Summary
Frey’s syndrome in children is rare and often erroneously attributed to food allergy. Here we describe a case of Frey’s syndrome in an infant and provide a review of the literature. Awareness of this condition is important for the Otolaryngologist in order to avoid unnecessary medical costs and procedures and provide reassurance to both parents and primary care providers in the setting of this benign condition.
Keywords: Infantile, Pediatric, Frey’s, Auriculotemporal nerve, Flushing
1. Introduction
Frey’s syndrome is a well-known phenomenon in adults. It is a common postoperative complication of parotid gland surgery, manifested as sweating and/or dermal flushing during salivary stimulation [1]. In the pediatric population, however, it is rare and often misdiagnosed as food allergy prompting unnecessary diagnostic testing and treatment [2]. In infants, Frey’s syndrome is thought to result from perinatal trauma to parasympathetic branches of the auriculotemporal nerve associated with forceps assistance at the time of delivery [3].
2. Case report
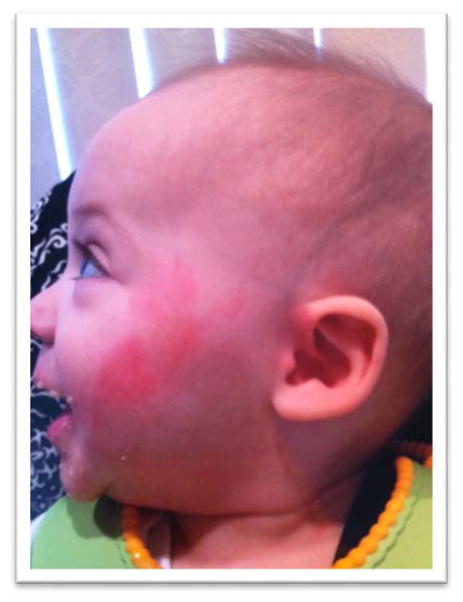
A 9 month old male presented to the Pediatric Otolaryngology clinic for evaluation of periodic left-sided facial flushing. The flushing was first noticed upon introduction of solid foods at the age of 6 months. The onset was typically 30–60 seconds after eating, with complete resolution within 30–60 minutes after a meal. The left facial erythema was concentrated over the distribution of the auriculotemporal nerve and was more pronounced with sweet, sour, or new foods. It was also occasionally elicited with vigorous chewing of toys. There was no associated sweating, pruritus, swelling or perceived discomfort.
The patient’s past medical history was notable for delivery at term with forceps assistance resulting in left malar ecchymosis (Fig. 1). He also was diagnosed with left sided torticollis that was treated conservatively. There was no history of prior surgery, trauma or food allergy. He was self-referred by his mother, who independently researched his symptoms and believed he was exhibiting a clinical picture consistent with Frey’s syndrome despite others expressing concern for possible food allergy.
Figure 1.
The patient shortly after birth demonstrating left facial ecchymosis from forceps assisted delivery.
In the Pediatric Otolaryngology clinic, the child was observed in the examination room after eating bananas. Within one minute he developed left facial erythema extending from the left temple, across the malar eminence and inferiorly to the left oral commissure (Fig. 2). There was no associated sweating, swelling, respiratory distress or facial motion asymmetry. The erythema began to fade within 10 minutes and completely resolved in 40 minutes. Given the patient’s history and physical exam findings, Frey’s syndrome was confirmed and it was determined that no further workup or treatment was necessary.
Figure 2.
The patient at 9 months old demonstrating left facial flushing shortly after eating bananas.
3. Discussion
Frey’s syndrome, also known as auriculotemporal nerve syndrome or gustatory sweating and flushing, was first described by Duphenix in 1757 [4]. The syndrome is named for Lucja Frey, a Polish neurologist, who identified the role of the auriculotemporal nerve in 1923 [5] (Fig. 3). The auriculotemporal nerve is a branch of the mandibular (third) division of the trigeminal nerve. It exits the skull via the foramen ovale, turns superiorly, anterior to the external auditory canal, and parallels the superficial temporal vessels to innervate the scalp. The nerve carries postganglionic parasympathetic fibers originating in the inferior salivatory nucleus from the otic ganglion to the parotid gland, which stimulate secretion. The most widely accepted mechanism for development of Frey’s syndrome is that it results from aberrant reinnervation of cholinergic sympathetic sweat glands and blood vessels in the skin with postganglionic parasympathetic fibers from the auriculotemporal nerve that have been exposed or injured. This most commonly follows parotid gland surgery [1], though other etiologies include facial trauma, carotid endarterectomy, thyroidectomy, other salivary gland surgery, herpes zoster infections, and neurofibromatosis [3, 6].
