Abstract
Background
Alcohol dependence/abuse and depression are positively related. Prior studies focused on relationships between drinking and driving and alcohol dependence/abuse, drinking and driving and problem drinking, or drinking and driving and depression separately. No study has addressed how depression is linked to drinking and driving through various underlying channels in the same study.
Methods
This study investigated relationships between depression, alcohol dependence/abuse, and the number of self-reported drinking and driving episodes. We also explored underlying behavioral channels between depression and alcohol dependence/abuse and binge drinking, reducing drinking amounts when planning to drive, and use of designated drivers. Data on 1,634 drinkers came from a survey fielded in eight U.S. cities. We employed ordinary least squares regression (OLS) and path analysis to assess drinking and driving and underlying channels.
Results
With OLS, being depressed increased the number of drinking and driving episodes during the past year by 0.572. This increase decreased to 0.411 episodes/year increase after adding socio-demographic characteristics and household income and lost statistical significance after controlling for alcohol dependence/abuse. The path analysis showed that depression is positively associated with drinking and driving, indirectly operating through not using a designated driver, but is not directly associated with drinking and driving. Alcohol dependence/abuse is directly associated with drinking and driving, and indirectly with drinking and driving through binge drinking.
Conclusion
Our results suggest that treatment should focus on helping individuals with depression to obtain assistance from others, such as obtaining a designated driver. Since self-control of drinking in anticipation of driving did not significantly reduce drinking and driving episodes, this study finds no empirical support for emphasizing improved self-control when the treatment objective is reducing drinking and driving frequency. While binge drinking is associated with drinking and driving, the more appropriate way to influence binge drinking is treating alcohol dependence/abuse rather than depression per se.
Keywords: depression, drinking and driving, alcohol dependence/abuse, designated driver, binge drinking, self-control
1. Introduction
Drinking and driving causes a substantial share of motor vehicle injuries.1 A comprehensive understanding of the risk factors for drinking and driving is important for proposing effective prevention strategies. Alcohol dependence/abuse and depression are positively related. Prevalence of depression is higher among persons arrested for driving while intoxicated (DWI) than in the general population.2,3 Persons with depressive symptoms are more likely to drink and drive.4 The number and severity of depressive symptoms is higher among repeat DWI offenders than first offenders.5 The rate of comorbid depression is underdiagnosed among repeat DWI offenders.6
In addition to being a risk factor for drinking and driving, alcohol dependence/abuse is clinically connected to depression, with high rates of comorbidity between depression and alcohol use disorders.7,8 Depression leads to worse outcomes from alcohol use disorders’ treatment.9,10 Individuals with depression often use alcohol to self-medicate, which increases frequency and volume of drinking, heavy drinking episodes, and binge drinking.11,12
While treating depression and alcohol use disorders jointly to prevent drinking and driving behavior has been proposed,13 mainstream DWI prevention programs continue to target alcohol use disorders separately. Depression, alcohol dependence/abuse, binge drinking, and drinking and driving are interrelated public health problems. A better understanding of the underlying relationships should provide a foundation for managing them more effectively. Studies to date have focused on relationships between those problems separately.4,14 No study has addressed how depression relates to drinking and driving through various underlying channels, e.g., exercise of self-control and using social interaction skills to obtain help in reducing harm from heavy alcohol use, in the same study.
There are at least three reasons to expect that depression and the drinking and driving are positively related and that they operate through three conceptually distinct channels. First, self-medicating with alcohol for a depressed mood increases the number of heavy drinking and binge drinking episodes,15 which naturally increases drinking-driving rates. Previous literature supports binge drinking as a drinking and driving precursor.16 Second, asking for help from non-intoxicated individuals as designated drivers is a common strategy for avoiding drinking and driving when intoxicated. But asking for help from others requires social interaction, and social withdrawal is common in depression.17 Individuals in a depressed mood may be reluctant to request help from non-intoxicated drivers after drinking, increasing the likelihood of drinking and driving. Prior research has documented a relationship between poor mental health and lower willingness to use protective behavioral strategies (e.g., driving slowly, use of designated drivers) to reduce the risk of negative drinking outcomes.18 Third, exercising control over alcohol consumption on a given occasion is an approach for avoiding drinking and driving.19 Drinking less in anticipation of driving requires self-control which may be compromised in persons with a depressed mood.20 Depression substantially impairs self-control and willpower. A depressed person may plan not to drink, yet become intoxicated due to lack of self-control.
This study addressed these issues: (1) What is the effect of depression on the number of self-reported drinking and driving episodes during the past year? (2) Through which behavioral channels does depression contribute to drinking and driving?
2. Conceptual Framework and Hypotheses
To isolate the effect of depression on drinking and driving, we accounted for the potential effect of alcohol dependence/abuse using this model:
We hypothesized three different channels through which depression affects the propensity to drink and drive with the signs of anticipated relationships in parentheses: binge drinking (+); use of a designated driver (−); and drinking less before driving (−).
While this illustration shows relationships for depression, our analysis also incorporated hypothesized effects of both depression and alcohol dependence/abuse on drinking and driving frequency.
