Abstract
Purpose
Patients with cancer commonly use complementary and alternative medicine, including herbs and supplements (HS), during cancer treatment. This national survey explored oncologists' knowledge, attitudes, and practice patterns regarding HS use by their patients.
Methods
A survey was sent by mail and e-mail to a random sample of 1,000 members of the American Society for Clinical Oncology. The questions covered several topics: communication patterns, attitudes about HS, education about HS, response to HS use among hypothetical patients with cancer, knowledge of HS adverse effects, and demographic information.
Results
Among eligible oncologists, 392 (42%) responded to the questionnaire. Most were white (75%) men (71%), with a mean age of 48 years (standard deviation, 9.8 years). On average, oncologists discussed use of HS with 41% of their patients; only 26% of discussions were initiated by the oncologist. Two of three oncologists indicated they did not have enough knowledge to answer questions from patients regarding HS, and 59% had not received any education about the topic. Physician factors associated with having initiated discussions with patients about the use of HS included female sex, higher self-reported knowledge, prior education about HS, increased knowledge about HS adverse effects and interactions, and estimating that > 40% of one's patients with cancer use HS.
Conclusion
Fewer than one half of oncologists are initiating discussions with patients about HS use, and many indicate that lack of knowledge and education is a barrier to such discussions. Improving physician education about HS may facilitate more physician-patient communication about this important topic.
INTRODUCTION
Oncologists commonly discuss with patients options for treating cancer, and as interest in and use of complementary and alternative medicine (CAM) has grown, so too have questions about the use of CAM for cancer treatment. The use of CAM increased in the United States among adults from 33.8% in 1990 to 42.1% in 1997,1 and studies suggest the prevalence of CAM use among patients with cancer exceeds that found among the general population. In 2000, a study from MD Anderson Cancer Center reported patient use of CAM at 68.7%, even after excluding spiritual and psychotherapy practices, and 88.2% of patients with advanced cancer enrolled onto phase I clinical trials at the Mayo Clinic reported using CAM.2,3 A similar prevalence has been documented in pediatric populations.4 The study conducted at MD Anderson Cancer Center also documented limited communication and discrepant views regarding CAM therapies.5 Similarly, in an international study, we found limited communication between patients and oncologists regarding CAM.6 In that study, despite reporting limited formal training about CAM therapies, nearly two thirds of oncologists indicated they would allow patients to use CAM during treatment of a curable cancer.
The prevalence of CAM use looms important, because many biologically based CAM modalities, such as herbs and supplements (HS), can interfere with chemotherapy efficacy and/or increase the risk for treatment-related toxicity and other complications. St John's wort, Panax ginseng, and green tea have all been found to have toxicities and to interact with medications, including chemotherapies.7–10 One study of adult patients with cancer estimated that 28% of patients were at risk for herbal interactions, and notably, 46% of these at-risk patients were being treated with curative intent.11 A more recent study of patients with ovarian cancer estimated that 40% were at risk of an interaction between the HS they were taking and their prescribed chemotherapy.12 Because HS use is prevalent and poses substantial risks to some patients, especially those undergoing active treatment, physicians are obligated to learn about commonly used HS and to inquire about patients' use of such therapies.
Research indicates that patients want to discuss the use of CAM with their clinicians,13 but little is known about whether and how oncologists specifically discuss the use of HS with their patients. To explore this area further, we conducted a national survey of US oncologists to explore their knowledge, opinions, and practices regarding the use of CAM by patients, focusing particularly on HS. We hypothesized that oncologists would report limited knowledge about HS and limited discussions with patients about such use and that they would underestimate the prevalence of HS use by patients.
METHODS
Participants were selected from the American Society for Clinical Oncology (ASCO) membership directory from the year 2008. Among those members who listed their specialty as medical oncology or medical oncology/hematology, provided a US mailing address, and provided an e-mail address, we selected at random 1,000 oncologists (approximately 5% of medical oncologists from directory). An initial mailing notified them that an e-mail would be sent asking for their participation in this study; it included a $5 gift card to Starbucks as a token of appreciation and survey incentive. Several days later, an e-mail was sent to all participants, using the address included in the ASCO directory. The e-mail included a unique URL link to a confidential Web-based questionnaire. When requested, we mailed or faxed a paper version of the questionnaire. Brief e-mail reminders were sent to nonresponders on a weekly basis for up to 8 weeks. In addition, those who had not responded by the end of the fourth week were mailed a paper version of the questionnaire with a self-addressed stamped return envelope. Recipients were considered eligible if their questionnaire was not returned undeliverable and if they reported actively practicing medical oncology/hematology. The study was approved by the institutional review board of the University of Chicago.
Questionnaire
The questionnaire was constructed by two of the authors (R.T.L., F.A.C.), and a focus group of oncologists refined the wording of questions and response elements for clarity. At the outset, participants indicated whether they were actively practicing hematology/oncology (if not, we asked them not to complete questionnaire). In the first section, participants were asked about the prevalence of HS use by patients, how they communicated with patients regarding HS, and whether they encouraged, discouraged, or were neutral about the use of HS (eg, “Please estimate the percentage of your patients who currently use herbs and/or supplements”). We defined HS in the survey as follows: “substances found in nature (such as vitamins, minerals, and herbs) that are taken at levels higher than those found in a typical diet. Some examples of herbs include gingko and St. John's Wort; while examples of supplements include mega-dose vitamins, glucosamine, and fish oil (NOT including standard doses of vitamins and minerals such as those in a multivitamin).” Lastly, if participants reported they did discuss the issue of HS with patients, we asked them to indicate how such discussions affected their physician-patient relationships. In the second section, participants indicated their agreement (ie, strongly agree, agree, disagree, or strongly disagree) with several statements about HS (eg, “I know enough to answer patients' questions about herbs and supplements”), and they indicated whether they personally used CAM therapies. The third section included two clinical vignettes. The first read as follows:
”You have just seen a newly diagnosed cancer patient. With chemotherapy, the patient has a less than 5% chance of 5 year survival and a median survival of less than 1 year. The patient tells you that he wants to combine treatment with the use of an unfamiliar herb about which there is limited published information.”
The second vignette was the same, except that the patient had an 85% chance of 5-year survival with chemotherapy. After each vignette, participants were asked to indicate: “In this case, would you most likely [strongly discourage, discourage, neutral opinion, encourage, strongly encourage, other] use of the herb.”
