Abstract
Objective
Evaluate determinants of mental health service use among depressed adolescents.
Method
We assessed mental health services use over the 12 months following screening among 113 adolescents (34 males, 79 females) from an integrated healthcare system who screened positive for depression (Patient Health Questionnaire-9 score > 11). Youth characteristics (demographics, depression severity, and co-morbidity) and parent characteristics (parent history of depression, parent-report of youth externalizing and internalizing problems) were compared among youth who had received mental health services and those who had not. Multivariate regression was used to evaluate the strongest factors associated with mental health service use.
Results
Overall, 52% of adolescents who screened positive for depression received mental health service in the year following screening. Higher parent-reported youth internalizing problems (OR 5.37 CI 1.77–16.35), parental history of depression/anxiety (OR 4.12 CI 1.36–12.48) were significant factors associated with mental health service use. Suicidality and functional impairment were not associated with increased mental health services use.
Conclusion
Parental factors including recognition of the adolescent’s internalizing symptoms and parental experience with depression/anxiety are strongly associated with mental health service use for depressed adolescents. This highlights the importance of educating parents about depression and developing systems to actively screen and engage youth in treatment for depression.
Keywords: depression, adolescent
Introduction
The lifetime prevalence of adolescent depressive disorders (combining across major depressive disorder and dysthymic disorder) is estimated to be up to 14% for 13–17 year olds and over half of these depressed youth (approximately 9%) are severely impaired.1 Depression is often chronic but also can follow an episodic course with frequent recurrences and is often associated with other comorbid psychiatric conditions such as anxiety, substance use, and externalizing disorders (e.g. attention deficit disorder, oppositional defiant disorder).2 As a result, there is often impairment in the development of social, emotional, cognitive, interpersonal skills, and in functioning.3–5 Depression is also a risk factor for suicide among adolescents.4
Despite accumulating evidence for the effectiveness of treatments for depression, few youth utilize mental health services or receive these treatments. 4–11 Studies examining factors associated with mental health service use, either for depression specifically or more broadly regardless of mental health diagnosis, have suggested that youth characteristics are related to service use. For example, adolescents from racial and ethnic minorities, particularly African Americans and Latinos, have been shown to be less likely to access mental health care.4–7, 12, 13 The effects of gender have been less straightforward, with some studies showing no gender differences in utilization, 10, 14 and others showing differential rates by gender.4, 7, 15, 16 Some studies have shown higher rates of utilization in boys17 and others have shown higher rates of utilization in girls.4, 17 Youth with externalizing symptoms are more likely to receive mental health diagnoses,17 and one hypothesized reason for gender differences in samples including younger children is that males are more likely to have a comorbid externalizing disorder and thus are more likely to be detected.7, 13, 17 Additional factors that have been associated with use of services include severity of depression and chronic health problems. Specifically, adolescents who receive mental health services for depression have been shown to be more severely impaired including having higher depressive symptom scores and a more recent suicide attempt than those who did not receive services.4, 9, 16 Youth with chronic medical conditions such as asthma and diabetes are also more likely to access mental health services.4, 8
In addition to youth characteristics, parental characteristics have been shown to be associated with service use.12, 13, 18, 19 One study found that parental perception of family burden due to the youth’s depression was strongly associated with parental identification of depression and service use.19 Mothers’ own experiences with depression have been shown to both predict new-onset disorders in their offspring20 and increase mental health use for their children, which have been hypothesized to be to the result of increased recognition of symptoms in their teen.13, 17 Socioeconomic status of the family has been shown to be one of the most robust factors associated with mental health service use among adolescents.4, 6, 7, 12, 13, 21, 22 Higher income has been associated with more mental health related visits along with an increased likelihood of seeing a mental health specialist versus a general practitioner.12
Most studies examining factors associated with mental health service use have used small samples with wide age ranges, encompassing multiple mental health conditions rather than depression alone. As a result, there is limited data on factors associated with mental health service use specifically in a population of depressed adolescents. Recently the US Preventative Services Task Force has added the recommendation to screen adolescents for depression.23 As more youth with depression are detected, it will be important to understand the factors that are associated with utilization of care in order to increase receipt of depression treatment among all affected youth. This is the first large population study to examine specific youth and parental factors associated with mental health service use in depressed adolescents in an insured population.
