Abstract
We evaluated culture-negative, community-acquired endocarditis by using indirect immunofluorescent assays and molecular analyses for Bartonella spp. and Coxiella burnetii and found a prevalence of 19.6% and 7.8%, respectively. Our findings reinforce the need to study these organisms in patients with culture-negative, community-acquired endocarditis, especially B. henselae in cat owners.
Keywords: endocarditis, Bartonella, Coxiella burnettii, Brazil, zoonoses, bacteria
Worldwide, Bartonella spp. and Coxiella burnetii endocarditis have varied prevalences and clinical effects (1,2). Detection is difficult in routine blood cultures, so different diagnosis methods are needed. Our study investigated the frequency of and the risk factors for Bartonella spp. and C. burnetii infection in cases of culture-negative, community-acquired endocarditis.
The Study
During January 2004–January 2009, the Infection Control Team from the university hospital at São Paulo, Brazil (Instituto do Coração–Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo) used active surveillance to identify 369 patients with endocarditis. The study focused on community-acquired endocarditis caused by fastidious bacteria. Patients >18 years of age with confirmed endocarditis were included as a prospective inception cohort of patients (3). Excluded were patients with health care–associated endocarditis (i.e., patients with prosthetic valve endocarditis in the first postoperative year, hemodialysis patients, and nosocomial endocarditis patients) (4).
Indirect immunofluorescence assays (IFAs) were performed for all patients with negative blood cultures <7 days after admission at a referral center for rickettsial infections (Adolfo Lutz Institute, São Paulo). The same observer analyzed all assays; IgG titers ≥1:800 for B. henselae and B. quintana (5) and anti–phase I IgG titers ≥1:800 for C. burnetii (6) were considered positive (Technical Appendix). New diagnostic criteria for Q fever endocarditis were used (6).
Immunohistochemical and molecular methods were applied to valve tissue specimens and serum samples of patients whose serum samples were positive for Bartonella spp. or C. burnetii. DNA from paraffin-embedded valve tissue specimens and serum samples were extracted. Samples positive for Bartonella by IFA were analyzed by using 5 different PCRs to 4 distinct regions. Tissue and serum DNA from patients positive for C. burnettii by IFA were tested by quantitative PCR (Technical Appendix Table 1) (7).
Of the 369 identified endocarditis patients, 221 (59.9%) were included in the study; median age of included patients was 53 years. Of included patients, 144 (65.2%) were male; 107 (48.4%) had prosthetic valves; 209 (94.6%) had left-sided endocarditis; and 152 (68.8%) had concurrent conditions. Of patients with concurrent conditions, 62 (40.8%) had hypertension, 17 (11.2%) had diabetes, 53 (34.9%) had heart failure, and 36 (23.7%) had other conditions. Of the 221 patients included in the study, microorganisms were identified in 170 (76.9%); specimens from 51 (23.1%) patients were culture negative.
A standardized questionnaire regarding exposure to cats, ectoparasites, or farm animals was administered to patients with culture-negative endocarditis. For the 170 samples in which microorganisms were found, the most commonly identified bacteria were viridans-type Streptococci (81 [47.6%]), Streptococcus bovis (17 [10.0%]), S. pneumonie (6 [3.5%]), S. agalactiae (2 [1.2%]), S. pyogenes (2 [1.2%]), Enterococcus fecalis (13 [7.6%]), E. faecium (3 [1.8%]), other enterococci (4 [2.4%]) and Staphylococcus aureus (14 [8.2%]).
For the 221 patients in the study, findings from 10 (4.5%; 95% CI 3.96%–5.09%) patients (Figure) showed Bartonella spp., and 4 (1.8%; 95% CI 1.58%–2.04%) showed C. burnetii endocarditis. For the 51 culture-negative endocarditis patients, Bartonella spp. was found in cultures from 10 (19.6%; 95% CI 9.8%–33.1%), and C. burnetii was found in 4 (7.8%; 95% CI 2.2%–18.9%). The Table shows the immunohistochemical and molecular biology analyses for patients with positive IFA results. Bartonella spp. DNA was detected with >1 PCR in all 6 patients whose paraffin-embedded valve tissue samples were found positive for Bartonella spp. For the other 4 patients with Bartonella spp., DNA was detected in 2 serum samples. Amplicons were sequenced, and their analyses showed that the cultures from 2 patients had 100% similarity with B. quintana (GenBank accession no. BX897700.1); cultures from 4 patients had 100% similarity with B. henselae infection (GenBank accession no. BX897699.1). Cultures from 2 patients were positive for Bartonella spp. by using IFA but negative by using PCR.
