Abstract
Over the past several years, more so recently, treatment options for hepatitis C virus (HCV) have seemed to exponentially grow. Up until recently, the regimen of pegylated interferon (peg-IFN) and ribavirin (RBV) stood as the standard of care. Direct acting antivirals, which target nonstructural proteins involved in replication and infection of HCV were first approved in 2011 as an addition to the peg-IFN and RBV regimen and with them have come increased sustained virological response rates (SVR). The previously reported 50%-70% SVR rates using the combination of peg-IFN and RBV are no longer the standard of care with direct acting antiviral (DAA) based regimens now achieving SVR of 70%-90%. Peg-IFN free as well as “all oral” regimens are also available. The current randomized controlled trials available show favorable SVRs in patients who are naive to treatment, non-cirrhotic, and not human immunodeficiency virus (HIV)-co-infected. What about patients who do not fit into these categories? In this review, we aim to discuss the currently approved and soon to be approved DAAs while focusing on their roles in patients that are treatment experienced, cirrhotic, or co-infected with HIV. In this discussion, review of the clinical trials leading to recent consensus guidelines as well as discussion of barriers to treatment will occur. A case will attempt will be made that social services, including financial support and drug/alcohol treatment, should be provided to all HCV infected patients to improve chances of cure and thus prevention of late stage sequela.
Keywords: Hepatitis C virus, Direct acting antiviral, Human immunodeficiency virus, Cirrhosis, Treatment experienced
Core tip: The current randomized controlled trials available show favorable sustained virologic responses in patients who are naive to treatment, non-cirrhotic, and not human immunodeficiency virus (HIV)-co-infected. What about patients who do not fit into these categories? In this review, we aim to discuss the currently approved and soon to be approved direct acting antivirals while focusing on their roles in patients that are treatment experienced, cirrhotic, or co-infected with HIV.
INTRODUCTION
In the most recent national health and nutrition examination survey the estimated prevalence of hepatitis C virus (HCV) infection was approximately 3.9 million in the United States alone, with an estimated 2.7 million with chronic infection[1]. Worldwide, the number living with chronic hepatitis C approaches 150 million[2]. These estimates likely fall significantly short given that nearly half of all infected patients have never been tested for HCV. This survey also excluded prisoners and the homeless; two well-known high-risk populations. Over the past several years, more so recently, treatment options for HCV have seemed to exponentially grow. Treatment for HCV began with Food and Drug Administration approval of interferon (IFN) in 1991, followed by combined IFN and ribavirin (RBV) in 1998, and later with pegylated IFN (peg-IFN) in 2001. Up until recently, the regimen of peg-IFN and RBV stood as the standard of care. Direct acting antivirals (DAAs), which target nonstructural proteins involved in replication and infection of HCV were first approved in 2011 as an addition to the peg-IFN and RBV regimen (Table 1).
Table 1.
Chronologically listed, Food and Drug Administration approved treatment regimens for hepatitis C virus
| HCV (identified in 1989) |
| Approved drugs 1991-2001 |
| Interferon (approved in 1991) |
| RBV + standard interferon (1998) |
| Peg-IFNs (approved in 2001) |
| Peg-IFN |
| Peg-IFN + RBV |
| DAAs 2011-present |
| Telaprevir and boceprevir |
| Increase SVR rates and provide the option of response-guided therapy and retreatment for genotype 1 patients |
| Telaprevir + peg-IFN + RBV, genotype 1 only (2011) |
| Boceprevir + peg-IFN + RBV, genotype 1 only (2011) |
| Sofosbuvir |
| Approved for use in all genotypes. High SVR rates with better tolerability, shorter duration, use in HIV-HCV co-infection, and first interferon-free all-oral regimen in genotype 2, 3 and certain other patients |
| Sofosbuvir + peg-IFN + RBV, in genotype 1 only (2013) |
| Sofosbuvir + RBV, without interferon, in genotype 2 and 3, in HIV-HCV co-infection, with any genotype, and in selected situations of genotype 1 (2013) |
| Simeprevir |
| High SVR rates with better tolerability and shorter duration for genotype 1 |
| Simeprevir + peg-IFN + RBV, in genotype 1 only (2013) |
Adapted from http://www.hepatitis.va.gov. DAAs: Direct acting antivirals; SVR: Sustained virological response; HIV: Human immunodeficiency virus; HCV: Hepatitis C virus; RBV: Ribavirin; Peg-IFN: Pegylated interferon.
Sustained virologic response (SVR), which is commonly defined as a lack of HCV detection 12-24 wk following treatment, with RBV and peg-IFN alone was marginal but has continued to improve. By understanding the genome of the HCV, scientists and researchers have been able to exploit its mechanism of transmission by creating inhibitors against several of the nonstructural proteins that are integral to HCV replication and function. As it currently stands, four classes of DAA exist which can be categorized according to the protein they inhibit. They include the NS3/4 protease, NS5A polymerase, and NS5B polymerases (nucleoside and non-nucleoside). The approval of telaprevir (TVR) and boceprevir (BOC) in 2011 marked the start of this new era. The approval of these NS3/4 protease inhibitors occurred following studies showing increased SVR, in comparison to IFN and RBV alone. Two years later this was followed by approval of sofosbuvir (SOF), a nucleoside NS5B inhibitor, and simeprevir (SIM), an NS3/4 protease inhibitor (Table 2). Several other agents are currently undergoing late stage clinical trials and expected to be approved in the near future (Table 3).
Table 2.
Currently available Food and Drug Administration approved pharmaceuticals for treatment of hepatitis C virus
| Approved treatments for hepatitis C | ||
|
Brand name |
Generic names |
Manufacturer name |
| Sovaldi | SOF | Gilead Sciences |
| Olysio | SIM | Janssen |
| Incivek | TVR | Vertex |
| Victrelis | BOC | Merck and Co. |
| Pegasys | Peg-IFN | Roche |
| CoPegus | RBV | Roche |
| Pegintron | Peg-IFN alpha-2b | Schering |
| Intron A | IFN alpha-2b | Schering |
| Rebetol | RBV | Schering |
| Roferon | IFN alpha-2a | Roche |
| Infergen | IFN aphacon-1 | Three Rivers Pharma |
Adapted from http://www.fda.gov/. SOF: Sofosbuvir; SIM: Simeprevir; TVR: Telaprevir; BOC: Boceprevir; RBV: Ribavirin; Peg-IFN: Pegylated interferon.
Table 3.
Food and Drug Administration approved and investigational drugs by mechanism of action
| HCV NS3/4 protease inhibitors | Nucleos(t)ide HCV NS5B polymerase inhibitors | Non-nucleos(t)ide HCV NS5B polymerase inhibitors | HCV NS5A inhibitors |
| Telaprevir1 | Sofosbuvir1 | BI-207127 | Daclatasvir |
| Boceprevir1 | Mericitabine | VX-222 | Ledipasvir |
| Danoprevir | ABT-333 | ABT-267 | |
| Simeprevir1 | BMS-791325 | ||
| ABT-450 (with ritonavir) | Tegobuvir | ||
| Faldaprevir | GS-9669 | ||
| Asunaprevir | |||
| GS-9451 |
Drugs have received Food and Drug Administration approval. Adapted from http://www.hepatitis.va.gov. HCV: Hepatitis C virus.