3. Methods
3.1. Overview
We used both ordinary least squares (OLS) and path analysis. OLS could show the marginal effects of being depressed on the number of drinking and driving episodes and mediator outcomes, but could not identify underlying behavioral channels.
Path analysis allowed for testing our model, which hypothesized the presence of both direct and indirect effects. Direct effects reflected the influence of depression and alcohol dependence/abuse on drinking and driving episode frequency. The indirect effects represented the influence of depression and alcohol dependence/abuse on drinking and driving episode frequency operating through mediator outcomes, engaging in binge drinking, use of designated drivers, and drinking less when persons anticipate driving,
By combining the two methods, we examined the magnitude of depression’s effect and how depression is associated with other variables. Specifically, with OLS, we investigated the role of depression and additional covariates to isolate the effect of depression on the number of self-reported drinking and driving episodes in the year before the survey. With path analysis, we studied the three channels through which we hypothesized depression and alcohol dependence/abuse are linked to drinking and driving: binge drinking; drinking less before driving; and securing a designated driver. For comparison purposes, we present standardized and unstandardized OLS results.
3.2. Data
We commissioned Battelle Memorial Institute to conduct the Survey of Alcohol and Driving (SAD) in eight U.S. cities in four states during 2010–2012. The overall objective of the SAD was to collect data on drinking and driving behavior and on plausible determinants of such behavior. The SAD collected data on drinking and driving, alcohol consumption, including number of binge drinking episodes and prior arrests for drinking and driving, health, and psychological characteristics, cognitive status, affect, risk and time preferences, characteristics of the person’s motor vehicle insurance policy, questions to be used to compute the cost to the individual of being involved in a motor vehicle accident leading to permanent physical disability, subjective beliefs about adverse events occurring conditional on heavy and binge drinking, knowledge about criminal penalties for drinking and driving in the individual’s state, and income of the household in which the person resided. When possible, the SAD was based on questions that had been used in previous surveys, albeit not all in the same questionnaire. The first wave was administered by telephone. Waves 2 and 3, which required visual displays to improve respondent comprehension of the questions, were administered by computer. The survey instrument and methods were approved by Duke University’s Institutional Review Board.
A screener questionnaire, administered at the beginning of telephone survey (Wave 1) asked respondents if they had consumed any alcohol and driven a motor vehicle in the past 30 days. Those persons who indicated that they had not consumed any alcohol or driven during this period or were under age 18 or did not live in one of the study cities were not interviewed after the screener survey was conducted.
Participants in SAD were recruited in various ways, initially by random digit dialing and from lists of persons who had recently been arrested for driving while intoxicated (DWI). These approaches were supplemented by posting flyers in places where persons consume alcohol (e.g., bars) and by using purchased lists of email addresses of persons residing in the areas in which the SAD was conducted. The flyers/emails described the objectives and generally content of the SAD, a payment of up to $90 for completion of the three survey waves, and an email address at which Battelle could be contacted.
Given our screening criteria and participants recruitment methods, SAD participants were all drinkers and much more likely to have reported having had at least one drinking and driving episode in the past year than previous reports of the same behaviors from general surveys of U.S. adults. The recruitment process was designed to oversample persons who consumed large amounts of alcohol. Of persons screened, 15.3 percent did not consume any alcohol in the past month; 5.2 percent did not drive. Study participants were residents of: Raleigh and Hickory, North Carolina; Philadelphia and Wilkes-Barre, Pennsylvania; Seattle and Yakima, Washington; and Milwaukee and La Cross, Wisconsin. These large and small cities are widely dispersed geographically. While data from eight cities cannot fully represent the U.S., the four study states in which the cities are located varied in alcohol consumption, DWI laws, DWI arrest rates, and demographic composition.
This study, one of several studies published from the data, only used data from the first of three waves. Other studies focused on accuracy of risk perceptions, decisions individuals made about motor vehicle insurance purchases, effects of criminal sanctions on drinking and driving frequency, and other topics. Since the survey’s focus was on drinking and driving and its determinants, respondents had to have driven a motor vehicle and consumed alcohol during the last month, lived in a study city, and be 18+. Wave 1 included questions on: demographic characteristics/income; alcohol consumption and dependence/abuse; health behaviors including the number of drinking-driving episodes in the past year. Of the 2,238 persons initially contacted, 1,634 completed Wave 1.
3.3. Measurement of depression and alcohol dependence/abuse
Our depression measure was based on DSM-IV criteria. DSM-IV specifies that a diagnosis of depression be made based on affirmative responses to depressed mood or loss of interest plus at least four other factors for two or more consecutive weeks.21 The SAD used the SIG E CAPS, a depression screener. The SIG E CAPS is widely used in clinical practice.22,23 Questions used to construct the SIG E CAPS variable were related to: S sleep (insomnia or hypersomnia); I interests (diminished interest in or pleasure from activities); G guilt (excessive or inappropriate guilt, feelings of worthlessness); E energy (loss of energy or fatigue); C concentration (diminished concentration or indecisiveness); A appetite (decrease or increase in appetite, weight loss or gain); psychomotor (retardation or agitation); and S suicide (recurrent thoughts of death, suicidal ideation or suicide attempt). 24 The SAD asked survey participants to indicate if they experienced the above depression symptoms during any full two-week period during the past year. A binary variable for depression was set to 1 if the person answered affirmatively to 5 of the 9 questions.
