Abstract
The purpose of the present study was to develop a novel transdermal drug-delivery system comprising a polyamidoamine dendrimer coupled with sonophoresis to enhance the permeation of diclofenac (DF) through the skin. The novel transdermal drug-delivery system was developed by using a statistical Plackett–Burman design. Hairless male Wistar rat skin was used for the DF-permeation study. Coupling media concentration, ultrasound-application time, duty cycle, distance from probe to skin, and a third-generation polyamidoamine-dendrimer concentration were selected as independent variables, while in vitro drug release was selected as a dependent variable. Independent variables were found to be statistically significant (P<0.05). DF gel without dendrimer and ultrasound treatment to skin (passive delivery, run 13) showed 56.69 µg/cm2 cumulative drug permeated through the skin, while the DF-dendrimer gel without sonophoresis treatment (run 14) showed 257.3 µg/cm2 cumulative drug permeated through the skin after 24 hours. However, when the same gel was applied to sonophoresis-treated skin, drastic permeation enhancement was observed. In the case of run 3, the cumulative drug that permeated through the skin was 935.21 µg/cm2. It was concluded that dendrimer-coupled sonophoresis-mediated transdermal drug delivery system has the potential to enhance the permeation of DF through the skin.
Keywords: sonophoresis, ultrasound, polyamidoamine, permeation enhancers, stratum corneum
Introduction
Diclofenac (DF) is a nonsteroidal anti-inflammatory drug. DF exhibits anti-inflammatory, analgesic, and antipyretic activities in animal models.1–3 DF has been used effectively in symptomatic management of musculoskeletal disorders, arthritis, toothache, dysmenorrhea, etc, for symptomatic relief of pain and inflammation.4–7 DF sodium has a short half-life of 2 hours, making it necessary to administer the drug several times in a day. The drug undergoes substantial hepatic first-pass metabolism, and thus only about 50% of the administered dose reaches systemic circulation.8 The bioavailability of DF is 40%–60%, and it causes serious gastrointestinal (GI) adverse effects, including inflammation, bleeding, ulceration, and perforation of the stomach, small intestine, or large intestine, which can be fatal.9,10 With regard to all the drawbacks of oral delivery of DF, there is a need for an alternative route of administration that can bypass hepatic first-pass metabolism, avoid GI adverse effects, and improve bioavailability. The trans-dermal route of administration is an alternative choice for such drugs. This route is best suited for drugs that undergo first-pass metabolism with low bioavailability.11,12 Also, it avoids GI side effects, which increases patient compliance.13 However, the major limiting factor for the development of a transdermal drug-delivery system (TDDS) is the epidermal layer and others beneath the lining of the skin. These barriers are hurdles for the penetration of drugs.
Dendrimers are monodisperse, hyperbranched, three dimensional, treelike macromolecules with host–guest entrapment properties. Dendrimers are a potent skin-permeation enhancer, as well as a solubility enhancer.14,15 Dendrimers are extensively used in pharmaceutical and biotechnological applications to deliver biomolecules.16 Dendrimers have been successfully utilized to improve the aqueous solubility of sulfamethoxazole, nadifloxacin, prulifloxacin, furosemide, ketoprofen, ibuprofen, diflunisal, albendazole, and ketoconazole.17 Recently extensive work related to dendrimers has been carried out that includes the development of novel TDDSs with polyhydroxyalkanoate and starburst polyamidoamine (PAMAM) dendrimers.18 Dendrimer-mediated transdermal delivery enhances the bioavailability of indomethacin19 and the effect of polyamidoamine dendrimer on skin permeation of 5-fluorouracil.20
Nowadays, apart from the use of permeation enhancers, ultrasound technology in the form of sonophoresis is used to deliver the active ingredient through the skin to achieve a more suitable therapeutic approach.21,22 In this technique, ultrasound is used to transfer the molecule through soft tissue as well as intact skin. It is one of the most promising novel DDSs, and has been shown to enhance the skin penetration and release rate of a number of drugs that have poor absorption or permeation profiles through the skin.23,24 This method is very rapid, convenient, and painless, functions independently of the drug’s electrical characteristics, and is useful for delivering low-molecular-weight drugs as well as macromolecules into skin.25 Many articles have summarized various aspects relating to sonophoresis, such as applications of sonophoresis and mechanisms and factors influencing sonophoresis in TDDSs. Enhanced skin permeation of DF by iontophoresis using this physical enhancement technique has been studied.21 Also, the effect of phonophoresis on skin permeation of the commercial anti-inflammatory gels sodium DF and ketoprofen was investigated.26 Sonophoresis-mediated transdermal and intradermal delivery for ketoprofen has been developed.27
A TDDS comprising sonophoresis and potent skin permeation-enhancing dendrimer is yet to be studied. Such drug-delivery technology would be synergistic in terms of the permeation enhancement of the drug molecules through the skin. It has now been found that acoustic cavitation (formation of oscillation of microbubbles in the coupling medium) plays an important role in ultrasound assisted delivery. The collapse of these microbubbles on the surface of the skin (stratum corneum [SC]) leads to skin permeation.28,29 Dendrimers are already a proven potential tool for skin-permeation enhancement for drug molecules. Due to the effect of sonophoresis on the skin, dendrimers lead to enhanced permeation of the drug through the skin. A TDDS is the potential technology for the transfer of active molecules through the skin.30,31 It serves as an alternative to an oral DDS. Transdermal delivery has certain advantages compared to the oral route. In particular, it is used when a drug has a significant first-pass effect as well as GI side effects.32,33 However, drug delivery through the skin is mainly limited by the SC, the topmost skin layer, which is composed of lipid-rich intercellular matrix and keratin-filled corneocytes.34,35 The lipid bilayer in the intercellular matrix is the major transport barrier for drug molecules.36,37 Drug molecules with molecular weight <500 Da and optimal physicochemical properties of log P 1–3 can be passively transported through the SC.38
Due to such specific requirements of the physicochemical properties of the drug molecule, it becomes a challenge to the scientist to deliver the active molecule through the skin. Various chemical and physical enhancement strategies have been adapted for the successful delivery of active molecules through the skin. These include different chemicals as permeation enhancers that can alter the properties of the SC to make it more permeable to drug molecules. Various enhancement strategies, including prodrugs, terpenes, fatty acids, iontophoresis, sonophoresis, and laser ablation, have been used to increase the skin permeation of drug molecules.39–42 The aim of the present study was to develop a TDDS for DF using a PAMAM dendrimer as a permeation enhancer along with the use of sonophoresis to maximize the permeation of active molecules through the skin.
