Ps < .05). Knowing that antibiotics are not needed for colds and flu did not significantly change among parents with either insurance type over time.
FIGURE 2.
Percentage correctly answering knowledge questions in 2000 versus 2013 among Medicaid-insured and commercially insured parents (weighted responses in select Massachusetts communities).
In multivariable modeling, the odds of a correct answer about green nasal discharge increased 4.8-fold between 2000 and 2013 among commercially insured respondents but only 2.1-fold in Medicaid-insured respondents (P < .01 for the difference in change between insurance types). We found no differential change in knowledge by insurance type for the 2 other questions of interest (antibiotics for bronchitis or for colds and flu). We did note differential changes in knowledge over time by other sociodemographic variables for particular questions. For example, the odds of a correct answer for colds and flu increased by 3.0-fold in 2013 versus 2000 among parents whose children were in child care but only 1.4-fold among those who were not in child care.
Among commercially insured, no significant differences over time were noted in the proportion of parents expressing a tendency to request antibiotics. However, Medicaid-insured parents in 2013 were more likely to answer ≥1 of these questions affirmatively compared with Medicaid-insured respondents in 2000 (46% in 2013 vs 25% in 2000, P < .01; Fig 3). This effect remained after we adjusted for other predictors and their interactions over time for 2 expectation questions: satisfaction with a visit if the child did not receive an antibiotic and a preference for an antibiotic rather than watchful waiting. For example, among Medicaid-insured parents, the odds of answering that they would give an antibiotic instead of watching and waiting increased 1.4-fold. In contrast, the commercially insured parents were less likely to answer this question affirmatively in 2013, with an OR of 0.17.
FIGURE 3.
Percentage endorsing statements suggesting an expectation for antibiotics in 2000 versus 2013 among Medicaid-insured and commercially insured parents (weighted responses in select Massachusetts communities).
Discussion
Despite substantial overall decreases in antibiotic use among children over the past decade, knowledge gaps are widespread and more common among parents of publicly insured children. Among both insurance groups, parents had high rates of acceptable answers regarding illnesses in which antibiotics are indicated (streptococcal pharyngitis, otitis media); however, they were not as good at identifying illnesses or symptoms for which antibiotics are not needed, such as green nasal discharge, for which nearly half of all parents believed antibiotics were indicated. There is still a common perception of a need for antibiotics for “bronchitis” that is also prevalent in adults, in whom the diagnosis accounts for a substantial fraction of antibiotic use.37,38
Collaboration with a Medicaid managed care plan and a commercial insurance plan provided us a diverse sample of respondents. Although insurance status is an imperfect proxy for other sociodemographic variables, insurers may have particular incentives to support educational and other initiatives in this area. We found that among those served by Medicaid, the improvements in knowledge have been more modest over time compared with their commercially insured counterparts. The decreases in the proportion of Medicaid-insured respondents answering the otitis media and strep throat questions correctly could result from differences in other unmeasured confounders in our 2 samples. It is also possible that interventions of the last decade that sought to decrease unnecessary antibiotic use were misunderstood by the general public regarding what illnesses would, or would not, benefit from antibiotic treatment. Younger parental age, minority race or ethnicity, and having less than a college degree were important predictors of less knowledge regarding antibiotic use in common childhood illnesses, irrespective of insurance type, consistent with other studies.19,20,39,40 Others have reported on the challenges that remain in appropriately tailoring education interventions for people who may have lower health literacy.41,42
