Abstract
Neighborhood deprivation is consistently associated with greater risk of low birthweight. However, large birth size is increasingly relevant but overlooked in neighborhood health research, and proximity within which neighborhood deprivation may affect birth outcomes is unknown. We estimated race/ethnic-specific effects of neighborhood deprivation index (NDI) within 1, 3, 5, and 8 km buffers around Oregon Pregnancy Risk Assessment Monitoring System (n=3,716; 2004-2007) respondents’ homes on small and large for gestational age (SGA, LGA). NDI was positively associated with LGA and SGA in most race/ethnic groups. The results varied little across the four buffer sizes.
Keywords: pregnancy outcome, neighborhood, socioeconomic factors, fetal growth
Background
Neighborhood context is recognized as an important risk factor for poor birth outcomes (Metcalfe, et al., 2011). Neighborhood socioeconomic deprivation is hypothesized to affect maternal health both through psychosocial factors and through access to material resources (Daniel, et al., 2008; Culhane and Elo, 2005; Schempf, et al., 2009). In a large body of literature, neighborhood deprivation is a strong, consistent predictor of low birthweight, preterm birth, and small for gestational age (SGA) (Sundquist, et al., 2011; Elo, et al., 2009; Janevic, et al., 2010; Zeka, et al., 2008; Agyemang, et al., 2009; Masi, et al., 2007; Farley, et al., 2006; Subramanian, et al., 2006; Schempf, et al., 2009; Nkansah-Amankra, et al., 2010; Collins, et al., 2009; Auger, et al., 2013; Buka, et al., 2003; Beard, et al., 2009; Garcia-Subirats, et al., 2012; Messer, et al., 2008). However, associations between neighborhood context and large for gestational age (LGA) have received little consideration.
Adverse health outcomes of small birth size are widely recognized, but infants born LGA also have greater risk of poor health outcomes ranging from infant mortality to diabetes and cardiovascular disease throughout the life span (Boney, et al., 2005; Barker and Thornburg, 2013; Barker, 1995; Bocca-Tjeertes, et al., 2014; Moore, et al., 2012; Wang, et al., 2007). LGA deliveries have greater risk of cesarean section, postpartum hemorrhage, and birth injury to the mother or infant (Weissmann-Brenner, et al., 2012). Moreover, LGA is of growing importance as prevalence of two major LGA risk factors – obesity and diabetes (Yessoufou and Moutairou, 2011; Boney, et al., 2005; Lu, et al., 2001) – continues to increase. Individual risk factors for birth outcomes are shaped by environmental context (Hogan, et al., 2001), and neighborhood deprivation is associated with obesity in adult men and women (Pearson, et al., 2014; Bell, et al., 2014), overweight in the first trimester of pregnancy (Clausen, et al., 2006), and gestational diabetes (Clausen, et al., 2006; Janghorbani, et al., 2006).
Our understanding of how neighborhood deprivation shapes birth outcomes is limited in several ways. In particular, the proximity within which area-level socioeconomic disadvantage might influence birth outcomes is unknown. Furthermore, delineation of meaningful geographic exposures may vary between SGA and LGA because they may involve different causal pathways (Coulton, et al., 2012; Diez Roux, 2007; Spielman and Yoo, 2009; Daniel, et al., 2008; Soobader, et al., 2006; Flowerdew, et al., 2008; Krieger, et al., 2003) . That is, we theorize effects on LGA to operate through neighborhood environments that promote obesity-related behaviors (Diez Roux and Mair, 2010; Schempf, et al., 2009; Daniel, et al., 2008; Culhane and Elo, 2005; Vinikoor-Imler, et al., 2011; Elo, et al., 2009; Metcalfe, et al., 2011). Behavioral pathways leading to LGA may involve smaller-scale neighborhood features than neighborhood effects on SGA, which are theorized to operate through stress pathways (Wadhwa, et al., 2011; Culhane and Elo, 2005; Vinikoor-Imler, et al., 2011; Elo, et al., 2009; Metcalfe, et al., 2011; Messer, et al., 2012a).
In addition, it is possible that neighborhood deprivation within varying proximity to residences may be differentially associated with SGA and LGA across racial and ethnic groups (Buka, et al., 2003; Vinikoor-Imler, et al., 2011; Love, et al., 2010; Janevic, et al., 2010; O'Campo, et al., 2008; Messer, et al., 2012b). Stark racial and ethnic disparities exist in SGA (Hogan, et al., 2012; Lu and Halfon, 2003; Blumenshine, et al., 2010; Geronimus, 1996; Collins, et al., 2004; Giscombe and Lobel, 2005), and evidence also suggests that disparities exist in LGA (Rodrigues, et al., 2000; Wassimi, et al., 2011; Dyer, et al., 2007; Homko, et al., 1995; Bowers, et al., 2013). Stress and obesity-related pathways may be more important in some race/ethnic groups, and transportation within a community may be more constrained in minority racial/ethnic groups. Using data from a diverse study population of Hispanic and non-Hispanic White, Black, Asian, and Native American women, we expand existing literature on effects of neighborhood deprivation on small birth size to include LGA, and compare associations across four proximity-based neighborhood boundaries.
Materials and Methods
Data sources
This study used 2004-2007 Oregon Pregnancy Risk Assessment Monitoring System (PRAMS) data. PRAMS is an ongoing population-based surveillance system that randomly samples women from the state birth record and collects information on experiences before, during, and shortly after pregnancy. Oregon PRAMS oversampled low birthweight deliveries (<2500g) and racial and ethnic minorities, and excluded women who did not live in Oregon or gave birth >180 days before sampling. Women were contacted up to four times by mail, and a telephone interview was attempted with non-responders; the final weighted response rate was 72.0%. Women reported as Hispanic on the birth certificate were contacted in both English and Spanish. The Oregon Office of Family Health linked Oregon birth certificate data to PRAMS survey responses. Survey response weights were adjusted for oversampling, non-response, and non-coverage.
Study Sample
We collected geographic information for all PRAMS respondents residing in the Portland Tri-County area (Multnomah, Clackamas, and Washington Counties; N=3,930). We limited the sample to singleton births with birthweight over 400g, gestational age 20-42 weeks, and maternal age 14-44 years. Of the remaining 3,759 women, 10 observations were missing the mother's race/ethnicity. Less than 1% of records were missing data on confounding variables (maternal age, education, parity, and insurance status), for a final sample size of 3,716 women with complete information.
Variables
Exposure: 1, 3, 5, and 8 km radius Neighborhood Deprivation Index
We constructed a standardized neighborhood deprivation index (NDI) as described previously (Janevic, et al., 2010; Elo, et al., 2009; O'Campo, et al., 2008; Messer, et al., 2006b). Briefly, we used principal components analysis on 20 Census Tract-level sociodemographic variables from the 2000 US census previously identified to approximate neighborhood-level environments (Messer, et al., 2006b) along with one additional variable, percent Hispanic ethnicity. Six variables had factor loadings greater than 0.25 and were retained in the final principal component analysis (supplement table A-1). Variable values were weighted according to final factor loadings to create a continuous index score for each Census Tract. To generate an NDI score for the area within 1, 3, 5, or 8 km of each woman's place of residence (individually-defined circular neighborhood buffers) from data available at the census tract level, a weighted average was calculated according to the proportion of each census tract falling within the buffer. A higher (positive) score represented greater neighborhood deprivation.
Outcome: Size for Gestational Age
Birthweight and the clinical estimate of gestational age reported on the birth certificate were used to assign the gestational week-specific percentile of weight according to a standard population distribution (Hadlock, et al., 1991). The clinical estimate of gestational age provided more complete data and may reduce systematic error present in the last menstrual period estimate (Hoffman, et al., 2008; Mustafa and David, 2001; Qin, et al., 2008; Lazariu, et al., 2013). Because maternal characteristics such as race are not modifiable, race-specific size for gestational age distributions are sometimes used for tracking fetal growth throughout a woman's pregnancy. However, differences in birthweight distributions of different racial groups are likely due to differences in confounding variables such as SES, and falling in an extreme of either end on a standard fetal growth curve is generally a marker for increased risk of future adverse outcomes regardless of race (Hutcheon, et al., 2011), although this has been questioned for LGA among Aboriginal women in Canada (Gray-Donald, 2011). This weight for gestational age percentile was categorized as SGA (10th percentile of the standard curve and under), AGA (between 10th and 90th percentiles), and LGA (90th percentile and above).