To assess participants' knowledge, we asked four questions regarding herbs that have documented potential harms for patients with cancer (eg, “A man with metastatic colon cancer is being treated with irinotecan. He wants to use the following supplements and herbs. Which one(s) should he avoid?”) For all four questions, response categories were: St John's wort, soy extract, gingko biloba, kava extracts, none of the above, and don't know. Respondents were asked to mark all answers that applied. Lastly, participants were asked to provide demographic information, including age, race, practice type, and religion.
Statistical Analysis
All data were coded and checked for errors by the principal investigator. Missing and ambiguous responses were excluded from analysis. Descriptive statistics (ie, frequency distribution, mean [± standard deviation (SD)], and median [range]) were used to summarize oncologist characteristics and outcome variables. Wilcoxon signed rank sum tests were performed to test for significant differences in the distribution of responses regarding the hypothetical patient with a curable cancer, as compared with those regarding the patient with incurable cancer.14 χ2 tests were performed to explore associations between oncologist characteristics and CAM practice patterns.15 Multivariable logistic regression models were used to determine whether associations persisted after controlling for demographics and other relevant predictors.16 Model building began with all variables having a P value ≤ .20 from the χ2 tests. A P value cutoff of .10 to enter and .05 to remain in the model were used. Age, sex, and race were kept in the model regardless of their significance. Once the list of variables to be used in our final model was selected, the functional form of each variable and multicollinearity between the variables were examined. All statistical analyses were performed using SAS software (version 9.3; SAS Institute, Cary, NC).
RESULTS
Among the 1,000 physicians randomly selected, 63 had nonworking addresses for both e-mail and postal mail; 24 were not actively practicing medical oncology/hematology, and seven did not indicate their specialty. A total of 392 participants responded for an adjusted response rate of 42%. Most (73%) responded online, and 98% of respondents completed at least 70% of the questions. Participants were from all 50 states and were predominantly men (71%), white (75%), and practicing in the community (58%), with a mean age of 48 years (SD, 9.8 years). One third of participants reported personal use of CAM therapies in the previous year (Table 1).