We measured alcohol dependence/abuse with the CAGE, a widely-used alcoholism screener. The CAGE consists of four questions: (1) Have you ever felt you needed to (C)ut down on your drinking? (2) Have people (A)nnoyed you by criticizing your drinking? (3) Have you ever felt (G)uilty about drinking? (4) Have you ever felt you needed a drink first thing in the morning (Eye-opener) to steady your nerves or to get rid of a hangover? Two or more affirmative answers indicate that the person may be alcohol dependent or abuse alcohol. CAGE is a validated screening technique.25 Our binary variable for alcohol dependence/abuse was set to 1 if the respondent answered two+ CAGE questions affirmatively. The CAGE was selected for use in the SAD because it has been widely used in previous research and it is simple to administer. Based on a comprehensive review of existing literature, Dhalla and Kopec reported that the CAGE demonstrates high test-retest reliability, and adequate correlations with other screening instruments, and high sensitivity and specificity.26 They concluded that the questionnaire is a valid tool for detecting alcohol abuse and dependence in medical and surgical inpatients, ambulatory medical patients, and psychiatric inpatients.
3.4. Measures of drinking and driving and mediator outcomes
We included one measure of the number of drinking and driving episodes during the past year and three different mediator outcome variables representing channels through which depression, alcohol dependence/abuse, and other explanatory variables were hypothesized to affect drinking-driving frequency. Drinking and driving episodes were the number of times during the past year the person said that s/he drove while slightly intoxicated. Response options were 0, 1, 2, 3, 4, or 5+. For persons answering “5+,” we set the number of DWI episodes to 7. Sensitivity analysis revealed that results were insensitive to the assumed value of 7.
The first mediator outcome variable was arranging for a designated driver. The SAD asked, “When you are going some places where you plan to drink, do you arrange for someone else to drive after you have been drinking?” When answered “yes,” the person was asked, “How often do you arrange for someone else to drive after you have been drinking?” Response categories were “always,” “usually,” and “sometimes.” We coded use of a designated driver as: “always” = 3; “usually” =2; “sometimes” = 1; and “never” = 0. The second mediator outcome was drinking less before driving. The SAD asked, “When you are in a drinking situation in which you expect to drive, do you ever drink less than you otherwise would?” If “yes,” the person was asked, “How often do you drink less than you would if you were not driving?” The SAD response categories were the same as for the designated driver variable. The third mediator outcome variable was a binary variable for binge drinking in the past year. We defined binge drinking as consuming 5+ drinks/occasion for men under 65 and 4+ drinks on one occasion for women and men 65+. 27–31
3.5. Other explanatory variables
We included covariates for demographic characteristics--age, gender, educational attainment in years, black, other race, and Hispanic ethnicity, household income expressed in units of $10,000s, and marital status (=1 if currently married).
3.6. Empirical analysis
Using OLS, we estimated regressions with dependent variables for drinking and driving behaviors and channels related to drinking and driving. We first included depression as the only covariate. Second, we included all covariates described above except alcohol dependence/abuse. Third, we added the binary variable for alcohol dependence/abuse based on the four CAGE questions.
In the path analysis, we assumed depression and alcohol dependence/abuse are exogenous. Binge drinking, using a designated driver, and drinking less before driving were endogenous mediator outcome variables. The number of self-reported drinking and driving episodes was the final outcome. We performed path analysis twice, first with only those covariates just mentioned, and second adding covariates for demographic and socioeconomic factors. Results were similar; only the latter path analysis results are presented below.
4. Results
The mean number of self-reported drinking and driving episodes in the past year was 1.37 (Table 1). Nearly two-fifths of respondents (39%) gave two+ affirmative answers to the CAGE questions and hence were classified as being alcohol dependent and/or an alcohol abuser, a much higher percentage than for the general U.S. adult population from the U.S. National Comorbidity Survey.32 The mean values for arranging for a designated driver and for drinking less before driving were between “sometimes” and “usually” for designated driver and about at “usually” for drinking less in anticipation of driving. Thus, drinking less tended to be a somewhat more common approach for avoiding a drinking and driving episode.
Table 1.
