Abstract
Background
Incidental durotomy is a familiar encounter during surgery for lumbar spinal stenosis. The impact of durotomy on long-term outcomes remains a matter of debate.
Objective
To determine the impact of durotomy on the long-term outcomes of patients in the Spine Patient Outcomes Research Trial (SPORT).
Methods
SPORT cohort participants with a confirmed diagnosis of spinal stenosis (SPS), without associated spondylolisthesis, undergoing standard, first-time, open decompressive laminectomy, with or without fusion, were followed from baseline at 6 weeks, and 3, 6, 12 months and yearly thereafter, at 13 spine clinics in 11 US states. Patient data from this prospectively gathered database was reviewed. As of May 2009, the mean follow-up among all analyzed patients was 43.8 months.
Results
409 patients underwent first-time open laminectomy with or without fusion. 37 (9%) of these patients had an incidental durotomy. No significant differences were observed with or without durotomy in age, sex, race, body mass index, the prevalence of smoking, diabetes and hypertension, decompression level, number of levels decompressed, or whether or not an additional fusion was performed. The durotomy group had significantly increased operative duration, operative blood loss and inpatient stay. There were however, no differences in incidence of nerve root injury, mortality, additional surgeries, primary outcomes (SF-36 scores of body pain or physical function, or Oswestry disability index) at yearly follow ups to 4 years.
Conclusions
Incidental durotomy during first time lumbar laminectomy for spinal stenosis did not impact long-term outcomes in affected patients.
Keywords: durotomy, spinal stenosis, lumbar spine, outcomes, complications
INTRODUCTION
Lumbar laminectomy for spinal stenosis is one of the most common spinal procedures performed. A frequent complication associated with laminectomy is incidental durotomy. Various series have estimated the incidence of an unintentional durotomy during lumbar spine surgery to be between 1 and 17%,1–20 with higher incidences associated with repeat surgery, increased patient age, and reduced surgeon experience.1, 3, 7, 8, 20–22
Dural tears have been associated with significant morbidity, most notably with spinal headaches, meningeal pseudocyst formation, and dural-cutaneous cerebrospinal fluid fistulas.8, 10 To avoid these sequelae, several interventions have been used once a dural tear is recognized. These include primary repair, lumbar drain placement and post-operative bed rest.1, 4, 6, 7, 23 Even when such precautions are taken, the effect of unintentional durotomy on long-term outcomes remains controversial.6, 10 In addition, the incidence and subsequent outcomes of dural tears during specific lumbar spine procedures (such as discectomy, or laminectomy for spinal stenosis) have not previously been studied.
The Spine Patient Outcomes Research Trial provides a significant opportunity to examine long-term outcomes after incidental durotomy during lumbar laminectomy for spinal stenosis given its large cohort size,24, 25 long-term follow-up and the multiple standardized outcome measures recorded in the trial. Furthermore, all laminectomies were performed using an open approach (i.e. without the use of a tubular retractor system) and all were performed in patients without previous history of lumbar spine surgery.
This study was undertaken in order to investigate whether incidental durotomy during first-time surgery for spinal stenosis across the 13 multidisciplinary spine clinics participating in the SPORT trial had any effects on long-term outcomes.
METHODS
Study Design
SPORT was conducted at 13 medical centers with multidisciplinary spine practices in 11 states in the United States. Institutional review board approval was obtained at each center. The trial was registered with ClinicalTrials.gov (NCT00000411). Additional background information is available in previous publications.24, 25
Patient Population
All patients had neurogenic claudication or radicular leg pain with associated neurological signs, spinal stenosis seen on cross-sectional imaging, symptoms that had persisted for at least twelve weeks, and surgeon (Orthopedic and/or Neurosurgeon) confirmation that they were surgical candidates. Pre-enrollment non-operative care included physical therapy, anti-inflammatory medications, opioid analgesics, epidural injections, and chiropractic care. Enrollment began in March 2000 and ended in February 2005.
Surgery Performed
The protocol surgery consisted of a standard open laminectomy at the affected level or levels with or without fusion. The use of a microscope was at the surgeon’s discretion but was not recorded as a SPORT data element.
Study Measures
The short-term outcome measures were operative duration, operative blood loss, inpatient length of stay, perioperative nerve root injury, requirement for blood transfusion, wound complications (e.g. infection) and post-operative mortality up to 3 months.