Methods
This study utilized data from the AdoleSCent Health Study, a prospective study evaluating the performance of depression-screening tools among adolescents in primary care. Adolescents were enrolled from Group Health (GHC), a large nonprofit integrated delivery system in the Pacific Northwest. The population of youth, in GHC, is demographically similar to the population in Seattle, Washington/King County where most are covered under parental employer-based insurance and 6–7% are covered via Medicaid or other state-based insurance plans. GHC offers in-system mental health services and contracts with private mental health practitioners to assure coverage for all enrollees. GHC members may self-refer to within system specialty mental health care through a behavioral health intake line. GHC also contracts with out of system behavioral health services in regions where in-system behavioral health resources are not available.
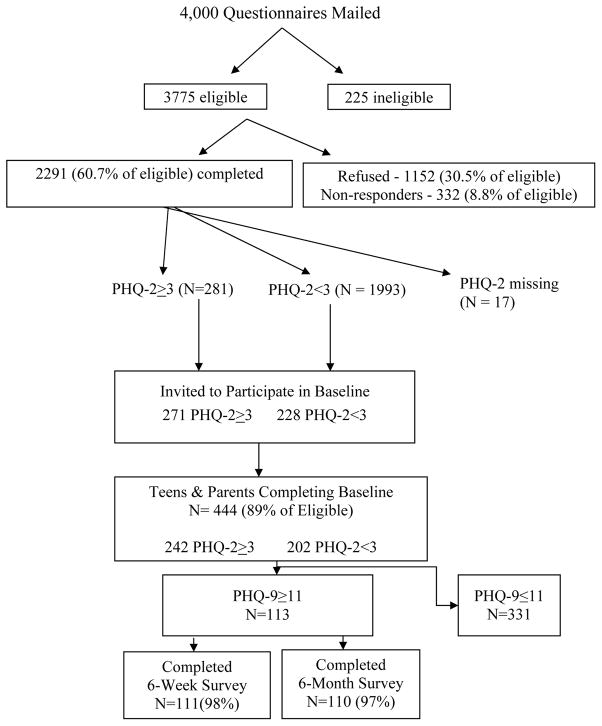
Participants were enrolled between September 2007 and June 2008. The study staff randomly selected 4000 enrollees (Figure 1), aged 13–17 years old who saw a provider in a GHC facility at least once in the previous 12 months. The parents/guardians were sent invitation letters, consent form and a brief survey for the child. The brief survey had 10 items with 2 of the items being the Patient Health Questionnaire (PHQ-2). A subset of youth was asked to participate in a telephone survey with in-depth information obtained regarding depressive symptoms and health behaviors. Youth, who screened positive for depression using the PHQ-2 (score of 3 or more) and an age and gender matched sample of youth, pulled from the same GHC population, who did not screen positive were asked to participate in a longitudinal interview study of depressive symptom persistence (n = 444). Participants were then given the Patient Health Questionarie (PHQ-9). Two stage screening in general population samples are recommended to avoid the cost of screening so many people without symptoms and markedly saves costs in epidemiologic work. This study was reviewed by the Group Health Internal Review Board and consent and assent were obtained from parents and youth, respectively. Surveys assessing depressive symptoms, functional impairment and other health behaviors were conducted via telephone at baseline as well as 6-week and 6-month follow-ups. This was an observational study and no treatment interventions were provided. The only exception was for youth who screened positive with a score of 2 or higher on the 9th item on the PHQ-9. These youth were contacted by a clinician, evaluated, and if determined to be at risk of self harm, were assisted in connecting with care.24 Data on health care utilization was gathered using administrative claims data for all health care visits and prescriptions as well as by youth self-report of interval mental health services use at the follow-up assessments.
Figure 1.