Materials and methods
Materials
DF was purchased from Shouguang Fukang Pharmacy (Shandong, People’s Republic of China [PRC]), and the third-generation PAMAM dendrimer (PAMAM G3) Carbopol 934 was purchased from Sigma-Aldrich (St Louis, MO, USA). Triethanolamine and other chemicals were purchased from Shanghai Chemical (Shanghai, PRC).
Methods
Experimental design
A Plackett–Burman design (PBD) is a two-level fractional factorial design. It enables the study of k = N–1 variables in N runs, when N is a multiple of 4. In this way, seven factors can be tested within seven runs, so the number of trials may be reduced down to an absolute minimum.43,44 The plan is dedicated to screening out numerous factors in order to choose the ones that mostly impact the process outcomes. Coupling media concentration (A), ultrasound application time (B), duty cycle (C), distance from probe to skin (D), and PAMAM G3 dendrimer concentration (E) were selected as independent variables, while in vitro drug release (Y1) was selected as a dependent variable. Different levels of dependent variables are shown in Table 1. The PBD was used to derive a second-order polynomial equation and construct contour plots to predict responses.
Table 1.
Variables and two levels
| Independent variable | Low level (−1) | High level (+1) |
|---|---|---|
| A: SLS concentration | 1 | 2 |
| B: ultrasound application time | 1 | 3 |
| C: duty cycle | 50 | 100 |
| D: distance from probe to skin | 0.5 | 1 |
| E: dendrimer concentration | 0.3 | 0.5 |
Notes: Low level (−1) is the minimum concentration of independent variable used during the experiment; High level (+1) is the highest concentration of independent variable used during the experiment.
Abbreviation: SLS, sodium lauryl sulfate.
Formulation of diclofenac dendrimer gel
DF (200 mg) was dissolved in the required quantity of distilled water and PAMAM G3 dendrimer solution, as shown in Table 2, and was added to DF solution. In another 5 mL of distilled water, 100 mg Carbopol 934 was added and stirred with the help of a magnetic stirrer. DF in PAMAM G3 solution was added to Carbopol 934 gel, and the whole system was stirred with the help of a magnetic stirrer till a uniform homogeneous gel was formed. Triethanolamine was added dropwise during stirring to maintain the pH of the gel at 6.4. The gel was left for 48 hours to settle prior to use. This gel was used in each experiment. A control gel was also prepared without the addition of dendrimer to compare the effect of dendrimer on the skin permeation of DF.
Table 2.
Formulation of diclofenac gel- and sonophoresis-treatment parameters
| Batch | Factor
|
Response)
|
||||
|---|---|---|---|---|---|---|
| A | B | C | D | E | Y1 (µg/cm2) | |
| Run 1 | −1 | +1 | −1 | −1 | −1 | 435.68 |
| Run 2 | +1 | +1 | −1 | +1 | −1 | 478.96 |
| Run 3 | +1 | +1 | +1 | −1 | +1 | 935.21 |
| Run 4 | +1 | +1 | −1 | +1 | +1 | 727.2 |
| Run 5 | +1 | −1 | +1 | −1 | −1 | 580.45 |
| Run 6 | +1 | −1 | +1 | +1 | −1 | 550.00 |
| Run 7 | −1 | −1 | −1 | +1 | +1 | 650.00 |
| Run 8 | −1 | −1 | +1 | +1 | +1 | 792.60 |
| Run 9 | −1 | +1 | +1 | +1 | −1 | 620.78 |
| Run 10 | −1 | +1 | +1 | −1 | +1 | 860.63 |
| Run 11 | −1 | −1 | −1 | −1 | −1 | 320.85 |
| Run 12 | +1 | −1 | −1 | −1 | +1 | 695.53 |
Notes: Factors A, B, C, D, E are independent variables. Y is the in vitro drug release through the skin.
Animal skin preparation
In this study, male Wistar rats (200–250 g) were used for the permeation study. These animals were housed in temperature-controlled rooms (23°C–25°C) with a full supply of water and diet. Hairless Wistar rats were killed using carbon dioxide asphyxiation. Abdominal skin was isolated, and subcutaneous fat adhering to the skin was removed carefully. A fresh defatted skin was used for each experiment. This experimental study was performed according to the ethical committee of the Zhejiang Chinese Medical University, and all the protocols were reviewed by the animal care and use committee.
Sonophoresis experimental setup
All the experiments were performed using low-frequency ultrasound of 20 kHz (VCX 130; Sonics and Materials, Newton, CT, USA) with tip diameter of 6 mm and probe length of 113 mm. The experimental setup was adjusted as described in Herwadkar et al.27 Briefly, hairless abdominal skin was placed under the sonicator probe in such a way that the epidermal surface of the rat skin faced the sonicator probe. The distance between the probe and the skin was adjusted according to the experimental design. A glass donor chamber, open from both ends, of the vertical diffusion cell was placed over the skin. A coupling medium of sodium lauryl sulfate (SLS) with varying concentrations as per the experimental design was placed in the donor chamber. The sonicator probe was then placed in the coupling medium and ultrasound was activated for a predetermined time as per the experimental design. After ultrasound pretreatment, the skin was mounted on a Franz diffusion cell for permeation studies.