The long-term outcome measures were the need for repeat surgery at 3 months, and 1, 2, 3 and 4 years, the Short Form-36 (SF-36) bodily pain, physical function and mental component scores, Stenosis bothersomeness index (SBI) and the American Academy of Orthopaedic Surgeons MODEMS (Musculoskeletal Outcomes Data Evaluation and Management System) version of the Oswestry Disability Index, measured at 3 months, and yearly up to 4 years. The effect of the incidental durotomy on long-term outcome was defined as the difference in the mean changes, as compared with baseline, between the durotomy and no-durotomy groups (the difference in the difference).
SF-36 scores range from 0 to 100 points, with higher scores indicating less severe symptoms; the Oswestry Disability Index ranges from 0 to 100 points, with lower scores indicating less severe symptoms; the Stenosis Bothersomeness Index ranges from 0 to 24 points, with lower scores indicating less severe symptoms.
Statistical Methods
The baseline characteristics and short- and long-term outcome measures were compared between the patients in the durotomy cohort and those in the no-durotomy cohort. The analyses consisted of comparisons of both groups. The baseline characteristics were only analyzed for patients in both groups that had at least one year of follow-up. Computations were performed with the use of the PROC MIXED procedure for continuous data and the PROC GENMOD procedure for binary and non-normal outcomes from the SAS software package (version 9.1; SAS Institute, Cary, North Carolina). Significance was defined as p < 0.05 on the basis of a two-sided hypothesis test with no adjustments made for multiple comparisons. The data for these analyses were collected through May 1, 2009.
RESULTS
Incidence of durotomy
A total of 409 patients underwent standard lumbar laminectomy with or without fusion. Of these, durotomy occurred in 37, for an incidence of 9%.
Follow-up
As of May 2009, the mean (SD) follow-up among all analyzed patients undergoing surgery for spinal stenosis was 43.8 (14) months (No durotomy: 43.2 vs. durotomy: 46, p-value=0.25). The median (range) follow-up time among all analyzed SPS patients was 47 (1, 95.6) months.
Baseline characteristics (Table 1)
Table 1.
Comparison of baseline characteristics between the durotomy and no durotomy groups.
| Characteristics | No durotomy (n=367) | Durotomy (n=37) | p-value |
|---|---|---|---|
| Mean Age (SD) | 63.9 (12.3) | 64 (11.9) | 0.96 |
| Female – no. (%) | 140 (38%) | 16 (43%) | 0.67 |
| Mean Body Mass Index (BMI), (SD) | 29.5 (5.3) | 28.7 (6.1) | 0.36 |
| Smoker | 34 (9%) | 3 (8%) | 0.95 |
| Comorbidities – no. (%) | |||
| Hypertension | 157 (43%) | 15 (41%) | 0.93 |
| Diabetes | 51 (14%) | 5 (14%) | 0.85 |
| Osteoporosis | 28 (8%) | 4 (11%) | 0.72 |
| Depression | 41 (11%) | 3 (8%) | 0.77 |
| Joint Problem | 194 (53%) | 21 (57%) | 0.78 |
| SF-36 scores, mean (SD) | |||
| Bodily Pain (BP) | 30.5 (18.8) | 29.6 (41%) | 0.78 |
| Physical Functioning (PF) | 31.9 (22) | 30.9 (68%) | 0.80 |
| Vitality (VT) | 41.4 (21.6) | 41.6 (41%) | 0.96 |
| Physical Component Summary (PCS) | 29 (8) | 28.5 (68%) | 0.71 |
| Mental Component Summary (MCS) | 48.6 (12) | 48.8 (41%) | 0.92 |
| Oswestry Disability Index (ODI)(SD)‡‡ | 45.9 (18) | 45.1 (16.2) | 0.80 |
| Stenosis Bothersome Index (0–24)(SD)§§ | 15.5 (5.3) | 14.7 (6.5) | 0.37 |
| Any Neurological Deficit | 197 (54%) | 20 (54%) | 0.90 |
| Reflexes-Asymmetric Depressed | 97 (26%) | 9 (24%) | 0.94 |
| Sensory-Asymmetric Decrease | 108 (29%) | 12 (32%) | 0.85 |
| Motor – Asymmetric Weakness | 93 (25%) | 11 (30%) | 0.70 |
| Stenosis Level | |||
| L2–L3 | 106 (29%) | 16 (43%) | 0.10 |
| L3–L4 | 244 (66%) | 29 (78%) | 0.20 |
| L4–L5 | 337 (92%) | 34 (92%) | 0.76 |
| L5–S1 | 91 (25%) | 13 (35%) | 0.24 |
| Number of Moderate/Severe Stenotic Levels | |||
| None | 6 (2%) | 0 (0%) | |
| One | 135 (37%) | 8 (22%) | |
| Two | 140 (38%) | 19 (51%) | |
| Three + | 86 (23%) | 10 (27%) | |
| Stenosis Locations | |||
| Central | 315 (86%) | 33 (89%) | 0.75 |
| Lateral Recess | 297 (81%) | 31 (84%) | 0.84 |
| Neural foramen | 106 (29%) | 16 (43%) | 0.10 |
| Stenosis Severity | |||
| Mild | 6 (2%) | 0 (0%) | |
| Moderate | 153 (42%) | 15 (41%) | |
| Severe | 208 (57%) | 22 (59%) | |
| Instability | 0 (0%) | 0 (0%) | |
| Prior lumbar epidural steroid injection | 204 (56%) | 21 (57%) | 0.97 |
Patients receiving surgery were classified according to whether they received surgical treatment during the first 4 years of enrollment.