Summary Statistics
| Panel A: Dependent Variables | ||||
|---|---|---|---|---|
| VARIABLE | Mean | Std. Dev. | Minimum | Maximum |
| # drunk driving episodes/year (0–7) | 1.37 | 2.02 | 0 | 6 |
| Arrange designated driver (0–3) | 1.59 | 1.24 | 0 | 3 |
| Drink less before driving (0–3) | 2.04 | 1.04 | 0 | 3 |
| Binge drinker (0,1) | 0.64 | 0.48 | 0 | 1 |
| Panel B: Explanatory Variables | ||||
| Depression (0,1) | 0.20 | 0.40 | 0 | 1 |
| Alcohol dependence/abuse (0,1) | 0.39 | 0.49 | 0 | 1 |
| Married (0,1) | 0.46 | 0.50 | 0 | 1 |
| Income (10,000 $s) | 8.02 | 6.54 | 0.75 | 35 |
| Age (years) | 42.67 | 12.55 | 18 | 82 |
| Female (0,1) | 0.52 | 0.50 | 0 | 1 |
| Educational attainment (years) | 15.46 | 2.03 | 11 | 18 |
| Black (0,1) | 0.11 | 0.32 | 0 | 1 |
| Hispanic (0,1) | 0.03 | 0.17 | 0 | 1 |
| Other race (0,1) | 0.04 | 0.20 | 0 | 1 |
Number of observations N=1641
The prevalence of depression was 20 percent, also higher than from other U.S. studies,8 which is plausible given depression’s association with alcohol consumption and abuse and resulting outcomes.7 On average, families had an annual income of about $80,000. Slightly under half of respondents were currently married. Mean age was 42 years. A slight majority was female. The vast majority of respondents were white (82%), and mean educational attainment was a nearly at a college level of completion.
With OLS, being depressed increased the number of drinking and driving episodes during the past year by 0.572 (Table 2, col. I), relative to the observational mean of 1.37. This increase in the number of drinking and driving episodes decreased to 0.411 episodes/year after adding socio-demographic characteristics and household income (col. II). Although the parameter estimate lost statistical significance after controlling for alcohol dependence/abuse (col. III), it nevertheless implies an increase of 0.168 drinking and driving episodes/year, an increase of over one-tenth relative to the observational mean. The standardized parameter estimate for depression was about one-sixth that for alcohol dependence/abuse when both depression and alcohol dependence/abuse were included as covariates (col. III, 0.033/0.201).
Table 2.
Regression Results on Number of Drinking and Driving Episodes and Behavioral Channels
| (I) | (II) | (III) | (I) | (II) | (III) | (I) | (II) | (III) | (I) | (II) | (III) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Drinking & driving episodes | Binge drinker | Arrange designated driver | Drink less before driving | |||||||||
| Depression | 0.572*** (0.128) 0.112 |
0.411** (0.127) 0.081 |
0.168 (0.128) 0.033 |
0.069* (0.030) 0.057 |
0.043 (0.029) 0.036 |
−0.020 (0.029) −0.016 |
−0.207** (0.079) −0.066 |
−0.199* (0.079) −0.064 |
−0.194* (0.081) −0.062 |
−0.260*** (0.065) −0.100 |
−0.196** (0.067) −0.075 |
−0.188** (0.069) −0.072 |
| Alcohol dependence/abuse | 0.835*** (0.104) 0.201 |
0.214*** (0.024) 0.218 |
−0.019 (0.066) −0.007 |
−0.030 (0.056) −0.014 |
||||||||
| Married | −0.717*** (0.113) −0.177 |
−0.679*** (0.111) −0.167 |
−0.077** (0.026) −0.080 |
−0.067** (0.025) −0.069 |
0.197** (0.071) 0.079 |
0.196** (0.071) 0.079 |
0.059 (0.060) −0.029 |
0.058 (0.060) 0.028 |
||||
| Income | 0.008 (0.009) 0.024 |
0.009 (0.009) 0.029 |
0.001 (0.002) 0.015 |
0.002 (0.002) 0.021 |
−0.006 (0.005) −0.030 |
−0.006 (0.005) −0.030 |
−0.004 (0.005) −0.026 |
−0.004 (0.005) −0.027 |
||||
| Age | −0.014*** (0.004) −0.089 |
−0.014*** (0.004) −0.085 |
−0.013*** (0.001) −0.330 |
−0.012*** (0.001) −0.325 |
−0.017*** (0.003) −0.169 |
−0.017*** (0.003) −0.170 |
−0.004 (0.002) −0.046 |
−0.004 (0.002) −0.046 |
||||
| Female | −0.759*** (0.101) −0.187 |
−0.655*** (0.100) −0.162 |
−0.098*** (0.023) −0.103 |
−0.072** (0.023) −0.075 |
0.451*** (0.063) 0.182 |
0.449*** (0.063) 0.181 |
0.183*** (0.054) 0.088 |
0.179** (0.054) 0.086 |
||||
| Education | −0.110*** (0.027) −0.110 |
−0.094*** (0.026) −0.094 |
−0.029*** (0.006) −0.123 |
−0.025*** (0.006) −0.106 |
0.004 (0.017) 0.007 |
0.004 (0.017) 0.006 |
0.064*** (0.014) 0.124 |
0.063*** (0.014) 0.123 |
||||
| Black | −0.280 (0.159) 0.044 |
−0.286 (0.156) −0.045 |
−0.115** (0.036) −0.076 |
−0.116** (0.035) −0.077 |
−0.266** (0.099) −0.068 |
−0.266** (0.099) −0.068 |
−0.132 (0.085) −0.040 |
−0.132 (0.085) −0.040 |
||||
| Hispanic | −0.301 (0.331) −0.022 |
−0.283 (0.324) −0.021 |
0.010 (0.076) 0.003 |
0.015 (0.074) 0.005 |
0.424* (0.206) 0.051 |
0.424** (0.206) 0.051 |
−0.102 (0.176) −0.015 |
−0.102 (0.176) −0.015 |
||||
| Other race | −0.790** (0.249) −0.078 |
−0.794** (0.244) −0.078 |
−0.086 (0.057) −0.036 |
−0.087 (0.055) −0.036 |
0.235 (0.155) 0.038 |
0.235 (0.155) 0.038 |
−0.058 (0.133) −0.011 |
−0.058 (0.133) −0.011 |
||||
| Observations | 1571 | 1521 | 1521 | 1571 | 1521 | 1521 | 1571 | 1521 | 1521 | 1571 | 1521 | 1521 |
| R-squared | 0.013 | 0.108 | 0.145 | 0.003 | 0.167 | 0.210 | 0.004 | 0.075 | 0.075 | 0.010 | 0.035 | 0.035 |
Standard errors in parentheses.