Table 1.
Respondent Characteristics (N = 392)

| Characteristic | No. | % |
|---|---|---|
| Age, years | ||
| Mean | 48.4 | |
| SD | 9.8 | |
| < 40 | 67 | 17.1 |
| 40-49 | 86 | 21.9 |
| 50-59 | 82 | 20.9 |
| > 60 | 45 | 11.5 |
| Sex | ||
| Male | 277 | 70.7 |
| Female | 111 | 28.3 |
| Practice setting | ||
| Academic | 160 | 40.8 |
| Community with academic affiliation | 79 | 20.2 |
| Community | 148 | 37.8 |
| Race | ||
| Black | 7 | 1.8 |
| Hispanic | 21 | 5.4 |
| East Asian or Pacific Islander | 30 | 7.7 |
| South Asian or Indian | 41 | 10.5 |
| White | 275 | 70.2 |
| Other | 9 | 2.3 |
| Personal use of CAM | ||
| Yes | 134 | 34.2 |
| No | 258 | 65.8 |
| Involved in clinical trial enrollment | ||
| Yes | 356 | 90.8 |
| No | 30 | 7.7 |
NOTE. Percentages may not add up to 100% because of missing values.
Abbreviations: CAM, complementary and alternative medicine; SD, standard deviation.
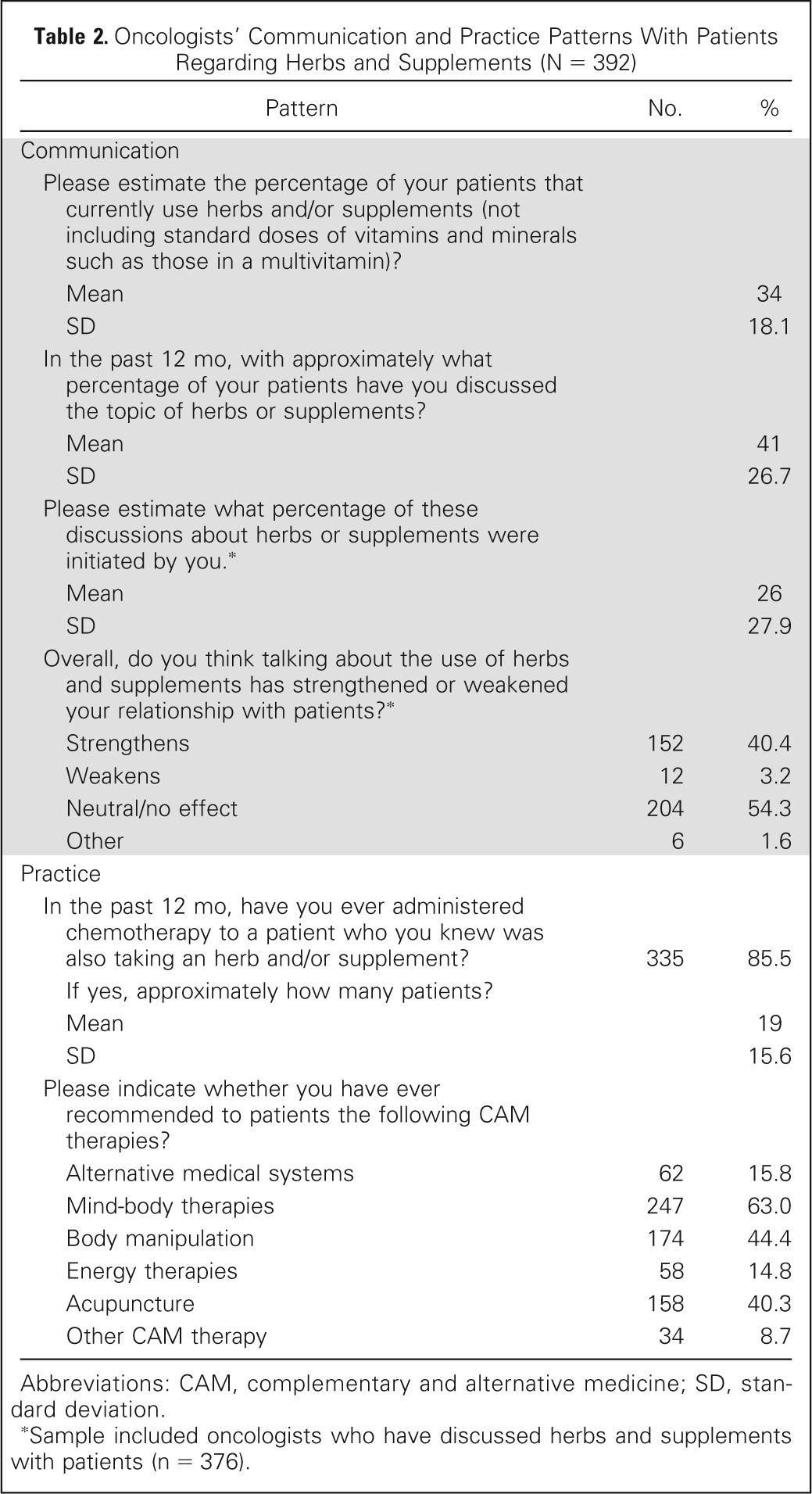
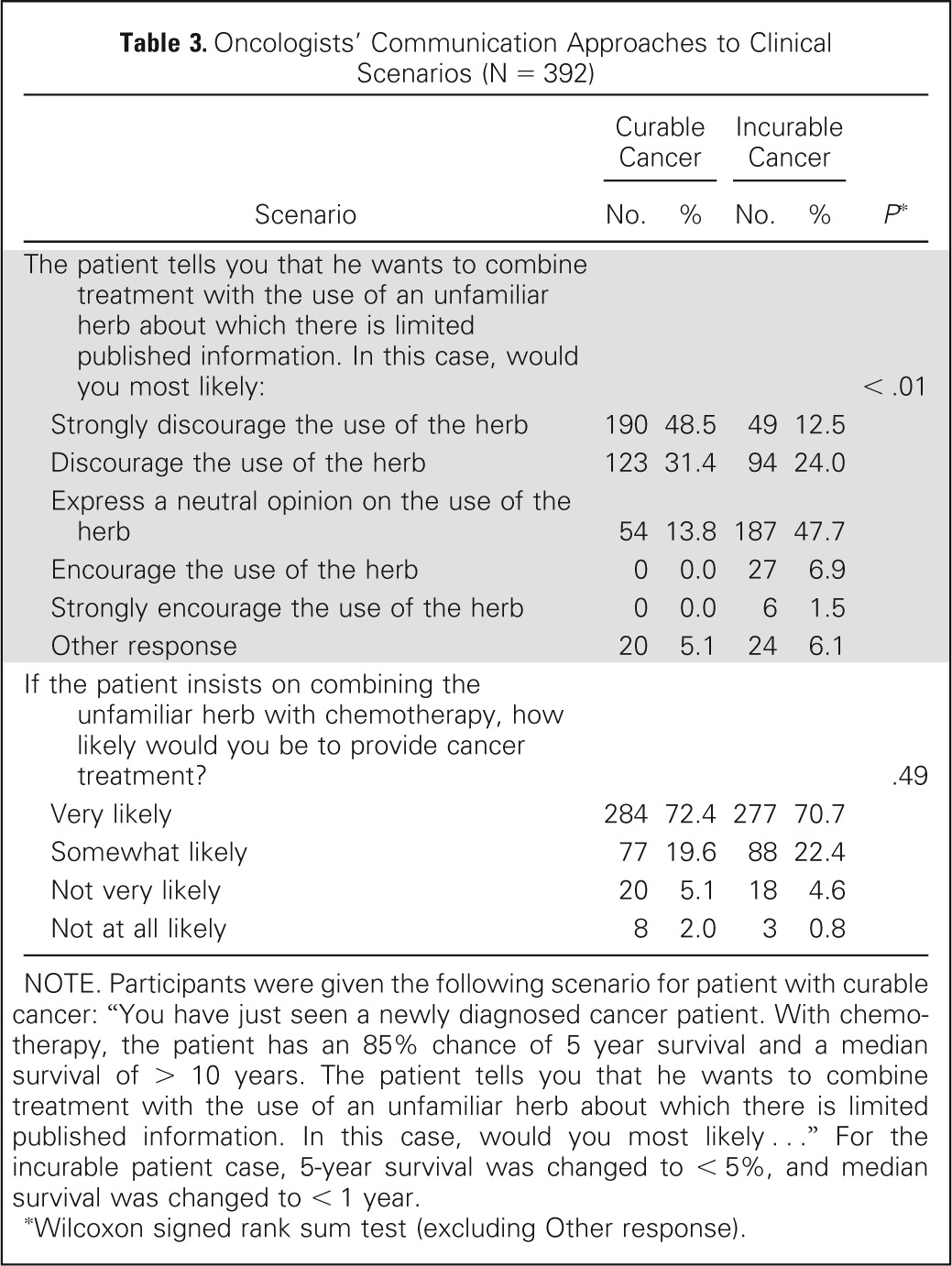
On average, respondents estimated that 34% (SD, 18.1%) of their patients were using HS and that they spoke with 41% (SD, 26.7%) of their patients about HS. Only one fourth of these discussions were initiated by oncologists. Oncologists were much more likely to believe that discussing HS strengthened their relationships with patients (40%) than they were to believe that it weakened the relationships (3%). Most (86%) reported providing chemotherapy to at least one patient in the previous 12 months who was concurrently taking HS, and on average, they estimated they had provided chemotherapy to 19 such patients in the past year (Table 2). When presented with a hypothetical patient with a potentially curable cancer, 80% of oncologists would actively discourage the use of an unknown herb with chemotherapy; however, when presented with a patient with an incurable cancer, only 37% would do so (with 48% remaining neutral). Regardless of the curability of the cancer, nine (90%) of 10 oncologists indicated they would likely provide chemotherapy even if the patient insisted on using the unknown herb (Table 3).
Table 2.