In vitro permeation studies
A specially designed glass diffusion cell was used to carry out an in vitro release study. Different ultrasound treatment conditions are shown in Table 2. An ultrasound-pretreated skin sample was mounted on the Franz diffusion cell in such a way that the epidermal surface of the skin faced toward the donor compartment of the cell. This skin was stretched around one end of the diffusion cell. The working surface area of the skin was 2.5 cm2. The receptor compartment was filled with 20 mL pH 6.8 phosphate buffer (Office of Generic Drugs dissolution media in which the drug has maximum solubility compared to other dissolution media), and the temperature was maintained at 32°C±0.5°C with circulating hot water through a glass jacket. DF dendrimer gel 50 mg was placed on the skin. The receptor medium was stirred at 50 rpm by keeping it on a hot plate magnetic stirrer. Aliquots (5 mL) of samples were withdrawn from the receptor medium at predetermined time intervals and replaced with equal volumes of fresh buffer to maintain the sink condition. Samples were analyzed with an ultraviolet spectrophotometer at 365 nm, and percentage drug release was calculated. Also, the control experiment was done with the same procedure without ultrasound treatment to the skin, and percentage drug release was calculated for the same experiment.
Results and discussion
Statistical analysis by PBD
PBD was used to evaluate the effects of dependent variables. Coupling media (SLS) concentration (A), ultrasound-application time (B), duty cycle (C), distance from horn to skin (D), and dendrimer concentration (E) were selected as independent variables, while in vitro drug release (Y1) was selected as the dependent variable. The effect of independent variables on the dependent variable was investigated by deriving polynomial equation and contour plots. In vitro skin permeation was performed in pH 6.8 phosphate buffer by using a modified diffusion cell. The in vitro drug permeation in 24 hours was found to be in the range of 320.85 µg/cm2 (run 11) to 935.21 µg/cm2 (run 3), as shown in Table 2. Diagnostic case statistics for various response variables are shown in Table 3, determining the residual value of each run. The polynomial equation obtained for in vitro permeation (Y1) was given by:
| (1) |
Table 3.
Diagnostic case statistics for various response variables
| Batch | Response variable | Actual value (µg/cm2) | Predicted value (µg/cm2) | Residual (F-test) |
|---|---|---|---|---|
| Run 1 | Y1 | 435.68 | 436.07 | −0.39 |
| Run 2 | Y1 | 478.96 | 479.35 | −0.39 |
| Run 3 | Y1 | 935.21 | 935.01 | 0.20 |
| Run 4 | Y | 727.2 | 727.00 | 0.20 |
| Run 5 | Y1 | 580.45 | 580.25 | 0.20 |
| Run 6 | Y1 | 550.00 | 549.80 | 0.20 |
| Run 7 | Y1 | 650.00 | 649.21 | 0.79 |
| Run 8 | Y1 | 792.60 | 793.58 | −0.98 |
| Run 9 | Y | 620.78 | 620.58 | 0.20 |
| Run 10 | Y1 | 860.63 | 860.43 | 0.20 |
| Run 11 | Y1 | 320.85 | 320.65 | 0.20 |
| Run 12 | Y1 | 695.53 | 695.92 | −0.39 |
Note: Values of F<0.05 indicate model terms are significant.
A positive value in this equation represents the synergistic effect of the independent variable on the dependent variable, while a negative value represents the inverse relationship (antagonistic effect), eg, +24.60 represents the positive or synergistic effect of independent factor A (coupling media concentration) on in vitro skin permeation, and −0.67 represents the antagonistic effect of independent factor D (distance from horn to skin) on in vitro skin permeation. The suggested model for Y1 was found to be 2FI with R2=0.9857, which is shown in Table 4. The P-value for the Y1 model was found to be <0.0063, which clearly indicated the model was statistically significant (P<0.05). The results showed that in vitro skin permeation was affected by the independent variables A, B, C, E, and AD, and that these were statistically significant model terms. Values greater than 0.1 indicated the model terms were not significant.
Table 4.
Summary of results of regression analysis for responses (Y1)
| Model | R2 | Adjusted R2 | Predicted R2 | SD | PRESS | CV | Adequate precision |
|---|---|---|---|---|---|---|---|
| Response (Y1) | |||||||
| 2FI | 0.9857 | 0.9752 | 0.9969 | 1.52 | 1,089.68 | 0.24 | 421.937 |
| Regression equation of the fitted model | |||||||
| Y1 = +637.32+24.60A+47.33B+72.18C−0.67D+131.39E−5.17AB−22.85AD−4.99AE−5.20BD−3.10DE | |||||||
Abbreviations: SD, standard deviation; PRESS, the predicted residual sum of squares; CV, coefficient of variation.
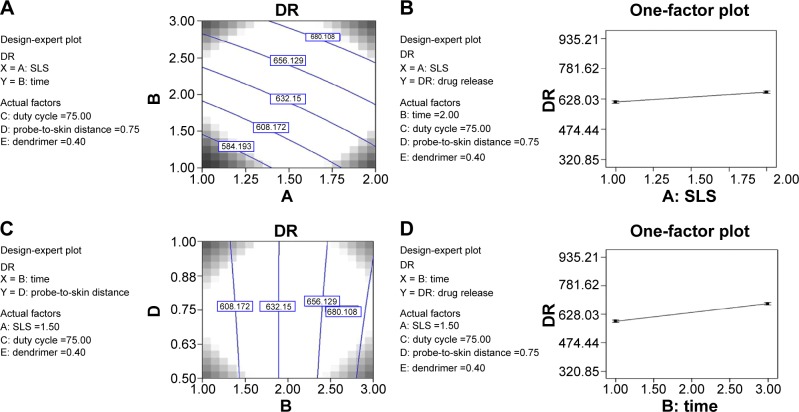
Also, among the five independent variables selected, only factor D (distance from horn to skin) was found to be statistically insignificant (P=0.4172), while the effect of factors A (P=0.0134), B (P=0.0077), C (P=0.0054), and E (P=0.0028) were found to be statistically significant, as shown in Table 5. In regression equation Y1, the main effects of A, B, C, D, and E represent the average results of changing one variable at a time from its low level to its high level. The interaction terms AB, AD, AE, BD, and DE showed how the skin permeation of drug changed when two variables were simultaneously changed. The negative coefficients of the independent variables indicated an unfavorable effect on skin permeation. The model F-value of 15,192.16 implies the model was significant. There is only a 0.63% chance that a model F-value this large could occur due to noise. Values of F<0.05 indicate model terms are significant. In this experiment, enhancement of skin permeation of DF was observed from 4.54-fold (run 14) to 16.50-fold (run 3) (Figure 1A).