Figure.
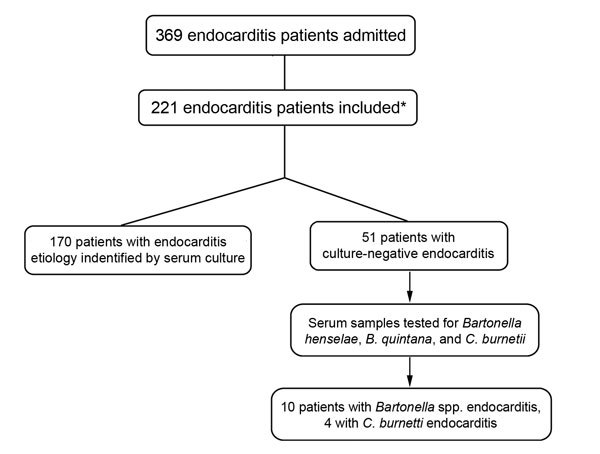
Distribution of patients etiologically diagnosed with endocarditis and admitted to the heart institute (Instituto do Coração) at the University of São Paulo Medical School, Sao Paulo, Brazil, January 2004–January 2009. *A modified Duke criteria (3) was used to determine inclusion of 221 patients. Excluded were 148 patients: 58 with unconfirmed endocarditis, 28 with endocarditis caused by cardiac implantable electronic devices, 47 with nosocomial endocarditis, and 15 hemodialysis patients.
Table. Serologic, immunohistopathologic, and molecular test results for patients with infective endocarditis caused by Bartonella spp. or Coxiella burnetii, Brazil*.
| Patient no., by infection type | Serum IgG ≥800 by IFA† | Immunohistochemical analysis of cardiac valve vegetation |
Microorganism by histologic analysis | PCR‡ | Species of Bartonella | |
|---|---|---|---|---|---|---|
| Bartonella spp. | C. burnetii | |||||
| Bartonella spp. | ||||||
| 1 | + | + | Neg | Gram-negative coccobacilli | + | B. quintana |
| 2 | + | + | Neg | Gram-negative coccobacilli | + | B. henselae |
| 3 | + | + | Neg | None | + | B. henselae |
| 4 | + | NA | NA | NA | Neg | NA |
| 5 | + | + | Neg | Gram-negative coccobacilli | + | NA |
| 6 | + | + | Neg | Gram-negative coccobacilli | + | B. quintana |
| 7 | + | NA | NA | NA | + | B. henselae |
| 8 | + | NA | NA | NA | + | NA |
| 9 | + | NA | NA | NA | Neg | NA |
| 10 | + | + | Neg | Gram-negative cocci | + | B. henselae |
| C. burnetii | Serum anti–phase I IgG ≥800 by IFA§ | Immunohistochemical analysis of cardiac valve vegetation |
Microorganism by histologic analysis | PCR‡ | Q fever endocarditis (6) | |
|---|---|---|---|---|---|---|
| Bartonella spp. | C. burnetii | |||||
| 11 | + | Neg | + | Small gram-negative coccobacilli | + | Definite 2A criteria |
| 12 | + | Neg | + | None | + | Definite 2A criteria |
| 13 | + | Neg | + | None | + | Definite 2A criteria |
| 14 | + | NA | NA | NA | + | Definite 2B criteria¶ |
*IFA, immunofluorescence assay; +, positive; Neg, negative; NA, material not available for analysis. ¶Serologic result >6,400 and vegetation on ecocardiography. †B. henselae or B. quintana. ‡Serum or tissue sample. §C. burnetii.
All patients used antimicrobial drugs for 7 days before sample collection. All endocarditis patients whose cultures were found to be positive for C. burnetii by using IFA were also positive by using quantitative PCR: 3 by serum samples and 2 by paraffin-embedded valve tissue specimens (Technical Appendix Table 2).