Oncologists' Communication and Practice Patterns With Patients Regarding Herbs and Supplements (N = 392)
| Pattern | No. | % |
|---|---|---|
| Communication | ||
| Please estimate the percentage of your patients that currently use herbs and/or supplements (not including standard doses of vitamins and minerals such as those in a multivitamin)? | ||
| Mean | 34 | |
| SD | 18.1 | |
| In the past 12 mo, with approximately what percentage of your patients have you discussed the topic of herbs or supplements? | ||
| Mean | 41 | |
| SD | 26.7 | |
| Please estimate what percentage of these discussions about herbs or supplements were initiated by you.* | ||
| Mean | 26 | |
| SD | 27.9 | |
| Overall, do you think talking about the use of herbs and supplements has strengthened or weakened your relationship with patients?* | ||
| Strengthens | 152 | 40.4 |
| Weakens | 12 | 3.2 |
| Neutral/no effect | 204 | 54.3 |
| Other | 6 | 1.6 |
| Practice | ||
| In the past 12 mo, have you ever administered chemotherapy to a patient who you knew was also taking an herb and/or supplement? | 335 | 85.5 |
| If yes, approximately how many patients? | ||
| Mean | 19 | |
| SD | 15.6 | |
| Please indicate whether you have ever recommended to patients the following CAM therapies? | ||
| Alternative medical systems | 62 | 15.8 |
| Mind-body therapies | 247 | 63.0 |
| Body manipulation | 174 | 44.4 |
| Energy therapies | 58 | 14.8 |
| Acupuncture | 158 | 40.3 |
| Other CAM therapy | 34 | 8.7 |
Abbreviations: CAM, complementary and alternative medicine; SD, standard deviation.
Sample included oncologists who have discussed herbs and supplements with patients (n = 376).
Table 3.
Oncologists' Communication Approaches to Clinical Scenarios (N = 392)
| Scenario | Curable Cancer |
Incurable Cancer |
P* | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| The patient tells you that he wants to combine treatment with the use of an unfamiliar herb about which there is limited published information. In this case, would you most likely: | < .01 | ||||
| Strongly discourage the use of the herb | 190 | 48.5 | 49 | 12.5 | |
| Discourage the use of the herb | 123 | 31.4 | 94 | 24.0 | |
| Express a neutral opinion on the use of the herb | 54 | 13.8 | 187 | 47.7 | |
| Encourage the use of the herb | 0 | 0.0 | 27 | 6.9 | |
| Strongly encourage the use of the herb | 0 | 0.0 | 6 | 1.5 | |
| Other response | 20 | 5.1 | 24 | 6.1 | |
| If the patient insists on combining the unfamiliar herb with chemotherapy, how likely would you be to provide cancer treatment? | .49 | ||||
| Very likely | 284 | 72.4 | 277 | 70.7 | |
| Somewhat likely | 77 | 19.6 | 88 | 22.4 | |
| Not very likely | 20 | 5.1 | 18 | 4.6 | |
| Not at all likely | 8 | 2.0 | 3 | 0.8 | |
NOTE. Participants were given the following scenario for patient with curable cancer: “You have just seen a newly diagnosed cancer patient. With chemotherapy, the patient has an 85% chance of 5 year survival and a median survival of > 10 years. The patient tells you that he wants to combine treatment with the use of an unfamiliar herb about which there is limited published information. In this case, would you most likely …” For the incurable patient case, 5-year survival was changed to < 5%, and median survival was changed to < 1 year.
Wilcoxon signed rank sum test (excluding Other response).
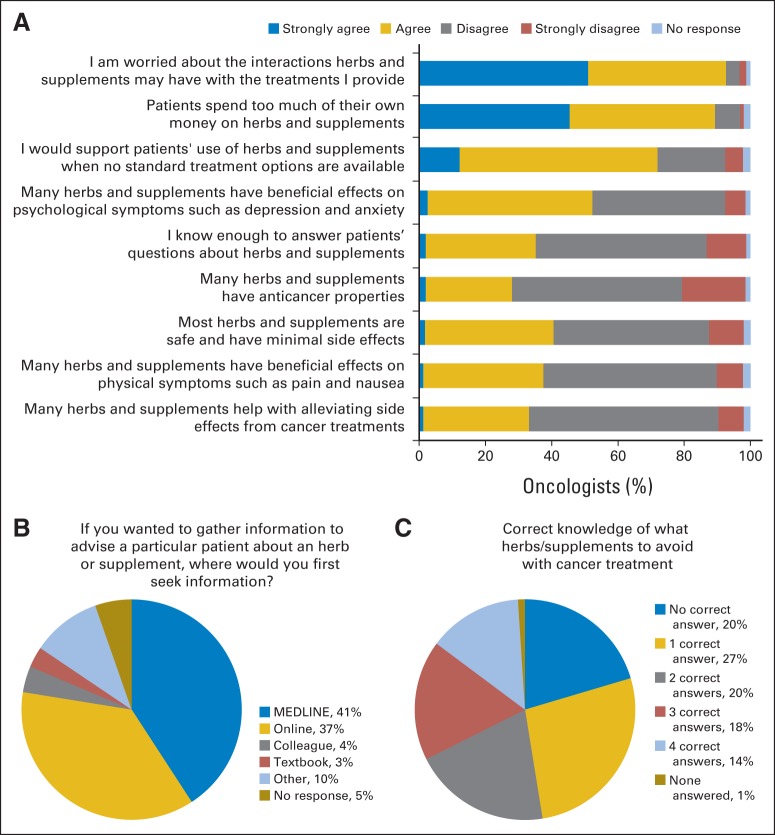
A majority (93%) of oncologists were concerned about potential interactions between HS and ongoing treatments, as well as about how much money patients spent on HS (89%). Two (64%) of three did not believe they knew enough to answer their patients' questions about HS, and fewer than half reported receiving any education on the topic. For those who had received some education, this was most commonly gained through informal discussions (76%) or lectures (70%), followed by conferences (38%), courses (14%), and other practices (31%; Fig 1).
Fig 1.
Oncologists' opinion patterns and knowledge about herbs and supplements (N = 392). (A) Percent of oncologists who agreed or disagreed with various statements about herbs and supplements (HS); (B) preferred sources of information about HS; (C) No. of questions about HS answered correctly by oncologists.
When asked about four specific HS-chemotherapy interactions, oncologists answered correctly about St John's wort and irinotecan (48%), gingko biloba and bleeding risk (39%), breast cancer and soy extracts (61%), and kava and liver damage (26%). Overall, only one third (32%) correctly answered at least three of the four questions, and 26% to 52% marked “I don't know” (respondents could mark more than one response category).