The body-mass index is the weight in kilograms divided by the square of the height in meters.
Other indicates problems related to stroke, cancer, lung, fibromyalgia, chronic fatigue syndrome, post traumatic stress disorder, alcohol, drug dependency, liver, kidney, blood vessel, nervous system, migraine,
The SF-36 scores range from 0 to 100, with higher score indicating less severe symptoms.
The Oswestry Disability Index ranges from 0 to 100, with lower scores indicating less severe symptoms.
The Stenosis Bothersomeness index range from 0 to 24, with lower scores indicating less severe symptoms.
Out of 409 patients that underwent surgery, 404 patients had greater than one-year follow-up and their baseline characteristics were reviewed. No significant differences were seen between the durotomy and no-durotomy groups in baseline clinical characteristics. These included age, sex, race, body mass index, the prevalence of smoking, diabetes and hypertension, pre-operative neurological symptoms or deficits, and pre-operative SF-36 and Oswestry disability index scores. There were also no differences in the stenosis level or number of levels, the location (central, lateral recess or neural foraminal) or severity (mild, moderate, severe) of the stenosis, or whether or not the patients had previous lumbar epidural steroid injections.
Operative events (Table 2)
Table 2.
Comparison of perioperative outcomes between the durotomy and no durotomy groups.
| Outcome | No durotomy (n=371) |
Durotomy (n=38) |
p-value |
|---|---|---|---|
| Specific Procedures† | 0.54 | ||
| Decompression Only | 321 (88%) | 33 (89%) | |
| Non instrumented Fusion | 19 (5%) | 3 (8%) | |
| Instrumented Fusion | 23 (6%) | 1 (3%) | |
| Multi-level Fusion | 15 (4%) | 1 (3%) | 0.99 |
| Decompression Level | |||
| L2–L3 | 129 (36%) | 17 (45%) | 0.35 |
| L3–L4 | 251 (69%) | 29 (76%) | 0.47 |
| L4–L5 | 335 (92%) | 36 (95%) | 0.82 |
| L5–S1 | 134 (37%) | 19 (50%) | 0.16 |
| Levels Decompressed | 0.082 | ||
| None | 8 (2%) | 0 (0%) | |
| 1 | 86 (23%) | 7 (18%) | |
| 2 | 120 (32%) | 7 (18%) | |
| 3+ | 157 (42%) | 24 (63%) | |
| Operation time (min) | 125.2 (66.8) | 161.7 (44.5) | 0.001 |
| Blood loss (ml) | 288.9 (396.1) | 534.4 (421.8) | <0.001 |
| Blood Replacement | |||
| Intraoperative replacement | 33 (9%) | 6 (16%) | 0.26 |
| Post-operative transfusion | 17 (5%) | 3 (8%) | 0.59 |
| Length of stay (days) | 3.1 (2.4) | 4.3 (2.1) | 0.003 |
| Intraoperative complications§ | |||
| Vascular injury | 0 (0%) | 0 (0%) | |
| Other | 3 (1%) | 0 (0%) | 0.66 |
| None | 368 (99%) | 38 (100%) |
Surgical information was available for 371 non-durotomy and 38 durotomy patients.
Specific procedure data was available for 363 non-durotomy and 37 durotomy patients.
No cases were reported of aspiration into the respiratory tract or operation at wrong level.
There were no differences between the two groups in decompression levels, number of levels, or the addition of instrumented or non-instrumented fusion to the decompression. There was a significantly increased operative duration (161.7 minutes versus 125.2 minutes, p=0.001) and operative blood loss (534.4ml versus 288.9ml, p<0.001) in the durotomy group. This amounted to an approximately 29% and 85% increase respectively. However, these patients did not have significantly increased needs for intra-operative or post-operative blood transfusion.