The previously reported 50%-70% SVR rates using the combination of peg-IFN and RBV are no longer the standard of care (Figure 1). New guidelines clearly echo this[3]. IFN free as well as “all oral” regimens are already in place for genotype 2 and probably for genotypes 1 and 4 by the end of the year. RBV free regimens are also being explored[4]. The current randomized controlled trials available convincingly show favorable SVR in patients who are naïve to treatment, non-cirrhotic, and in non-human immunodeficiency virus (HIV)-co-infected, but what about patients who do not fit into these categories? Furthermore, concern for side-effect profile, unfamiliar practitioners and concern for drug-drug interaction has led to avoidance in all but treatment-naive and otherwise healthy patients.
Figure 1.
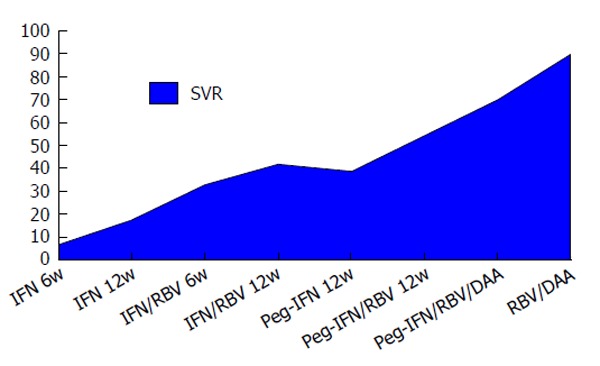
Sustained virologic response of various treatment regimens. DAAs: Direct acting antivirals; RBV: Ribavirin; Peg-IFN: Pegylated interferon.
In this review, we aim to discuss the currently approved and soon to be approved DAAs while focusing on their roles in patients that are treatment experienced, cirrhotic, or co-infected with HIV. In this discussion, particular attention will be paid to the continued barriers of treatment including ongoing psychological conditions such as addiction or depression, lack of access to care, poor social support, lack of financial resources, and many others. A case will attempt to be made that social services such as financial support and drug or alcohol treatment should be provided to all HCV infected patients in hopes that cure of hepatitis C will become a preventative measure for future development of HCV associated conditions; the most well-known being cirrhosis and hepatocellular carcinoma.
TREATMENT-EXPERIENCED PATIENTS
Treatment-experienced patients is perhaps the largest percentage of the patients to be discussed in this review. Patients who have been previously treated pose perhaps one of the most common dilemmas that practitioners face. This group can be divided into patients who have relapsed, those who partially responded to therapy, and to those who did not respond to treatment or null responders. Other variables to be considered are those that underwent incomplete treatment secondary to drop out and noncompliance.
TVR and BOC
REALIZE: Previous peg-IFN + RBV treated and peg-IFN + RBV failures: Non-responders, partial responders or those who have suffered a relapse were randomized into three treatment groups separated by treatment duration. An SVR rate of 66% was achieve in the 12-wk treatment arm utilizing TVR, peg-IFN, and RBV. Additionally, this study was also able to show a decreased relapse rate of 1% compared to 26% in the control group[5]. In a study published by the Journal of Hepatology treatment of prior non-responders, partial responders, and those with relapse using BOC in combination peg-IFN and RBV was able to achieve rates of SVR of 63% percent of all treated followed by 38%, 67%, 93% respectively for each subgroup. The most commonly reported adverse events related to combination therapy utilizing BOC included anemia, fatigue, and dysgeusia[6].
RESPOND-2: Previous peg-IFN + RBV failure: In the RESPOND-2 trial conducted by Bacon et al[7] over 400 patients were randomized to receive treatment with BOC along with peg-IFN and RBV following previously failed treatment to peg-IFN and RBV alone. In this trial an SVR of 59%-66% in the BOC group, was achieved as compared with the control group SVR of 21%.
CUPIC: Previous peg-IFN + RBV failure: In this trial Hézode et al[8] looked at genotype-1, previously treated with peg-interferon and RBV patients with a baseline MELD < 13 and Child-Pugh A compensated cirrhosis and examined SVR rates using TVR or BOC in combination with interferon and RBV. Compared with the REALIZE and RESPOND-2 trial, similar rates of SVR at 12 wk was achieved. In the TVR treatment arm an SVR of 75%, 40% and 20% were achieved in previously relapsed patients, partial responders, and null-responders, respectively. The BOC treatment group received slightly less encouraging results with rates of 54%, 38%, 0%, comparatively. Significant side effects occurred in almost half of all those treated in the study. Fifty patients (10%) experienced severe complications or death, with nearly half of these occurring during the first 12 wk of treatment. As has been previously noted in prior studies, severe anemia, requiring either discontinuation or reduction in dosing, as well as transfusion occurred in 134 and 78 of the 511 studied patients, respectively. Multivariate analysis suggested higher risk of side effects in patients with severe hypoalbuminemia and thrombocytopenia. Given the poor response of prior null responders, treatment utilizing BOC or TVR in combination with peg-IFN and RBV is not recommended. Due to adverse events, the authors also recommend considering not treating patients with platelet counts < 100000/mm3 and serum albumin < 3.5 g/dL.
Simeprevir
In a phase II clinic trial by Zeuzem et al[9], previously treated, genotype-1 infected patients underwent randomization to receive simeprevir in combination with peg-IFN and RBV for either 12, 24, or 48 wk or peg-IFN and RBV alone for 48 wk. The rate of overall SVR was significantly higher in the simeprevir group with 61%-80% vs 23% in the peg-IFN + RBV (PR) group. When examining prior null responders, an SVR rate of 38%-59% vs 19% was noted. Partial responders and relapsers achieved even higher rates; 48%-86% and 77%-89%, respectively. All groups had comparable numbers of adverse events.
In follow-up, a phase III trial conducted by Forns et al[10] randomized genotype 1, PR failure patients into either a 12 wk course of SIM + PR (followed by either a 12 or 36 wk course of PR) or 48 wk of PR. SVR12 of 79.2% vs 36.1% was noted in the study groups, respectively. Similar adverse events were noted regardless of therapy.
SOF
FUSION: Previous PR + PR failures: Jacobson et al[11] looked at treatment with SOF and RBV in genotype 2 and 3 patients who previously failed peg-IFN based therapy. Patients were randomized to receive either 12 or 16 wk of treatment. Patients receiving 16 wk of therapy fared better than the 12 wk group and were able to achieve rates of SVR at 12 wk post therapy of 50% (50/100) and 73% (69/95), respectively. Breakdown of subgroups identified that genotype 2 patients had higher SVR rates than genotype 3. Additionally, non-cirrhotic patients had higher rates of response as compared with cirrhotic patients.