Clinical and follow-up findings from Bartonella spp. and C. burnetii endocarditis patients are shown in Technical Appendix Table 3. Bartonella spp. infection was associated with low levels of C-reactive protein on admission and chronic symptoms related to endocarditis (Technical Appendix Table 4). Three (75%) of 4 patients with Bartonella henselae endocarditis were associated with a cat living in the patient’s home, compared with 6 (12.8%) of 47 patients with culture-negative Bartonella henselae negative endocarditis (p = 0.015 by Student t-test). Hydroxychloroquine was unavailable in our facility; therefore, we used a second-line therapy for C. burnetii endocarditis. Hydroxychloroquine was replaced with ciprofloxacin, and treatment was extended for 72 months (8). Subsequently, symptoms resolved, and antibody titers reduced substantially, considered a favorable response (9) (Technical Appendix Table 3).
Conclusions
In this study, the systematic use of IFA detected a 4.5% (10/221) prevalence of community-acquired endocarditis due to Bartonella spp. and a 1.8% (4/221) prevalence due to C. burnetii. For the 51 culture-negative endocarditis patients, IFA enabled recognition of the endocarditis etiology in 14 (27.5%) patients (Bartonella spp. in 10 [19.6%] and C. burnetii in 4 [7.8%]). Some of these patients have been recognized as having the first cases of endocarditis caused by these microorganisms in Brazil (10,11).
Prevalences of Bartonella spp. endocarditis vary worldwide by region studied (1). In a broad series of 759 culture-negative endocarditis patients in France, serum samples showed high sensitivity for detection of C. burnetii and Bartonella spp. infections, compared with other diagnostic tools, such as PCR, cell culture, and immunohistochemical analysis (2). In Brazil, studies of Bartonella spp. infection among culture-negative endocarditis patients have shown varied results. A retrospective case series of 51 surgically treated, culture-negative endocarditis patients found 2 cases of Bartonella spp. and 1 case of C. burnetii by using PCR on valvular tissue (12). Another series of 46 culture-negative endocarditis patients from the city of São Paulo used PCR to investigate Bartonella spp. in blood and found 13 (28%) patients with positive results (13).
We found an association between B. henselae endocarditis and the presence of a cat living at a patient´s home, a risk factor indicating that clinicians should consider this infection when assessing endocarditis patients. The relatively small sample of patients with endocarditis caused by Bartonella spp. and C. burnetii limited the statistical analyses of factors associated with these infections. Serologic investigations of infections by these agents were applied only to patients with negative cultures. Although rare (2,14), co-infection by these microorganisms in culture-positive endocarditis is possible, so frequency of Bartonella spp. and C. burnetii infections in these patients may be higher than shown. Our study indicates that systematic serologic research for Bartonella spp. and C. burnetii in community-acquired, culture-negative endocarditis may be clinically useful, particularly in screening for B. henselae in cat owners.
Technical Appendix. Investigative methods and findings for patients diagnosed with endocarditis and admitted to the heart institute (Instituto do Coração) at the University of Sao Paulo Medical School, Sao Paulo, Brazil, January 2004–January 2009.
Biography
Dr. Siciliano is an infectious disease specialist working in infection control at the Heart Institute at the university hospital at São Paulo, Brazil, a tertiary care hospital dedicated to care of heart disease patients. His clinical research interest is endocarditis.