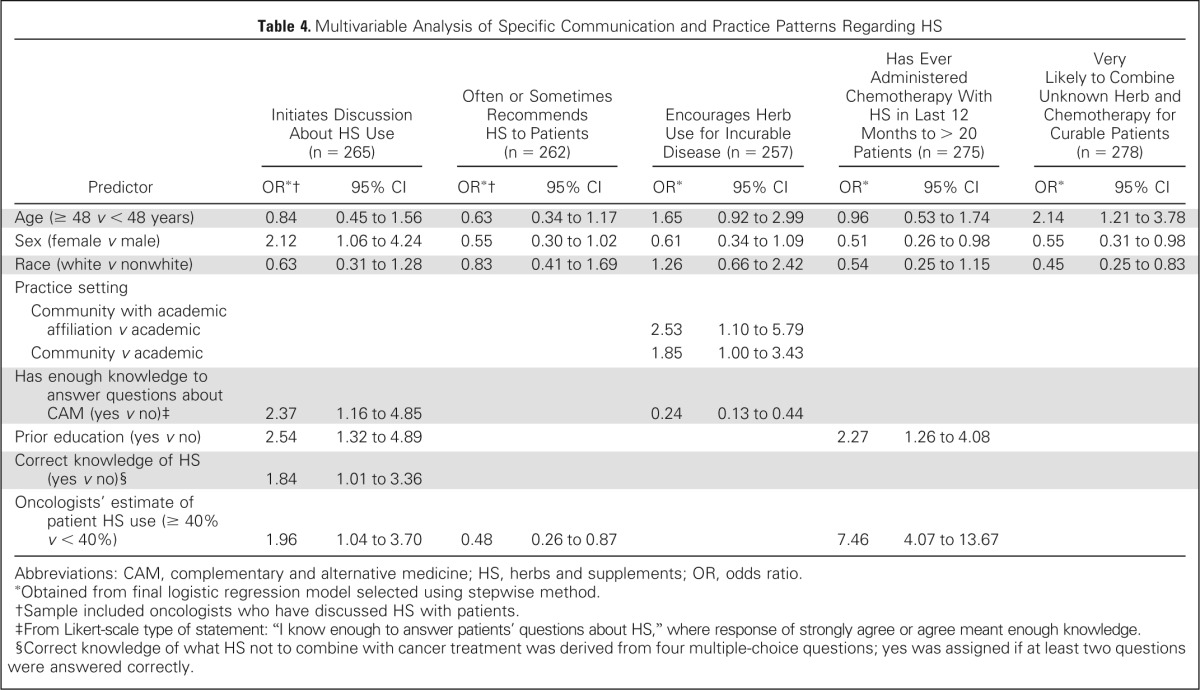
Multivariable Analysis
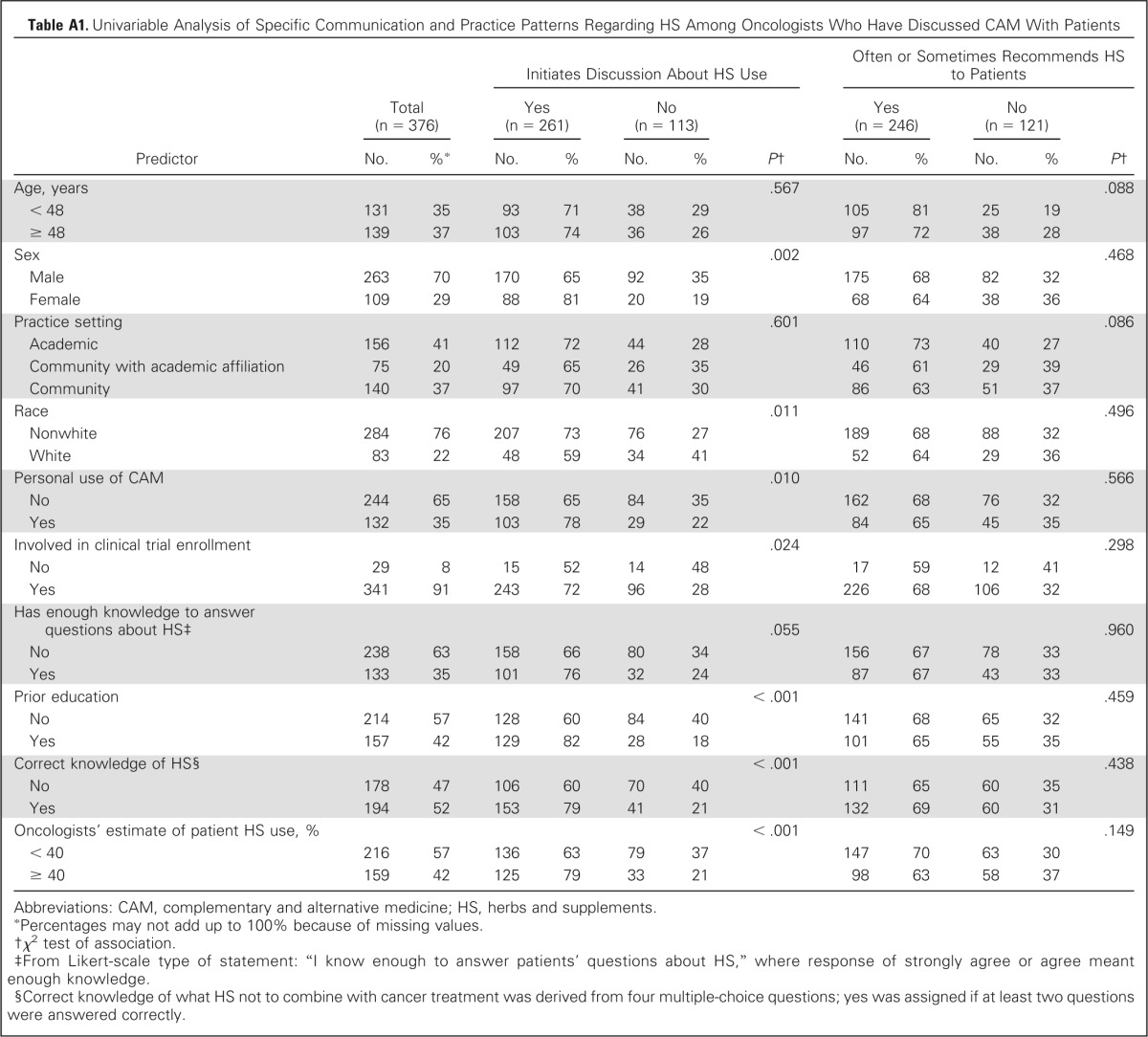
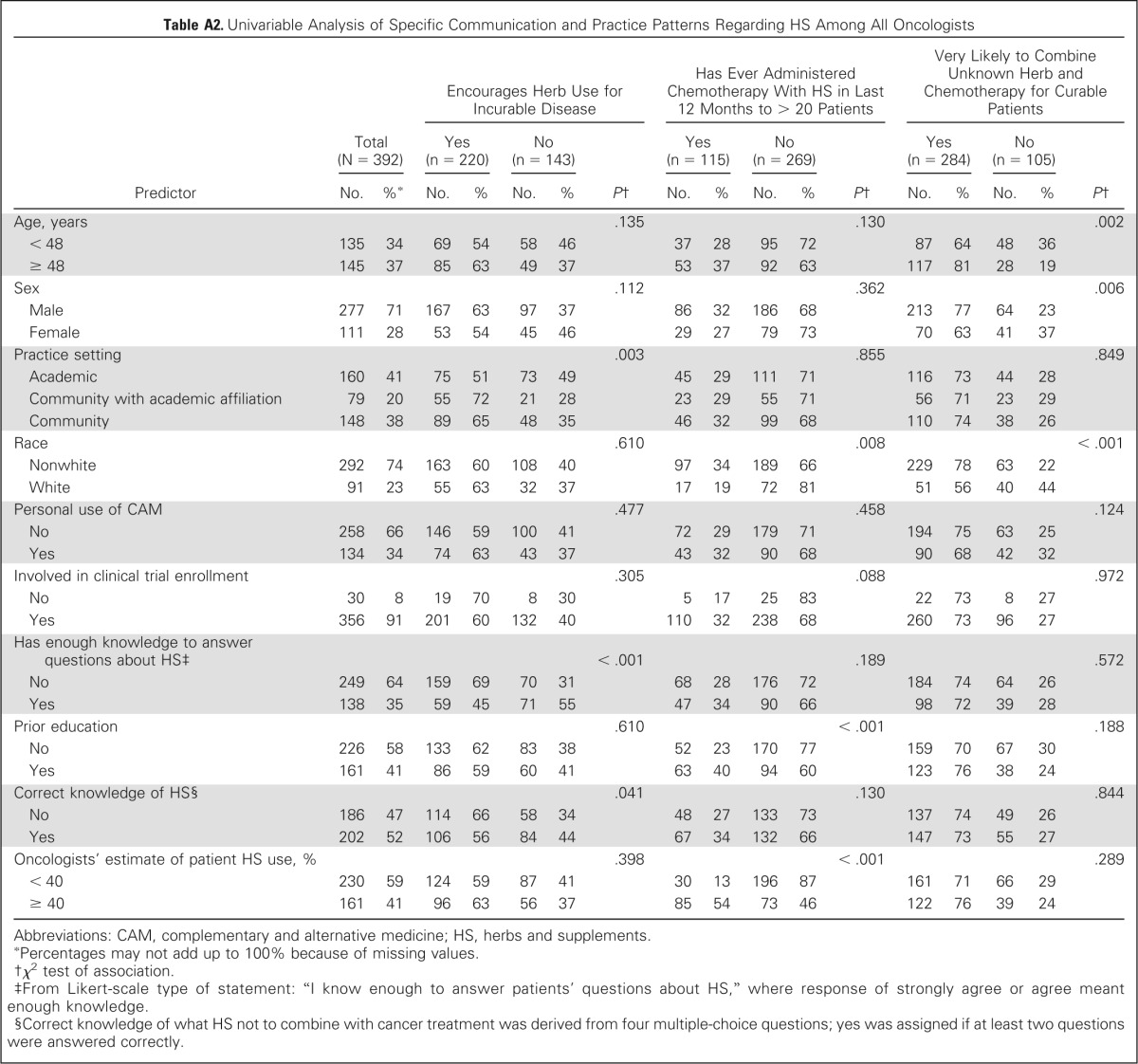
We explored which factors were associated with five specific outcomes: initiating discussion about HS, recommending a CAM therapy, encouraging HS use for incurable cancer, providing chemotherapy concurrently with HS to > 20 patients in the past 12 months, and likely to combine chemotherapy with an unknown herb for treatment of patients with a curable cancer. Female sex (odds ratio [OR], 2.12; 95% CI, 1.06 to 4.24), higher self-reported knowledge (OR, 2.4; 95% CI, 1.2 to 4.9), prior education about HS (OR, 2.5; 95% CI, 1.3 to 4.9), correctly answering ≥ two knowledge questions (OR, 1.84; 95% CI, 1.01 to 3.36), and estimating a higher prevalence of HS use among patients (OR, 1.96; 95% CI, 1.04 to 3.7) were all significantly associated with initiating a discussion about HS. Practicing in a community setting with or without academic affiliation (OR, 2.5; 95% CI, 1.1 to 5.79 and OR, 1.85; 95% CI, 1.00 to 3.43, respectively) and self-reported lack of knowledge about HS (OR, 4.17; 95% CI, 2.27 to 7.69) were associated with encouraging herb use during treatment of an incurable cancer. Older age (OR, 2.14; 95% CI, 1.21 to 3.78), male sex (OR, 1.81; 95% CI, 1.02 to 3.23), and nonwhite race (OR, 2.22; 95% CI, 1.20 to 4.00) were all associated with providing chemotherapy to curable patients taking an unknown herb (Table 4). Results of the univariable analysis are summarized in Appendix Tables A1 and A2 (online only).
Table 4.