SOF/simeprevir
COSMOS: Previous PR failures: A phase II clinical trial randomized 167 treatment naive and previously treated genotype 1 patients to receive both SOF and SIM alone or in combination with RBV[12]. Additionally, these patients were selected to receive either a 12 or 24-wk course of treatment. Among prior null responders with Metavir scores of F0-2 and without the Q80K mutation an SVR12 of 100% was achieved regardless of treatment regimen or duration. In patients with either F3-4 Metavir scores SVR12 fell slightly to 92% (38/41) in the 12 wk treatment arm regardless of treatment regimen. Among all subgroups, the presence of the Q80K mutation in genotype 1a patients conferred a decreased chance of achieving SVR. The extent of treatment resistance remains an area of future study but never the less should be noted when considering simeprevir-containing regimens.
SOF/ledipasvir
ION-2: Previous PR and DAA + PR failures: A trial by Afdhal et al[13] published in New England Journal of Medicine in 2014 looked at 440 patients who had failed previous peg-IFN and RBV therapy and treated them with SOF and ledipasvir (LED), a nucleoside 5A inhibitor, either with or without RBV. Treatment course was either 12 or 24 wk. In the 12 wk group, triple therapy with RBV resulted in a 96% SVR compared with a 94% in the dual treatment group. When the duration of treatment was extended to 24 wk both treatment arms had 99% SVR.
LONESTAR: Previous DAA + DAA failure: Lawitz et al[14] gathered 40 patients previously treated with BOC or TVR who then went on to fail therapy or have recurrence and randomized them to receive SOF and LED with or without RBV for a total of 12 wk. At 12 wk following therapy 95% (18/19) achieved SVR in the dual therapy group vs 100% (21/21) in the triple therapy group. Anemia was more common with those treated with RBV, occurring in 6 of the 21 patients, but did not lead to treatment failure or discontinuation.
SOF/daclatasvir
In a study by Sulkowski et al[4], 41 of 211 patients with genotype 1 were noted to have previously been treated with protease inhibitors, either BOC or TVR, without achieving SVR. In this subgroup, randomization to daclatasvir, a nucleoside 5A inhibitor, and SOF with or without RBV for a total of 24 wk showed SVR12 of 100% (21/21) and 95% (19/20), respectively. Notable side effects included nausea, fatigue and headache and were reported in a majority of subjects. Side effects did not lead to discontinuation of treatment.
ABT-450/r/ombitasvir/dasabuvir/RBV
SAPPHIRE-II: Previous PR failures: In a phase III trial conducted by Zeuzem et al[15], 394 genotype 1 patients with prior treatment failure underwent randomization to receive 12 wk of treatment with the study drug regimen or placebo. SVR12 in the active regimen group was noted to be 96.3% (286/297). With only 1% drop out due to side effects and only 4.7% experiencing grade 2 or 3 anemia, this regimen shows some of the best results for HCV therapy to date. Additionally, SVR12 of prior null responders was 95.3% (139/146).
HIV/HCV CO-INFECTION
HIV-infected individuals with concomitant hepatitis C are known to have an increased morbidity and mortality[16]. They are also known to have relatively poor responses to peg-IFN and RBV therapy, as compared with mono-infected patients[17,18]. In a study by Benhamou et al[19] which examined HCV-related liver fibrosis progression, a CD4 count below 200/microliter, heavy alcohol consumption, and absence of protease inhibitor therapy were all identified as independent risk factors for progression to cirrhosis in HIV co-infected patients. Several mechanisms are described throughout the literature aiming to address this finding. On a molecular level, it has been noticed that when compared to the HCV mono-infected, HCV-HIV co-infected persons have higher levels of HCV RNA. The higher viral lode of HCV RNA is suspected to be secondary to an increased replication of HCV RNA by HIV proteins[20]. It is also thought that the overall state of immunodeficiency leads to an environment of rapid hepatocyte destruction and fibrosis progression[21].
Following the development of highly active antiretroviral therapy (HAART) there has been an ever-increasing percentage of HIV infected patients who are dying from liver disease. In HIV infected patients, death from liver disease remains far more prevalent than death attributable to HIV-related complications[22,23]. The increased mortality from liver-related illness appears to be uniquely associated with co-infected patients only. In a large, multi-center, prospective trial examining HAART-related liver mortality in patients not infected with HCV or HBV the rate of death was 0.04/1000 person-years. Of the 12 recorded liver related deaths, seven were deemed to be due to excessive alcohol use while the other five were deemed to be related to HAART-related toxicity[24]. There also exists a mechanism by which HCV and HIV co-infection is thought to increase the risk for both HAART-related liver toxicity and cirrhosis. This mechanism consists of direct cell stress, mitochondrial dysfunction and immune reaction[25]. Though not completely clear, liver related deaths in HIV co-infected patients has been speculated to be the result of either of two reasons; increased lifespan from appropriately treated HIV (leading to the natural progression of HCV related cirrhosis and liver dysfunction) or HAART therapy induced liver toxicity[26]. Confound this with the potential drug-drug interactions, particularly with the newest of DAAs, and it is no wonder trepidation to providing treatment exists[27,28].
Prior to the creation of DAA, RBV and peg-IFN had been used with modest results. In a study published by Torriani et al[17] in the New England Journal of Medicine, 868 co-infected patients were randomized to receive either peg-IFN and RBV or peg-interferon and placebo for a total of 48 wk. Among the genotype-1 patients who received both peg-IFN as well as RBV an SVR of 29% compared with 62% in those with genotype 2 or 3 was achieved. In particular, a subgroup utilizing a higher dosing regimen proved to be the most efficacious, albeit with a greater prevalence of RBV associated anemia. Additional studies showing similar results exist[29-31].
TVR
With the approval of DAAs, subsequent studies looking at rates of SVR in the HIV co-infected population have shown promising results. In a study by Sulkowski et al[32] published in the Annals of Internal Medicine in 2013, a relatively small, yet randomized treatment population underwent combination therapy utilizing TVR in addition to peg-IFN and RBV. In this study 62 patients co-infected with both HCV and HIV were enrolled at multiple investigational sites. Genotype-1 infected patients, without cirrhosis, who had not had any previous HCV treatment and were noted to have “stable HIV disease” where eligible. Stable disease was classified as CD4 counts greater than 0.500 × 109 cells/L and HIV RNA levels < 100000 copies/mL. Antiretroviral regimens were allowed. SVR occurred in 74% (28/30) patients receiving TVR, peg-IFN and RBV vs 45% (10/22) of patients receiving peg-IFN and RBV alone. Side effects of pruritus, headache, rash and rectal pain were noted to be higher in the treatment group. Two patients were noted to have HCV breakthrough with TVR resistant variants. With these findings TVR in combination with peg-IFN and RBV improved upon previous rates SVR without appreciable drug-drug interaction or significant side effect.
BOC
In a phase II trial by Sulkowski et al[33] 99 patients with co-infection of HIV and HCV were randomized in a 1:2 ratio to receive a 48-wk treatment course of either placebo or BOC in combination with RBV and peg-IFN. SVR in the triple therapy group was noted to be 63% compared with 29% in the control group. Adverse events were more common in the triple therapy arm leading to significant amount of dropout (12 of 65). Reported adverse events included anemia, pyrexia, dysgeusia, vomiting and neutropenia. Additionally, HIV virological breakthrough occurred in seven patients; three receiving triple therapy and four in the control group. Considerable variability among patients that had breakthrough existed. In comparison to patients with HCV alone, co-infected patients who did not achieve SVR were noted to have significantly more (80% vs 53%) had resistant variants. Given some of the findings in this study, larger trials should be done to better characterize safety and efficacy of this regimen.