Study Enrollment Flow Diagram
Measures
Youth Characteristics
Demographics and Chronic Health Conditions
Age and race/ethnicity was assessed via self report. Families’ addresses and zip codes were used to estimate the median household income within census block group. To adjust for the impact of other health conditions on utilization, automated pharmacy records were used to generate the Pediatric Chronic Disease Score (PCDS), which has been shown to predict subsequent 1-year utilization and health care cost.25
Depression Status
Depression at baseline was assessed using the Patient Health Questionnaire 9-item depression screener (PHQ-9). In prior work using these data, we found that a cutoff of ≥11 on the PHQ-9 had a sensitivity of 89.5% and specificity of 77.5% for detecting youth who meet criteria for a Major Depressive Disorder based on a structured diagnostic interview.26 Total symptom score on the PHQ-9 has also been shown to be predictive of depressive symptom persistence.9
Psychological Impairment
Youth also completed the Columbia Impairment Scale (CIS), a 13-item assessment of overall psychosocial impairment, including questions regarding functioning in school, home and relationships each scored on a 0–4 Likert scale.27 The CIS was included in the analysis as a continuous variable to assess impact of psychological/functional impairment on use of services.27
Anxiety
Anxiety comorbidity was assessed using the 5-item Screen for Child Anxiety Related Emotional Disorders (SCARED).28 The SCARED was included as a continuous measure in all analysis. With a range of 0–10, a cut point of >3 on the SCARED has been show to have a 74% sensitivity and 73% specificity for identifying youth with probable anxiety disorders.28
Problem Substance Use
To measure problem substance use among the participants, the CRAFFT substance use screener was used. This questionnaire included 6 yes/no items resulting in a range of 0–6 and was included as a continuous measure in all analyses.29
Parent Characteristics
Parental History of Depression/anxiety
The responding parent’s history of depression and/or anxiety was assessed with a two items asking 1) if they have ever been diagnosed with depression or anxiety, and 2) whether they had received treatment for depression or anxiety. In preliminary analyses with these data, we found that 92% of parents who indicated that they had a history of diagnoses also indicated that they had received treatment. Thus only the diagnosis question was included in analyses as a categorical variable.
Parental Report of Youth Symptoms
Parents were asked to complete the parent-report version of the externalizing and internalizing subscales of the Pediatric Symptom Checklist-17 (PSC-17). The externalizing component of the screening tool assesses acting out behaviors as associated with conduct disorder and other externalizing diagnoses and has been shown to have 62% sensitivity and 89% specificity in detecting youth who meet criteria for an externalizing disorder based on structured interviews.30 The internalizing component of the PSC-17 measures for depressive and anxiety symptoms and has been shown to have 73% sensitivity and 74% specificity for detecting major depression among youth. 30 Both the internalizing and externalizing scales were included as continuous measures to assess the impact of higher scale scores on the likelihood of service use.
Treatment Utilization
We used an inclusive measure of mental health treatment utilization that combined administrative data on outpatient mental health visits and SSRI prescription fills with self-reported mental health care utilization for depression. Group Health pharmacy and administrative automated databases were used to identify each of the following in the 12 months after screening: (1) antidepressants or antianxiety prescriptions; and (2) any specialty mental health visits regardless of diagnosis.
To assess potential receipt of mental health services outside of the integrated health system, we also conducted follow-up surveys with youth to determine if they had received any treatment for depression in the 6 months following screening. Data from the youth surveys and administrative data were combined such that youth were considered to have received services if they had an indication of mental health services use on either the administrative data or in self-reported surveys.8 The self-report measure is based on adolescent report only and does not include caregivers.
Statistical Analysis
We examined overall factors associated with mental health service use using univariate analysis in the entire sample (n=444). We then used Pearson’s chi-squared test to compare those youth who screened positive for depression on the PHQ-9 (n = 113) to those who did not (n=331) in their receipt of mental health services. To control for the potential confounding effects of other chronic health issues, all analyses were adjusted for PCDS. Logistic regression models were analyzed using the sample of depressed youth in order to identify the strongest youth and parental characteristics predictive of mental health service use. As we wanted to understand the unique and incremental value of parental characteristics in the context of youth characteristics, we constructed two separate logistic regression models. The first model focused on youth characteristics only, and a second model examined the additional contribution of parent characteristics to youth characteristics. Median area income was not included in the regression model as it was a community level variable and was not reflective individual youth or parent income.
Results
A total of 444 youth were assessed, 65% were white and 27% multi-racial or “other” with a mean age of 15 years old. Seventy-one percent were female. Of the total participants, 113 participants met study criteria for probable depression (>11 on the PHQ-9). In administrative data, mental health services use was greater among youth who screened positive for depression than those who screened negative: 18% of youth who were depressed had utilized specialty mental health services or had a prescription in the year following screening compared to 12% of non-depressed youth (Table 1). In self-report data, 44% of depressed adolescents and 9% of nondepressed adolescents reported receiving treatment for depression in the 6-months post screening. Combining both variables, we found that 53% of depressed youth received some type of mental health services or antidepressant within the last year, compared to 21% of nondepressed youth.