Medicaid-insured respondents were more likely to express strong expectations for antibiotics than those commercially insured, and the proportion expressing such expectations increased among Medicaid-insured parents in our 2013 sample. Socioeconomic drivers, such as child care, employment, or transportation needs, may be behind the increased expectation and deserve additional study. The perception of parental expectations of receiving antibiotics affects the decision to prescribe.12,26,27 Whether the responses to these items reflect lower parent–provider trust would be important to determine in order to find ways to meet patients’ needs while still decreasing unnecessary antibiotic use.43
The survey included assessment of sources parents rely on for their medical information. Across insurance type, parents place high trust in their health care providers. Previous successful interventions, most in primary care settings, have invariably attempted to improve communication within visits to address parental concerns and expectations.14,19,28,30,44–52 Medicaid-insured respondents were less trusting of more formal avenues of information, including physicians, the Centers for Disease Control and Prevention, and the department of public health compared with their commercially insured counterparts. Limiting educational interventions to these sources may miss opportunities to reach audiences that rely on other sources. For example, parents in this sample also reported high levels of trust in information obtained through pharmacies, suggesting they may also be potential sites for interventions, particularly as more care is provided in retail-based clinics.53,54
The respondents surveyed do not make up a nationally representative sample. Although our response rates were similar to those seen in other studies, including among Medicaid-insured participants, the results may not be representative of nonrespondents.19,20,55,56 Because this survey was conducted in written English within a multilingual population, biases in who responded to our survey may have resulted. The modeling of race or ethnicity included a forced category of “Latino/Hispanic” for race to compare across study years. Although some terms such as virus, bacteria, or even antibiotic may not have been understandable to respondents, it is the health literacy related to these terms that was of interest, so that we can better understand how they should be used in future educational campaigns.
Conclusions
Despite large-scale educational campaigns to decrease antibiotic misuse, deficits in parental knowledge persist. In our sample, the majority of commercially insured parents were better informed about appropriate use of antibiotics, and misconceptions (and misguided expectations) for antibiotics may even be growing among those publicly insured. From the perspective of patients, the concepts involved are quite complex. They include differences between viruses and bacteria and the fact that the former are never treated (with the exception of influenza), whereas the latter may be (but are not always). Developing additional population-level interventions will require a deep understanding of disparities in access to specific streams of information and tailoring messages for families with varying health literacy levels. New strategies to change expectations about antibiotic use must be a continued focus of public health initiatives. These initiatives will be more effective if they address local knowledge and attitudes and tailor interventions to combat specific misconceptions.
Acknowledgments
The authors thank Ms Laurel Curran for helping in the survey of Neighborhood Health Plan participants.
Glossary
- CI
confidence interval
- OR
odds ratio
APPENDIX.