Table 5.
Analysis of variance of models for Y1
| Source | df | Sum of squares | Mean square | F-value | P-value |
|---|---|---|---|---|---|
| Model for Y1 | 10 | 3.514E+005 | 35,136.54 | 15,192.16 | 0.063 |
| A | – | 5,234.99 | 5,234.99 | 2,263.48 | 0.0134 |
| B | – | 15,932.33 | 15,932.33 | 6,888.74 | 0.0077 |
| C | – | 32,064.35 | 32,064.35 | 13,863.83 | 0.0054 |
| D | – | 3.91 | 3.91 | 1.69 | 0.4172 |
| E | – | 1.237E+005 | 1.237E+005 | 53,500.99 | 0.0028 |
| AB | – | 190.35 | 190.35 | 82.30 | 0.0699 |
| AD | – | 3,480.97 | 3,480.97 | 1,505.08 | 0.0164 |
| AE | – | 165.97 | 165.97 | 71.76 | 0.0748 |
| BD | – | 180.41 | 180.41 | 78.00 | 0.0718 |
| DE | – | 68.17 | 68.17 | 29.48 | 0.1160 |
| Residual | 1 | 2.31 | 2.31 | ||
| Corrected total | 11 | 3.514E+005 |
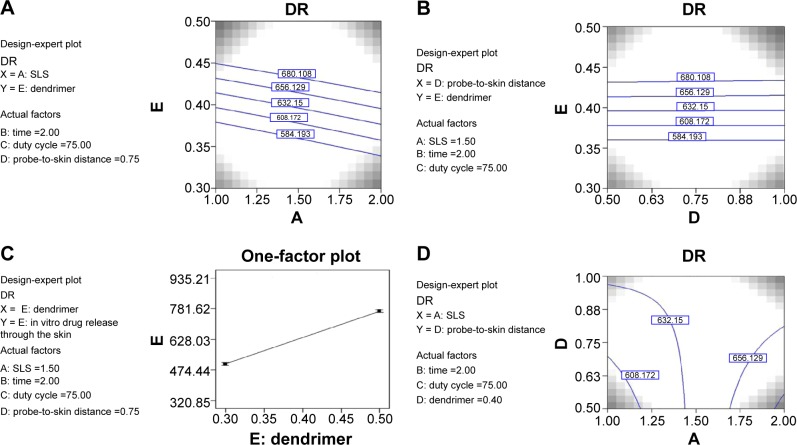
Figure 1.
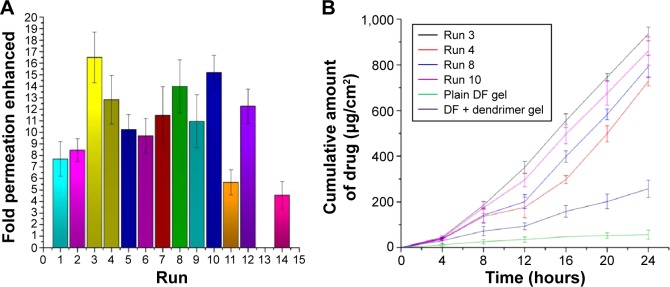
Comparative permeation enhancement effect of dendrimer on DF.
Notes: (A) Runs 1–12 represent the number-fold enhancements of permeation of diclofenac (DF) after ultrasonic treatment to skin at different conditions (run 3 shows maximum enhancement of 16.5-fold, while run 11 shows 5.5-fold enhancement). Run 14 shows the effect of dendrimer on untreated skin. (B) Comparative permeation enhancement of selected runs with plain DF gel. Run 3, run 4, run 8, and run 10 had maximum permeation-enhancement effects compared to other runs and plain DF gel.
Effect of dendrimer concentration
Dendrimers are potential skin-permeation enhancers.19,20 The potential of dendrimers as permeation enhancers has been demonstrated by enhancing the permeation of 5-fluorouracil and indomethacin through the skin. In this experiment, further enhancement of the permeation potential of dendrimers using sonophoresis treatment was studied. From Figure 1B, it is clear that plain DF gel (without dendrimer) and without ultrasound treatment to skin (passive delivery) showed 56.69 µg/cm2 cumulative drug permeated through the skin, while DF dendrimer gel without sonophoresis treatment (run 14) showed 257.3 µg/cm2 cumulative drug permeated through the skin. This enhancement was 4.54-fold compared to plain DF gel. However, when the same gel was applied to sonophoresis-treated skin, drastic permeation enhancement was observed. In the case of run 3, the dendrimer concentration was 0.5 mL in gel, and cumulative drug permeated through the skin was 935.21 µg/cm2. From this, it is clear that 16.5-fold permeation was enhanced when dendrimer was coupled with ultrasonic treatment to the skin.
From the contour plots (Figure 2A and B), it can be concluded that as the concentration of dendrimer increases, permeation through the skin also increases. The effect of dendrimer concentration on skin permeation was found to be statistically significant (P=0.0028). Also, Figure 2C shows the effect of one factor ie, dendrimer, on skin permeation of DF. From this, it is also clear that as the concentration of dendrimer increases, the skin permeation also increases. Permeation enhancers are small molecules that cause skin irritation or irreversibly alter the skin barrier to penetrate the skin in significant amounts.45,46 Among these permeation enhancers, dendrimers have proved to be a potential tool for enhanced delivery of drugs through the skin. Dendrimers have proved to be very potent chemicals in DDS. Earlier studies have shown that dendrimers increases the solubility of drugs in water through complexation with the surface functional groups and/or encapsulation within the dendrimer core.19,20,43,47–49 Dendrimers are monodisperse hyperbranched polymers with a core–shell architecture containing a high density of tunable surface-functional groups. Dendrimers have a spherical architecture that provides a compact structure with a small hydrodynamic radius (1–10 nm) for transport across biological membranes.50 Due to these unique features, dendrimers have been widely investigated as drug and gene carriers by various routes of administration.51 Dendrimers act as a carrier and transport the drug in the solubilized form to the skin surface, from where it partitions into the SC, due to the high affinity of the lipophilic drug for skin lipids.