Table 1.
Receipt of Mental Health Treatment for youth who screened positive for depression*(N = 113)
| Variable | Depression (N = 113) N (%) |
|---|---|
| MENTAL HEALTH TREATMENT VARIABLES | |
| ADMINISTRATIVE DATA IN 12 MONTHS FOLLOWING BASELINE† | |
| Any Antidepressant or antianxiety Medication fills | 13 (12) |
| Any outpatient health visit | 10 (9) |
| Either any antidepressant/antianxiety medication fill OR any outpatient health visit | 20 (18) |
| YOUTH SELF-REPORT RATING† | |
| Self report of mental health treatment by 6 months from baseline | 48 (44) |
| EITHER ADMINISTRATIVE DATA OR YOUTH REPORT† | |
| Received any services based on self-report or administrative data | 58 (53) |
Depression based on PHQ-9 ≥ 11;
Ratings based on administrative medical record data, youth report or both
When examining youth characteristics, there were no significant demographic differences between depressed adolescents who received services and those who did not. Within a bivariate analysis, youth with higher PCDS scores, indicating more chronic health conditions, were more likely to access mental health services than those with lower scores (p=0.005). The severity of depression (total PHQ-9 score), suicidal ideation, anxiety comorbidity, functional/psychological impairment, and problem substance use behavior did not predict mental health service use among depressed youth.
Examining parental characteristics, we found that youth who had received mental health services had higher parent-reported internalizing symptoms on the PSC-17 internalizing scale at the baseline interview (p<0.001). In bivariate analyses, there was a nonsignificant trend suggesting that parental history of depression or anxiety was also associated with increased youth mental health service use (p=0.074).
In the logistic regression model, with youth characteristics alone, none of the youth characteristics were significantly associated with service use. (Table 3) In the second regression model adding parental characteristics, we found that parental history of depression/ anxiety and parent- report of youths internalizing symptoms were both significant factors associated with mental health service use. (Table 3) One surprising finding was that depressed youth with more psychosocial impairment, as indicated by a higher CIS score, were significantly less likely to receive mental health services (OR 0.91 0.84–0.99).
Table 3.
Multivariate Logistic Regression Analysis of Factors associated with mental health service use of Mental Health Service use for depression among Youth with a Baseline PHQ-9 >11 (Depression) (N=110)
| Variable | Model 1 OR (95% CI) |
Model 2 OR (95% CI) |
|---|---|---|
| YOUTH CHARACTERISTICS | ||
| Age | 1.47 0.96–2.10 | 1.42 0.93–2.17 |
| Male (vs female) | 0.42 0.15–1.17 | 0.45 0.15–1.38 |
| White (vs nonwhite) | 1.04 0.40–2.67 | 1.10 0.37–3.28 |
| Depression Severity | 1.12 0.97–1.29 | 1.11 0.95–1.29 |
| Anxiety Symptoms | 1.05 0.84–1.32 | 1.11 0.85–1.44 |
| Functional Impairment Score | 0.95 0.89–1.02 | 0.91 0.84–0.99 |
| Problem Alcohol or Drug Use | 0.87 0.62–1.23 | 0.78 0.52–1.18 |
| PARENT CHARACTERISTICS | ||
| Parent History of Depression/Anxiety | 4.12 1.36–12.48 | |
| Parent Report of Youth Externalizing Symptoms | 1.10 0.31–3.95 | |
| Parent Report of Youth Internalizing Symptoms | 5.37 1.77–16.35 | |
Model 1 includes all youth characteristics; Model 2 adds parental characteristics.
All models controlled for Pediatric Chronic Disease Score.