Responses to Knowledge and Demand Questions Among Parents in 2000 Versus 2013 for Medicaid and Commercial Insurance, Weighted
| Medicaid Insurance | Commercial Insurance | ||||||
|---|---|---|---|---|---|---|---|
| 2000, N (%) | 2013, N (%) | P | 2000, N (%) | 2013, N (%) | P | ||
| Total knowledge | |||||||
| 1. How often are antibiotics needed for sore throat? | Sometimes or almost never | 211 (83) | 126 (80) | NS | 680 (90) | 173 (94) | NS |
| 2. How often are antibiotics needed for colds or flu? | Almost never | 109 (45) | 69 (44) | NS | 560 (74) | 142 (78) | NS |
| 3. How often are antibiotics needed for ear infection? | Almost always or sometimes | 244 (96) | 139 (87) | <.01 | 740 (96) | 176 (94) | NS |
| 4. How often are antibiotics needed for runny nose or green nasal discharge? | Almost never | 56 (22) | 50 (32) | .02 | 176 (23) | 91 (49) | <.01 |
| 5. How often are antibiotics needed for deep cough or bronchitis? | Almost never | 13 (5) | 19 (12) | <.01 | 66 (9) | 26 (14) | .02 |
| 6. How often are antibiotics needed for middle ear fluid? | Sometimes or almost never | 74 (29) | 66 (43) | <.01 | 337 (44) | 104 (56) | <.01 |
| 7. How often are antibiotics needed for strep throat? | Almost always | 232 (90) | 110 (71) | <.01 | 684 (89) | 162 (87) | NS |
| 8. Are most colds caused by bacteria or viruses? | Virus | 165 (61) | 98 (61) | NS | 610 (81) | 163 (86) | NS |
| 9. Are antibiotics helpful in treating bacteria, viruses, or both? | Bacterial | 137 (51) | 60 (38) | <.01 | 552 (73) | 137 (72) | NS |
| 10. If my child does not receive an antibiotic for cold, will he or she be sick for a longer time? | Disagree or strongly disagree | 131 (48) | 82 (51) | NS | 527 (69) | 138 (73) | NS |
| High antibiotic expectation | |||||||
| 1. I will take my child to another doctor. | Strongly agree or agree | 28 (10) | 40 (25) | <.01 | 59 (8) | 19 (10) | NS |
| 2. If I expect an antibiotic, I am less satisfied if I don’t receive one. | Strongly agree or agree | 26 (10) | 39 (24) | <.01 | 109 (14) | 29 (15) | NS |
| 3. I would rather give my child an antibiotic than wait and see. | Strongly agree or agree | 25 (9) | 30 (19) | <.01 | 62 (8) | 11 (6) | NS |
Footnotes
Dr Vaz conceptualized and designed the study, carried out the analyses and interpreted the data, and drafted the manuscript; Dr Kleinman conceptualized the study, supervised the analyses, and reviewed and revised the manuscript; Mr Lakoma carried out the analyses, interpreted the data, and revised the manuscript; Ms Dutta-Linn helped administer the survey, interpreted the data, and revised the manuscript; Ms Nahill assisted with survey administration and data collection and revised the manuscript; Dr Hellinger assisted in interpretation of the results and edited the manuscript for critical content; Dr Finkelstein conceptualized and designed the study, supervised all analyses, assisted in interpretation of the results, and edited the manuscript for critical content; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: Ms Nahill has stock ownership in Johnson & Johnson, Merck Co, Lily Eli & Company, and Pfizer Incorporated. The other authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by National Institutes of Health (NIH) grant 1K24HD060786 (principal investigator J.A.F.). Dr Vaz was supported under National Research Service Award training grants T32HD066148 and T32HD075727. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: Ms Nahill has stock ownership in Johnson & Johnson, Merck Co, Lily Eli & Company, and Pfizer Incorporated. The other authors have indicated they have no potential conflicts of interest to disclose.
COMPANION PAPER: A companion to this article can be found on page 387, and online at www.pediatrics.org/cgi/doi/10.1542/peds.2015-1780.
References
- 1.Costelloe C, Metcalfe C, Lovering A, Mant D, Hay AD. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ. 2010;340(18):c2096. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. A public health action plan to combat antimicrobial resistance. 2012. Available at: www.cdc.gov/drugresistance/actionplan/actionplan.html. Accessed May 17, 2014