Figure 2.
Contour plots showing the effect of independent variables on skin permeation of DF.
Notes: (A) Combined effect of dendrimer and sodium lauryl sulfate (SLS) on skin permeation-enhancement effect of diclofenac (DF) through the skin. Both factors showed linear enhancement in permeation. (B) Combined effect of dendrimer and probe-to-skin distance on skin permeation-enhancement effect of DF through the skin. Both factors show linear enhancement in permeation. (C) Effect of single-factor dendrimer on skin permeation of DF. The effect was statistically significant (P=0.0028) on DF permeation through the skin. (D) Combined effect of SLS and probe-to-skin distance on skin permeation-enhancement effect of DF through the skin.
In earlier studies, dendrimer increased the permeation of drugs by increasing its water solubility through complexation with the surface functional groups and/or encapsulation within the dendrimer core.19,20 This per meation-enhancement effect was coupled with ultrasonic treatment on the skin that led to more permeation of DF through skin. Due to ultrasonic wave treatment through the coupling media, the medium absorbs the ultrasonic beam, which leads to a rise in temperature of the medium and causes a thermal effect. This thermal effect is responsible for the change in permeation behavior of the skin.52,53 Also, the cavitation site of action is responsible for the permeation-enhancement effect. This cavitation takes place through the creation of gaseous bubbles. After a few ultrasonic cycles, these bubbles get collapsed either inside or outside the skin. The transient bubbles get collapsed in the donor compartment to produce a shock wave with an amplitude of about 10 kbar, which perturbs the structure of the SC.54 All these events finally lead to permeation enhancement of active molecules through the skin.
Effect of sodium lauryl sulfate on skin permeation
During sonophoretic treatment of skin, SLS 1% and 2% was used as a coupling medium. It is an already proven fact that SLS enhances drug delivery several-fold when used alone. In this experiment, passive diffusion of DF from the gel (without dendrimer) was also tested without ultrasound treatment to the skin. In this case (run 13), 56.69 µg/cm2 cumulative drug permeated through the skin during 24 hours. However, due to SLS treatment at varying concentrations, DF permeation through the skin was improved. The contour plots (Figure 2A and D, and Figure 3A) show the combined effect of SLS concentration and other factors on DF skin permeation. It was clear that as the concentration of SLS increased, the skin permeation of DF also increased. The effect of SLS concentration (1% and 2%) was found to be statistically significant on DF skin permeation. Also, from Figure 3B, the same conclusion can be drawn, which shows the effect of a single factor on DF skin permeation. Iontophoretic fluxes of propranolol hydrochloride were effectively increased twofold in the SC pretreated with SLS.55 The use of SLS as a coupling media resulted in increases in dimensions of lacunar regions. It is also claimed that SLS is responsible for the increasing pore radii of sonophoresis-treated skin.56 Due to sonophoretic treatment, there may be chances of imperfections in the SC that led to increased DF skin permeation. Sonophoresis–SLS treatment leads to more consistent skin perturbation in comparison to sonophoresis treatment alone.
Figure 3.
Contour plots and one factor plot showing the effect of independent variables on skin permeation of DF.
Notes: (A) Combined effect of sodium lauryl sulfate (SLS) and time of ultrasound application on skin permeation-enhancement effect of diclofenac (DF) through the skin. Both factors showed linear enhancement in permeation. (B) Effect of single-factor SLS concentration on skin permeation of DF. The effect was statistically significant (P=0.0134) on DF permeation through the skin. (C) Combined effect of ultrasonic application time and probe-to-skin distance on skin permeation-enhancement effect of DF through the skin. (D) Effect of single-factor ultrasound-application time on skin permeation of DF. The effect was statistically significant (P=0.0077) on DF permeation through the skin.
Effect of ultrasound-application time
It is a well-known fact that ultrasound treatment to skin causes the permeation enhancement of active molecules. This permeation intensity depends on the intensity, frequency, and application time of the ultrasound. In this experiment. the frequency was kept constant at 20 kHz. Before application of the gel, the skin was treated with ultrasound with a probe sonicator at different time periods. The aim was to find out the effect of ultrasound treatment on DF skin permeation. One experiment was also conducted without the application of ultrasound treatment to the skin. The effect of ultrasound-application time was studied at two different levels: −1 and +1. From Figure 3A and C, it is clear that as the ultrasound-application time increased, DF skin permeation also increased. Figure 3D shows the effect of a single factor (application time) on skin permeation. This clearly indicates that ultrasound treatment had a positive effect on the skin-permeation studies. Statistically, the effect of sonophoresis was found to be significant (P=0.0193). These results are similar with a study conducted on transdermal insulin.57
Effect of probe-to-skin distance
To investigate the effect of probe-to-skin distance on DF permeation, the experiment was performed at two different levels (−1 and +1). In this experiment, the working distance was maintained at 0.5 cm and 1 cm between the skin and the probe. As the distance between the skin and the probe increased, the percentage drug release, ie, permeation of drugs, decreased.27 The same conclusion could be drawn from this experiment also. It can also be proved from Figure 4A (single-factor graph). From Figure 2B and D, and Figure 3D, it is clear that as the distance increased, the permeation effect decreased. However, this permeation-enhancement effect was not statistically significant (P=0.4172). It was found that generation of small holes and cavitation within the surface of the skin enhanced the permeation of active molecules through the skin. Increasing the distance between the probe and the skin reduced the cavitation effect on the skin, hence decreasing the permeability.
Figure 4.
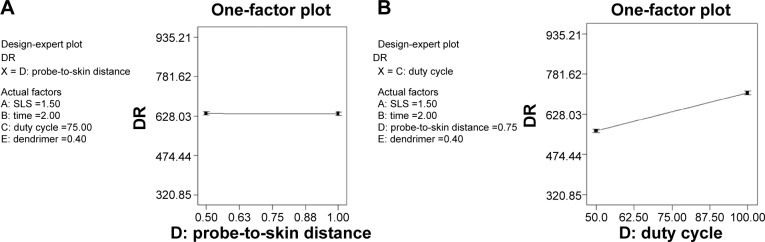
One factor plot showing the effect of probe to skin distance and duty cycle on drug release.