Stratification variable: Race and ethnicity
The mother's race/ethnicity was reported on the birth certificate. We grouped women into mutually exclusive race/ethnicity categories: Hispanic (any race), and four non-Hispanic groups: White, Black, Asian/Pacific Islander, Native American.
Control variables
In order to maintain comparability across models with four measures of NDI, we selected a fixed set of a priori confounders from published literature on neighborhood deprivation and SGA or low birthweight (Cubbin, et al., 2008; Elo, et al., 2009; Janevic, et al., 2010; Messer, et al., 2008; Nkansah-Amankra, et al., 2010; O'Campo, et al., 2008; Schempf, et al., 2009; Schempf, et al., 2011; Masi, et al., 2007; Agyemang, et al., 2009; Zeka, et al., 2008; Subramanian, et al., 2006; Urquia, et al., 2009; Auger, et al., 2013). All of the identified studies adjusted for maternal age (mean-centered), education, and an additional measure of individual SES, if available. Half of these studies also adjusted for parity (Agyemang, et al., 2009; Zeka, et al., 2008; Masi, et al., 2007; Schempf, et al., 2011; Janevic, et al., 2010; Cubbin, et al., 2008; Auger, et al., 2013), which was defined as nulliparous versus ≥1 previous births. Neighborhood deprivation may influence income and education attainment, as well as fertility and family planning decisions (Tumen, 2012; Simon and Tamura, 2009); thus, individual SES and parity may mediate effects of neighborhood deprivation on birth size. However, influences of individual SES and household size on residential selection decisions that balance housing cost and size are likely stronger (Sampson and Sharkey, 2008; Lund, 2006; Walker and Li, 2007), at least in the short term. Therefore, we treated individual SES and parity as confounders, rather than mediators. We avoided potential bias due to exclusion of individuals with missing income information by using education (≤12, >12 years) and insurance status (private health insurance, other source paid for birth) as indicators of individual socioeconomic position. However, results controlling for individual income were similar (data not shown).
Fewer studies adjusted for pre-pregnancy BMI (Janevic, et al., 2010; Agyemang, et al., 2009), smoking (Elo, et al., 2009; Agyemang, et al., 2009; Masi, et al., 2007; Zeka, et al., 2008; Janevic, et al., 2010), prenatal care (Agyemang, et al., 2009; Masi, et al., 2007; Zeka, et al., 2008), or other medical risk factors (Elo, et al., 2009; Zeka, et al., 2008). We did not adjust for BMI, smoking, or prenatal care because they are theorized as mediators of the relationship between neighborhood deprivation and size for gestational age (Vinikoor-Imler, et al., 2011; Messer, et al., 2012b; Schempf, et al., 2009).
Statistical analysis
We used the suite of survey procedures in SAS version 9.2 to adjust for stratified sampling and weighting. Using repeated measures ANOVA, we determined if the mean NDI measurements were significantly different across buffer size, taking into account survey weights but not sampling strata. All subsequent analyses were stratified by race/ethnicity to estimate race/ethnic-specific effects and avoid comparing groups for whom we have not completely controlled for confounding by socioeconomic status (Kaufman, et al., 1997).
To examine the association between neighborhood deprivation and size for gestational age, we used race-specific multivariable multinomial logistic regression models with nominal outcomes SGA, LGA, and AGA with the AGA category as the reference level. The multinomial regression models adjusted for stratified sampling (oversampled subpopulations, and by survey year) and survey weighting using proc surveylogistic with generalized logit link. Our primary exposure of interest was NDI, and all models were adjusted for a priori confounding variables. We measured NDI as a continuous variable to incorporate variation across the range of NDI, with careful assessment of its functional form. Specifically, we assessed linearity of NDI, as well as maternal age, in logit for each race/ethnicity stratum and included significant (p<0.05) higher order terms (e.g. quadratic, cubic) to account for non-linear associations.
To facilitate interpretation of non-monotonic associations, we used estimated coefficients for the continuous NDI variables to calculate odds ratios comparing high (90th percentile of NDI: 0.911, 1 km; 0.549, 3 km; 0.326, 5 km; 0.137, 8 km) and medium deprivation (50th percentile; −0.515, 1 km; −0.533, 3 km; −0.684, 5 km; −0.736, 8 km) to low deprivation (10th percentile; −1.580, 1 km; −1.415, 3 km; −1.374, 5 km; −1.247, 8 km) based on percentiles in the pooled sample. The pooled 10th and 90th percentiles of NDI were within the range of NDI for each race/ethnic group and did not represent extreme outliers in any group. In the Black group, which had the highest mean NDI, the pooled 10th percentile of NDI corresponded to approximately the 3rd percentile of NDI in Blacks for all buffer sizes. The Asian group had the lowest average NDI scores, and the pooled 90th percentile of NDI was between the 90th and 92nd percentile of NDI in Asians.
Our regression models adjusted for stratified sampling (oversampled subpopulations, and by survey year) and survey weighting. They were not multilevel because the geographic exposure was defined at the individual-level, as performed by previous studies using circular buffers to define neighborhoods (Boone-Heinonen, et al., 2010; Leung, et al., 2011; Auchincloss, et al., 2008). Race/ethnicity-stratified models contained an average of 1.7 to 4.0 observations per census tract (Table 1) over the study period. Our analysis corrected for clustering within year, and separate random effects logit models predicting SGA/AGA or LGA/AGA showed relatively small intraclass correlations (ICC) within census tracts. LGA race-specific ICCs were ≤0.04 and SGA ICCs were <0.01 overall; race-specific SGA ICCs were generally small in magnitude, though larger in some subgroups (White: ICC=0.06; Black: ICC=0.11; Hispanic: ICC=0.32). We omitted Hispanic women with SGA infants from our multivariate analysis, largely due to the small number of SGA observations in this group.
Table 1.
Characteristics of Oregon PRAMS respondents in Tri-County area by race and ethnicity, 2004-2007 [%/mean (SE)]a
| White | Black | Asian | Hispanic | Native American | |
|---|---|---|---|---|---|
| Count (n)b | 980 | 746 | 925 | 811 | 254 |
| Maternal age (mean (SE)) | 29.2 (0.22) | 26.7 (0.23) | 30.8 (0.18) | 27.0 (0.21) | 26.5 (0.38) |
| > 12 years education (%) | 68.21 | 43.44 | 71.66 | 17.32 | 41.18 |
| % FPL (mean(SE)) | 246.5 (5.0) | 131.8 (4.3) | 251.1 (4.3) | 98.9 (3.5) | 158.2 (7.7) |
| Nulliparous (%) | 45.71 | 43.23 | 45.56 | 32.85 | 44.02 |
| Private health insurance (%) | 75.63 | 41.17 | 80.09 | 26.82 | 44.50 |
| Married (%) | 76.31 | 34.32 | 85.93 | 53.89 | 44.04 |
| Size for gestational age (%) | |||||
| Small (SGA) | 5.59 | 14.39 | 13.02 | 5.39 | 2.74 |
| Appropriate (AGA) | 86.93 | 77.29 | 81.35 | 82.62 | 83.12 |
| Large (LGA) | 7.48 | 8.32 | 5.63 | 11.98 | 14.13 |
| Observations per census tractc | |||||
| LGA versus AGA (mean (range)) | 3.0 (1, 38) | 3.5 (1, 61) | 3.7 (1, 52) | 3.9 (1, 87) | 1.7 (1, 21) |
| SGA versus AGA (mean (range)) | 3.4 (1, 45) | 3.8 (1, 62) | 4.0 (1, 59) | 3.6 (1, 79) | 1.7 (1, 21) |
| NDI (mean (SE))d | |||||
| 1 km | −0.56 (0.03) | 0.25 ( 0.03) | −0.61 (0.03) | 0.01 (0.03) | −0.07 (0.05) |
| 3 km | −0.58 (0.03) | 0.00 (0.02) | −0.62 (0.03) | −0.25 (0.02) | −0.24 (0.04) |
| 5 km | −0.61 (0.02) | −0.11 (0.02) | −0.64 (0.02) | −0.43 (0.02) | −0.36 (0.04) |
| 8 km | −0.66 (0.02) | −0.27 (0.02) | −0.66 (0.02) | −0.59 (0.02) | −0.49 (0.03) |
Oregon PRAMS respondents restricted to Portland Tri-County area residents with complete information on maternal age, race/ethnicity, parity, and health insurance status. Weighted estimates were corrected for complex survey sample design. Race categories included non-Hispanic White (White), non-Hispanic Black (Black), non-Hispanic Asian/Pacific Islander (Asian), and non-Hispanic American Indian/Alaska Native (Native American).