- 3.Hersh AL, Jackson MA, Hicks LA, American Academy of Pediatrics Committee on Infectious Diseases . Principles of judicious antibiotic prescribing for upper respiratory tract infections in pediatrics. Pediatrics. 2013;132(6):1146–1154 [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. New guidance limits antibiotic for common infections in children. 2013. Available at: www.cdc.gov/media/releases/2013/p1118-get-smart.html. Accessed May 19, 2014
- 5.Taylor S, Marchisio P, Vergison A, Harriague J, Hausdorff WP, Haggard M. Impact of pneumococcal conjugate vaccination on otitis media: a systematic review. Clin Infect Dis. 2012;54(12):1765–1773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vaz LE, Kleinman KP, Raebel MA, et al. Recent trends in outpatient antibiotic use in children. Pediatrics. 2014;133(3):375–385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Greene SK, Kleinman KP, Lakoma MD, et al. Trends in antibiotic use in Massachusetts children, 2000–2009. Pediatrics. 2012;130(1):15–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hersh AL, Shapiro DJ, Pavia AT, Shah SS. Antibiotic prescribing in ambulatory pediatrics in the United States. Pediatrics. 2011;128(6):1053–1061 [DOI] [PubMed] [Google Scholar]
- 9.Weissman J, Besser RE. Promoting appropriate antibiotic use for pediatric patients: a social ecological framework. Semin Pediatr Infect Dis. 2004;15(1):41–51 [DOI] [PubMed] [Google Scholar]
- 10.Finkelstein JA, Stille CJ, Rifas-Shiman SL, Goldmann D. Watchful waiting for acute otitis media: are parents and physicians ready? Pediatrics. 2005;115(6):1466–1473 [DOI] [PubMed] [Google Scholar]
- 11.Bagshaw SM, Kellner JD. Beliefs and behaviours of parents regarding antibiotic use by children. Can J Infect Dis Med Microbiol. 2001;12(2):93–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mangione-Smith R, Elliott MN, Stivers T, McDonald L, Heritage J, McGlynn EA. Racial/ethnic variation in parent expectations for antibiotics: implications for public health campaigns. Pediatrics. 2004;113(5). Available at: www.pediatrics.org/cgi/content/full/113/5/e385 [DOI] [PubMed] [Google Scholar]
- 13.Shlomo V, Adi R, Eliezer K. The knowledge and expectations of parents about the role of antibiotic treatment in upper respiratory tract infection: a survey among parents attending the primary physician with their sick child. BMC Fam Pract. 2003;4(20):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hemo B, Shamir-Shtein NH, Silverman BG, et al. Can a nationwide media campaign affect antibiotic use? Am J Manag Care. 2009;15(8):529–534 [PubMed] [Google Scholar]
- 15.Palmer DA, Bauchner H. Parents’ and physicians’ views on antibiotics. Pediatrics. 1997;99(6). Available at: www.pediatrics.org/cgi/content/full/99/6/e6 [DOI] [PubMed] [Google Scholar]
- 16.Collett CA, Pappas DE, Evans BA, Hayden GF. Parental knowledge about common respiratory infections and antibiotic therapy in children. South Med J. 1999;92(10):971–976 [DOI] [PubMed] [Google Scholar]
- 17.Cabral C, Horwood J, Hay AD, Lucas PJ. How communication affects prescription decisions in consultations for acute illness in children: a systematic review and meta-ethnography. BMC Fam Pract. 2014;15(1):63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Trepka MJ, Belongia EA, Chyou P-H, Davis JP, Schwartz B. The effect of a community intervention trial on parental knowledge and awareness of antibiotic resistance and appropriate antibiotic use in children. Pediatrics. 2001;107(1). Available at: www.pediatrics.org/cgi/content/full/107/1/e6 [DOI] [PubMed] [Google Scholar]
- 19.Huang SS, Rifas-Shiman SL, Kleinman K, et al. Parental knowledge about antibiotic use: results of a cluster-randomized, multicommunity intervention. Pediatrics. 2007;119(4):698–706 [DOI] [PubMed] [Google Scholar]
- 20.Kuzujanakis M, Kleinman K, Rifas-Shiman S, Finkelstein JA. Correlates of parental antibiotic knowledge, demand, and reported use. Ambul Pediatr. 2003;3(4):203–210 [DOI] [PubMed] [Google Scholar]