p<0.001,
p<0.01,
p<0.05
Standardized parameter estimates in italics.
(I) Depression status is the only explanatory variable.
(II) Regressions with all explanatory variables except CAGE.
(III) Model including CAGE.
Similar changes in depression’s coefficient following the addition of covariates occurred in the binge drinker analysis. Individuals with depression were significantly more likely to be binge drinkers (col. I), but the statistical difference disappeared after adding other covariates (cols. II and III). By contrast, persons with alcohol dependence/abuse had a 0.214 higher probability of reporting binge drinking (col. III).
Persons with depression were less likely to use a designated driver in all three specifications. The parameter estimates on depression did not differ in magnitude among the specifications. Persons in the alcohol dependent/abuse category did not differ from others in using a designated driver. The parameter estimate of −0.194 in the full specification is relative to an observational mean of 1.59.
The results for depression on drinking less before driving were similar to those for arranging a designated driver in signs and parameter estimate magnitudes and statistical significance. The parameter estimate in the full specification is −0.188, which is relative to the observational mean of 2.04. Also, as with use of designated driver, being alcohol dependent or an alcohol abuser was unrelated to drinking less before driving.
The signs of the parameter estimates on the demographic and socioeconomic covariates were plausible. Married persons and females tended to be more cautious, reporting fewer drinking and driving episodes, were more likely to use a designated driver, and were less likely to binge drink. But there was no difference between married persons and others in drinking less before driving, perhaps because of lower initial levels of alcohol consumption and/or a higher propensity to secure a designated driver. More highly educated persons were less likely to drink and drive and to binge drink, and more likely to drink less before driving, but there was no difference in using a designated driver.
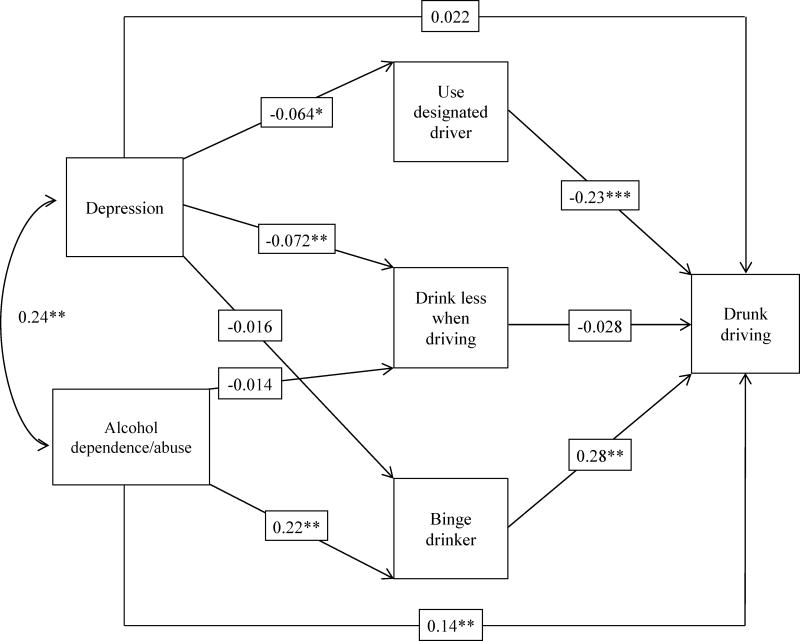
With path analysis, the goodness-of-fit index (GFI) was 0.99 (adjusted GFI, 0.86, Fig. 1). The path analysis controlled for all socio-demographic and income covariates (results for these covariates not shown in Fig. 1). There was a significant positive correlation between depression and alcohol dependence/abuse, 0.24. Depression had no direct causal effect on drinking and driving frequency. Depression was negatively associated with using a designated driver and with self-control over drinking when driving was anticipated, but effect sizes were small, −0.064 for using a designated driver and −0.072 for drinking less when expecting to drive. Depression was not related to binge drinking.