Notes: (A) Effect of single-factor probe-to-skin distance on skin permeation of diclofenac (DF). The effect was statistically insignificant (P=0.4172) on DF permeation through the skin. As the distance between the probe and skin increased, permeation decreased and vice versa. (B) Effect of single-factor duty cycle on skin permeation of DF. The effect was statistically significant (P=0.0054) on DF permeation through the skin. As the duty cycle increased (from 50% to 100%), permeation increased.
Effect of duty cycle
In this experiment, ultrasound was applied in pulsed (sequential) and continuous mode (100% duty cycle). Due to the application of ultrasound, a rise in temperature of coupling media occurs. This rise in temperature effect is faster and more intense with the continuous mode. Transdermal diffusion of prednisolone was increased in vitro by two- to fivefold when exposure time was increased from 10 to 60 minutes with 1 MHz ultrasound at intensity 4.3 W/cm2 in continuous mode.56 The pulsed mode is frequently used, because it reduces the severity of such side effects as thermal effects. Transdermal permeation of fentanyl was more effective with the pulsed mode of sonophoresis.58 In the present study also, similar results were observed. From Figure 4B, it is clear that DF skin permeation increased in the 100% duty cycle compared to the 50% duty cycle. The effect of duty cycle was found to be statistically significant (P=0.0054).
Conclusion
The present study reported a novel permeation-enhancement technique based on dendrimer-coupled sonophoresis for the transdermal drug delivery of DF. The TDDS was developed using a Plackett–Burman statistical design. The effect of all independent variables on permeation enhancement was found to be statistically significant. Dendrimer-coupled sonophoresis delivery increased DF permeation by 16.5-fold. From this study, it can be concluded that dendrimer-coupled sonophoresis is a novel technique to enhance the skin permeation of active molecules.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Nishihata T, Kamada A, Sakai K, et al. Percutaneous absorption of diclofenac in rats and humans: aqueous gel formulation. Int J Pharm. 1988;46:1–7. [Google Scholar]
- 2.Sharquie KE, Al-Hamamy HM, Noaimib AA, Al-Shawi IA, Adil AN, Israa AA. Treatment of pityriasis versicolor using 1% diclofenac gel and clotrimazole cream (comparative therapeutic study) J Saudi Soc Dermatol Dermatol Surg. 2011;15:19–23. [Google Scholar]
- 3.Asasutjarit R, Thanasanchokpibull S, Fuongfuchat A, Veeranondha S. Optimization and evaluation of thermoresponsive diclofenac sodium ophthalmic in situ gels. Int J Pharm. 2011;411:128–135. doi: 10.1016/j.ijpharm.2011.03.054. [DOI] [PubMed] [Google Scholar]
- 4.Dugowson CE, Gnanashanmugam P. Nonsteroidal anti-inflammatory drugs. Phys Med Rehabil Clin N Am. 2006;17:347–354. doi: 10.1016/j.pmr.2005.12.012. [DOI] [PubMed] [Google Scholar]
- 5.Chan FK, Hung LC, Suen BY, et al. Celecoxib versus diclofenac plus omeprazole in high risk arthritis patients: results of a randomized double-blind trial. Gastroenterology. 2004;127:1038–1043. doi: 10.1053/j.gastro.2004.07.010. [DOI] [PubMed] [Google Scholar]
- 6.Wong VW, Chan FK. Review: Misoprostol or COX-2-specific or selective NSAIDs reduce gastrointestinal complications and symptomatic ulcers. ACP J Club. 2005;142:75. [PubMed] [Google Scholar]
- 7.O’Neil MJ, Heckelman PE, Koch CB, Roman KJ, Kenny CM, D’Arecca MR. The Merck Index. 14th ed. New York: Merck; 2006. [Google Scholar]
- 8.US Food Drug Administration Diclofenac [prescribing information] [Accessed March 03, 2015]. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2011/021005s013lbl.pdf.
- 9.Rostom A, Dube C, Wells G, et al. Prevention of NSAID-induced gastroduodenal ulcers. Cochrane Database Syst Rev. 2002;4:CD002296. doi: 10.1002/14651858.CD002296. [DOI] [PubMed] [Google Scholar]
- 10.Silverstein FE, Faich G, Goldstein JL, et al. Gastrointestinal toxicity with celecoxib vs nonsteroidal anti-inflammatory drugs for osteoarthritis and rheumatoid arthritis. The CLASS study: a randomized controlled trial. JAMA. 2008;284:1247–1255. doi: 10.1001/jama.284.10.1247. [DOI] [PubMed] [Google Scholar]
- 11.Nesseem DI, Eid SF, El-Houseny SS. Development of novel transdermal self-adhesive films for tenoxicam, an anti-inflammatory drug. Life Sci. 2011;89:430–438. doi: 10.1016/j.lfs.2011.06.026. [DOI] [PubMed] [Google Scholar]
- 12.Khurana S, Jain NK, Bedi PM. Development and characterization of a novel controlled release drug delivery system based on nanostructured lipid carriers gel for meloxicam. Life Sci. 2013;93:763–772. doi: 10.1016/j.lfs.2013.09.027. [DOI] [PubMed] [Google Scholar]
- 13.Mazzenga GC, Berner B. The transdermal delivery of zwitterionic drugs I: the solubility of zwitterion salts. J Control Release. 1991;16:77–88. [Google Scholar]