Discussion
This is the first large population-based study to examine both youth and parent factors associated with mental health service use among depressed adolescents. This study found that mental health service utilization was low overall and that the main factors associated with mental health service use were parental identification of youth internalizing symptoms and parental history of depression. Our findings are consistent with prior studies that have shown that parental perceived burden of the mental health disorder in their child is a strong predictor of receipt of treatment,4, 14, 19, 31–33 as well as studies that have found that outpatient mental health service utilization is more likely when the youth’s symptoms are reported to be impacting the family.4, 12, 19, 32 This suggests that youth may not be the ones making treatment decisions and that parent’s likely play a crucial role. Another important finding of this work is that parental history of depression and /or anxiety is a significant predictor of service use independent of the parent’s perception of youth burden. In our sample, 92% of parents who self-identified as having a previous depression/anxiety diagnosis also received mental health treatment. While other studies have found that parental depression predicts service use,15 this is the first study to examine it alongside parental perception of youth symptoms. Teens’ families contribute to youths’ decisions to seek care for depression, and known family history of depression through family interactions has significant influence on depression treatment.34 It is possible that parents who have experienced the repercussions of depression first-hand may also be more able to recognize similar symptoms in their children, and more likely to recommend and/or help their adolescent seek treatment. Parents who have been treated for depression may also have enhanced skills in seeking mental health care and more comfort with available treatments.
Given the evidence that higher depressive symptom burden is associated with increased risk of persistence, 9 it is concerning that higher symptom severity was not associated with increased likelihood of services use. Prior work, including one study using these data, has found that suicidal youth were not more likely to receive services compared to nonsuicidal youth with comparable depression. 16, 24 These findings emphasize the need to combine screening with stepped care guidelines such as the Guidelines for Adolescent Depression in Primary Care in order to increase the engagement of youth with more severe symptoms in treatment.35
Our study was the first to find that the more psychosocially impaired the depressed adolescent was, the less likely they were to utilize mental health services. This finding is contradictory to findings for mental health care use in general, which is usually higher in the presence of higher functional/psychological impairment.10, 17 Examples of psychosocial impairment questions include having trouble in school or issues with getting along with friends or family. We hypothesize that in cases of very high impairment; there may be competing demands on the parents’ and youths’ time and resources that impede treatment access. Also, increased conflict between the youth and the parent over the psychosocial issues may result in less closeness, thereby decreasing parental opportunities for detection of depressive symptoms and/or youth disclosure of depression. Thus, the relationship between function/psychological impairment and care seeking may differ in conditions with more subtle symptoms (i.e. depression) versus conditions that are more overt. However, as this is the first study to find this association, we cautiously consider this finding, which may be unique to this population of depressed adolescents. Future study is warranted to confirm and explore this association further.
There are a few limitations to our study. First, the study population was drawn from a single integrated health care system in the Pacific Northwest where most youth can access mental health services without referral and with less out-of-pocket expense due to low co-pays and may not be generalizable to a broader population. However, this may also be a strength since it allows us to explore youth and parent factors in the absence of the systematic barrier of access and availability of resources. Second, while we used validated measures to detect depression among youth, health care utilization data were based on administrative data and youth report. Thus, we were not able to examine care seeking separately from receipt of treatment. In addition, although man of the youth who were screened as severely depressed did not access mental health care, there is a possibility that the PHQ-2 did not detect all of the depressed adolescents. Lastly, although this study has a relatively large sample size relative to other studies of this topic, this study may not have been adequately powered to detect significant differences, depending on the characteristics of the measures and the variable being considered.
Conclusion
The results of this study highlight the important role that the parents play in the engagement of youth in depression treatment. This has several important implications. Providers working with depressed youth need to acknowledge the role that the parents play in care seeking. It may be particularly important to engage parents regarding their knowledge of depression and to address any biases regarding diagnosis in order to increase youth access to mental health care. Second, further work is needed to understand why parents with a history of depression are more likely to have adolescents who receive care for depression. This may provide useful information to inform future interventions that engage parents in order to improve recognition and treatment engagement for youth with depression. Finally, it is concerning that the results of this study and others suggest that depression treatment receipt is not associated with depressive symptom severity. Severely depressed youth are not receiving mental health care, therefore new systems are needed to help identify these youth. Such services could be school-based health centers or mental health services that are integrated into primary health care settings such as stepped-care model used in adult mental health care.37 There is a current movement toward a stepped-care model, whereby treatment begins at the lowest appropriate service tier at the onset of depression and is subsequently stepped up to more intensive services. In this model, we would expect that youth who are persistently depressed would get increased service utilization and treatment with antidepressants and/or additional treatments if their depression is not improving. Moving forward, more work is needed to assure that depression treatment is reaching those with the greatest severity of symptoms.
Table 2.