- 21.Mainous AG, III, Hueston WJ, Eberlein C. Colour of respiratory discharge and antibiotic use. Lancet. 1997;350(9084):1077. [DOI] [PubMed] [Google Scholar]
- 22.Chan GC, Tang SF. Parental knowledge, attitudes and antibiotic use for acute upper respiratory tract infection in children attending a primary healthcare clinic in Malaysia. Singapore Med J. 2006;47(4):266–270 [PubMed] [Google Scholar]
- 23.Mangione-Smith R, McGlynn EA, Elliott MN, McDonald L, Franz CE, Kravitz RL. Parent expectations for antibiotics, physician–parent communication, and satisfaction. Arch Pediatr Adolesc Med. 2001;155(7):800–806 [DOI] [PubMed] [Google Scholar]
- 24.Wilson AA, Crane LA, Barrett PH, Gonzales R. Public beliefs and use of antibiotics for acute respiratory illness. J Gen Intern Med. 1999;14(11):658–662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Watson RL, Dowell SF, Jayaraman M, Keyserling H, Kolczak M, Schwartz B. Antimicrobial use for pediatric upper respiratory infections: reported practice, actual practice, and parent beliefs. Pediatrics. 1999;104(6):1251–1257 [DOI] [PubMed] [Google Scholar]
- 26.Mangione-Smith R, McGlynn EA, Elliott MN, Krogstad P, Brook RH. The relationship between perceived parental expectations and pediatrician antimicrobial prescribing behavior. Pediatrics. 1999;103(4 pt 1):711–718 [DOI] [PubMed] [Google Scholar]
- 27.Stivers T, Mangione-Smith R, Elliott MN, McDonald L, Heritage J. Why do physicians think parents expect antibiotics? What parents report vs what physicians believe. J Fam Pract. 2003;52(2):140–148 [PubMed] [Google Scholar]
- 28.Finkelstein JA, Davis RL, Dowell SF, et al. Reducing antibiotic use in children: a randomized trial in 12 practices. Pediatrics. 2001;108(1):1–7 [DOI] [PubMed] [Google Scholar]
- 29.Hanage WP, Bishop CJ, Lee GM, et al. Clonal replacement among 19A Streptococcus pneumoniae in Massachusetts, prior to 13 valent conjugate vaccination. Vaccine. 2011;29(48):8877–8881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Finkelstein JA, Huang SS, Kleinman K, et al. Impact of a 16-community trial to promote judicious antibiotic use in Massachusetts. Pediatrics. 2008;121(1). Available at: www.pediatrics.org/cgi/content/full/121/1/e15 [DOI] [PubMed] [Google Scholar]
- 31.Huang SS, Finkelstein JA, Rifas-Shiman SL, Kleinman K, Platt R. Community-level predictors of pneumococcal carriage and resistance in young children. Am J Epidemiol. 2004;159(7):645–654 [DOI] [PubMed] [Google Scholar]
- 32.Lieberthal AS, Carroll AE, Chonmaitree T, et al. The diagnosis and management of acute otitis media [published correction appears in Pediatrics. 2014;133(2):346]. Pediatrics. 2013;131(3). Available at: www.pediatrics.org/cgi/content/full/131/3/e964 [DOI] [PubMed] [Google Scholar]
- 33.Chow AW, Benninger MS, Brook I, et al. Infectious Diseases Society of America . IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012;54(8):e72–e112 [DOI] [PubMed] [Google Scholar]
- 34.Shulman ST, Bisno AL, Clegg HW, et al. Infectious Diseases Society of America . Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America [published correction appears in Clin Infect Dis. 2014;58(10):1496]. Clin Infect Dis. 2012;55(10):e86–e102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stockmeyer NO. Using Microsoft Word’s readability program. Michigan Bar J. 2009;88(1):46–47. Available at: www.michbar.org/journal/pdf/pdf4article1467.pdf. Accessed December 2, 2014
- 36.SAS Institute. SAS (version) 9.4 statistical software. Cary, NC: SAS Institute, Inc; 2014 [Google Scholar]
- 37.Gonzales R, Malone DC, Maselli JH, Sande MA. Excessive antibiotic use for acute respiratory infections in the United States. Clin Infect Dis. 2001;33(6):757–762 [DOI] [PubMed] [Google Scholar]
- 38.Barnett ML, Linder JA. Antibiotic prescribing for adults with acute bronchitis in the United States, 1996–2010. JAMA. 2014;311(19):2020–2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Céspedes A, Larson E. Knowledge, attitudes, and practices regarding antibiotic use among Latinos in the United States: review and recommendations. Am J Infect Control. 2006;34(8):495–502 [DOI] [PubMed] [Google Scholar]