- 14.Ma M, Cheng Y, Xu Z, et al. Evaluation of polyamidoamine (PAMAM) dendrimers as drug carriers of anti-bacterial drugs using sulfamethoxazole (SMZ) as a model drug. Eur J Med Chem. 2007;42:93–98. doi: 10.1016/j.ejmech.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 15.Bosnjakovic A, Mishra MK, Ren W, et al. Poly(amidoamine) dendrimer-erythromycin conjugates for drug delivery to macrophages involved in periprosthetic inflammation. Nanomedicine. 2011;7:284–294. doi: 10.1016/j.nano.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 16.Choksi A, Sarojini KV, Vadnal P, Dias C, Suresh PK, Khandare J. Comparative anti-inflammatory activity of poly(amidoamine) (PAMAM) dendrimer-dexamethasone conjugates with dexamethasone-liposomes. Int J Pharm. 2013;449:28–36. doi: 10.1016/j.ijpharm.2013.03.056. [DOI] [PubMed] [Google Scholar]
- 17.Gupta U, Agashe HB, Asthana A, Jain NK. Dendrimers: novel polymeric nanoarchitectures for solubility enhancement. Biomacromolecules. 2006;7:649–658. doi: 10.1021/bm050802s. [DOI] [PubMed] [Google Scholar]
- 18.Wang Z, Itoh Y, Hosaka Y, et al. Novel transdermal drug delivery system with polyhydroxyalkanoate and starburst polyamidoamine dendrimer. J Biosci Bioeng. 2003;95:541–543. doi: 10.1016/s1389-1723(03)80059-2. [DOI] [PubMed] [Google Scholar]
- 19.Chauhan AS, Sridevi S, Chalasani KB, et al. Dendrimer-mediated transdermal delivery: enhanced bioavailability of indomethacin. J Control Release. 2003;90:335–343. doi: 10.1016/s0168-3659(03)00200-1. [DOI] [PubMed] [Google Scholar]
- 20.Venuganti VV, Perumal OP. Effect of poly(amidoamine) (PAMAM) dendrimer on skin permeation of 5-fluorouracil. Int J Pharm. 2008;361:230–238. doi: 10.1016/j.ijpharm.2008.05.034. [DOI] [PubMed] [Google Scholar]
- 21.Vargese E, Khar RK. Enhanced skin permeation of diclofenac by iontophoresis: in vitro and in vivo studies. J Control Release. 1996;38:21–27. [Google Scholar]
- 22.Motta AF, Borges NG, Jr, da Fonseca JC, Tonussi CR. The antinociceptive effect of iontophoretic direct application of diclofenac to arthritic knee-joints of rats. Life Sci. 2003;73:1995–2004. doi: 10.1016/s0024-3205(03)00539-3. [DOI] [PubMed] [Google Scholar]
- 23.Polat BE, Figueroa PL, Blankschtein D, Langer R. Transport pathways and enhancement mechanisms within localized and non-localized transport regions in skin treated with low-frequency sonophoresis and sodium lauryl sulfate. J Pharm Sci. 2011;100:512–529. doi: 10.1002/jps.22280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Polat BE, Hart D, Langer R, Blankschtein D. Ultrasound-mediated transdermal drug delivery: mechanisms, scope, and emerging trends. J Control Release. 2011;152:330–348. doi: 10.1016/j.jconrel.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tang H, Wang CC, Blankschtein D, Langer R. An investigation of the role of cavitation in low-frequency ultrasound-mediated transdermal drug transport. Pharm Res. 2002;19:1160–1169. doi: 10.1023/a:1019898109793. [DOI] [PubMed] [Google Scholar]
- 26.Souza J, Meira A, Volpato NM, Mayorga P, Gottfried C. Effect of phonophoresis on skin permeation of commercial anti-inflammatory gels: sodium diclofenac and ketoprofen. Ultrasound Med Biol. 2013;39:1623–1630. doi: 10.1016/j.ultrasmedbio.2013.02.009. [DOI] [PubMed] [Google Scholar]
- 27.Herwadkar A, Sachdev V, Taylor LF, Silver H, Banga AK. Low frequency sonophoresis mediated transdermal and intradermal delivery of ketoprofen. Int J Pharm. 2012;423:289–296. doi: 10.1016/j.ijpharm.2011.11.041. [DOI] [PubMed] [Google Scholar]
- 28.Ueda H, Mutoh M, Seki T, Kobayashi D, Morimoto Y. Acoustic cavitation as an enhancing mechanism of low-frequency sonophoresis for transdermal drug delivery. Biol Pharm Bull. 2009;32:916–920. doi: 10.1248/bpb.32.916. [DOI] [PubMed] [Google Scholar]
- 29.Ueda H, Sugibayashi K, Morimoto Y. Skin penetration-enhancing effect of drugs by phonophoresis. J Control Release. 1995;37:291–297. [Google Scholar]
- 30.Osborne JL, Sanchez IC, Paul DR. An asymptotic analysis of drug delivery from transdermal patches. J Memb Sci. 2013;442:27–30. [Google Scholar]
- 31.Kim MH, Park DH, Yang JH, Choy YB, Choy JH. Drug-inorganic-polymer nanohybrid for transdermal delivery. Int J Pharm. 2013;444:120–127. doi: 10.1016/j.ijpharm.2012.12.043. [DOI] [PubMed] [Google Scholar]
- 32.Mura P, Bragagni M, Mennini N, Cirri M, Maestrelli F. Development of liposomal and microemulsion formulations for transdermal delivery of clonazepam: effect of randomly methylated β-cyclodextrin. Int J Pharm. 2014;475:306–314. doi: 10.1016/j.ijpharm.2014.08.066. [DOI] [PubMed] [Google Scholar]
- 33.Delgado-Charro MB, Guy RH. Effective use of transdermal drug delivery in children. Adv Drug Deliver Rev. 2014;73:63–82. doi: 10.1016/j.addr.2013.11.014. [DOI] [PubMed] [Google Scholar]
- 34.Alexander A, Dwivedi S, Ajazuddin M, et al. Approaches for breaking the barriers of drug permeation through transdermal drug delivery. J Control Release. 2012;164:26–40. doi: 10.1016/j.jconrel.2012.09.017. [DOI] [PubMed] [Google Scholar]
- 35.El-Nabarawi MA, Bendas ER, El Rehem RT, Abary MY. Transdermal drug delivery of paroxetine through lipid-vesicular formulation to augment its bioavailability. Int J Pharm. 2013;443:307–317. doi: 10.1016/j.ijpharm.2013.01.016. [DOI] [PubMed] [Google Scholar]