Figure 1. Path Model Estimates.
*** p<0.001, **p<0.01, * p<0.05
Alcohol dependence/abuse had a statistically significant direct causal effect on drinking and driving frequency with a path coefficient of 0.14. Alcohol dependence/abuse led to binge drinking with a significant path coefficient of 0.22, but there was no statistical relationship with drinking less before the respondent expected to drive.
Among the three mediating variables, binge drinking and use of a designated driver led to higher drinking and driving frequency. The path coefficients were −0.23 for arranging a designated driver and 0.28 for binge drinking. These direct effects imply that using a designated driver and not being a binge drinker indeed do reduce drinking and driving frequency. The indirect effect of depression on drinking and driving was 0.015 (−0.064×−0.23), i.e., less than the statistically insignificant indirect effect on drinking and driving of 0.022.
5. Discussion
Our results explain channels through which depression and alcohol dependence/abuse affect drinking and driving frequency. Being alcohol dependent and/or an alcohol abuser was linked to frequency of drinking and driving both because of their higher levels of alcohol consumption in general (direct effect) and their higher propensity to engage in heavy drinking on particular occasions (binge drinking, indirect effect).
Being depressed was much less strongly associated with the number of self-reported drinking-driving episodes/year than was alcohol dependence/abuse. In contrast to alcohol dependence/abuse, our results indicated that being depressed has a minor direct influence on use of a designated driver and self-control of drinking. Since being depressed was positively related to alcohol dependence and abuse, depression was also linked to drinking and driving frequency through alcohol dependence/abuse. The hypothesis that depression is positively linked to binge drinking was not confirmed by our empirical analysis. Rather to the extent that a relationship exists, it operates indirectly through alcohol dependence/abuse.
Treating depression and alcohol dependence/abuse together has a potential benefit. Clinical studies have documented that treating depression can enhance efficacy of alcohol treatment, which indicates that treating depression yields an indirect benefit of controlling drinking and driving.33 Our results suggest that treatment should focus on helping individuals with depression to obtain assistance from others. Individuals with depression have difficulty using designated drivers for two reasons: (1) non-use of a designated driver, perhaps caused by a combination of low self-esteem, self-efficacy and motivation; and (2) a social withdrawal effect of depression, caused by self-hate and shame or a narrower social network.34 Although effect sizes in path analysis were small, persons with depression used a designated driver less often. Behavioral treatments for depression should emphasize the importance of using a designated driver and combating the shameful feeling and low motivation when asking for help. Using designated drivers alone can reduce drinking and driving with an effect size similar to the effect size for alcohol dependence/abuse. Another benefit of addressing depression as part of DWI prevention is that individuals with depression tend to have higher motivation for changing their problematic behaviors than do individuals without depression,13,35,36 but they have lower confidence and self-efficacy in alcohol-related treatments they receive.37,38
This study adds to the literature in employing path analysis to assess mechanisms through which depression relates to drinking and driving frequency. The analysis controlled for alcohol problems to help isolate the unique role of being depressed in drinking and driving.
We acknowledge several study limitations. First, our survey oversampled heavy alcohol consumers and persons with alcohol-related problems. Nevertheless, results on key demographic variables are plausible and consistent with previous studies.4,16 Second, drunk-driving frequency was self-reported. The number could be underreported since drunk driving is potentially illegal (depending on whether the person’s blood alcohol content level exceeds the level specified in the state’s statute). Third, we identified two channels through which depression may affect drinking and driving. While these are important channels, there may be others, including that drinking and driving stem from suicidal tendencies.39 Fourth, our survey only interviewed drinkers. Persons arrested and convicted of DWI offenses were a small fraction of respondents. Fifth, our survey used screens for depression and alcohol dependence/abuse and did not use more intensive methods to assess presence of these two conditions.
Particularly since there are policy interventions specifically designed to deal with persons convicted of DWI offenses, and depression is more common among such persons, it would be useful to replicate our methodology with a sample of persons convicted of DWI. Another extension would analyze data on persons with clinical depression diagnoses and for whom severity of depression has been measured.
In sum, our findings imply that treatment should help individuals with depression to obtain help from others, such as obtaining a designated driver. Since self-control of drinking in anticipation of driving did not significantly reduce drinking and driving episodes, we found no empirical support for emphasizing improved self-control when the program objective is to reduce drinking and driving frequency. While binge drinking is associated with drinking and driving, the more appropriate way to influence binge drinking is through treating alcohol dependence/abuse rather than depression per se.
Acknowledgments
This research was supported by a grant from the National Institute on Alcohol Abuse and Alcoholism, Grant 5R01-AA-017913-03. The sponsor had no involvement in study design, collection, analysis and interpretation of the data, in the writing of the manuscript or in the decision to submit the manuscript for publication. We acknowledge the capable research assistance of Sabrina McCutchan and Yanzhi Xu.