- 40.Lee GM, Friedman JF, Ross-Degnan D, Hibberd PL, Goldmann DA. Misconceptions about colds and predictors of health service utilization. Pediatrics. 2003;111(2):231–236 [DOI] [PubMed] [Google Scholar]
- 41.Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. 2006;15(3):259–268 [Google Scholar]
- 42.Barry MM, D’Eath M, Sixsmith J. Interventions for improving population health literacy: insights from a rapid review of the evidence. J Health Commun. 2013;18(12):1507–1522 [DOI] [PubMed] [Google Scholar]
- 43.Coenen S, Francis N, Kelly M, et al. GRACE Project Group . Are patient views about antibiotics related to clinician perceptions, management and outcome? A multi-country study in outpatients with acute cough. PLoS ONE. 2013;8(10):e76691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Francis NA, Butler CC, Hood K, Simpson S, Wood F, Nuttall J. Effect of using an interactive booklet about childhood respiratory tract infections in primary care consultations on reconsulting and antibiotic prescribing: a cluster randomised controlled trial. BMJ. 2009;339:b2885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Macfarlane JT, Holmes WF, Macfarlane RM. Reducing reconsultations for acute lower respiratory tract illness with an information leaflet: a randomized controlled study of patients in primary care. Br J Gen Pract. 1997;47(424):719–722 [PMC free article] [PubMed] [Google Scholar]
- 46.Taylor JA, Kwan-Gett TSC, McMahon EM, Jr. Effectiveness of an educational intervention in modifying parental attitudes about antibiotic usage in children. Pediatrics. 2003;111(5 pt 1). Available at: www.pediatrics.org/cgi/content/full/111/5/e548 [DOI] [PubMed] [Google Scholar]
- 47.Vodicka TA, Thompson M, Lucas P, et al. TARGET Programme team . Reducing antibiotic prescribing for children with respiratory tract infections in primary care: a systematic review. Br J Gen Pract. 2013;63(612):e445–e454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ranji SR, Steinman MA, Shojania KG, Gonzales R. Interventions to reduce unnecessary antibiotic prescribing: a systematic review and quantitative analysis. Med Care. 2008;46(8):847–862 [DOI] [PubMed] [Google Scholar]
- 49.Finch RG, Metlay JP, Davey PG, Baker LJ, International Forum on Antibiotic Resistance Colloquium . Educational interventions to improve antibiotic use in the community: report from the International Forum on Antibiotic Resistance (IFAR) Colloquium, 2002. Lancet Infect Dis. 2004;4(1):44–53 [DOI] [PubMed] [Google Scholar]
- 50.Andrews T, Thompson M, Buckley DI, et al. Interventions to influence consulting and antibiotic use for acute respiratory tract infections in children: a systematic review and meta-analysis. PLoS ONE. 2012;7(1):e30334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gonzales R, Steiner JF, Lum A, Barrett PH, Jr. Decreasing antibiotic use in ambulatory practice: impact of a multidimensional intervention on the treatment of uncomplicated acute bronchitis in adults. JAMA. 1999;281(16):1512–1519 [DOI] [PubMed] [Google Scholar]
- 52.Committee on Hospital Care and Institute for Patient- and Family-Centered Care . Patient- and family-centered care and the pediatrician’s role. Pediatrics. 2012;129(2):394–404 [DOI] [PubMed] [Google Scholar]
- 53.Northey A, McGuren T, Stupans I. Patients’ antibiotic knowledge: a trial assessing the impact of verbal education. Int J Pharm Pract. 2015;23(2):158–160 [DOI] [PubMed] [Google Scholar]
- 54.Cassel CK. Retail clinics and drugstore medicine. JAMA. 2012;307(20):2151–2152 [DOI] [PubMed] [Google Scholar]
- 55.Fredrickson DD, Jones TL, Molgaard CA, et al. Optimal design features for surveying low-income populations. J Health Care Poor Underserved. 2005;16(4):677–690 [DOI] [PubMed] [Google Scholar]
- 56.Beebe TJ, Davern ME. Increasing response rates in a survey of Medicaid enrollees. Med Care. 2005;43(4):411–420 [DOI] [PubMed] [Google Scholar]