Figure 3.
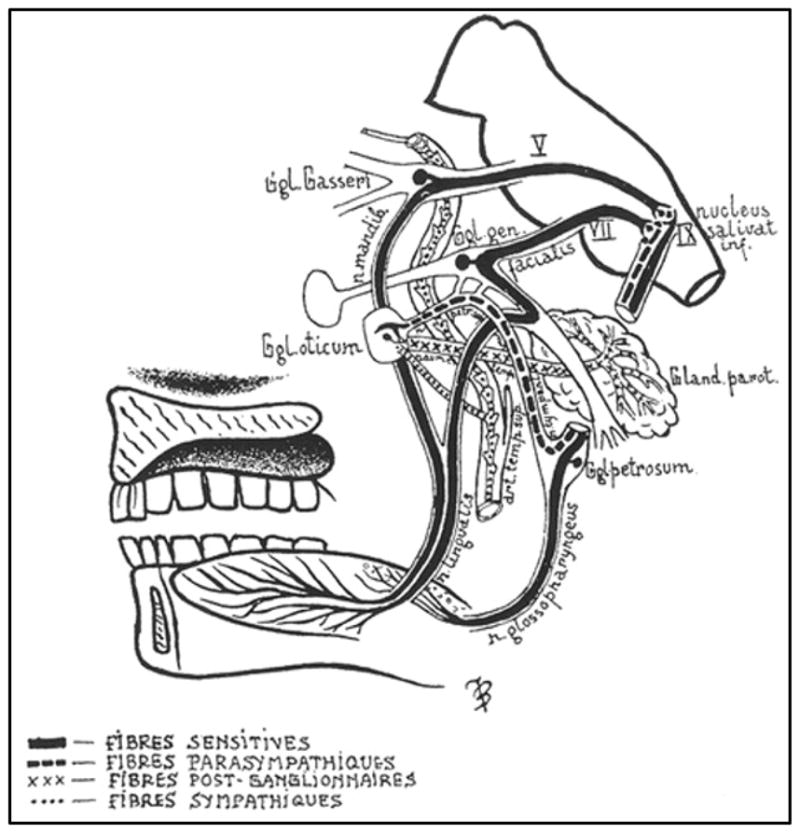
Auriculotemporal nerve anatomy described by Lucja Frey in 1923.
The disorder is rare in children and thought to result from local trauma to the parotid region during delivery, especially if forceps assistance it needed, as was the case for our patient [7]. In children, there is often only the presence of gustatory flushing over the cheek without sweating [7, 8]. This has occasionally been referred to as “incomplete Frey’s syndrome” or “atypical Frey’s syndrome” [9, 10]. The flushing can be quite distressing to individuals and families, even in the absence of other symptoms. Given that many of these cases present when the child first starts to take in a greater variety of foods, concern for food allergies is common [2].
In Frey’s syndrome, the presentation tends to be unilateral with a segmental distribution (consistent with the auriculotemporal nerve), limited to erythema, lacking sweating, and without itching, angioedema, respiratory, or gastrointestinal symptoms. Food allergies are far more likely to involve the bilateral face and skin of other anatomic regions as well as to be accompanied by itching, edema, respiratory, or gastrointestinal symptoms. Foods commonly stimulating the erythema of Frey’s syndrome include citrus, vegetables, and sweet foods. Food allergies are more commonly attributed to cow’s milk, egg, soy, wheat, peanuts, fish, and shellfish [11]. In the absence of symptoms beyond localized, segmentally distributed erythema that appears with feeding and resolves within minutes to hours, no allergy work up is necessary [12, 13, 14]. There are several accounts of spontaneous resolution of erythema over the course of months to years [7, 8]. For refractory cases that are bothersome to the patient, one could consider local intradermal injection of botulinum toxin; however, no treatment for this benign condition is necessary [15].