Multivariable Analysis of Specific Communication and Practice Patterns Regarding HS
| Predictor | Initiates Discussion About HS Use (n = 265) |
Often or Sometimes Recommends HS to Patients (n = 262) |
Encourages Herb Use for Incurable Disease (n = 257) |
Has Ever Administered Chemotherapy With HS in Last 12 Months to > 20 Patients (n = 275) |
Very Likely to Combine Unknown Herb and Chemotherapy for Curable Patients (n = 278) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR*† | 95% CI | OR*† | 95% CI | OR* | 95% CI | OR* | 95% CI | OR* | 95% CI | |
| Age (≥ 48 v < 48 years) | 0.84 | 0.45 to 1.56 | 0.63 | 0.34 to 1.17 | 1.65 | 0.92 to 2.99 | 0.96 | 0.53 to 1.74 | 2.14 | 1.21 to 3.78 |
| Sex (female v male) | 2.12 | 1.06 to 4.24 | 0.55 | 0.30 to 1.02 | 0.61 | 0.34 to 1.09 | 0.51 | 0.26 to 0.98 | 0.55 | 0.31 to 0.98 |
| Race (white v nonwhite) | 0.63 | 0.31 to 1.28 | 0.83 | 0.41 to 1.69 | 1.26 | 0.66 to 2.42 | 0.54 | 0.25 to 1.15 | 0.45 | 0.25 to 0.83 |
| Practice setting | ||||||||||
| Community with academic affiliation v academic | 2.53 | 1.10 to 5.79 | ||||||||
| Community v academic | 1.85 | 1.00 to 3.43 | ||||||||
| Has enough knowledge to answer questions about CAM (yes v no)‡ | 2.37 | 1.16 to 4.85 | 0.24 | 0.13 to 0.44 | ||||||
| Prior education (yes v no) | 2.54 | 1.32 to 4.89 | 2.27 | 1.26 to 4.08 | ||||||
| Correct knowledge of HS (yes v no)§ | 1.84 | 1.01 to 3.36 | ||||||||
| Oncologists' estimate of patient HS use (≥ 40% v < 40%) | 1.96 | 1.04 to 3.70 | 0.48 | 0.26 to 0.87 | 7.46 | 4.07 to 13.67 | ||||
Abbreviations: CAM, complementary and alternative medicine; HS, herbs and supplements; OR, odds ratio.