Unweighted frequency.
Mean and range of unweighted observations used to predict each outcome per census tract—LGA row includes women with LGA or AGA infants and SGA row includes women with SGA or AGA infants.
Neighborhood deprivation index was generated for 1-8 km radius circular buffers from sociodemographic variables from the 2000 Census.
The NDI was defined using the participant's residential address at the time she gave birth. The PRAMS survey did not include previous residences or a measure of duration of residence. In a sensitivity analysis, we repeated the multivariate multinomial regression in the sample of women who reported that they had not moved to a new address within 12 months before giving birth. The point estimates of this analysis were similar to those for the group overall, but imprecise because they relied on only about half of the total observations (data not shown). Strength of the adjusted association was our primary criterion for comparing buffer sizes. For example, if estimated effects of NDI measured within the 8 km buffer size were particularly strong, our findings would provide evidence that NDI may operate on a large scale, and that the 8 km buffer was suitable for measuring neighborhood deprivation. Simulation (Spielman and Yoo, 2009) and an empirical study (Lovasi, et al., 2008) suggest that model fit has minimal utility as a criterion for the most appropriate neighborhood definition. We present overall model fit as corroboration of these prior findings, but focus discussion on the strength of the adjusted association.
Results
Table 1 describes maternal, infant, and neighborhood characteristics in the population of 3,716 Oregon PRAMS respondents in the study area, stratified by race/ethnicity. Native American and Hispanic women had a higher proportion of LGA infants, and we observed an elevated prevalence of SGA among Black and Asian infants. Substantial racial and ethnic differences were observed in almost all individual-level socioeconomic position indicators. Regardless of buffer size, Black, Hispanic, and Native American mothers resided in more deprived areas than White and Asian mothers, although the range of NDI scores was similar across race and ethnic groups, particularly within larger buffer sizes.
NDI measures at each size buffer were correlated with one another, and the level of correlation between measurements decreased as the buffer size increased, presumably incorporating more heterogeneous areas (Table 2). Each buffer radius captured significantly different mean deprivation levels than the other buffer sizes (repeated measures ANOVA: overall p<0.0001; p<0.0001 for pairwise comparisons).
Table 2.
Partial Pearson correlation coefficients between NDI measured at each size buffer and repeated measures ANOVA results (N=3,716).a
| 1 km | 3 km | 5 km | 8 km | Mean NDI | |
|---|---|---|---|---|---|
| 1 km | 1 | 0.91 | 0.77 | 0.62 | −0.4066 |
| 3 km | 0.91 | 1 | 0.94 | 0.82 | −0.4873 |
| 5 km | 0.77 | 0.94 | 1 | 0.95 | −0.5526 |
| 8 km | 0.62 | 0.82 | 0.95 | 1 | −0.6271 |
ANOVA F-value=294.1, Huynh-Feldt Epsilon-adjusted p-value <0.0001. Estimates were corrected for sample weights. See Table 1 notes for data sources.
In multivariate analysis, neighborhood deprivation was strongly related to LGA among White women; this association was weaker among Native American and Hispanic women. These relationships are illustrated for the 3 km buffer in Figure 1. In contrast, Black women residing in high deprivation neighborhoods had lower odds of delivering a LGA infant. The adjusted odds ratios for SGA were smaller in magnitude than for LGA and not statistically significant.
Figure 1.
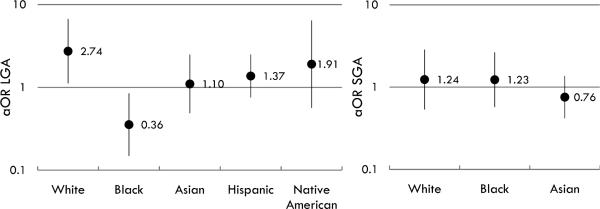
Adjusted odds of LGA (left) and SGA (right) for women living in high vs. low deprivation areas.
Notes: Adjusted odds of LGA (left) and SGA (right) for women living in high deprivation areas compared to low deprivation areas (Odds at 90th percentile of NDI/odds at 10th percentile of NDI) as measured by 3 km circular buffer. Adjusted for maternal age, education, parity, and insurance status and corrected for complex survey design. Error bars represent 95% confidence intervals. See Table 1 notes for data sources. Native American and Hispanic women are omitted for the SGA outcome due to limited sample size.
In general, estimates were similar in magnitude and direction for all buffer sizes. Within each race/ethnic group, the largest differences in the strength of association were generally observed between the 1 and 3 km buffers for LGA and between the 5 and 8 km buffers for SGA (Table 3). In some cases, there was a non-monotonic relationship between the continuous NDI and either outcome, but this generally did not change the overall study conclusions. In one exception, the negative association between NDI and LGA in Black women was only apparent at high levels of NDI. Differences in model fit (maximum adjusted pseudo R-square) among race/ethnic groups were much stronger than differences in model fit across neighborhood size.
Table 3.
Estimated race/ethnicity-specific associations between NDI and SGA or LGA [OR (95% CI)]a
| White (n=980) | Black (n=746) | Asian (n=925) | Hispanic (n=768) | Native American (n=247) | |
|---|---|---|---|---|---|
| 1 km | |||||
| SGA | |||||
| Hi/Low | 1.28 (0.52, 3.15) | 1.15 (0.50, 2.65) | 0.67 (0.37, 1.23) | — b | — b |
| Med/Low | 1.13 (0.64, 2.00) | 1.09 (0.50, 2.36) | 0.61 (0.42, 0.89) | ||
| LGA | |||||
| Hi/Low | 2.63 (1.01, 6.82) | 0.54 (0.21, 1.38) | 1.34 (0.57, 3.12) | 1.87 (0.74, 4.73) | 1.57 (0.47, 5.19) |
| Med/Low | 1.49 (0.85, 2.60) | 1.36 (0.54, 3.45) | 0.87 (0.50, 1.53) | 1.69 (0.65, 4.36) | 1.21 (0.73, 2.02) |
| R-squaredc | 0.2035 | 0.0345 | 0.0444 | 0.0670 | 0.0035 |
| 3 km | |||||
| SGA | |||||
| Hi/Low | 1.24 (0.53, 2.86) | 1.23 (0.57, 2.65) | 0.76 (0.42, 1.37) | — b | — b |
| Med/Low | 0.92 (0.49, 1.73) | 1.35 (0.73, 2.52) | 0.60 (0.39, 0.92) | ||
| LGA | |||||
| Hi/Low | 2.74 (1.12, 6.71) | 0.36 (0.15, 0.85) | 1.10 (0.49, 2.49) | 1.37 (0.76, 2.49) | 1.91 (0.57, 6.44) |
| Med/Low | 1.08 (0.60, 1.95) | 1.08 (0.47, 2.44) | 0.94 (0.51, 1.72) | 1.15 (0.88, 1.51) | 1.34 (0.77, 2.31) |
| R-squaredc | 0.2243 | 0.0318 | 0.0361 | 0.0555 | 0.0072 |
| 5 km | |||||
| SGA | |||||
| Hi/Low | 1.12 (0.52, 2.39) | 1.14 (0.51, 2.55) | 0.79 (0.45, 1.37) | — b | — b |
| Med/Low | 0.72 (0.39, 1.33) | 1.38 (0.71, 2.69) | 0.92 (0.64, 1.30) | ||
| LGA | |||||
| Hi/Low | 2.15 (0.96, 4.83) | 0.34 (0.15, 0.80) | 1.01 (0.44, 2.28) | 1.25 (0.70, 2.21) | 2.32 (0.72, 7.45) |
| Med/Low | 0.84 (0.47, 1.50) | 1.06 (0.51, 2.20) | 1.21 (0.74, 1.97) | 1.09 (0.87, 1.38) | 1.41 (0.88, 2.26) |
| R-squaredc | 0.2386 | 0.0372 | 0.0192 | 0.0530 | 0.0129 |
| 8 km | |||||
| SGA | |||||
| Hi/Low | 0.90 (0.42, 1.92) | 0.83 (0.42, 1.61) | 0.84 (0.46, 1.52) | — b | — b |
| Med/Low | 0.58 (0.34, 0.98) | 0.98 (0.58, 1.68) | 1.37 (0.90, 2.08) | ||
| LGA | |||||
| Hi/Low | 2.12 (0.94, 4.78) | 0.39 (0.17, 0.88) | 0.94 (0.40, 2.23) | 1.12 (0.64, 1.96) | 2.23 (0.75, 6.65) |
| Med/Low | 0.98 (0.57, 1.67) | 1.17 (0.61, 2.26) | 1.54 (0.90, 2.63) | 1.04 (0.85, 1.28) | 0.58 (0.25, 1.34) |
| R-squaredc | 0.2442 | 0.0370 | 0.0326 | 0.0512 | 0.0424 |
Race/ethnicity-stratified multinomial logistic regressions modeling size for gestational age (SGA and LGA compared to referent outcome AGA) as a function of continuous NDI, adjusted for confounders maternal age, education, insurance status, and parity, and corrected for complex survey design. NDI exhibited non-monotonic relationships with SGA and AGA. We calculated the OR for SGA and LGA at 90th vs. 10th percentile of NDI (Hi/Low) and 50th vs. 10th percentile of NDI (Med/Low) to show these relationships. See supplement Tables A2 – A5 for details on coefficients for all variables in each model. See Table 1 notes for data sources.