SOF
PHOTON-1: Genotype 1 patients with HIV infection: Sulkowski et al[34] conducted a trial utilizing an interferon sparing, 24-wk regimen comprised of SOF and RBV in genotype-1, 2 and 3. In the genotype 1 group an SVR of 76% regardless of antiretroviral regimen and with minimal drug-drug interactions was achieved. Based on this study, extrapolations of this data in co-infected patients with genotypes 2, 4, 5, and 6 current HCV guidelines recommend treatment with SOF in combination with RBV for 12 wk. Genotype 1 and 3 patients are recommended to undergo treatment with a 12 or 24-wk course of SOF, RBV and peg-IFN, respectively. Alternatives for patients who are peg-IFN intolerant exist. These regimens typically include combination therapy with SOF, simeprevir and RBV[3].
SOF/LED
NIAID ERADICATE: Genotype 1 patients with HIV infection: In the abstract presented by Osinusi et al[35], 50 HCV and HIV co-infected patients were given a 12-wk course of SOF and LED. Grouping based on HAART naivevs on HAART showed no difference in the 100% SVR rates achieved in both groups. No adverse events or discontinuations were noted during the treatment period.
CIRRHOTIC PATIENTS
Development of cirrhosis in patients with chronic hepatitis C infection occurs by molecular mechanisms involving inappropriate collagen deposition via the hepatic stellate cell. As described by Fontana et al[36] HCV infection is thought first to lead to release of metalloproteinases, which break down the surrounding low-density matrix within the sub-endothelial space. Then, recruitment and activation of stellate and Kupffer cells go on to deposit various forms of collagen within the extracellular matrix, forming what is termed fibrosis. More specifically, fibrosis is characterized by the presence of portal-central and portal-portal bands of this deposited collagen. With this change in the typical architecture, eventual disruption of normal processes of blood flow and nutrient exchange occurs, leading to the physiological manifestations of cirrhosis. Although new imaging modalities such as computed tomography, magnetic resonance imaging, ultrasound and transient elastography remain promising noninvasive methods for diagnosing and grading cirrhosis, the ability to distinguish moderate, less advanced, disease is lacking. The gold standard for diagnosis and monitoring both the extent of fibrosis and portal hypertension remains liver biopsy and measurement of the hepatic venous portal gradient, respectively[37]. Of all patients with HCV, 80% are estimated to go on to developed chronic infection, 10%-15% of which will develop cirrhosis at 20 years after contracting the illness[38].
BOC
Cirrhosis, regardless of its level of compensation, has been documented on several occasions to result in decreased SVR in patients being treated for HCV. A meta-analysis done by Vierling et al[6] examined 5, phase III, clinical trials of biopsy proven cirrhosis patients treated with either RBV and peg-IFN alone or in combination with BOC. Pooled estimates from these studies revealed a 55% SVR in the triple therapy group compared with 17% in the RBV and peg-IFN group. In terms of adverse side effects, anemia and diarrhea were significantly more prevalent in the triple therapy treatment arm. This postulated to be the result of either added side effects of BOC or the patient’s underlying cirrhosis.
Simeprevir
PROMISE: Genotype 1, previous PR, with cirrhosis: In the trial by Forns et al[10] as mentioned above, a subpopulation of patients with cirrhosis/advanced fibrosis were studied and were able to achieve an SVR of 74%, compared to 79% when not taking into account presence of cirrhosis. Common adverse events included rash, flulike illness, pruritus and therefore had a better side effect profile than its predecessor’s BOC and TVR. One factor that must be considered when using simeprevir is testing for the Q80K mutation prior to treatment initiation. Diminished responses were noted in genotype 1A with the mutation.
SOF
FISSION: Genotype 2 and genotype 3, treatment naïve, with and without cirrhosis: Four hundred and ninety nine genotype 2 and 3 patients were treated with either 12 wk of SOF and RBV or 24 wk of peg-IFN and RBV. Of the 499, 70% were genotype 3 and of these 20% were documented cirrhotic. The trial met the non-inferiority endpoint, showing an overall SVR rate of 67%, however analysis based on HCV genotype showed genotype 2 patients achieved 93% SVR, compared to only 56% in genotype 3 patients. Furthermore, liver fibrosis further decreased SVR to 34%. Cirrhosis in the genotype-2 patients did not influence SVR rates (91%) comparatively[14].
FUSION: Genotype 2 and genotype 3, previous PR, with and without cirrhosis: In the FUSION trial, subgroup analysis among cirrhotic patients with HCV treated with either 12 or 16 wk of SOF and RBV showed favorable results among genotype 2 patients treated for 16 wk. In this group an SVR of 78% was achieved. Less favorable results were noted in the 12-wk group with slightly better results occurring in those with genotype 2 (Figure 2).
Figure 2.
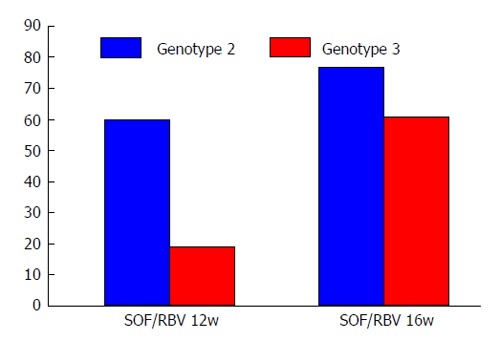
Cirrhotic patients in the fusion trial. SOF: Sofosbuvir; RBV: Ribavirin.
SOF/LED
A recently published randomized trial by Gane et al[39] in Gastroenterology focusing on treatment with SOF in combination with LED with or without RBV for treatment of null responders with cirrhosis showed promising results. All patients (9/9) receiving triple therapy were able to achieve SVR. In the group of those receiving only SOF and LED, 7 of 10 achieved SVR. Both the unknown degree of cirrhosis and the small sample size remain limiting factors in this study. Adverse effects related to the RBV regimen are consistent with prior studies of cirrhotic patients showing a greater percentage of anemia in this group. In the RBV free regimen patients remained with stable hemoglobin levels suggesting that RBV and not cirrhosis itself contributes the anemia seen with typical treatment regimens.
LONESTAR: Previous DAA + DAA failure: In the trial by Lawitz et al[14], similar success rates in cirrhotic patients being treated with SOF based regimens vs non-cirrhotic patients was noted. Twenty two of 40 previously treated patients with compensated cirrhosis fared well overall, given that 39/40 of the patients achieved SVR, however this study is limited by its relatively small size.