Obtained from final logistic regression model selected using stepwise method.
Sample included oncologists who have discussed HS with patients.
From Likert-scale type of statement: “I know enough to answer patients' questions about HS,” where response of strongly agree or agree meant enough knowledge.
Correct knowledge of what HS not to combine with cancer treatment was derived from four multiple-choice questions; yes was assigned if at least two questions were answered correctly.
DISCUSSION
This national survey of US oncologists found that despite a high prevalence of HS use by patients with cancer, fewer than half of oncologists are discussing the topic with their patients. This proportion is lower than that found by Rhodes et al,17 who reported that 77.1% of a sample of primarily gynecologic oncologists routinely asked patients about CAM use. Another study among pediatric oncologists found that 50% asked open-ended questions about CAM use at least half the time and that the frequency of inquiry varied by the CAM modality in question.18 Our lower proportion may reflect the fact that we focused specifically on the topic of HS rather than the broader category of CAM therapies. That being said, our relatively low level of discussion is consistent with other data indicating that ≥ 40% of patients using CAM do not disclose this to their oncologists.19 A recent study of patients finishing radiation therapy found that only 12.1% of all patients surveyed had discussed the topic with their physician.20 Our study also found that only one in four discussions that did take place were initiated by the oncologist, even though most oncologists had administered chemotherapy to at least one patient in the previous 12 months who was concurrently using HS.
Barriers to physician-patient communication about HS exist at multiple levels. One barrier is the fact that according to patient reports, many physicians never ask.5,21,22 We found, as hypothesized, that physicians with less knowledge about HS were less likely to discuss HS with patients. Unfortunately, only one in three oncologists indicated they had enough knowledge to answer questions about HS—a finding similar to reports from studies in other countries.23–26 As we hypothesized, oncologists' estimates about the prevalence of HS use by patients were generally lower than estimates from studies of patients with cancer themselves.3,11,12 This decreased awareness of prevalence of HS use was also associated with a lower likelihood of initiating a discussion with patients about HS use. Educating medical oncologists about the high prevalence of HS use and about commonly used HS may help improve communication patterns.
Discussing HS use with patients could have several benefits. An Australian study of 381 adult patients with cancer found that patients reported higher levels of satisfaction with their clinical visit when they reported discussing HS.22 Our study found that oncologists are much more likely to believe that discussing HS use strengthens physician-patient relationships than they are to believe it weakens those relationships. This is consistent with findings from a study conducted by Richardson et al.5 In addition, studies have found users of CAM more broadly are significantly more likely to be suffering psychosocial distress, report poorer quality of life, have active coping behaviors (eg, information seeking), and prefer patient-centered decision making.27–31 As such, physicians who communicate with patients about the use of HS may thereby gain greater understanding of their patients' experience of illness and strengthen physician-patient relationships.
Several factors were found to be associated with practice patterns regarding HS use with cancer treatment. Participants practicing in the community setting as well as having poor knowledge of HS were more likely to encourage the use of herbs for incurable cancer. This finding could indicate that oncologists in the community may generally be less informed about the topic of HS or that community oncologists are more willing to explore other treatment options for patients with a limited prognosis than those practicing in an academic environment. In contrast, combining chemotherapy with an unknown herb for curable patients was associated with older, nonwhite male oncologists. This practice pattern association is interesting, considering younger female patients tend to use CAM therapies more than their counterparts.32,33 These findings are hypothesis generating and limited, because the study was not designed to explore these specific areas.
Few studies have explored the prevalence of toxicities directly related to HS use during anticancer treatment. A pilot study by Engdal et al34 found that among 136 herb-drug combinations, 47 different potential interactions were identified. However, data on potential interactions were lacking for nearly half of the herbs. In another study of drug interactions among patients with cancer, including over-the-counter medications, found that increasing use of over-the-counter drugs was associated with more identifiable potential drug interactions.35 The clinical impact of the use of HS during anticancer therapy remains unclear, but the potential for harm does exist. For example, a study of antioxidant vitamins during radiation therapy for patients with head and neck cancer found a trend toward increased recurrence of cancer and second primary cancers.36 Because definitive data are lacking about the impact of HS, we encourage medical oncologists to discuss with patients the potential risks and benefits of HS in combination with anticancer treatments. Clinical decisions will need to be personalized and incorporate patient goals of care as well as available data regarding the HS in question.
This study has limitations. We studied only members of ASCO who lived in the United States. The results were not adjusted for multiple comparisons; as such, statistically significant findings about which we did not have prior hypotheses should be considered provisional until confirmed in future studies. Our response rate was typical for physician surveys, but nonresponders may have differed from respondents in ways that bias our results. The initial mailings and e-mails indicated the survey was about the use of HS by patients with cancer, and this topic may have discouraged those with no interest in or negative opinions about the topic. Thus, this sample may overly represent those with more positive opinions about HS. Analysis of the online survey indicated that 5% of those who visited the link answered no questions, and another 1% completed less than half of the survey. This could indicate that a small percentage of nonresponders had limited interest in or knowledge about the topic of HS use by patients with cancer.
Notwithstanding these limitations, this study suggests that US oncologists generally report a lack of knowledge regarding HS and relatively infrequently discuss use of HS with their patients, even when a patient is receiving chemotherapy, and even when a patient's cancer is potentially curable. Given the high prevalence of HS use by patients and the potential for adverse interactions with some cancer treatments, future efforts should seek to improve oncologists' knowledge about HS. Such efforts may lead to more open discussions with patients about this important topic, thereby improving patient care.