Limited observations of Native American and Hispanic women with SGA infants prevented estimation of the association with SGA for these groups. LGA estimates for the Native American and Hispanic groups are results of logistic regressions with outcome LGA vs. referent category AGA; confounders, OR construction, and survey design corrections are identical to those described in (a) above.
R2 is the change in maximum-adjusted pseudo R2 (R2 for full model – R2 for model with covariates only).
Discussion
In general, women living in high deprivation neighborhoods had greater odds of LGA and SGA deliveries than women living in low deprivation neighborhoods. However, high levels of neighborhood deprivation were associated with lower odds of LGA or smaller birth size in Black women. The magnitude and direction of the associations changed little from one buffer size to the next. There was substantial heterogeneity in model fit between race/ethnic groups, but little change in model fit between buffer sizes.
Estimated effects of neighborhood deprivation on SGA versus LGA
Neighborhood deprivation is hypothesized to affect maternal health through psychosocial factors and access to material resources. Neighborhood deprivation may induce psychosocial stress (Messer, et al., 2012a; Culhane and Elo, 2005), which can restrict fetal growth and development through unhealthy coping behaviors (Vinikoor-Imler, et al., 2011; Elo, et al., 2009; Metcalfe, et al., 2011; Messer, et al., 2012a) or increase susceptibility to infection (Wadhwa, et al., 2011; Culhane, et al., 2001; Lu and Halfon, 2003). We found weaker associations with SGA than LGA and NDI. However, the magnitude of the associations we observed with SGA was similar to existing literature on neighborhood socioeconomic measures and SGA in other regions of the United States (Elo, et al., 2009; Masi, et al., 2007; Zeka, et al., 2008) and in the Netherlands (Agyemang, et al., 2009). Adjusted odds ratio estimates from these studies ranged from 1.05 (for a 1 SD increase in neighborhood economic disadvantage index) (Masi, et al., 2007) to 1.93 (comparing the highest and lowest quartiles of neighborhood income) (Agyemang, et al., 2009), which were similar to the associations we observed comparing odds of SGA at high and low levels of NDI.
We found that greater neighborhood deprivation was associated with higher odds of LGA for most groups in our population. The lack of studies on LGA and neighborhood deprivation prevents comparison of our results for this outcome to other study populations, but a positive association is consistent with the theory that neighborhood deprivation might promote obesity and lead to LGA. Pathways leading to LGA may include lack of access to nutritious food or opportunities for exercise in disadvantaged neighborhoods (Diez Roux and Mair, 2010; Schempf, et al., 2009; Daniel, et al., 2008; Culhane and Elo, 2005), creating environments that promote obesity and diabetes (Vinikoor-Imler, et al., 2011; Elo, et al., 2009; Metcalfe, et al., 2011), which in turn contribute to accelerated fetal growth (Yessoufou and Moutairou, 2011; Boney, et al., 2005; Janghorbani, et al., 2006; Clausen, et al., 2006; Baptiste-Roberts, et al., 2012; Lu, et al., 2001).
Variation in associations across race and ethnic groups
We found variation in associations between neighborhood deprivation and SGA and LGA across race/ethnic groups. This finding is consistent with prior research reporting racial and ethnic differences in associations between built environment characteristics and pregnancy outcomes (Buka, et al., 2003; Vinikoor-Imler, et al., 2011; Love, et al., 2010; Janevic, et al., 2010; O'Campo, et al., 2008; Messer, et al., 2012b).
In particular, the inverse association between neighborhood deprivation and LGA in Black women likely reflected well-documented smaller birth size in Black women (Hogan, et al., 2012; Lu and Halfon, 2003; Blumenshine, et al., 2010; Geronimus, 1996; Collins, et al., 2004; Giscombe and Lobel, 2005). Notably, the negative association between neighborhood deprivation and LGA was only observed at high levels of neighborhood deprivation; odds of LGA at median deprivation compared to low deprivation was near the null value among black women. Chronic psychosocial stress may play an important role in risk of fetal growth restriction for Black women living in high deprivation neighborhoods, which is consistent with the traditional focus on stress as an underlying mechanism restricting fetal growth (Entringer, et al., 2012). Exposure to chronic stress and mothers’ perception of their residential environment has been linked to very low birthweight in a population of Black women (Collins, et al., 1998). Chronic stress can have a cumulative effect on physiologic systems over the life course above and beyond effects of acute stressors (Giscombe and Lobel, 2005; Wadhwa, et al., 2011; Geronimus, et al., 2006). This is theorized to be one cause of smaller birth size in Black women, who may experience persistent stress due to intrapersonal/personal, and institutional racism (Wadhwa, et al., 2011; Giscombe and Lobel, 2005; Mendez, et al., 2012; Geronimus, 1996). We theorize that stress due to neighborhood deprivation may have a stronger effect on fetal growth restriction among Black women due to the cumulative effects of multiple sources of chronic stress.
We found positive associations between NDI and LGA in Hispanic and Native American women, but both were smaller in magnitude than for White women. Hispanic and Native American populations have increased prevalence of obesity, diabetes and other risk factors for LGA (Rodrigues, et al., 2000; Wassimi, et al., 2011; Dyer, et al., 2007; Homko, et al., 1995). We did not control for these other risk factors because they could stem from environmental causes (Schempf, et al., 2009; Vinikoor-Imler, et al., 2011; Messer, et al., 2012b), but these more proximal risk factors may play a greater role in LGA for Hispanic or Native American women than in White women.
Sensitivity of associations to neighborhood size
The validity of estimated neighborhood effects on birth outcomes depends on the extent to which neighborhood exposures are measured within relevant neighborhood boundaries (Coulton, et al., 2012; Diez Roux, 2007; Spielman and Yoo, 2009; Daniel, et al., 2008; Soobader, et al., 2006; Flowerdew, et al., 2008). Inconsistent neighborhood definitions can lead to inconsistent findings across studies and spurious associations (Spielman and Yoo, 2009). Overall, we found minimal differences in the association between neighborhood deprivation and either outcome across buffer sizes. The buffer size producing the strongest or weakest association varied across race/ethnic groups and outcomes, but conclusions did not depend greatly on the size of the neighborhood buffer. That is, strong relationships remained so regardless of buffer size, and weaker associations were near the null for all neighborhood buffers. Previous studies have found inconsistent relationships between birth outcomes and neighborhood deprivation at varying administrative boundaries (e.g., zip codes, census tracts) (Subramanian, et al., 2006; Krieger, et al., 2003; Messer, et al., 2012b). Compared to administrative boundaries, proximity-based measures like circular buffers are more consistent with the theorized importance of distance to health-related resources such as tobacco or food retail outlets (Block, et al., 2011; Reitzel, et al., 2011).
The geographic area of the study included urban, suburban, and urban fringe areas, likely characterized by differential access to resources. The effective neighborhood size may be different across locations within our study or in other cities due to heterogeneity in built and social neighborhood characteristics and in common transit modes, both of which determine access to resources (Spielman and Yoo, 2009; Culhane and Elo, 2005; Messer, et al., 2006a). It may have been more appropriate to use a 3 km buffer for women residing in urban core areas and the 5 km or 8 km buffer in less urban areas, but our study lacked sufficient sample size within geographic strata to examine such differences. Likewise, one could base the buffer size on access to transit that would increase the area easily accessible to an individual.