It remains essential that we understand that development of cirrhosis in patients with hepatitis C leads to a potentially devastating disease. Once decompensation with either development of ascites, variceal hemorrhage, encephalopathy, coagulopathy, the probability of survival is only 50% at five years, with a median survival of only two years[40,41]. Therefore, pursuit of a cure using direct antiviral therapy should be pursued. Of the discussed DAAs, SOF-based regimens appear to provide the best chance of this and are consistent with the recommended treatment regimens of recently published consensus guidelines.
BARRIERS TO TREATMENT
Hepatitis C is a physical, mental, and social disease affecting not only the individual, but also the individual’s loved ones and society as a whole. Considered a global disease, and for that matter the only currently curable chronic viral infection, the importance of pursuing treatment for hepatitis C remains paramount. Despite this, several barriers hindering this effort have been identified. These include: awareness of available therapy, financial constraints, and practitioners willing to prescribe treatment.
Comorbid psychiatric illness
It is well known the concomitant psychiatric illness plagues patients with hepatitis C. It is currently estimated that the largest at risk population for contracting hepatitis C is it that of intravenous (iv) drug users[42]. The problem is two-fold, in a study done by Johnson et al[43] in the American Journal of Gastroenterology, 309 current iv drug users undergoing substance abuse treatment were evaluated. In this group over 50% of test subjects were found to be positive for HCV antibodies and of the HCV positive patients, over half were noted to have concomitant depression. In addition to the pre-existing depression seen in this group, the treatment for HCV itself up until this point had also significantly contributed to depressive symptoms. Interferon in particular, has had a documented side effect profile consisting of fatigue, anxiety, and depression. Despite the black box warning associated with peg-IFN, studies show that patients with mood disorders currently in remission and receiving treatment should not be excluded from receiving interferon therapy[44]. Additionally, treatment of interferon associated depression and cognitive disorders can be achieved with the use of antidepressants and stimulators[45,46].
It is estimated that one in six incarcerated patients have hepatitis C and therefor the public perception remains that hepatitis C is acquired illness. As such, I anticipate continued difficulty obtaining social and financial support for concomitant iv drug use treatment, despite the fact that studies show co-administration of strict drug treatment program decreased risk of relapse and increase completion of treatment and monitoring.
Cost
Despite the excitement and promise these new therapies all hold, the cost-effectiveness of pursuing cure for hepatitis C has been a tougher pill to swallow than the actual treatment itself. SOF has been drawing attention recently. At around one thousand dollars per pill, 12 wk, a standard treatment course would run the patient and their insurance provider approximately $84000 with other DAA sharing similar price tags. The endeavor of validating coverage depends on the potential long-term savings from providing a cure. It is difficult to estimate the exact savings per patient due to the various other factors involved, however rough estimates are possible. Consider this, the average annual health care costs for patients with chronic hepatitis C infection without cirrhosis is $17277. Once cirrhosis develops costs rise to $22752 among patients with compensated cirrhosis, and $59995 once end-stage liver disease develops[47]. Patients with compensated cirrhosis have been documented to live for at least a decade prior to development of decompensation[40]. This would amount to approximately $275000 in health care costs over this decade. Considering the median two-year survival for decompensated cirrhosis an additional $120000 would accrue. Lastly, if a candidate, liver transplantation with an average price tag ranging in upwards of $575000, per United Network for Organ Sharing, brings the total to over $1 million in health care costs[48]. Looking back at the treatment price tag of $84000 little hesitation should be had. This is not the case however because many variables play a part. Notably, incomplete treatment, unsuccessful treatment, and reinfection are always possible, particularly in patients with comorbid psychiatric illness, concomitant drug addiction, and poor social support; all known risks factors for contracting HCV[49]. In the long run this issue should continue to fade in its controversy given that minimum manufacturing costs for producing direct acting antivirals have been estimated at $100-$250 for a 12 wk course of treatment once patent expires and production of generic versions is available[50].
Aside from the cost savings achieved when no longer needing to treat the manifestations of chronic hepatitis C, cure of hepatitis C has been shown to provide additional benefits. Beside the improvement in psychological and social well-being which accompanies cure of hepatitis C, treatment also has been shown to decrease and potentially reverse cirrhosis, esophageal varices, and the risk for development of hepatocellular carcinoma[51-53].
Practitioner experience
In patients who are co-infected with HIV as well as HCV, the potential for complex drug interactions between HAART and direct antiviral agents can lead to trepidation among primary care providers when debating the initiation of treatment for HCV. Additionally, a practitioner’s concerns about reinfection as well as their bias regarding iv drug users also represent barriers to engagement in treatment of HCV in patients[54]. Therefore, it is recommended, as outlined in the recent consensus article published in The Infectious Disease Society of America, that only practitioners who are comfortable in routine treatment of HIV, cirrhosis, and/or have familiarity with DAA should be involved in treatment for HCV. Therefor infectious disease specialists and hepatologists should be the providers responsible for initiating treatment of HCV for co-infected individuals, cirrhotic patients, and patients who have previously failed treatment.
Tolerability
Treatment for HCV had long been known to be as unpleasant as it was burdensome, leading to noncompliance and decreased quality of life during treatment. IFN based regimens, in particular, are riddled with adverse side effects[55]. For example, both the BOC and TVR regimens have complex dosing schedules and heavy pill burdens that will invariably lead to both incomplete compliance and treatment dropout[56]. As new treatments arise, the effect of the various regimens should not only be examined for response rates but should be evaluated for their tolerability. In several studies, Younossi et al[57,58] did just that. Examination of patient reported outcomes and health related quality of life data of patients in four different phase III clinical trials noted that patients who received treatment with the peg-IFN free regimen of SOF and RBV noted the smallest decline in quality of life scores among all treatment groups suggesting that INF free regimens lead to better tolerability and better adherence; both factors essential in increasing compliance. Aside from side effects, route of administration will surely have patients asking for IFN free regimens[59].
CONCLUSION
As indicated in several of the studies reviewed, SOF appears to currently be one of the best choices in all-comers. Further studies with larger populations of difficult to treat patients are warranted to fully assess the continued success, safety and side effects. Based on the studies examined, most of which included phase II and III trials, the current literature favors usage of a SOF-based regimen in patients with cirrhosis, HIV/HCV co-infection and prior treatment failure. As shown, SOF has proven efficacy in both cirrhotic and non-cirrhotic patients and also appears to span all genotypes. The limited drug-drug interactions make it a favorable option in patients co-infected with HIV. Additionally, the route of administration and the favorable side effect profile will lead to overall improvement in quality of life and compliance. Treatment and cure of hepatitis C is now probable, even in “difficult to treat” patients. Without financial assistance programs, practitioner awareness, and co-administered substance abuse treatment programs the potential gains these revolutionary drugs offer will fail to render an impact on prevention of long-term hepatitis C complications.