Contributor Information
Ye Zhang, Email: yz137@duke.edu, Duke University School of Nursing, 307 Trent Drive, DUMC 3322, Durham, NC 27710, Office: (919)-668-9976, Cell: (919)-995-2510
Frank A. Sloan, Email: fsloan@duke.edu, Department of Economics, 213 Social Sciences Building, Box 90097, Duke University, Durham, NC 27708, Phone: (919) 613-9358, Fax: (919) 681-7984
References
- 1.Room R, Babor T, Rehm J. Alcohol and public health. The Lancet. 2005;365(9458):519–530. doi: 10.1016/S0140-6736(05)17870-2. [DOI] [PubMed] [Google Scholar]
- 2.DiStefano G, Hohman M, Ruyle CA. Addressing co-occurring disorders and other clinical issues in a DUI population. J Dual Diagn. 2010;6(1):46–57. [Google Scholar]
- 3.Hubicka B, Kallmen H, Hiltunen A, Bergman H. Personality traits and mental health of severe drunk drivers in Sweden. Social Psychiatry and Psychiatric Epidemiology. 2010;45(7):723–731. doi: 10.1007/s00127-009-0111-8. [DOI] [PubMed] [Google Scholar]
- 4.Stoduto G, Dill P, Mann RE, Wells-Parker E, Toneatto T, Shuggi R. Examining the link between drinking-driving and depressed mood. Journal of Studies on Alcohol and Drugs. 2008;69(5):777–780. doi: 10.15288/jsad.2008.69.777. [DOI] [PubMed] [Google Scholar]
- 5.McMillian DL, Adams MS, Wells-Parker E, Pang MG, Anderson BJ. Personality-traits and behaviors of alcohol-impaired drivers - a comparison of 1st and multiple offenders. Addictive Behaviors. 1992;17(5):407–414. doi: 10.1016/0306-4603(92)90001-c. [DOI] [PubMed] [Google Scholar]
- 6.McMillian GP, Timken DS, Lapidus J, C’de Baca J, McNeal J. Underdiagnosis of comorbid mental illness in repeat DUI offenders mandated to treatment. Journal of Substance Abuse Treatment. 2008;34(3):320–325. doi: 10.1016/j.jsat.2007.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grant BF, Harford TC. Comorbidity between DSM-IV alcohol use disorders and major depression: Results of a national survey. Drug and Alcohol Dependence. 1995;39(3):197–206. doi: 10.1016/0376-8716(95)01160-4. [DOI] [PubMed] [Google Scholar]
- 8.Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiology Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61(8):807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 9.Boden JM, Fergusson DM. Alcohol and depression. Addiction. 2011;106(5):906–914. doi: 10.1111/j.1360-0443.2010.03351.x. [DOI] [PubMed] [Google Scholar]
- 10.Hasin D, Liu X, Nunes E, McCloud S, Samet S, Endicott J. Effects of major depression on remission and relapse of substance dependence. Archives of General Psychiatry. 2002;59(4):375–380. doi: 10.1001/archpsyc.59.4.375. [DOI] [PubMed] [Google Scholar]
- 11.Bolton JM, Robinson J, Sareen J. Self-medication of mood disorders with alcohol and drugs in the National Epidemiologic Survey on Alcohol and Related Conditions. J Affect Disord. 2009;115(3):367–375. doi: 10.1016/j.jad.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 12.Mushquash AR, Stewart SH, Sherry SB, Sherry DL, Mushquash CJ, MacKinnon AL. Depressive symptoms are a vulnerability factor for heavy episodic drinking: A short-term, four-wave longitudinal study of undergraduate women. Addictive Behaviors. 2013;38(5):2180–2186. doi: 10.1016/j.addbeh.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 13.Wells-Parker E, Williams M. Enhancing the effectiveness of traditional interventions with drinking drivers by adding brief individual intervention components. Journal of Studies on Alcohol. 2002;63(6):655–664. doi: 10.15288/jsa.2002.63.655. [DOI] [PubMed] [Google Scholar]
- 14.Vander Weg MW, DeBon M, Sherrill-Mittleman D, Klesges RC, Relyea GE. Binge drinking, drinking and driving, and riding with a driver who had been drinking heavily among Air National Guard and Air Force Reserve Personnel. Military Medicine. 2006;171(2):177–183. doi: 10.7205/milmed.171.2.177. [DOI] [PubMed] [Google Scholar]
- 15.Cerda M, Tracy M, Galea S. A prospective population based study of changes in alcohol use and binge drinking after a mass traumatic event. Drug Alcohol Depend. 2011;115(1–2):1–8. doi: 10.1016/j.drugalcdep.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sloan FA, Reilly BA, Schenzler C. Effects of tort liability and insurance on heavy drinking and drinking and driving. Journal of Law & Economics. 1995;38:49–77. [Google Scholar]