Footnotes
Suggested citation for this article: Siciliano RF, Castelli JB, Mansur AJ, Pereira dos Santos F, Colombo S, Nascimento EM, et al. Bartonella spp. and Coxiella burnetii associated with community-acquired, culture-negative endocarditis, Brazil. Emerg Infect Dis. 2015 Aug [date cited]. http://dx.doi.org/10.3201/eid2108.140343
References
- 1.Tattevin P, Watt G, Revest M, Arvieux C, Fournier PE. Update on blood culture-negative endocarditis. Med Mal Infect. 2015;45:1–8. 10.1016/j.medmal.2014.11.003 [DOI] [PubMed] [Google Scholar]
- 2.Fournier PE, Thuny F, Richet H, Lepidi H, Casalta JP, Arzouni JP, et al. Comprehensive diagnostic strategy for blood culture-negative endocarditis: a prospective study of 819 new cases. Clin Infect Dis. 2010;51:131–40. 10.1086/653675 [DOI] [PubMed] [Google Scholar]
- 3.Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG Jr, Ryan T, et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis. 2000;30:633–8. 10.1086/313753 [DOI] [PubMed] [Google Scholar]
- 4.Ben-Ami R, Giladi M, Carmeli Y, Orni-Wasserlauf R, Siegman-Igra Y. Hospital-acquired infective endocarditis: should the definition be broadened? Clin Infect Dis. 2004;38:843–50. 10.1086/381971 [DOI] [PubMed] [Google Scholar]
- 5.Fournier PE, Mainardi JL, Raoult D. Value of microimmunofluorescence for diagnosis and follow-up of Bartonella endocarditis. Clin Diagn Lab Immunol. 2002;9:795–801 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raoult D. Chronic Q fever: expert opinion versus literature analysis and consensus. J Infect. 2012;65:102–8. 10.1016/j.jinf.2012.04.006 [DOI] [PubMed] [Google Scholar]
- 7.Schneeberger PM, Hermans MH, van Hannen EJ, Schellekens JJ, Leenders AC, Wever PC. Real-time PCR with serum samples is indispensable for early diagnosis of acute Q fever. Clin Vaccine Immunol. 2010;17:286–90. 10.1128/CVI.00454-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raoult D, Houpikian P, Tissot Dupont H, Riss JM, Arditi-Djiane J, Brouqui P. Treatment of Q fever endocarditis: comparison of 2 regimens containing doxycycline and ofloxacin or hydroxychloroquine. Arch Intern Med. 1999;159:167–73. 10.1001/archinte.159.2.167 [DOI] [PubMed] [Google Scholar]
- 9.Rolain JM, Mallet MN, Raoult D. Correlation between serum doxycycline concentrations and serologic evolution in patients with Coxiella burnetii endocarditis. J Infect Dis. 2003;188:1322–5. 10.1086/379082 [DOI] [PubMed] [Google Scholar]
- 10.Siciliano RF, Strabelli TM, Zeigler R, Rodrigues C, Castelli JB, Grinberg M, et al. Infective endocarditis due to Bartonella spp. and Coxiella burnetii: experience at a cardiology hospital in Sao Paulo, Brazil. Ann N Y Acad Sci. 2006;1078:215–22. 10.1196/annals.1374.123 [DOI] [PubMed] [Google Scholar]
- 11.Siciliano RF, Ribeiro HB, Furtado RH, Castelli JB, Sampaio RO, Santos FC, et al. Endocarditis due to Coxiella burnetii (Q fever): a rare or underdiagnosed disease? Case report [in Portuguese]. Rev Soc Bras Med Trop. 2008;41:409–12. 10.1590/S0037-86822008000400017 [DOI] [PubMed] [Google Scholar]
- 12.Lamas CC, Ramos RG, Lopes GQ, Santos MS, Golebiovski WF, Weksler C, et al. Bartonella and Coxiella infective endocarditis in Brazil: molecular evidence from excised valves from a cardiac surgery referral center in Rio de Janeiro, Brazil, 1998 to 2009. Int J Infect Dis. 2013;17:e65–6. 10.1016/j.ijid.2012.10.009 [DOI] [PubMed] [Google Scholar]
- 13.Corrêa FG, Pontes CLS, Verzola RMM, Mateos JCP, Velho PENF, Schijman AG, et al. Association of Bartonella spp bacteremia with Chagas cardiomyopathy, endocarditis and arrythmias in patients from South America. Braz J Med Biol Res. 2012;45:644–51. 10.1590/S0100-879X2012007500082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Raoult D, Casalta JP, Richet H, Khan M, Bernit E, Rovery C, et al. Contribution of systematic serological testing in diagnosis of infective endocarditis. J Clin Microbiol. 2005;43:5238–42. 10.1128/JCM.43.10.5238-5242.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Technical Appendix. Investigative methods and findings for patients diagnosed with endocarditis and admitted to the heart institute (Instituto do Coração) at the University of Sao Paulo Medical School, Sao Paulo, Brazil, January 2004–January 2009.