Footnotes
P- Reviewer: Lim YS S- Editor: Gong XM L- Editor: A E- Editor: Liu SQ
Conflict-of-interest statement: The authors have no conflicts of interest to declare.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: August 26, 2014
First decision: December 17, 2014
Article in press: July 17, 2015
References
- 1.Denniston MM, Jiles RB, Drobeniuc J, Klevens RM, Ward JW, McQuillan GM, Holmberg SD. Chronic hepatitis C virus infection in the United States, National Health and Nutrition Examination Survey 2003 to 2010. Ann Intern Med. 2014;160:293–300. doi: 10.7326/M13-1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO. Hepatitis C, Fact sheet N°164. [Updated 2014 April] Available from: http://www.who.int/mediacentre/factsheets/fs164/en/ [Google Scholar]
- 3.American Association for the Study of Liver Diseases and the Infectious Diseases Society of America. Recommendations for Testing, Managing, and Treating Hepatitis C. Available from: http://www.hcvguidelines.org. [DOI] [PMC free article] [PubMed]
- 4.Sulkowski MS, Gardiner DF, Rodriguez-Torres M, Reddy KR, Hassanein T, Jacobson I, Lawitz E, Lok AS, Hinestrosa F, Thuluvath PJ, et al. Daclatasvir plus sofosbuvir for previously treated or untreated chronic HCV infection. N Engl J Med. 2014;370:211–221. doi: 10.1056/NEJMoa1306218. [DOI] [PubMed] [Google Scholar]
- 5.Zeuzem S, Andreone P, Pol S, Lawitz E, Diago M, Roberts S, Focaccia R, Younossi Z, Foster GR, Horban A, et al. Telaprevir for retreatment of HCV infection. N Engl J Med. 2011;364:2417–2428. doi: 10.1056/NEJMoa1013086. [DOI] [PubMed] [Google Scholar]
- 6.Vierling JM, Zeuzem S, Poordad F, Bronowicki JP, Manns MP, Bacon BR, Esteban R, Flamm SL, Kwo PY, Pedicone LD, et al. Safety and efficacy of boceprevir/peginterferon/ribavirin for HCV G1 compensated cirrhotics: meta-analysis of 5 trials. J Hepatol. 2014;61:200–209. doi: 10.1016/j.jhep.2014.03.022. [DOI] [PubMed] [Google Scholar]
- 7.Bacon BR, Gordon SC, Lawitz E, Marcellin P, Vierling JM, Zeuzem S, Poordad F, Goodman ZD, Sings HL, Boparai N, et al. Boceprevir for previously treated chronic HCV genotype 1 infection. N Engl J Med. 2011;364:1207–1217. doi: 10.1056/NEJMoa1009482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hézode C, Fontaine H, Dorival C, Zoulim F, Larrey D, Canva V, De Ledinghen V, Poynard T, Samuel D, Bourliere M, et al. Effectiveness of telaprevir or boceprevir in treatment-experienced patients with HCV genotype 1 infection and cirrhosis. Gastroenterology. 2014;147:132–142.e4. doi: 10.1053/j.gastro.2014.03.051. [DOI] [PubMed] [Google Scholar]
- 9.Zeuzem S, Berg T, Gane E, Ferenci P, Foster GR, Fried MW, Hezode C, Hirschfield GM, Jacobson I, Nikitin I, et al. Simeprevir increases rate of sustained virologic response among treatment-experienced patients with HCV genotype-1 infection: a phase IIb trial. Gastroenterology. 2014;146:430–41.e6. doi: 10.1053/j.gastro.2013.10.058. [DOI] [PubMed] [Google Scholar]
- 10.Forns X, Lawitz E, Zeuzem S, Gane E, Bronowicki JP, Andreone P, Horban A, Brown A, Peeters M, Lenz O, et al. Simeprevir with peginterferon and ribavirin leads to high rates of SVR in patients with HCV genotype 1 who relapsed after previous therapy: a phase 3 trial. Gastroenterology. 2014;146:1669–79.e3. doi: 10.1053/j.gastro.2014.02.051. [DOI] [PubMed] [Google Scholar]
- 11.Jacobson IM, Gordon SC, Kowdley KV, Yoshida EM, Rodriguez-Torres M, Sulkowski MS, Shiffman ML, Lawitz E, Everson G, Bennett M, et al. Sofosbuvir for hepatitis C genotype 2 or 3 in patients without treatment options. N Engl J Med. 2013;368:1867–1877. doi: 10.1056/NEJMoa1214854. [DOI] [PubMed] [Google Scholar]
- 12.Lawitz E, Sulkowski MS, Ghalib R, Rodriguez-Torres M, Younossi ZM, Corregidor A, DeJesus E, Pearlman B, Rabinovitz M, Gitlin N, et al. Simeprevir plus sofosbuvir, with or without ribavirin, to treat chronic infection with hepatitis C virus genotype 1 in non-responders to pegylated interferon and ribavirin and treatment-naive patients: the COSMOS randomised study. Lancet. 2014;384:1756–1765. doi: 10.1016/S0140-6736(14)61036-9. [DOI] [PubMed] [Google Scholar]
- 13.Afdhal N, Reddy KR, Nelson DR, Lawitz E, Gordon SC, Schiff E, Nahass R, Ghalib R, Gitlin N, Herring R, et al. Ledipasvir and sofosbuvir for previously treated HCV genotype 1 infection. N Engl J Med. 2014;370:1483–1493. doi: 10.1056/NEJMoa1316366. [DOI] [PubMed] [Google Scholar]
- 14.Lawitz E, Poordad FF, Pang PS, Hyland RH, Ding X, Mo H, Symonds WT, McHutchison JG, Membreno FE. Sofosbuvir and ledipasvir fixed-dose combination with and without ribavirin in treatment-naive and previously treated patients with genotype 1 hepatitis C virus infection (LONESTAR): an open-label, randomised, phase 2 trial. Lancet. 2014;383:515–523. doi: 10.1016/S0140-6736(13)62121-2. [DOI] [PubMed] [Google Scholar]
- 15.Zeuzem S, Jacobson IM, Baykal T, Marinho RT, Poordad F, Bourlière M, Sulkowski MS, Wedemeyer H, Tam E, Desmond P, et al. Retreatment of HCV with ABT-450/r-ombitasvir and dasabuvir with ribavirin. N Engl J Med. 2014;370:1604–1614. doi: 10.1056/NEJMoa1401561. [DOI] [PubMed] [Google Scholar]
- 16.Zeremski M, Martinez AD, Talal AH. Editorial commentary: Management of hepatitis C Virus in HIV-infected patients in the era of direct-acting antivirals. Clin Infect Dis. 2014;58:880–882. doi: 10.1093/cid/cit804. [DOI] [PubMed] [Google Scholar]
- 17.Torriani FJ, Rodriguez-Torres M, Rockstroh JK, Lissen E, Gonzalez-García J, Lazzarin A, Carosi G, Sasadeusz J, Katlama C, Montaner J, et al. Peginterferon Alfa-2a plus ribavirin for chronic hepatitis C virus infection in HIV-infected patients. N Engl J Med. 2004;351:438–450. doi: 10.1056/NEJMoa040842. [DOI] [PubMed] [Google Scholar]
- 18.Opravil M, Rodriguez-Torres M, Rockstroh J, Snoeck E, Chung RT, Tietz A, Torriani FJ. The dose-response relationship of peginterferon alfa-2a and ribavirin in the treatment of patients coinfected with HIV-HCV. HIV Clin Trials. 2012;13:33–45. doi: 10.1310/hct1301-033. [DOI] [PubMed] [Google Scholar]