Furthermore, effective neighborhood size may vary across population subgroups within a given geographic location. We theorized that neighborhoods with higher deprivation may have more obesity-promoting resources such as food retailers providing affordable, energy dense foods (e.g., fast food restaurants) (Larson, et al., 2009; Walker, et al., 2010) or fewer health-promoting resources such as parks (Estabrooks, et al., 2003). Yet, access to such resources may differ across race, due to economic or social barriers to access. As an extreme example, undocumented immigrants were not allowed to hold a drivers license in Oregon during the study period. This restriction limited transportation options for certain populations, and it might be appropriate to use a smaller buffer size for these groups than others. Individual heterogeneity in effective area size can bias the association toward the null (Spielman and Yoo, 2009), indicating that use of standard neighborhood definitions may under-estimate the strength of the relationships between neighborhood deprivation and size for gestational age. We explored differences in model fit at each neighborhood size. As in a simulation study (Spielman and Yoo, 2009) and a previous empirical study (Lovasi, et al., 2008), buffer size had little impact on model fit. Furthermore, model fit for White women was much higher than for minority race/ethnic groups (Table 3). These differences were considerably larger than the differences in model fit due to neighborhood size, and the R-squared values for the minority groups were very low. The relatively small proportion of explained variance is consistent with limited understanding of the causes of adverse birth outcomes, especially among minority populations (Giscombe and Lobel, 2005).
Strengths and Limitations
This study had several strengths and limitations. Cross-sectional data and limited information on duration of residence limited our ability to make causal inferences about the effects of neighborhood deprivation on birth size. Moreover, life-long residence in low-income neighborhoods may have a stronger effect on birth outcomes than residence in a low-income neighborhood at one point in time (Collins, et al., 2009), but the present study was limited to neighborhood information at the time a woman gave birth. However, sensitivity analysis restricted to women who had not moved in the year before giving birth yielded results similar to those in the full study population. Our buffer-based NDI measures did not take into account racial residential segregation or characteristics of neighborhoods that are nearby but beyond the buffer radius. The NDI measures were estimated from census tract-level data; yet, in the study area, buffers were large relative to the census tracts. Further, buffer-based measures were weighted according to the area within each buffer and enabled the first investigation of neighborhood deprivation within varying proximities of residential locations.
Our study presented estimated odds ratios although for some race/ethnic groups the prevalence of the outcome was greater than the 10% threshold where the odds ratio may no longer approximate relative risk. Relative risks estimated using proc genmod with a Poisson distribution and log link were similar in magnitude to the odds ratios we present here (data not shown). We presented the odds ratios because the survey procedure provided variance estimates that more appropriately accounted for complex survey design and the multinomial outcome, and the estimated odds ratios were very similar in magnitude to the estimated relative risk.
Small numbers in minority race/ethnic groups limited the precision of our estimates. Specific ethnicity and maternal nativity would enable assessment of our research questions in more homogeneous groups, but were not recorded in Oregon PRAMS. However, the diversity present in the available sample and the stratified analysis were important strengths of this study. By comparing estimates generated using a variety of neighborhood sizes, this study also contributes information about the sensitivity of associations between neighborhood environments and birth outcomes to neighborhood size. Lastly, we explored neighborhood deprivation as a predictor of LGA, which is an often-overlooked but increasingly relevant outcome.
Conclusion
High neighborhood deprivation is associated with higher odds of both SGA and LGA in most race/ethnic groups. Conclusions drawn from this study did not differ substantially for any neighborhood size. Future studies of neighborhood deprivation and LGA would be helpful to understand race/ethnic variation in this relationship. Studies of other more specific contextual factors in addition to neighborhood deprivation could explain some of the heterogeneity in effect size between racial and ethnic groups or suggest more specific pathways. Furthermore, investigation of heterogeneity in buffer size for different levels of urbanicity and different racial and ethnic groups is needed to accurately measure relevant neighborhood exposures in diverse populations.
Supplementary Material
Highlights.
-
1.)
Large birth size is increasingly relevant but overlooked in neighborhood research.
-
2.)
We estimated neighborhood effects on large & small birth size in a population survey.
-
3.)
Neighborhood deprivation is associated with accelerated and restricted fetal growth.
-
4.)
1-8 km radius circular buffer neighborhoods yielded similar measures of association.
Acknowledgements
This research was supported by funding from Collins Medical Trust and a Building Interdisciplinary Research Careers in Women's Health (BIRCWH) career development award (K12HD043488). The authors would like to thank Dr. Kenneth D. Rosenberg and Mr. Alfredo Sandoval at the Oregon Health Authority (OHA) for their assistance with Oregon PRAMS data access and linkage and OHA Oregon Center for Health Statistics for approving this study. We appreciate technical Geographic Information System and research support from Ashley Howell and Sam Hermes, and thank Sheila Markwardt for excellent research assistance.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agyemang C, Vrijkotte TG, Droomers M, van der Wal MF, Bonsel GJ, Stronks K. The effect of neighbourhood income and deprivation on pregnancy outcomes in Amsterdam, The Netherlands. Journal of Epidemiology & Community Health. 2009;63:755–760. doi: 10.1136/jech.2008.080408. doi: 10.1136/jech.2008.080408. [DOI] [PubMed] [Google Scholar]
- Auchincloss AH, Diez Roux AV, Brown DG, Erdmann CA, Bertoni AG. Neighborhood resources for physical activity and healthy foods and their association with insulin resistance. Epidemiology. 2008;19:146–157. doi: 10.1097/EDE.0b013e31815c480. doi: 10.1097/EDE.0b013e31815c480. [DOI] [PubMed] [Google Scholar]
- Auger N, Park AL, Daniel M. Contribution of local area deprivation to cultural-linguistic inequalities in foetal growth restriction: trends over time in a Canadian metropolitan centre. Health & Place. 2013;22:38–47. doi: 10.1016/j.healthplace.2013.03.003. doi: 10.1016/j.healthplace.2013.03.003. [DOI] [PubMed] [Google Scholar]
- Baptiste-Roberts K, Nicholson WK, Wang NY, Brancati FL. Gestational diabetes and subsequent growth patterns of offspring: the National Collaborative Perinatal Project. Maternal and Child Health Journal. 2012;16:125–132. doi: 10.1007/s10995-011-0756-2. doi: 10.1007/s10995-011-0756-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker DJ. Fetal origins of coronary heart disease. BMJ. 1995;311:171–174. doi: 10.1136/bmj.311.6998.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker DJP, Thornburg KL. The obstetric origins of health for a lifetime. Clinical obstetrics and gynecology. 2013;56:511–519. doi: 10.1097/GRF.0b013e31829cb9ca. [DOI] [PubMed] [Google Scholar]
- Beard JR, Lincoln D, Donoghue D, Taylor D, Summerhayes R, Dunn TM, Earnest A, Morgan G. Socioeconomic and maternal determinants of small-for-gestational age births: patterns of increasing disparity. Acta Obstetricia et Gynecologica Scandinavica. 2009;88:575–583. doi: 10.1080/00016340902818170. doi: 10.1080/00016340902818170. [DOI] [PubMed] [Google Scholar]