Short-term outcomes (Table 3)
Table 3.
Comparison of post-operative outcomes between the durotomy and no durotomy groups.
| Outcome | No durotomy (n=371) | Durotomy (n=38) | p-value |
|---|---|---|---|
| Postoperative complications¶ | |||
| Nerve root injury | 0 (0%) | 0 (0%) | |
| Wound hematoma | 4 (1%) | 0 (0%) | 0.81 |
| Wound Infection | 7 (2%) | 2 (5%) | 0.43 |
| Other | 20 (5%) | 4 (11%) | 0.34 |
| None | 325 (88%) | 29 (78%) | 0.15 |
| Post-operative mortality (death within 6 weeks of surgery) | 1 (0.2%) | 0 (0%) | |
| Post-operative mortality (death within 3 months of surgery) | 1 (0.2%) | 0 (0%) | |
| Additional surgeries (1-year rate)‖ | 20 (5%) | 1 (3%) | 0.461 |
| Additional surgeries (2-year rate)‖ | 28 (8%) | 3 (8%) | 0.959 |
| Additional surgeries (3-year rate)‖ | 41 (11%) | 3 (8%) | 0.554 |
| Additional surgeries (4-year rate)‖ | 49 (13%) | 3 (8%) | 0.363 |
| Recurrent stenosis/progressive lesthesis | 22 (6%) | 1 (3%) | |
| Pseudoarthrosis/fusion exploration | 0 (0%) | 0 (0%) | |
| Complication or Other | 15 (4.1%) | 2 (5.3%) | |
| New Condition | 7 (1.9%) | 1 |
Surgical information was available for 371 non-durotomy and 38 durotomy patients.
Complications or events occurring up to 8 weeks after surgery are listed. There were no reported cases of bone-graft complication, cerebrospinal fluid leak, paralysis, cauda equina injury or pseudarthrosis.
Rates of repeated surgery at 1, 2, 3, and 4 years are Kaplan-Meier estimates. P values were calculated with the use of the log-rank test. Numbers and percentages are based on the first additional surgery if more than one additional surgery.
There was a significantly increased length of hospital stay among the durotomy group (4.3 versus 3.1 days, p=0.003). This amounted to an approximately 39% increase in hospital stay. There were no increases in the incidence of wound hematoma or infection and post-operative nerve root injury. No occurrences of CSF fistula formation, wound dehiscence, bone graft complication, paralysis or cauda equina injury, pseudoarthrosis, or other complications attributable to surgery were observed. One patient (in the no durotomy group) died 9 days after surgery from a myocardial infarction.
Long-term outcomes (Table 3, Table 4, Figure 1)
Table 4.
Change scores and their differences (“No durotomy” minus “durotomy”) for SF- 36 scores, Oswestry disability index scores and Stenosis bothersome index scores, according to status of durotomy.
| 3-month | 1-year | 2-year | 3-year | 4-year | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Difference† (95% CI) |
p-value | Difference† (95% CI) |
p-value | Difference† (95% CI) |
p-value | Difference† (95% CI) |
p-value | Difference† (95% CI) |
p-value | AUC p-value | |
| SF-36 Bodily Pain (SE)‡ | −2.4 (−11.7, 6.9) | 0.61 | −8.2 (−18, 1.7) | 0.10 | −7.2 (−18.2, 3.8) | 0.20 | −2 (−11.4, 7.4) | 0.68 | −7 (−19.8, 5.8) | 0.28 | 0.13 |
| SF-36 Physical Function (SE)‡ | −0.9 (−10, 8.3) | 0.86 | −6.3 (−13.1, 6.2) | 0.49 | −4.7 (−15.4, 5.9) | 0.38 | −2.2 (−11.4, 7.1) | 0.65 | −4.4 (−16.7, 7.9) | 0.48 | 0.45 |
| SF-36 Mental Component Summary (SE)‡ | −2.7 (−6.6, 1.1) | 0.16 | −1.8 (−5.9, 2.2) | 0.38 | −2.7 (−7.3, 1.8) | 0.24 | 0.2 (−3.7, 4.1) | 0.92 | 0.5 (−4.8, 5.8) | 0.86 | 0.40 |
| Oswestry Disability Index (SE)§ | 2.8 (−4.5, 10.1) | 0.46 | 2.7 (−5.1, 10.4) | 0.50 | 2.6 (−5.9, 11) | 0.55 | −0.4 (−7.7, 7) | 0.92 | 5.5 (−4.2, 15.3) | 0.27 | 0.38 |
| Stenosis Bothersomeness Index (SE)¶ | 1 (−2, 3.9) | 0.53 | 0.7 (−1.8, 3.2) | 0.58 | 1.5 (−1.4, 4.3) | 0.31 | 1.2 (−1.3, 3.6) | 0.36 | 2.5 (−0.7, 5.7) | 0.12 | 0.22 |
Adjusted for age, gender, BMI and baseline score.