- 36.Elias PM, Friend DS. The permeability barrier in mammalian epidermis. J Cell Biol. 1975;65:180–191. doi: 10.1083/jcb.65.1.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gao S, Singh J. Mechanism of transdermal transport of 5-fluorouracil by terpenes: carvone, 1,8-cineole and thymol. Int J Pharm. 1997;154:67–77. [Google Scholar]
- 38.Prausnitz MR, Mitragotri S, Langer R. Current status and future potential of transdermal drug delivery. Nat Rev Drug Discov. 2004;3:115–124. doi: 10.1038/nrd1304. [DOI] [PubMed] [Google Scholar]
- 39.Kalia YN, Guy RH. Modeling transdermal drug release. Adv Drug Deliver Rev. 2001;48:159–172. doi: 10.1016/s0169-409x(01)00113-2. [DOI] [PubMed] [Google Scholar]
- 40.Azagury A, Khoury L, Enden G, Kost J. Ultrasound mediated transdermal drug delivery. Adv Drug Deliver Rev. 2014;72:127–143. doi: 10.1016/j.addr.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 41.Pikal MJ. The role of electroosmotic flow in transdermal iontophoresis. Adv Drug Deliver Rev. 1992;9:201–237. doi: 10.1016/s0169-409x(00)00138-1. [DOI] [PubMed] [Google Scholar]
- 42.Langer R. Transdermal drug delivery: past progress, current status, and future prospects. Adv Drug Deliver Rev. 2004;56:557–558. doi: 10.1016/j.addr.2003.10.021. [DOI] [PubMed] [Google Scholar]
- 43.El-Malah Y, Nazzal S. Hydrophilic matrices: application of Placket-Burman screening design to model the effect of POLYOX-carbopol blends on drug release. Int J Pharm. 2006;309:163–170. doi: 10.1016/j.ijpharm.2005.11.032. [DOI] [PubMed] [Google Scholar]
- 44.Wang P, Wang ZW, Wu ZC. Insights into the effect of preparation variables on morphology and performance of polyacrylonitrile membranes using Plackett-Burman design experiments. Chem Eng J. 2012;193–194:50–58. [Google Scholar]
- 45.He N, Warner KS, Higuchi WI, Li SK. Model analysis of flux enhancement across hairless mouse skin induced by chemical permeation enhancers. Int J Pharm. 2005;297:9–21. doi: 10.1016/j.ijpharm.2005.01.041. [DOI] [PubMed] [Google Scholar]
- 46.Pfister WR, Hsieh DS. Permeation enhancers compatible with trans-dermal drug delivery systems. Part I: selection and formulation considerations. Med Device Technol. 1990;1:48–55. [PubMed] [Google Scholar]
- 47.Cheng Y, Man N, Xu T, et al. Transdermal delivery of nonsteroidal anti-inflammatory drugs mediated by polyamidoamine (PAMAM) dendrimers. J Pharm Sci. 2007;96:595–602. doi: 10.1002/jps.20745. [DOI] [PubMed] [Google Scholar]
- 48.Park D, Park H, Seo J, Lee S. Sonophoresis in transdermal drug deliverys [sic] Ultrasonics. 2014;54:56–65. doi: 10.1016/j.ultras.2013.07.007. [DOI] [PubMed] [Google Scholar]
- 49.Park D, Ryu H, Kim HS, et al. Sonophoresis using ultrasound contrast agents for transdermal drug delivery: an in vivo experimental study. Ultrasound Med Biol. 2012;38:642–650. doi: 10.1016/j.ultrasmedbio.2011.12.015. [DOI] [PubMed] [Google Scholar]
- 50.Kitchens KM, El-Sayed M, Ghandehari H. Transepithelial and endothelial transport of poly(amidoamine) dendrimers. Adv Drug Deliv Rev. 2005;57:2163–2176. doi: 10.1016/j.addr.2005.09.013. [DOI] [PubMed] [Google Scholar]
- 51.Cheng Y, Xu Z, Ma M, Xu T. Dendrimers as drug carriers: applications in different routes of drug administration. J Pharm Sci. 2008;97:123–143. doi: 10.1002/jps.21079. [DOI] [PubMed] [Google Scholar]
- 52.Cagnie B, Vinck E, Rimbaut S, Vanderstraeten G. Phonophoresis versus topical application of ketoprofen: comparison between tissue and plasma levels. Phys Ther. 2003;83:707–712. [PubMed] [Google Scholar]
- 53.Merino G, Kalia YN, Delgado-Charro MB, Potts RO, Guy RH. Frequency and thermal effects on the enhancement of transdermal transport by sonophoresis. J Control Release. 2003;88:85–94. doi: 10.1016/s0168-3659(02)00464-9. [DOI] [PubMed] [Google Scholar]
- 54.Lavon I, Grossman N, Kost J, Kimmel E, Enden G. Bubble growth within the skin by rectified diffusion might play a significant role in sonophoresis. J Control Release. 2007;117:246–255. doi: 10.1016/j.jconrel.2006.10.027. [DOI] [PubMed] [Google Scholar]
- 55.Chesnoy S, Durand D, Doucet J, Couarraze G. Structural parameters involved in the permeation of propranolol HCl by iontophoresis and enhancers. J Control Release. 1999;58:163–175. doi: 10.1016/s0168-3659(98)00155-2. [DOI] [PubMed] [Google Scholar]
- 56.Seto JE, Polat BE, Lopez RF, Blankschtein D, Langer R. Effects of ultrasound and sodium lauryl sulfate on the transdermal delivery of hydrophilic permeants: comparative in vitro studies with full-thickness and split-thickness pig and human skin. J Control Release. 2010;145:26–32. doi: 10.1016/j.jconrel.2010.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lee S, Snyder B, Newnham RE, Smith NB. Noninvasive ultrasonic transdermal insulin delivery in rabbits using the light-weight cymbal array. Diabetes Technol Ther. 2004;6:808–815. doi: 10.1089/dia.2004.6.808. [DOI] [PubMed] [Google Scholar]
- 58.Boucaud A, Machet L, Arbeille B, et al. In vitro study of low-frequency ultrasound-enhanced transdermal transport of fentanyl and caffeine across human and hairless rat skin. Int J Pharm. 2001;228:69–77. doi: 10.1016/s0378-5173(01)00820-1. [DOI] [PubMed] [Google Scholar]