- Bell JA, Hamer M, Shankar A. Gender-specific associations of objective and perceived neighborhood characteristics with body mass index and waist circumference among older adults in the english longitudinal study of ageing. American Journal of Public Health. 2014;104:1279–1286. doi: 10.2105/AJPH.2014.301947. doi: 10.2105/AJPH.2014.301947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block JP, Christakis NA, O'Malley AJ, Subramanian SV. Proximity to food establishments and body mass index in the Framingham Heart Study offspring cohort over 30 years. American Journal of Epidemiology. 2011;174:1108–1114. doi: 10.1093/aje/kwr244. doi: 10.1093/aje/kwr244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenshine P, Egerter S, Barclay CJ, Cubbin C, Braveman PA. Socioeconomic disparities in adverse birth outcomes: a systematic review. American Journal of Preventive Medicine. 2010;39:263–272. doi: 10.1016/j.amepre.2010.05.012. doi: 10.1016/j.amepre.2010.05.012. [DOI] [PubMed] [Google Scholar]
- Bocca-Tjeertes IF, Kerstjens JM, Reijneveld SA, Veldman K, Bos AF, de Winter AF. Growth patterns of large for gestational age children up to age 4 years. Pediatrics. 2014;133:e643–9. doi: 10.1542/peds.2013-0985. doi: 10.1542/peds.2013-0985. [DOI] [PubMed] [Google Scholar]
- Boney CM, Verma A, Tucker R, Vohr BR. Metabolic syndrome in childhood: association with birth weight, maternal obesity, and gestational diabetes mellitus. Pediatrics. 2005;115:e290–6. doi: 10.1542/peds.2004-1808. doi: 10.1542/peds.2004-1808. [DOI] [PubMed] [Google Scholar]
- Boone-Heinonen J, Popkin BM, Song Y, Gordon-Larsen P. What neighborhood area captures built environment features related to adolescent physical activity? Health & Place. 2010;16:1280–1286. doi: 10.1016/j.healthplace.2010.06.015. doi: 10.1016/j.healthplace.2010.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowers K, Laughon SK, Kiely M, Brite J, Chen Z, Zhang C. Gestational diabetes, pre-pregnancy obesity and pregnancy weight gain in relation to excess fetal growth: variations by race/ethnicity. Diabetologia. 2013;56:1263–1271. doi: 10.1007/s00125-013-2881-5. doi: 10.1007/s00125-013-2881-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buka SL, Brennan RT, Rich-Edwards JW, Raudenbush SW, Earls F. Neighborhood support and the birth weight of urban infants. American Journal of Epidemiology. 2003;157:1–8. doi: 10.1093/aje/kwf170. doi: 10.1093/aje/kwf170. [DOI] [PubMed] [Google Scholar]
- Clausen T, Oyen N, Henriksen T. Pregnancy complications by overweight and residential area. A prospective study of an urban Norwegian cohort. Acta Obstetricia et Gynecologica Scandinavica. 2006;85:526–533. doi: 10.1080/00016340500523644. doi: 10.1080/00016340500523644. [DOI] [PubMed] [Google Scholar]
- Collins JW, Jr, David RJ, Handler A, Wall S, Andes S. Very low birthweight in African American infants: the role of maternal exposure to interpersonal racial discrimination. American Journal of Public Health. 2004;94:2132–2138. doi: 10.2105/ajph.94.12.2132. doi: 10.2105/AJPH.94.12.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins JW, Jr, David RJ, Symons R, Handler A, Wall S, Andes S. African-American mothers' perception of their residential environment, stressful life events, and very low birthweight. Epidemiology. 1998;9:286–289. doi: 10.1097/00001648-199805000-00012. [PubMed] [Google Scholar]
- Collins JW, Jr, Wambach J, David RJ, Rankin KM. Women's lifelong exposure to neighborhood poverty and low birth weight: a population-based study. Maternal and Child Health Journal. 2009;13:326–333. doi: 10.1007/s10995-008-0354-0. doi: 10.1007/s10995-008-0354-0. [DOI] [PubMed] [Google Scholar]
- Coulton CJ, Jennings MZ, Chan T. How Big is My Neighborhood? Individual and Contextual Effects on Perceptions of Neighborhood Scale. American Journal of Community Psychology. 2012;51:140–50. doi: 10.1007/s10464-012-9550-6. doi: 10.1007/s10464-012-9550-6. [DOI] [PubMed] [Google Scholar]
- Cubbin C, Marchi K, Lin M, Bell T, Marshall H, Miller C, Braveman P. Is neighborhood deprivation independently associated with maternal and infant health? Evidence from Florida and Washington. Maternal and Child Health Journal. 2008;12:61–74. doi: 10.1007/s10995-007-0225-0. doi: 10.1007/s10995-007-0225-0. [DOI] [PubMed] [Google Scholar]
- Culhane JF, Elo IT. Neighborhood context and reproductive health. American Journal of Obstetrics and Gynecology. 2005;192:S22–9. doi: 10.1016/j.ajog.2005.01.071. doi: 10.1016/j.ajog.2005.01.071. [DOI] [PubMed] [Google Scholar]
- Culhane JF, Rauh V, McCollum KF, Hogan VK, Agnew K, Wadhwa PD. Maternal stress is associated with bacterial vaginosis in human pregnancy. Maternal and Child Health Journal. 2001;5:127–134. doi: 10.1023/a:1011305300690. doi: 10.1023/A:1011305300690. [DOI] [PubMed] [Google Scholar]
- Daniel M, Moore S, Kestens Y. Framing the biosocial pathways underlying associations between place and cardiometabolic disease. Health & Place. 2008;14:117–132. doi: 10.1016/j.healthplace.2007.05.003. doi: 10.1016/j.healthplace.2007.05.003. [DOI] [PubMed] [Google Scholar]
- Diez Roux AV. Neighborhoods and health: Where are we and were do we go from here? Revue d'Epidemiologie et de Sante Publique. 2007;55:13–21. doi: 10.1016/j.respe.2006.12.003. doi: 10.1016/j.respe.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux AV, Mair C. Neighborhoods and health. Annals of the New York Academy of Sciences. 2010;1186:125–145. doi: 10.1111/j.1749-6632.2009.05333.x. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- Dyer JS, Rosenfeld CR, Rice J, Rice M, Hardin DS. Insulin resistance in Hispanic large-for-gestational-age neonates at birth. Journal of Clinical Endocrinology and Metabolism. 2007;92:3836–3843. doi: 10.1210/jc.2007-0079. doi: 10.1210/jc.2007-0079. [DOI] [PubMed] [Google Scholar]
- Elo IT, Culhane JF, Kohler IV, O'Campo P, Burke JG, Messer LC, Kaufman JS, Laraia BA, Eyster J, Holzman C. Neighbourhood deprivation and small-for-gestational-age term births in the United States. Paediatric and Perinatal Epidemiology. 2009;23:87–96. doi: 10.1111/j.1365-3016.2008.00991.x. doi: 10.1111/j.1365-3016.2008.00991.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Entringer S, Buss C, Swanson JM, Cooper DM, Wing DA, Waffarn F, Wadhwa PD. Fetal programming of body composition, obesity, and metabolic function: the role of intrauterine stress and stress biology. Journal of Nutrition and Metabolism. 2012;2012:632548. doi: 10.1155/2012/632548. doi: 10.1155/2012/632548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estabrooks PA, Lee RE, Gyurcsik NC. Resources for physical activity participation: Does availability and accessibility differ by neighborhood socioeconomic status? Annals of Behavioral Medicine. 2003;25:100–104. doi: 10.1207/S15324796ABM2502_05. doi: 10.1207/S15324796ABM2502_05. [DOI] [PubMed] [Google Scholar]
- Farley TA, Mason K, Rice J, Habel JD, Scribner R, Cohen DA. The relationship between the neighbourhood environment and adverse birth outcomes. Paediatric and Perinatal Epidemiology. 2006;20:188–200. doi: 10.1111/j.1365-3016.2006.00719.x. doi: 10.1111/j.1365-3016.2006.00719.x. [DOI] [PubMed] [Google Scholar]
- Flowerdew R, Manley DJ, Sabel CE. Neighbourhood effects on health: Does it matter where you draw the boundaries? Social Science & Medicine. 2008;66:1241–1255. doi: 10.1016/j.socscimed.2007.11.042. doi: 10.1016/j.socscimed.2007.11.042. [DOI] [PubMed] [Google Scholar]
- Garcia-Subirats I, Perez G, Rodriguez-Sanz M, Ruiz-Munoz D, Salvador J. Neighborhood inequalities in adverse pregnancy outcomes in an urban setting in Spain: a multilevel approach. Journal of Urban Health. 2012;89:447–463. doi: 10.1007/s11524-011-9648-4. doi: 10.1007/s11524-011-9648-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus AT. Black/white differences in the relationship of maternal age to birthweight: a population-based test of the weathering hypothesis. Social Science & Medicine. 1996;42:589–597. doi: 10.1016/0277-9536(95)00159-x. doi: 10.1016/0277-9536(95)00159-X. [DOI] [PubMed] [Google Scholar]
- Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among Blacks and Whites in the United States. American Journal of Public Health. 2006;96:826–833. doi: 10.2105/AJPH.2004.060749. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giscombe CL, Lobel M. Explaining disproportionately high rates of adverse birth outcomes among African Americans: the impact of stress, racism, and related factors in pregnancy. Psychological Bulletin. 2005;131:662–683. doi: 10.1037/0033-2909.131.5.662. doi: 10.1037/0033-2909.131.5.662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray-Donald K. Does being born big confer advantages? Canadian Medical Association Journal. 2011;183:295–296. doi: 10.1503/cmaj.101700. doi: 10.1503/cmaj.101700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadlock FP, Harrist RB, Martinez-Poyer J. In utero analysis of fetal growth: a sonographic weight standard. Radiology. 1991;181:129–133. doi: 10.1148/radiology.181.1.1887021. doi: 10.1148/radiology.181.1.1887021. [DOI] [PubMed] [Google Scholar]
- Hoffman CS, Messer LC, Mendola P, Savitz DA, Herring AH, Hartmann KE. Comparison of gestational age at birth based on last menstrual period and ultrasound during the first trimester. Paediatric and Perinatal Epidemiology. 2008;22:587–596. doi: 10.1111/j.1365-3016.2008.00965.x. doi: 10.1111/j.1365-3016.2008.00965.x. [DOI] [PubMed] [Google Scholar]
- Hogan VK, Njoroge T, Durant TM, Ferre CD. Eliminating disparities in perinatal outcomes--lessons learned. Maternal and Child Health Journal. 2001;5:135–140. doi: 10.1023/a:1011357317528. doi: 10.1023/A:1011357317528. [DOI] [PubMed] [Google Scholar]
- Hogan VK, Rowley D, Bennett T, Taylor KD. Life course, social determinants, and health inequities: toward a national plan for achieving health equity for African American infants--a concept paper. Maternal and Child Health Journal. 2012;16:1143–1150. doi: 10.1007/s10995-011-0847-0. doi: 10.1007/s10995-011-0847-0. [DOI] [PubMed] [Google Scholar]
- Homko CJ, Sivan E, Nyirjesy P, Reece EA. The interrelationship between ethnicity and gestational diabetes in fetal macrosomia. Diabetes Care. 1995;18:1442–1445. doi: 10.2337/diacare.18.11.1442. doi: 10.2337/diacare.18.11.1442. [DOI] [PubMed] [Google Scholar]
- Hutcheon JA, Zhang X, Platt RW, Cnattingius S, Kramer MS. The case against customised birthweight standards. Paediatric and Perinatal Epidemiology. 2011;25:11–16. doi: 10.1111/j.1365-3016.2010.01155.x. doi: 10.1111/j.1365-3016.2010.01155.x. [DOI] [PubMed] [Google Scholar]
- Janevic T, Stein CR, Savitz DA, Kaufman JS, Mason SM, Herring AH. Neighborhood deprivation and adverse birth outcomes among diverse ethnic groups. Annals of Epidemiology. 2010;20:445–451. doi: 10.1016/j.annepidem.2010.02.010. doi: 10.1016/j.annepidem.2010.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janghorbani M, Stenhouse EA, Jones RB, Millward BA. Is neighbourhood deprivation a risk factor for gestational diabetes mellitus? Diabetic Medicine. 2006;23:313–317. doi: 10.1111/j.1464-5491.2006.01774.x. doi: 10.1111/j.1464-5491.2006.01774.x. [DOI] [PubMed] [Google Scholar]
- Kaufman JS, Cooper RS, McGee DL. Socioeconomic status and health in blacks and whites: the problem of residual confounding and the resiliency of race. Epidemiology. 1997;8:621–628. doi: 10.1097/00001648-199710000-00002. [PubMed] [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Choosing area based socioeconomic measures to monitor social inequalities in low birth weight and childhood lead poisoning: The Public Health Disparities Geocoding Project (US). Journal of Epidemiology & Community Health. 2003;57:186–199. doi: 10.1136/jech.57.3.186. doi: 10.1136/jech.57.3.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the U.S. American Journal of Preventive Medicine. 2009;36:74–81. doi: 10.1016/j.amepre.2008.09.025. doi: 10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- Lazariu V, Davis CF, McNutt L- Comparison of two measures of gestational age among low income births. The potential impact on health studies, New York, 2005. Maternal and Child Health Journal. 2013;17:42–48. doi: 10.1007/s10995-012-0944-8. doi: 10.1007/s10995-012-0944-8. [DOI] [PubMed] [Google Scholar]
- Leung CW, Laraia BA, Kelly M, Nickleach D, Adler NE, Kushi LH, Yen IH. The influence of neighborhood food stores on change in young girls’ body mass index. American Journal of Preventive Medicine. 2011;41:43–51. doi: 10.1016/j.amepre.2011.03.013. doi: 10.1016/j.amepre.2011.03.013 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovasi GS, Moudon AV, Smith NL, Lumley T, Larson EB, Sohn DW, Siscovick DS, Psaty BM. Evaluating options for measurement of neighborhood socioeconomic context: evidence from a myocardial infarction case-control study. Health & Place. 2008;14:453–467. doi: 10.1016/j.healthplace.2007.09.004. doi: 10.1016/j.healthplace.2007.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Love C, David RJ, Rankin KM, Collins JW. Exploring weathering: effects of lifelong economic environment and maternal age on low birth weight, small for gestational age, and preterm birth in African-American and white women. American Journal of Epidemiology. 2010;172:127–134. doi: 10.1093/aje/kwq109. doi: 10.1093/aje/kwq109. [DOI] [PubMed] [Google Scholar]
- Lu GC, Rouse DJ, DuBard M, Cliver S, Kimberlin D, Hauth JC. The effect of the increasing prevalence of maternal obesity on perinatal morbidity. American Journal of Obstetrics and Gynecology. 2001;185:845–849. doi: 10.1067/mob.2001.117351. doi: 10.1067/mob.2001.117351. [DOI] [PubMed] [Google Scholar]
- Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: a life-course perspective. Maternal and Child Health Journal. 2003;7:13–30. doi: 10.1023/a:1022537516969. doi: 10.1023/A:1022537516969. [DOI] [PubMed] [Google Scholar]
- Lund H. Reasons for living in a transit-oriented development, and associated transit use. Journal of the American Planning Association. 2006;72:357–366. doi: 10.1080/01944360608976757. [Google Scholar]
- Masi CM, Hawkley LC, Piotrowski ZH, Pickett KE. Neighborhood economic disadvantage, violent crime, group density, and pregnancy outcomes in a diverse, urban population. Social Science & Medicine. 2007;65:2440–2457. doi: 10.1016/j.socscimed.2007.07.014. doi: 10.1016/j.socscimed.2007.07.014. [DOI] [PubMed] [Google Scholar]
- Mendez DD, Hogan VK, Culhane JF. Stress during Pregnancy: The Role of Institutional Racism. Stress and Health. 2012;29:266–274. doi: 10.1002/smi.2462. doi: 10.1002/smi.2462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messer LC, Kaufman JS, Dole N, Herring A, Laraia BA. Violent crime exposure classification and adverse birth outcomes: a geographically-defined cohort study. International Journal of Health Geographics. 2006a;5:22. doi: 10.1186/1476-072X-5-22. doi: 10.1186/1476-072X-5-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messer LC, Laraia BA, Kaufman JS, Eyster J, Holzman C, Culhane J, Elo I, Burke JG, O'Campo P. The development of a standardized neighborhood deprivation index. Journal of Urban Health. 2006b;83:1041–1062. doi: 10.1007/s11524-006-9094-x. doi: 10.1007/s11524-006-9094-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messer LC, Maxson P, Miranda ML. The urban built environment and associations with women's psychosocial health. Journal of Urban Health. 2012a;90:857–871. doi: 10.1007/s11524-012-9743-1. doi: 10.1007/s11524-012-9743-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messer LC, Vinikoor-Imler LC, Laraia BA. Conceptualizing neighborhood space: consistency and variation of associations for neighborhood factors and pregnancy health across multiple neighborhood units. Health & Place. 2012b;18:805–813. doi: 10.1016/j.healthplace.2012.03.012. doi: 10.1016/j.healthplace.2012.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messer LC, Vinikoor-Imler LC, Laraia BA, Kaufman JS, Eyster J, Holzman C, Culhane J, Elo I, Burke JG, O'Campo P. Socioeconomic domains and associations with preterm birth. Social Science & Medicine. 2008;67:1247–1257. doi: 10.1016/j.socscimed.2008.06.009. doi: 10.1016/j.socscimed.2008.06.009. [DOI] [PubMed] [Google Scholar]