Difference is the difference between no durotomy group mean change from baseline and had durotomy group mean change from baseline.
The SF-36 scores range from 0 to 100, with higher score indicating less severe symptoms.
The Oswestry Disability Index ranges from 0 to 100, with lower scores indicating less severe symptoms
The Stenosis Bothersomeness Index ranges from 0 to 24, with lower scores indicating less severe symptoms
Figure 1.
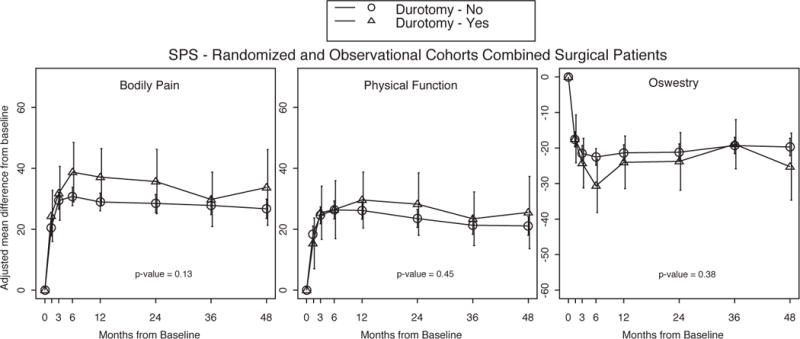
Outcome results over time by status of durotomy with area under curve p-value that compares the durotomy group to the no-durotomy group
There were no significant differences between the durotomy and no-durotomy groups in the incidence of recurrent stenosis or development of listhesis. One-, two-, three- and four-year post-surgical re-operation rates were calculated from Kaplan-Meier plots and no significant difference was observed between the two groups. (Table 3).
There were no differences between the durotomy and no-durotomy groups in mean difference from baseline for SF-36 bodily pain, physical function and mental component summary scores, at 3 months, 1 year, 2 years, 3 years and 4 years. Similarly there were no difference in Oswestry disability index and Stenosis bothersomeness index at 3 months, and 1, 2, 3 and 4 years (Table 4, Figure 1).
DISCUSSION
Incidental durotomy occurred in less than 10% of SPORT cases of spinal stenosis during lumbar spine surgery. Although durotomy has been associated with a number of medical malpractice lawsuits,26 the effects of this complication in patient outcomes has remained controversial, at best. In addition, there has to date been limited information on the incidence of dural tears and their outcomes in patients undergoing specific spinal procedures.
Several studies attempting to analyze effects on outcome after durotomy have yielded inconsistent results. Wang et al7 demonstrated that dural tears do not have any deleterious effects on outcomes in the largest series of incidental durotomies (88 patients) presented to date. Jones et al1 did not identify any difference in outcome between their 17 patients with incidental durotomies and appropriately matched controls. Cammisa et al8 reached similar conclusions in their study group of 66 incidental durotomies. In agreement with these results, the current study has demonstrated that in patients undergoing lumbar laminectomies for spinal stenosis, incidental durotomies – while affecting intraoperative blood loss and hospital length of stay – do not increase the risk of other perioperative morbidities or adversely affect patient outcome at 6 weeks, 3 months or at 1, 2, 3 or 4 years. However, all the previous studies were retrospective in nature and took into account all lumbar spine procedures, including lumbar discectomy and surgery for spondylolisthesis, in addition to revision surgeries. These confounding variables have been addressed in the current study, where prospectively collected data from patients with a single pathology and operation (open lumbar laminectomy), that were part of a multi-institution study, are analyzed.
Saxler et al10 had contrasting results after retrospectively analyzing their group of 41 lumbar discectomy patients in whom durotomy occurred intraoperatively, and comparing them with appropriately matched controls. Patients with incidental durotomy had a poorer outcome after surgery, with a decreased Tenger Score, more re-operations, more postoperative headaches, a longer inability to work, more back pain and functional limitations related to it. Although these data contradict most of the literature on durotomies, they are not in conflict with the present study on laminectomy for spinal stenosis patients, since they deal exclusively with discectomy patients. However, several methodological pitfalls raise concerns about the applicability of these data. Recall bias can hinder the validity of these results, while the retrospective nature of the study makes it possible that patients with good postoperative results were lost at follow up further confounding the outcomes. The current study overcomes several of these limitations by describing standardized outcomes in a multi-center cohort of prospectively collected data of patients undergoing first time surgery.