Characteristics of Adolescents with Depression (PHQ9≥11) by Mental health use status as determined in table 1 (N= 110)
| Variable | No MHS use (N =52) | MHS use (N =58) | P value |
|---|---|---|---|
|
| |||
| N (%) or Mean (SD) | N (%) or Mean (SD) | ||
|
| |||
|
YOUTH CHARACTERISTICS
| |||
| Mean Age | 15.0 (1.3) | 15.4 (1.2) | 0.381 |
|
| |||
| Male Sex | 19 (37) | 13 (22) | 0.101 |
|
| |||
| Race | |||
| White | 33 (63) | 39 (67) | 0.271 |
| African American | 0 (0) | 3 (5) | |
| Asian/Pacific Islander | 2 (4) | 3 (5) | |
| Native American | 0 (0) | 0 (0) | |
| Other | 17 (33) | 13 (22) | |
|
| |||
| Hispanic Ethnicity | 3 (6) | 4 (7) | 0.871 |
|
| |||
| PHQ-9 Score at baseline | 14.4 ± 3.2 | 15.2 ± 3.9 | 0.282 |
|
| |||
| Suicidal ideation | 5 (10) | 9 (16) | 0.351 |
|
| |||
| SCARED Score | 3.1 ± 1.9 | 3.4 ± 2.1 | 0.572 |
|
| |||
| Columbia Impairment Scale | 24.2 ± 7.5 | 23 ± 7.5 | 0.322 |
|
| |||
| CRAFFT | 1.5±1.6 | 1.4±1.5 | 0.681 |
|
| |||
| PCDS | 374 ± 581 | 583 ± 805 | 0.0053 |
|
| |||
| PARENT CHARACTERISTICS | |||
|
| |||
| Parent History of Depression/Anxiety | 13 (27) | 25 (43) | 0.0741 |
|
| |||
| Parent History of Depression/Anxiety Treatment | 12 (92) | 23 (92) | 0.971 |
|
| |||
| Parent Report of Youth Internalizing symptoms | 4.0 ± 2.1 | 6.0 ± 2.1 | < 0.0012 |
|
| |||
| Parent Report of Youth Externalizing Symptoms | 3.8 ± 2.8 | 4.0 ± 3.2 | 0.172 |
Mental Health Service = MHS; PCDS = Pediatric Chronic Disease Score;
Pearson test;
Wilcoxon test;
Proportional odds likelihood ratio test
Acknowledgments
Funding Sources: This work was supported by grants from the Group Health Community Foundation Child and Adolescent Grant Program, the University of Washington Royalty Research Fund, a Seattle Children’s Hospital Steering Committee Award and through a K23 award from the NIMH for Dr. Richardson (5K23 MH069814-01A1).
Abbreviations
- SES
socioeconomic status
- MHS
mental health services
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zahn-Waxler C, Shirtcliff EA, Marceau K. Disorders of childhood and adolescence: gender and psychopathology. Annu Rev Clin Psychol. 2008;4:275–303. doi: 10.1146/annurev.clinpsy.3.022806.091358. [DOI] [PubMed] [Google Scholar]
- 3.Birmaher B, Brent DA, Benson RS. Summary of the practice parameters for the assessment and treatment of children and adolescents with depressive disorders. American Academy of Child and Adolescent Psychiatry. J Am Acad Child Adolesc Psychiatry. 1998;37(11):1234–1238. doi: 10.1097/00004583-199811000-00029. [DOI] [PubMed] [Google Scholar]
- 4.Cheung A, Dewa C, Cairney J, Veldhuizen S, Schaffer A. Factors associated with use of mental health services for depressed and/or suicidal youth aged 15–24. Community Ment Health J. 2009;45(4):300–306. doi: 10.1007/s10597-009-9205-8. [DOI] [PubMed] [Google Scholar]
- 5.Cummings JR, Druss BG. Racial/ethnic differences in mental health service use among adolescents with major depression. J Am Acad Child Adolesc Psychiatry. 2011;50(2):160–170. doi: 10.1016/j.jaac.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Domino ME, Burns BJ, Mario J, Reinecke MA, Vitiello B, Weller EB, et al. Service use and costs of care for depressed adolescents: who uses and who pays? J Clin Child Adolesc Psychol. 2009;38(6):826–836. doi: 10.1080/15374410903259023. [DOI] [PubMed] [Google Scholar]
- 7.Kataoka SH, Zhang L, Wells KB. Unmet need for mental health care among U.S. children: variation by ethnicity and insurance status. Am J Psychiatry. 2002;159(9):1548–1555. doi: 10.1176/appi.ajp.159.9.1548. [DOI] [PubMed] [Google Scholar]
- 8.Katon WJ, Richardson L, Russo J, Lozano P, McCauley E. Quality of mental health care for youth with asthma and comorbid anxiety and depression. Med Care. 2006;44(12):1064–1072. doi: 10.1097/01.mlr.0000237421.17555.8f. [DOI] [PubMed] [Google Scholar]