- Metcalfe A, Lail P, Ghali WA, Sauve RS. The association between neighbourhoods and adverse birth outcomes: a systematic review and meta-analysis of multi-level studies. Paediatric and Perinatal Epidemiology. 2011;25:236–245. doi: 10.1111/j.1365-3016.2011.01192.x. doi: 10.1111/j.1365-3016.2011.01192.x. [DOI] [PubMed] [Google Scholar]
- Moore GS, Kneitel AW, Walker CK, Gilbert WM, Xing G. Autism risk in small-and large-for-gestational-age infants. American Journal of Obstetrics and Gynecology. 2012;206:314.e1–314.e9. doi: 10.1016/j.ajog.2012.01.044. doi: 10.1016/j.ajog.2012.01.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustafa G, David RJ. Comparative accuracy of clinical estimate versus menstrual gestational age in computerized birth certificates. Public Health Reports. 2001;116:15–21. doi: 10.1093/phr/116.1.15. doi: 10.1016/S0033-3549(04)50018-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nkansah-Amankra S, Luchok KJ, Hussey JR, Watkins K, Liu X. Effects of maternal stress on low birth weight and preterm birth outcomes across neighborhoods of South Carolina, 2000-2003. Maternal and Child Health Journal. 2010;14:215–226. doi: 10.1007/s10995-009-0447-4. doi: 10.1007/s10995-009-0447-4. [DOI] [PubMed] [Google Scholar]
- O'Campo P, Burke JG, Culhane J, Elo IT, Eyster J, Holzman C, Messer LC, Kaufman JS, Laraia BA. Neighborhood deprivation and preterm birth among non-Hispanic Black and White women in eight geographic areas in the United States. American Journal of Epidemiology. 2008;167:155–163. doi: 10.1093/aje/kwm277. doi: 10.1093/aje/kwm277. [DOI] [PubMed] [Google Scholar]
- Pearson AL, Bentham G, Day P, Kingham S. Associations between neighbourhood environmental characteristics and obesity and related behaviours among adult New Zealanders. BMC Public Health. 2014;14:553–2458-14-553. doi: 10.1186/1471-2458-14-553. doi: 10.1186/1471-2458-14-553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin C, Hsia J, Berg CJ. Variation between last-menstrual-period and clinical estimates of gestational age in vital records. American Journal of Epidemiology. 2008;167:646–652. doi: 10.1093/aje/kwm345. doi: 10.1093/aje/kwm345. [DOI] [PubMed] [Google Scholar]
- Reitzel LR, Cromley EK, Li Y, Cao Y, Dela Mater R, Mazas CA, Cofta-Woerpel L, Cinciripini PM, Wetter DW. The effect of tobacco outlet density and proximity on smoking cessation. American Journal of Public Health. 2011;101:315–320. doi: 10.2105/AJPH.2010.191676. doi: 10.2105/AJPH.2010.191676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodrigues S, Robinson EJ, Kramer MS, Gray-Donald K. High rates of infant macrosomia: a comparison of a Canadian native and a non-native population. Journal of Nutrition. 2000;130:806–812. doi: 10.1093/jn/130.4.806. [DOI] [PubMed] [Google Scholar]
- Sampson RJ, Sharkey P. Neighborhood selection and the social reproduction of concentrated racial inequality. Demography. 2008;45:1–29. doi: 10.1353/dem.2008.0012. doi: 10.1353/dem.2008.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schempf A, Strobino D, O'Campo P. Neighborhood effects on birthweight: an exploration of psychosocial and behavioral pathways in Baltimore, 1995--1996. Social Science & Medicine. 2009;68:100–110. doi: 10.1016/j.socscimed.2008.10.006. doi: 10.1016/j.socscimed.2008.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schempf AH, Kaufman JS, Messer LC, Mendola P. The neighborhood contribution to black-white perinatal disparities: an example from two North Carolina counties, 1999-2001. American Journal of Epidemiology. 2011;174:744–752. doi: 10.1093/aje/kwr128. doi: 10.1093/aje/kwr128. [DOI] [PubMed] [Google Scholar]
- Simon CJ, Tamura R. Do higher rents discourage fertility? Evidence from U.S. cities, 1940-2000. Regional Science and Urban Economics. 2009;39:33–42. doi: 10.1016/j.regsciurbeco.2008.08.002. [Google Scholar]
- Soobader M, Cubbin C, Gee GC, Rosenbaum A, Laurenson J. Levels of analysis for the study of environmental health disparities. Environmental research. 2006;102:172–180. doi: 10.1016/j.envres.2006.05.001. doi: 10.1016/j.envres.2006.05.001. [DOI] [PubMed] [Google Scholar]
- Spielman SE, Yoo EH. The spatial dimensions of neighborhood effects. Social Science & Medicine. 2009;68:1098–1105. doi: 10.1016/j.socscimed.2008.12.048. doi: 10.1016/j.socscimed.2008.12.048. [DOI] [PubMed] [Google Scholar]
- Subramanian SV, Chen JT, Rehkopf DH, Waterman PD, Krieger N. Comparing individual- and area-based socioeconomic measures for the surveillance of health disparities: A multilevel analysis of Massachusetts births, 1989-1991. American Journal of Epidemiology. 2006;164:823–834. doi: 10.1093/aje/kwj313. doi: 10.1093/aje/kwj313. [DOI] [PubMed] [Google Scholar]
- Sundquist J, Sundquist K, Johansson SE, Li X, Winkleby M. Mothers, places and small for gestational age births: a cohort study. Archives of Disease in Childhood. 2011;96:380–385. doi: 10.1136/adc.2009.180042. doi: 10.1136/adc.2009.180042. [DOI] [PubMed] [Google Scholar]
- Tumen S. Fertility decisions and endogenous residential sorting. Regional Science and Urban Economics. 2012;42:78–87. doi: 10.1016/j.regsciurbeco.2011.07.001. [Google Scholar]
- Urquia ML, Frank JW, Glazier RH, Moineddin R, Matheson FI, Gagnon AJ. Neighborhood context and infant birthweight among recent immigrant mothers: a multilevel analysis. American Journal of Public Health. 2009;99:285–293. doi: 10.2105/AJPH.2007.127498. doi: 10.2105/AJPH.2007.127498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinikoor-Imler LC, Messer LC, Evenson KR, Laraia BA. Neighborhood conditions are associated with maternal health behaviors and pregnancy outcomes. Social Science & Medicine. 2011;73:1302–1311. doi: 10.1016/j.socscimed.2011.08.012. doi: 10.1016/j.socscimed.2011.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadhwa PD, Entringer S, Buss C, Lu MC. The contribution of maternal stress to preterm birth: issues and considerations. Clinics in Perinatology. 2011;38:351–384. doi: 10.1016/j.clp.2011.06.007. doi: 10.1016/j.clp.2011.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker JL, Li J. Latent lifestyle preferences and household location decisions. Journal of Geographical Systems. 2007;9:77–101. doi: 10.1007/s10109-006-0030-0. [Google Scholar]
- Walker RE, Keane CR, Burke JG. Disparities and access to healthy food in the United States: A review of food deserts literature. Health & Place. 2010;16:876–884. doi: 10.1016/j.healthplace.2010.04.013. doi: 10.1016/j.healthplace.2010.04.013. [DOI] [PubMed] [Google Scholar]
- Wang X, Liang L, Junfen FU, Lizhong DU. Metabolic syndrome in obese children born large for gestational age. Indian Journal of Pediatrics. 2007;74:561–565. doi: 10.1007/s12098-007-0108-9. doi: 10.1007/s12098-007-0108-9. [DOI] [PubMed] [Google Scholar]
- Wassimi S, Wilkins R, Mchugh NG, Xiao L, Simonet F, Luo ZC. Association of macrosomia with perinatal and postneonatal mortality among First Nations people in Quebec. Canadian Medical Association Journal. 2011;183:322–326. doi: 10.1503/cmaj.100837. doi: 10.1503/cmaj.100837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissmann-Brenner A, Simchen MJ, Zilberberg E, Kalter A, Weisz B, Achiron R, Dulitzky M. Maternal and neonatal outcomes of large for gestational age pregnancies. Acta Obstetricia et Gynecologica Scandinavica. 2012;91:844–849. doi: 10.1111/j.1600-0412.2012.01412.x. doi: 10.1111/j.1600-0412.2012.01412.x. [DOI] [PubMed] [Google Scholar]
- Yessoufou A, Moutairou K. Maternal diabetes in pregnancy: early and long-term outcomes on the offspring and the concept of “metabolic memory”. Experimental Diabetes Research. 2011;2011:218598. doi: 10.1155/2011/218598. doi: 10.1155/2011/218598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeka A, Melly SJ, Schwartz J. The effects of socioeconomic status and indices of physical environment on reduced birth weight and preterm births in Eastern Massachusetts. Environmental Health. 2008;7:60. doi: 10.1186/1476-069X-7-60. doi: 10.1186/1476-069X-7-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