The rate of incidental durotomy in the present study was 9%, comparable to that reported for lumbar spine surgery in previous series.1, 4, 7, 8, 10 The reported incidence of dural tears ranges from 1–17% and varies according to the patient characteristics, surgeon experience and the surgical procedure performed.11 Our rate in this series may be partially attributable to the nature of the surgery analyzed; previous studies have suggested a higher rate of durotomy in patients undergoing surgery for longstanding spinal stenosis.12 Deyo et al21 evaluated operative complications, including dural tears, in a large series of spinal procedures. The morbidity was lower for younger patients and for discectomies, while worst outcomes were associated with increased age, spinal stenosis, and re-operations. Several other authors have confirmed these results1, 3, 7, 8, 11, 22. Although several of these studies have supported the finding that fusion is also associated with an increased risk of durotomy, our two groups (durotomy versus no-durotomy) did not demonstrate any significant difference in the incidence of fusion. However, as expected in stenosis without listhesis, the overall rate of fusion was very low, limiting our ability to assess any potential difference, but rates were similar in the SPORT degenerative spondylolisthesis cohort (9% in the observational group and 11% in the randomized group) wherein fusion was performed in most cases.
The complications associated with dural tears are varied. They include postoperative headache, pseudomeningocele, nerve root entrapment with resultant neurological damage, wound infection, meningitis, and arachnoiditis.1, 20, 26 In addition, several rarer complications have been reported, including symptomatic pneumorachis27, spinal subdural empyema28, bilateral subdural hematomas29, and cerebral vasospasm30. While in the present study a significantly increased length of hospital stay among the durotomy group was observed, we did not observe an increase in the incidence of post-operative nerve root injury or wound infection. There were no occurrences of CSF fistula formation, wound dehiscence, neurological complications, or other complications attributable to surgery. The observed increased length of stay among patients with dural tears may be attributed to the tendency for increased post-operative bed rest and slower mobilization of these patients.
Several outcome measures have been used in the literature to quantify long-term outcomes in patients with incidental durotomies10. In the current study, there were no significant differences between the durotomy and no-durotomy groups in the incidence of recurrent stenosis, development of listhesis, or re-operations (Table 3). There were no differences between the durotomy and no-durotomy groups in mean difference from baseline for SF-36 bodily pain, physical function and mental component summary scores, and in Oswestry Disability Index and stenosis bothersome index scores over time. (Table 4).
The results from the current study should be interpreted with its limitations in mind. We did not have access to the precise methods of treatment followed in the different centers for the incidental durotomies and therefore their homogeneity cannot be assessed, and a comparison with the treatments of the literature cannot be attempted. Data on the use of microscope were also not collected and therefore we cannot provide an answer as to whether the incidence of durotomy can be altered by its use, nor did we have cases using percutaneous tubular decompressions.
The power of the present study in evaluating differences in outcome should also be considered. While the sample size is relatively large (409 patients, with 37 durotomies) in comparison to previously reported series, the 95% confidence intervals for the differences in the long-term outcome measures (SF-36, Oswestry Disability Index, Stenosis Bothersomeness Index) between the durotomy and no-durotomy groups in this study are relatively broad, and are in some instances greater than 10 points from zero (Table 4). However, the tendency at all of these data points is for better outcomes in the durotomy group (higher SF-36 scores and lower Oswestry Disability Index and Stenosis Bothersomeness Index scores), although this is not statistically significant. Hence, while the broad confidence intervals suggest that a difference in outcome cannot be excluded, this difference, if it exists, appears to be the direction of improved outcomes after durotomy. While improved outcomes cannot be easily explained, the broad confidence intervals that raise this possibility highlight the limited power of this study for detecting differences in outcome and suggest a need for larger observational studies to confirm equivalence in outcome after durotomy.
Conclusions
Incidental durotomy is a relatively uncommon complication during lumbar laminectomy for spinal stenosis (<10%). In the current study, patients in whom durotomy occurred had significantly increased operative duration, operative blood loss and inpatient stays. There were however, no differences in incidence of nerve root injury, post-operative wound complications, additional surgeries, SF-36 scores of body pain or physical function, or Oswestry disability index at 1, 2, 3 and 4 years. Therefore, incidental durotomy during first time lumbar laminectomy for spinal stenosis does not appear to affect long-term outcome in affected patients.