- 17.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4(6):561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 18.LaBrie JW, Kenner SR, Lac A. The use of protective behavioral strategies is related to reduced risk in heavy drinking college students with poorer mental and physical health. Journal of Drug Education. 2010;40(4):361–378. doi: 10.2190/DE.40.4.c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.D’Lima GM, Pearson MR, Kelley ML. Protective behavioral strategies as a mediator and moderator of the relationship between self-regulation and alcohol-related consequences in frst-year college students. Psychol Addict Behav. 2012;26(2):330–337. doi: 10.1037/a0026942. [DOI] [PubMed] [Google Scholar]
- 20.Baumeister R, Zell AL, Tice DM, Gross J. How emotions facilitate and impair self-regulation. In: Gross JJ, editor. Handbook of emotion regulation. New York, New York: The Guilford Press; 2007. pp. 408–426. [Google Scholar]
- 21.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, D.C: American Psychiatric Press; 1994. [Google Scholar]
- 22.Wise MG, Rundell JR. Concise guide to consultation psychiatry. Washington, D.C: American Psychiatry Press; 1994. [Google Scholar]
- 23.Lieberman JA. Identifying depression in primary care. Postgraduate Medicine. 2003;114(5 Suppl Treating):5–9. doi: 10.3810/pgm.11.2003.suppl29.157. [DOI] [PubMed] [Google Scholar]
- 24.Guck TP, Elsasser GN, Kavan MG, Eugene J. Depression and congestive heart failure. Congestive Heart Failure. 2003;9(3):163–169. doi: 10.1111/j.1527-5299.2003.01356.x. [DOI] [PubMed] [Google Scholar]
- 25.Bernadt MW, Mumford J, Taylor C, Smith B, Murray RM. Comparison of questionnaire and laboratory tests in the detection of excessive drinking and alcoholism. Lancet. 1982;1(8267):325–328. doi: 10.1016/s0140-6736(82)91579-3. [DOI] [PubMed] [Google Scholar]
- 26.Dhalla S, Kopec JA. The CAGE Questionnaire for Alcohol Misuse: A Review of Reliability and Validity Studies. Clinical & Investigative Medicine. 2007;30(1):33–41. doi: 10.25011/cim.v30i1.447. [DOI] [PubMed] [Google Scholar]
- 27.Brewer RD, Swahn MH. Binge drinking and violence. JAMA. 2005;294(5):616–618. doi: 10.1001/jama.294.5.616. [DOI] [PubMed] [Google Scholar]
- 28.Naimi TS, Brewer RD, Mokdad A, Denny C, Serdula MK, Marks JS. Binge drinking among US adults. JAMA: The Journal of the American Medical Association. 2003;289(1):70–75. doi: 10.1001/jama.289.1.70. [DOI] [PubMed] [Google Scholar]
- 29.Naimi TS, Nelson DE, Brewer RD. The intensity of binge alcohol consumption among U.S. adults. American Journal of Preventive Medicine. 2010;38(2):201–207. doi: 10.1016/j.amepre.2009.09.039. [DOI] [PubMed] [Google Scholar]
- 30.Wechsler H, Austin SB. Binge drinking: The five/four measure. Journal on Studies of Alcohol. 1998;59:122–124. doi: 10.15288/jsa.1998.59.122. [DOI] [PubMed] [Google Scholar]
- 31.Wechsler H, Nelson TF. Binge drinking and the American college students: What’s five drinks? Psychology of Addictive Behaviors. 2001;15(4):287–291. doi: 10.1037//0893-164x.15.4.287. [DOI] [PubMed] [Google Scholar]
- 32.Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Archives of General Psychiatry. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 33.Greenfield SF, Weiss RD, Muenz LR, et al. The effect of depression on return to drinking: a prospective study. Archives of General Psychiatry. 1998;55(3):259–265. doi: 10.1001/archpsyc.55.3.259. [DOI] [PubMed] [Google Scholar]
- 34.Beck AT, Alford BA. Depression: Causes and treatments. 2. Philadelphia, PA: University of Pennsylvania Press; 2009. [Google Scholar]
- 35.Nochajski TH, Staiewicz PR, Patterson DA. Depression, readiness for change, and treatment among court-mandated DUI offenders. Journal of Dual Diagnosis. 2013;9(2):139–148. doi: 10.1080/15504263.2013.779092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wells-Parker E, Dill P, Williams M, Stoduto G. Are depressed drinking/driving offenders more receptive to brief intervention? Addictive Behaviors. 2006;31(2):339–350. doi: 10.1016/j.addbeh.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 37.Dill PL, Wells-Parker E, Cross GW, et al. The relationship between depressed mood, self-efficacy and affective states during the drinking driving sequence. Addict Behav. 2007;32(8):1714–1718. doi: 10.1016/j.addbeh.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 38.Holt LJ, O’Malley SS, Rounsaville BJ, Ball SA. Depressive Symptoms, Drinking Consequences, and Motivation to Change in First Time DWI Offenders. American Journal of Alcohol Abuse. 2009;35(3):117–122. doi: 10.1080/00952990802585398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Carpenter C. Heavy alcohol use and youth suicide: Evidence from tougher drunk driving laws. J Policy Anal Manage. 2004;23(4):831–842. [Google Scholar]