- 9.Richardson LP, McCauley E, McCarty CA, Grossman DC, Myaing M, Zhou C, et al. Predictors of persistence after a positive depression screen among adolescents. Pediatrics. 2012;130(6):e1541–1548. doi: 10.1542/peds.2012-0450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Richardson LP, Russo JE, Lozano P, McCauley E, Katon W. Factors associated with detection and receipt of treatment for youth with depression and anxiety disorders. Acad Pediatr. 2010;10(1):36–40. doi: 10.1016/j.acap.2009.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Potter R, Mars B, Eyre O, Legge S, Ford T, Sellers R, et al. Missed opportunities: mental disorder in children of parents with depression. Br J Gen Pract. 2012;62(600):e487–493. doi: 10.3399/bjgp12X652355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cunningham PJ, Freiman MP. Determinants of ambulatory mental health services use for school-age children and adolescents. Health Serv Res. 1996;31(4):409–427. [PMC free article] [PubMed] [Google Scholar]
- 13.Zimmerman FJ. Social and economic determinants of disparities in professional help-seeking for child mental health problems: evidence from a national sample. Health Serv Res. 2005;40(5 Pt 1):1514–1533. doi: 10.1111/j.1475-6773.2005.00411.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tanielian T, Jaycox LH, Paddock SM, Chandra A, Meredith LS, Burnam MA. Improving treatment seeking among adolescents with depression: understanding readiness for treatment. J Adolesc Health. 2009;45(5):490–498. doi: 10.1016/j.jadohealth.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 15.Wu P, Hoven CW, Cohen P, Liu X, Moore RE, Tiet Q, et al. Factors associated with use of mental health services for depression by children and adolescents. Psychiatr Serv. 2001;52(2):189–195. doi: 10.1176/appi.ps.52.2.189. [DOI] [PubMed] [Google Scholar]
- 16.Wu P, Katic BJ, Liu X, Fan B, Fuller CJ. Mental health service use among suicidal adolescents: findings from a U.S. national community survey. Psychiatr Serv. 2010;61(1):17–24. doi: 10.1176/ps.2010.61.1.17. [DOI] [PubMed] [Google Scholar]
- 17.Wu P, Hoven CW, Bird HR, Moore RE, Cohen P, Alegria M, et al. Depressive and disruptive disorders and mental health service utilization in children and adolescents. J Am Acad Child Adolesc Psychiatry. 1999;38(9):1081–1090. doi: 10.1097/00004583-199909000-00010. discussion 1090–1082. [DOI] [PubMed] [Google Scholar]
- 18.Cornelius JR, Pringle J, Jernigan J, Kirisci L, Clark DB. Correlates of mental health service utilization and unmet need among a sample of male adolescents. Addict Behav. 2001;26(1):11–19. doi: 10.1016/s0306-4603(00)00075-7. [DOI] [PubMed] [Google Scholar]
- 19.Logan DE, King CA. Parental identification of depression and mental health service use among depressed adolescents. J Am Acad Child Adolesc Psychiatry. 2002;41(3):296–304. doi: 10.1097/00004583-200203000-00009. [DOI] [PubMed] [Google Scholar]
- 20.Sellers R, Collishaw S, Rice F, Thapar AK, Potter R, Mars B, et al. Risk of psychopathology in adolescent offspring of mothers with psychopathology and recurrent depression. Br J Psychiatry. 2012 doi: 10.1192/bjp.bp.111.104984. [DOI] [PubMed] [Google Scholar]
- 21.Amaddeo F, Jones J. What is the impact of socio-economic inequalities on the use of mental health services? Epidemiol Psichiatr Soc. 2007;16(1):16–19. [PubMed] [Google Scholar]
- 22.Mulvale G, Hurley J. Insurance coverage and the treatment of mental illness: effect on medication and provider use. J Ment Health Policy Econ. 2008;11(4):177–199. [PubMed] [Google Scholar]