4. Conclusion
Awareness of this condition by the Otolaryngologist is important to avoid unnecessary medical costs and provide reassurance to both parents and primary care providers.
Supplementary Material
References
- 1.Johnson J, Newlands S, Bailey B. Head and Neck Surgery – Otolaryngology. 4. Lippincott, Williams & Wilkins; 2006. [Google Scholar]
- 2.Giovannini-Chami L, Blanc S, Albertini M, et al. Frey’s syndrome: differential diagnosis of food allergy. Arch Dis Child. 2014;99(5):457. doi: 10.1136/archdischild-2013-305508. [DOI] [PubMed] [Google Scholar]
- 3.Kaddu S, Smolle J, Komericki P, et al. Auriculotemporal (Frey) syndrome in late childhood: an unusual variant presenting as gustatory flushing mimicking food allergy. Pediatr Dermatol. 2000;17:126–128. doi: 10.1046/j.1525-1470.2000.01729.x. [DOI] [PubMed] [Google Scholar]
- 4.Clayman A, Clayman S, Sengle M. A review of the surgical and medical treatment of Frey syndrome. Ann Plast Surg. 2006;57:581–584. doi: 10.1097/01.sap.0000237085.59782.65. [DOI] [PubMed] [Google Scholar]
- 5.Frey L. Le syndrome du nerf auriculo-temporal. Rev Neurol. 1923;2:97–104. [Google Scholar]
- 6.Caulley L, Hong P. Pediatric auriculotemporal nerve (Frey) syndrome. CMAJ. 2013;6:185. doi: 10.1503/cmaj.120443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dizon M, Fischer G, Jopp-McKay A, et al. Localized facial flushing in infancy Auriculotemporal nerve (Frey) syndrome. Arch Dermatol. 1997;133:1143–1145. [PubMed] [Google Scholar]
- 8.Cliff S, Lever R, Moss A, et al. Frey’s syndrome without hyperhidrosis. Journal of the Royal Society of Medicine. 1998;91(7):388–9. doi: 10.1177/014107689809100714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thoma-Uszynski S, Mahler V. Incomplete auriculotemporal nerve syndrome--mimicry of oral allergy syndrome. European Journal of Dermatology : EJD. 2007;17(2):157–9. doi: 10.1684/ejd.2007.0131. [DOI] [PubMed] [Google Scholar]
- 10.Güerrissi J, Stoyanoff J. Atypical Frey syndrome as a complication of Obwegeser osteotomy. The Journal of Craniofacial Surgery. 1998;9(6):543–547. doi: 10.1097/00001665-199811000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Sethuraman S, Mancini A. Familial Auriculotemporal Nerve (Frey) Syndrome. Pediatric Dermatology. 2009;26:302–305. doi: 10.1111/j.1525-1470.2009.00909.x. [DOI] [PubMed] [Google Scholar]
- 12.Humphrey J, Black G, Wild L. Facial Flushing with food: the auriculotemporal syndrome. J Gen Intern Med. 2013;28(3):475–476. doi: 10.1007/s11606-012-2175-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ott H, Brost H, Poblete-Gutiérrez P, et al. Auriculotemporal syndrome in childhood. Acta Dermato-Venereologica. 2004;84(2):160–161. doi: 10.1080/00015550310006239. [DOI] [PubMed] [Google Scholar]
- 14.Hussain N, Dhanarass M, Whitehouse W. Frey’s syndrome: a masquerader of food allergy. Postgraduate Medical Journal. 2010;86:62. doi: 10.1136/pgmj.2009.090225. [DOI] [PubMed] [Google Scholar]
- 15.Von Lindern J, Niederhagen B, Berge G, et al. Frey syndrome: treatment with type A botulinum toxin. Cancer. 2000;89:1659–1663. doi: 10.1002/1097-0142(20001015)89:8<1659::aid-cncr2>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.