- 19.Benhamou Y, Di Martino V, Bochet M, Colombet G, Thibault V, Liou A, Katlama C, Poynard T. Factors affecting liver fibrosis in human immunodeficiency virus-and hepatitis C virus-coinfected patients: impact of protease inhibitor therapy. Hepatology. 2001;34:283–287. doi: 10.1053/jhep.2001.26517. [DOI] [PubMed] [Google Scholar]
- 20.Deng A, Chen C, Ishizaka Y, Chen X, Sun B, Yang R. Human immunodeficiency virus type 1 Vpr increases hepatitis C virus RNA replication in cell culture. Virus Res. 2014;184:93–102. doi: 10.1016/j.virusres.2014.02.017. [DOI] [PubMed] [Google Scholar]
- 21.Di Martino V, Rufat P, Boyer N, Renard P, Degos F, Martinot-Peignoux M, Matheron S, Le Moing V, Vachon F, Degott C, et al. The influence of human immunodeficiency virus coinfection on chronic hepatitis C in injection drug users: a long-term retrospective cohort study. Hepatology. 2001;34:1193–1199. doi: 10.1053/jhep.2001.29201. [DOI] [PubMed] [Google Scholar]
- 22.Weber R, Sabin CA, Friis-Møller N, Reiss P, El-Sadr WM, Kirk O, Dabis F, Law MG, Pradier C, De Wit S, et al. Liver-related deaths in persons infected with the human immunodeficiency virus: the D: A: D study. Arch Intern Med. 2006;166:1632–1641. doi: 10.1001/archinte.166.15.1632. [DOI] [PubMed] [Google Scholar]
- 23.Sherman KE. Treatment of hepatitis C virus and human immunodeficiency virus co-infection. Clin Gastroenterol Hepatol. 2005;3:S118–S121. doi: 10.1016/s1542-3565(05)00704-4. [DOI] [PubMed] [Google Scholar]
- 24.Kovari H, Sabin CA, Ledergerber B, Ryom L, Worm SW, Smith C, Phillips A, Reiss P, Fontas E, Petoumenos K, et al. Antiretroviral drug-related liver mortality among HIV-positive persons in the absence of hepatitis B or C virus coinfection: the data collection on adverse events of anti-HIV drugs study. Clin Infect Dis. 2013;56:870–879. doi: 10.1093/cid/cis919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Russmann S, Kullak-Ublick GA, Grattagliano I. Current concepts of mechanisms in drug-induced hepatotoxicity. Curr Med Chem. 2009;16:3041–3053. doi: 10.2174/092986709788803097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thomas DL. The challenge of hepatitis C in the HIV-infected person. Annu Rev Med. 2008;59:473–485. doi: 10.1146/annurev.med.59.081906.081110. [DOI] [PubMed] [Google Scholar]
- 27.Chen EY, North CS, Fatunde O, Bernstein I, Salari S, Day B, Jain MK. Knowledge and attitudes about hepatitis C virus (HCV) infection and its treatment in HCV mono-infected and HCV/HIV co-infected adults. J Viral Hepat. 2013;20:708–714. doi: 10.1111/jvh.12095. [DOI] [PubMed] [Google Scholar]
- 28.Karageorgopoulos DE, El-Sherif O, Bhagani S, Khoo SH. Drug interactions between antiretrovirals and new or emerging direct-acting antivirals in HIV/hepatitis C virus coinfection. Curr Opin Infect Dis. 2014;27:36–45. doi: 10.1097/QCO.0000000000000034. [DOI] [PubMed] [Google Scholar]
- 29.Carrat F, Bani-Sadr F, Pol S, Rosenthal E, Lunel-Fabiani F, Benzekri A, Morand P, Goujard C, Pialoux G, Piroth L, et al. Pegylated interferon alfa-2b vs standard interferon alfa-2b, plus ribavirin, for chronic hepatitis C in HIV-infected patients: a randomized controlled trial. JAMA. 2004;292:2839–2848. doi: 10.1001/jama.292.23.2839. [DOI] [PubMed] [Google Scholar]
- 30.Chung RT, Andersen J, Volberding P, Robbins GK, Liu T, Sherman KE, Peters MG, Koziel MJ, Bhan AK, Alston B, et al. Peginterferon Alfa-2a plus ribavirin versus interferon alfa-2a plus ribavirin for chronic hepatitis C in HIV-coinfected persons. N Engl J Med. 2004;351:451–459. doi: 10.1056/NEJMoa032653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Laguno M, Murillas J, Blanco JL, Martínez E, Miquel R, Sánchez-Tapias JM, Bargallo X, García-Criado A, de Lazzari E, Larrousse M, et al. Peginterferon alfa-2b plus ribavirin compared with interferon alfa-2b plus ribavirin for treatment of HIV/HCV co-infected patients. AIDS. 2004;18:F27–F36. doi: 10.1097/00002030-200409030-00003. [DOI] [PubMed] [Google Scholar]
- 32.Sulkowski MS, Sherman KE, Dieterich DT, Bsharat M, Mahnke L, Rockstroh JK, Gharakhanian S, McCallister S, Henshaw J, Girard PM, et al. Combination therapy with telaprevir for chronic hepatitis C virus genotype 1 infection in patients with HIV: a randomized trial. Ann Intern Med. 2013;159:86–96. doi: 10.7326/0003-4819-159-2-201307160-00654. [DOI] [PubMed] [Google Scholar]
- 33.Sulkowski M, Pol S, Mallolas J, Fainboim H, Cooper C, Slim J, Rivero A, Mak C, Thompson S, Howe AY, et al. Boceprevir versus placebo with pegylated interferon alfa-2b and ribavirin for treatment of hepatitis C virus genotype 1 in patients with HIV: a randomised, double-blind, controlled phase 2 trial. Lancet Infect Dis. 2013;13:597–605. doi: 10.1016/S1473-3099(13)70149-X. [DOI] [PubMed] [Google Scholar]
- 34.Sulkowski MS, Naggie S, Lalezari J, Fessel WJ, Mounzer K, Shuhart M, Luetkemeyer AF, Asmuth D, Gaggar A, Ni L, et al. Sofosbuvir and ribavirin for hepatitis C in patients with HIV coinfection. JAMA. 2014;312:353–361. doi: 10.1001/jama.2014.7734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Osinusi A, Kohli A, Marti MM, Nelson A, Zhang X, Meissner EG, Silk R, Townsend K, Pang PS, Subramanian GM, et al. Re-treatment of chronic hepatitis C virus genotype 1 infection after relapse: an open-label pilot study. Ann Intern Med. 2014;161:634–638. doi: 10.7326/M14-1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fontana RJ, Everson GT, Tuteja S, Vargas HE, Shiffman ML. Controversies in the management of hepatitis C patients with advanced fibrosis and cirrhosis. Clin Gastroenterol Hepatol. 2004;2:183–197. doi: 10.1016/s1542-3565(04)00002-3. [DOI] [PubMed] [Google Scholar]