- 23.Williams SB, O’Connor EA, Eder M, Whitlock EP. Screening for child and adolescent depression in primary care settings: a systematic evidence review for the US Preventive Services Task Force. Pediatrics. 2009;123(4):e716–735. doi: 10.1542/peds.2008-2415. [DOI] [PubMed] [Google Scholar]
- 24.McCarty CA, Russo J, Grossman DC, Katon W, Rockhill C, McCauley E, et al. Adolescents with suicidal ideation: health care use and functioning. Acad Pediatr. 2011;11(5):422–426. doi: 10.1016/j.acap.2011.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fishman PA, Shay DK. Development and estimation of a pediatric chronic disease score using automated pharmacy data. Med Care. 1999;37(9):874–883. doi: 10.1097/00005650-199909000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Richardson LP, McCauley E, Grossman DC, McCarty CA, Richards J, Russo JE, et al. Evaluation of the Patient Health Questionnaire-9 Item for detecting major depression among adolescents. Pediatrics. 2010;126(6):1117–1123. doi: 10.1542/peds.2010-0852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bird HRS, David, Fisher, Prudence, Madalyn S, et al. The Columbia Impairment Scale (CIS): Pilot finding on a measure of global impairment for children and adolescents. International Journal of Methods in Psychiatric Research. 1993;3(3):167–176. [Google Scholar]
- 28.Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. J Am Acad Child Adolesc Psychiatry. 1999;38(10):1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- 29.Knight JR, Sherritt L, Harris SK, Gates EC, Chang G. Validity of brief alcohol screening tests among adolescents: a comparison of the AUDIT, POSIT, CAGE, and CRAFFT. Alcohol Clin Exp Res. 2003;27(1):67–73. doi: 10.1097/01.ALC.0000046598.59317.3A. [DOI] [PubMed] [Google Scholar]
- 30.Gardner W, Lucas A, Kolko DJ, Campo JV. Comparison of the PSC-17 and alternative mental health screens in an at-risk primary care sample. J Am Acad Child Adolesc Psychiatry. 2007;46(5):611–618. doi: 10.1097/chi.0b013e318032384b. [DOI] [PubMed] [Google Scholar]
- 31.Campo JV, Jansen-McWilliams L, Comer DM, Kelleher KJ. Somatization in pediatric primary care: association with psychopathology, functional impairment, and use of services. J Am Acad Child Adolesc Psychiatry. 1999;38(9):1093–1101. doi: 10.1097/00004583-199909000-00012. [DOI] [PubMed] [Google Scholar]
- 32.Farmer EM, Stangl DK, Burns BJ, Costello EJ, Angold A. Use, persistence, and intensity: patterns of care for children’s mental health across one year. Community Ment Health J. 1999;35(1):31–46. doi: 10.1023/a:1018743908617. [DOI] [PubMed] [Google Scholar]
- 33.Gould MS, Marrocco FA, Hoagwood K, Kleinman M, Amakawa L, Altschuler E. Service use by at-risk youths after school-based suicide screening. J Am Acad Child Adolesc Psychiatry. 2009;48(12):1193–1201. doi: 10.1097/CHI.0b013e3181bef6d5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wisdom JP, Agnor C. Family heritage and depression guides: family and peer views influence adolescent attitudes about depression. J Adolesc. 2007;30(2):333–346. doi: 10.1016/j.adolescence.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 35.Cheung AH, Zuckerbrot RA, Jensen PS, Ghalib K, Laraque D, Stein RE. Guidelines for Adolescent Depression in Primary Care (GLAD-PC): II. Treatment and ongoing management. Pediatrics. 2007;120(5):e1313–1326. doi: 10.1542/peds.2006-1395. [DOI] [PubMed] [Google Scholar]
- 36.U.S. Department of Commerse. State & County QuickFacts. United States’ Census Bureau; [Accessed 7/24/2013]. http://quickfacts.census.gov/qfd/states/00000.html. [Google Scholar]
- 37.Katon W, Von Korff M, Lin E, et al. Stepped collaborative care for primary care patients with persistent symptoms of depression: A randomized trial. Archives of General Psychiatry. 1999;56(12):1109–1115. doi: 10.1001/archpsyc.56.12.1109. [DOI] [PubMed] [Google Scholar]