Acknowledgments
The authors would like to acknowledge funding from the following sources: The National Institute of Arthritis and Musculoskeletal and Skin Diseases (U01-AR45444) and the Office of Research on Women’s Health, the National Institutes of Health, and the National Institute of Occupational Safety and Health, the Centers for Disease Control and Prevention.
Footnotes
Trial Registration: Spine Patient Outcomes Research Trial (SPORT): Spinal Stenosis; 3 #NCT00000411; http://www.clinicaltrials.gov/ct/show/NCT00000411?order=4
References
- 1.Jones AA, Stambough JL, Balderston RA, Rothman RH, Booth REJ. Long-term results of lumbar spine surgery complicated by unintended incidental durotomy. Spine (Phila Pa 1976) 1989;14(4):443–446. doi: 10.1097/00007632-198904000-00021. [DOI] [PubMed] [Google Scholar]
- 2.Rampersaud YR, Moro ER, Neary MA, et al. Intraoperative adverse events and related postoperative complications in spine surgery: implications for enhancing patient safety founded on evidence-based protocols. Spine (Phila Pa 1976) 2006;31(13):1503–1510. doi: 10.1097/01.brs.0000220652.39970.c2. [DOI] [PubMed] [Google Scholar]
- 3.Stolke D, Sollmann WP, Seifert V. Intra- and postoperative complications in lumbar disc surgery. Spine (Phila Pa 1976) 1989;14(1):56–59. doi: 10.1097/00007632-198901000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Tafazal SI, Sell PJ. Incidental durotomy in lumbar spine surgery: incidence and management. Eur Spine J. 2005;14(3):287–290. doi: 10.1007/s00586-004-0821-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wiesel SW. The multiply operated lumbar spine. Instr Course Lect. 1985;34:68–77. [PubMed] [Google Scholar]
- 6.Jankowitz BT, Atteberry DS, Gerszten PC, et al. Effect of fibrin glue on the prevention of persistent cerebral spinal fluid leakage after incidental durotomy during lumbar spinal surgery. Eur Spine J. 2009;18(8):1169–1174. doi: 10.1007/s00586-009-0928-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang JC, Bohlman HH, Riew KD. Dural tears secondary to operations on the lumbar spine. Management and results after a two-year-minimum follow-up of eighty-eight patients. J Bone Joint Surg Am. 1998;80(12):1728–1732. doi: 10.2106/00004623-199812000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Cammisa FPJ, G FP, Sangani PK, Parvataneni HK, Cadag S, Sandhu HS. Incidental durotomy in spine surgery. Spine (Phila Pa 1976) 2000;25(20):2663–2667. doi: 10.1097/00007632-200010150-00019. [DOI] [PubMed] [Google Scholar]
- 9.Khan MH, Rihn J, Steele G, et al. Postoperative management protocol for incidental dural tears during degenerative lumbar spine surgery: a review of 3,183 consecutive degenerative lumbar cases. Spine (Phila Pa 1976) 2006;31(22):2609–2613. doi: 10.1097/01.brs.0000241066.55849.41. [DOI] [PubMed] [Google Scholar]
- 10.Saxler G, Krämer J, Barden B, Kurt A, Pförtner J, Bernsmann K. The long-term clinical sequelae of incidental durotomy in lumbar disc surgery. Spine (Phila Pa 1976) 2005;30(20):2298–2302. doi: 10.1097/01.brs.0000182131.44670.f7. [DOI] [PubMed] [Google Scholar]
- 11.Sin AH, Caldito G, Smith D, Rashidi M, Willis B, Nanda A. Predictive factors for dural tear and cerebrospinal fluid leakage in patients undergoing lumbar surgery. J Neurosurg Spine. 2006;5(3):224–227. doi: 10.3171/spi.2006.5.3.224. [DOI] [PubMed] [Google Scholar]
- 12.Agrillo U, Simonetti G, Martino V. Postoperative CSF problems after spinal and lumbar surgery. General review. J Neurosurg Sci. 1991;35(2):93–95. [PubMed] [Google Scholar]
- 13.Black P. Cerebrospinal fluid leaks following spinal surgery: use of fat grafts for prevention and repair. Technical note. J Neurosurg. 2002;96(2 Suppl):250–252. doi: 10.3171/spi.2002.96.2.0250. [DOI] [PubMed] [Google Scholar]