- 37.Kim MY, Jeong WK, Baik SK. Invasive and non-invasive diagnosis of cirrhosis and portal hypertension. World J Gastroenterol. 2014;20:4300–4315. doi: 10.3748/wjg.v20.i15.4300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.National Institutes of Health Consensus Development Conference Statement: Management of hepatitis C 2002 (June 10-12, 2002) Gastroenterology. 2002;123:2082–2099. doi: 10.1053/gast.2002.1232082. [DOI] [PubMed] [Google Scholar]
- 39.Gane EJ, Stedman CA, Hyland RH, Ding X, Svarovskaia E, Subramanian GM, Symonds WT, McHutchison JG, Pang PS. Efficacy of nucleotide polymerase inhibitor sofosbuvir plus the NS5A inhibitor ledipasvir or the NS5B non-nucleoside inhibitor GS-9669 against HCV genotype 1 infection. Gastroenterology. 2014;146:736–743.e1. doi: 10.1053/j.gastro.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 40.Fattovich G, Giustina G, Degos F, Tremolada F, Diodati G, Almasio P, Nevens F, Solinas A, Mura D, Brouwer JT, et al. Morbidity and mortality in compensated cirrhosis type C: a retrospective follow-up study of 384 patients. Gastroenterology. 1997;112:463–472. doi: 10.1053/gast.1997.v112.pm9024300. [DOI] [PubMed] [Google Scholar]
- 41.D’Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44:217–231. doi: 10.1016/j.jhep.2005.10.013. [DOI] [PubMed] [Google Scholar]
- 42.Aspinall EJ, Corson S, Doyle JS, Grebely J, Hutchinson SJ, Dore GJ, Goldberg DJ, Hellard ME. Treatment of hepatitis C virus infection among people who are actively injecting drugs: a systematic review and meta-analysis. Clin Infect Dis. 2013;57 Suppl 2:S80–S89. doi: 10.1093/cid/cit306. [DOI] [PubMed] [Google Scholar]
- 43.Johnson ME, Fisher DG, Fenaughty A, Theno SA. Hepatitis C virus and depression in drug users. Am J Gastroenterol. 1998;93:785–789. doi: 10.1111/j.1572-0241.1998.225_a.x. [DOI] [PubMed] [Google Scholar]
- 44.Malek-Ahmadi P. Mood disorders associated with interferon treatment: theoretical and practical considerations. Ann Pharmacother. 2001;35:489–495. doi: 10.1345/aph.10172. [DOI] [PubMed] [Google Scholar]
- 45.Valentine AD, Meyers CA. Neurobehavioral effects of interferon therapy. Curr Psychiatry Rep. 2005;7:391–395. doi: 10.1007/s11920-005-0042-3. [DOI] [PubMed] [Google Scholar]
- 46.Angelino AF, Treisman GJ. Evidence-informed assessment and treatment of depression in HCV and interferon-treated patients. Int Rev Psychiatry. 2005;17:471–476. doi: 10.1080/02646830500381567. [DOI] [PubMed] [Google Scholar]
- 47.Gordon SC, Pockros PJ, Terrault NA, Hoop RS, Buikema A, Nerenz D, Hamzeh FM. Impact of disease severity on healthcare costs in patients with chronic hepatitis C (CHC) virus infection. Hepatology. 2012;56:1651–1660. doi: 10.1002/hep.25842. [DOI] [PubMed] [Google Scholar]
- 48.Reau NS, Jensen DM. Sticker shock and the price of new therapies for hepatitis C: is it worth it? Hepatology. 2014;59:1246–1249. doi: 10.1002/hep.27039. [DOI] [PubMed] [Google Scholar]
- 49.Alter MJ. Epidemiology of hepatitis C virus infection. World J Gastroenterol. 2007;13:2436–2441. doi: 10.3748/wjg.v13.i17.2436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hill A, Khoo S, Fortunak J, Simmons B, Ford N. Minimum costs for producing hepatitis C direct-acting antivirals for use in large-scale treatment access programs in developing countries. Clin Infect Dis. 2014;58:928–936. doi: 10.1093/cid/ciu012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Morgan RL, Baack B, Smith BD, Yartel A, Pitasi M, Falck-Ytter Y. Eradication of hepatitis C virus infection and the development of hepatocellular carcinoma: a meta-analysis of observational studies. Ann Intern Med. 2013;158:329–337. doi: 10.7326/0003-4819-158-5-201303050-00005. [DOI] [PubMed] [Google Scholar]
- 52.Bruno S, Crosignani A, Facciotto C, Rossi S, Roffi L, Redaelli A, de Franchis R, Almasio PL, Maisonneuve P. Sustained virologic response prevents the development of esophageal varices in compensated, Child-Pugh class A hepatitis C virus-induced cirrhosis. A 12-year prospective follow-up study. Hepatology. 2010;51:2069–2076. doi: 10.1002/hep.23528. [DOI] [PubMed] [Google Scholar]
- 53.Poynard T, McHutchison J, Manns M, Trepo C, Lindsay K, Goodman Z, Ling MH, Albrecht J. Impact of pegylated interferon alfa-2b and ribavirin on liver fibrosis in patients with chronic hepatitis C. Gastroenterology. 2002;122:1303–1313. doi: 10.1053/gast.2002.33023. [DOI] [PubMed] [Google Scholar]
- 54.Zeremski M, Zibbell JE, Martinez AD, Kritz S, Smith BD, Talal AH. Hepatitis C virus control among persons who inject drugs requires overcoming barriers to care. World J Gastroenterol. 2013;19:7846–7851. doi: 10.3748/wjg.v19.i44.7846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Marinho RT, Barreira DP. Hepatitis C, stigma and cure. World J Gastroenterol. 2013;19:6703–6709. doi: 10.3748/wjg.v19.i40.6703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Younossi ZM, Singer ME, Mir HM, Henry L, Hunt S. Impact of interferon free regimens on clinical and cost outcomes for chronic hepatitis C genotype 1 patients. J Hepatol. 2014;60:530–537. doi: 10.1016/j.jhep.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 57.Younossi ZM, Stepanova M, Henry L, Gane E, Jacobson IM, Lawitz E, Nelson D, Gerber L, Nader F, Hunt S. Effects of sofosbuvir-based treatment, with and without interferon, on outcome and productivity of patients with chronic hepatitis C. Clin Gastroenterol Hepatol. 2014;12:1349–1359.e13. doi: 10.1016/j.cgh.2013.11.032. [DOI] [PubMed] [Google Scholar]
- 58.Younossi ZM, Stepanova M, Henry L, Gane E, Jacobson IM, Lawitz E, Nelson D, Nader F, Hunt S. Minimal impact of sofosbuvir and ribavirin on health related quality of life in chronic hepatitis C (CH-C) J Hepatol. 2014;60:741–747. doi: 10.1016/j.jhep.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 59.Feld JJ. The beginning of the end: what is the future of interferon therapy for chronic hepatitis C? Antiviral Res. 2014;105:32–38. doi: 10.1016/j.antiviral.2014.02.005. [DOI] [PubMed] [Google Scholar]