- 14.Keenen TL, Antony J, Benson DR. Dural tears associated with lumbar burst fractures. J Orthop Trauma. 1990;4(3):243–245. doi: 10.1097/00005131-199004030-00001. [DOI] [PubMed] [Google Scholar]
- 15.Laus M, Pignatti G, Alfonso C, Ferrari D, De Cristofaro R, Giunti A. Complications in the surgical treatment of lumbar stenosis. Chir Organi Mov. 1990;77(1):65–71. [PubMed] [Google Scholar]
- 16.Leung PC. Complications in the first 40 cases of microdiscectomy. J Spinal Disord. 1988;1(4):306–310. doi: 10.1097/00002517-198800140-00005. [DOI] [PubMed] [Google Scholar]
- 17.Lu CH, Ho ST, Kong SS, Cherng CH, Wong CS. Intracranial subdural hematoma after unintended durotomy during spine surgery. Can J Anaesth. 2002;49(1):100–102. doi: 10.1007/BF03020428. [DOI] [PubMed] [Google Scholar]
- 18.Shapiro SA, Snyder W. Spinal instrumentation with a low complication rate. Surg Neurol. 1997;48(6):566–574. doi: 10.1016/s0090-3019(97)00296-6. [DOI] [PubMed] [Google Scholar]
- 19.Stewart G, Sachs BL. Patient outcomes after reoperation on the lumbar spine. J Bone Joint Surg Am. 1996;78(5):706–711. doi: 10.2106/00004623-199605000-00010. [DOI] [PubMed] [Google Scholar]
- 20.Finnegan WJ, Fenlin JM, Marvel JP, Nardini RJ, Rothman RH. Results of surgical intervention in the symptomatic multiply-operated back patient. Analysis of sixty-seven cases followed for three to seven years. J Bone Joint Surg Am. 1979;61(7):1077–1082. [PubMed] [Google Scholar]
- 21.Deyo RA, Cherkin DC, Loeser JD, Bigos SJ, Ciol MA. Morbidity and mortality in association with operations on the lumbar spine. The influence of age, diagnosis, and procedure. J Bone Joint Surg Am. 1992;74(4):536–543. [PubMed] [Google Scholar]
- 22.Eismont FJ, Wiesel SW, Rothman RH. Treatment of dural tears associated with spinal surgery. J Bone Joint Surg Am. 1981;63(7):1132–1136. [PubMed] [Google Scholar]
- 23.Hodges SD, Humphreys SC, Eck JC, Covington LA. Management of incidental durotomy without mandatory bed rest. A retrospective review of 20 cases. Spine (Phila Pa 1976) 1999;24(19):2062–2064. doi: 10.1097/00007632-199910010-00017. [DOI] [PubMed] [Google Scholar]
- 24.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT) observational cohort. JAMA. 2006;296(20):2451–2459. doi: 10.1001/jama.296.20.2451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical versus nonoperative treatment for lumbar disc herniation: four-year results for the Spine Patient Outcomes Research Trial (SPORT) Spine (Phila Pa 1976) 2008;33(25):2789–2800. doi: 10.1097/BRS.0b013e31818ed8f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goodkin R, Laska LL. Unintended “incidental” durotomy during surgery of the lumbar spine: medicolegal implications. Surg Neurol. 1995;43(1):4–12. doi: 10.1016/0090-3019(95)80031-b. [DOI] [PubMed] [Google Scholar]
- 27.Rovlias A, Pavlakis E, Kotsou S. Symptomatic pneumorachis associated with incidental durotomy during microscopic lumbar disc surgery. Case report. J Neurosurg Spine. 2006;5(2):165–167. doi: 10.3171/spi.2006.5.2.165. [DOI] [PubMed] [Google Scholar]
- 28.Wu AS, Griebel RW, Meguro K, Fourney DR. Spinal subdural empyema after a dural tear. Case report. Neurosurg Focus. 2004;17(6):E10. doi: 10.3171/foc.2004.17.6.10. [DOI] [PubMed] [Google Scholar]
- 29.Buvanendran A, Byrne RW, Kari M, Kroin JS. Occult cervical (C1–2) dural tear causing bilateral recurrent subdural hematomas and repaired with cervical epidural blood patch. J Neurosurg Spine. 2008;9(5):483–487. doi: 10.3171/SPI.2008.9.11.483. [DOI] [PubMed] [Google Scholar]
- 30.Chaves C, Freidberg SR, Lee G, Zerris V, Ries S, Chavali R. Cerebral vasospasm following intracranial hypotension caused by cerebrospinal fluid leak from an incidental lumbar durotomy. Case report. J Neurosurg. 2005;102(1):152–155. doi: 10.3171/jns.2005.102.1.0152. [DOI] [PubMed] [Google Scholar]