Appendix
Table A1.
Univariable Analysis of Specific Communication and Practice Patterns Regarding HS Among Oncologists Who Have Discussed CAM With Patients
| Predictor | Total (n = 376) |
Initiates Discussion About HS Use |
Often or Sometimes Recommends HS to Patients |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes (n = 261) |
No (n = 113) |
P† | Yes (n = 246) |
No (n = 121) |
P† | |||||||
| No. | %* | No. | % | No. | % | No. | % | No. | % | |||
| Age, years | .567 | .088 | ||||||||||
| < 48 | 131 | 35 | 93 | 71 | 38 | 29 | 105 | 81 | 25 | 19 | ||
| ≥ 48 | 139 | 37 | 103 | 74 | 36 | 26 | 97 | 72 | 38 | 28 | ||
| Sex | .002 | .468 | ||||||||||
| Male | 263 | 70 | 170 | 65 | 92 | 35 | 175 | 68 | 82 | 32 | ||
| Female | 109 | 29 | 88 | 81 | 20 | 19 | 68 | 64 | 38 | 36 | ||
| Practice setting | .601 | .086 | ||||||||||
| Academic | 156 | 41 | 112 | 72 | 44 | 28 | 110 | 73 | 40 | 27 | ||
| Community with academic affiliation | 75 | 20 | 49 | 65 | 26 | 35 | 46 | 61 | 29 | 39 | ||
| Community | 140 | 37 | 97 | 70 | 41 | 30 | 86 | 63 | 51 | 37 | ||
| Race | .011 | .496 | ||||||||||
| Nonwhite | 284 | 76 | 207 | 73 | 76 | 27 | 189 | 68 | 88 | 32 | ||
| White | 83 | 22 | 48 | 59 | 34 | 41 | 52 | 64 | 29 | 36 | ||
| Personal use of CAM | .010 | .566 | ||||||||||
| No | 244 | 65 | 158 | 65 | 84 | 35 | 162 | 68 | 76 | 32 | ||
| Yes | 132 | 35 | 103 | 78 | 29 | 22 | 84 | 65 | 45 | 35 | ||
| Involved in clinical trial enrollment | .024 | .298 | ||||||||||
| No | 29 | 8 | 15 | 52 | 14 | 48 | 17 | 59 | 12 | 41 | ||
| Yes | 341 | 91 | 243 | 72 | 96 | 28 | 226 | 68 | 106 | 32 | ||
| Has enough knowledge to answer questions about HS‡ | .055 | .960 | ||||||||||
| No | 238 | 63 | 158 | 66 | 80 | 34 | 156 | 67 | 78 | 33 | ||
| Yes | 133 | 35 | 101 | 76 | 32 | 24 | 87 | 67 | 43 | 33 | ||
| Prior education | < .001 | .459 | ||||||||||
| No | 214 | 57 | 128 | 60 | 84 | 40 | 141 | 68 | 65 | 32 | ||
| Yes | 157 | 42 | 129 | 82 | 28 | 18 | 101 | 65 | 55 | 35 | ||
| Correct knowledge of HS§ | < .001 | .438 | ||||||||||
| No | 178 | 47 | 106 | 60 | 70 | 40 | 111 | 65 | 60 | 35 | ||
| Yes | 194 | 52 | 153 | 79 | 41 | 21 | 132 | 69 | 60 | 31 | ||
| Oncologists' estimate of patient HS use, % | < .001 | .149 | ||||||||||
| < 40 | 216 | 57 | 136 | 63 | 79 | 37 | 147 | 70 | 63 | 30 | ||
| ≥ 40 | 159 | 42 | 125 | 79 | 33 | 21 | 98 | 63 | 58 | 37 | ||
Abbreviations: CAM, complementary and alternative medicine; HS, herbs and supplements.
Percentages may not add up to 100% because of missing values.
χ2 test of association.
From Likert-scale type of statement: “I know enough to answer patients' questions about HS,” where response of strongly agree or agree meant enough knowledge.
Correct knowledge of what HS not to combine with cancer treatment was derived from four multiple-choice questions; yes was assigned if at least two questions were answered correctly.
Table A2.
Univariable Analysis of Specific Communication and Practice Patterns Regarding HS Among All Oncologists
| Predictor | Total (N = 392) |
Encourages Herb Use for Incurable Disease |
Has Ever Administered Chemotherapy With HS in Last 12 Months to > 20 Patients |
Very Likely to Combine Unknown Herb and Chemotherapy for Curable Patients |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes (n = 220) |
No (n = 143) |
P† | Yes (n = 115) |
No (n = 269) |
P† | Yes (n = 284) |
No (n = 105) |
P† | |||||||||
| No. | %* | No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | ||||
| Age, years | .135 | .130 | .002 | ||||||||||||||
| < 48 | 135 | 34 | 69 | 54 | 58 | 46 | 37 | 28 | 95 | 72 | 87 | 64 | 48 | 36 | |||
| ≥ 48 | 145 | 37 | 85 | 63 | 49 | 37 | 53 | 37 | 92 | 63 | 117 | 81 | 28 | 19 | |||
| Sex | .112 | .362 | .006 | ||||||||||||||
| Male | 277 | 71 | 167 | 63 | 97 | 37 | 86 | 32 | 186 | 68 | 213 | 77 | 64 | 23 | |||
| Female | 111 | 28 | 53 | 54 | 45 | 46 | 29 | 27 | 79 | 73 | 70 | 63 | 41 | 37 | |||
| Practice setting | .003 | .855 | .849 | ||||||||||||||
| Academic | 160 | 41 | 75 | 51 | 73 | 49 | 45 | 29 | 111 | 71 | 116 | 73 | 44 | 28 | |||
| Community with academic affiliation | 79 | 20 | 55 | 72 | 21 | 28 | 23 | 29 | 55 | 71 | 56 | 71 | 23 | 29 | |||
| Community | 148 | 38 | 89 | 65 | 48 | 35 | 46 | 32 | 99 | 68 | 110 | 74 | 38 | 26 | |||
| Race | .610 | .008 | < .001 | ||||||||||||||
| Nonwhite | 292 | 74 | 163 | 60 | 108 | 40 | 97 | 34 | 189 | 66 | 229 | 78 | 63 | 22 | |||
| White | 91 | 23 | 55 | 63 | 32 | 37 | 17 | 19 | 72 | 81 | 51 | 56 | 40 | 44 | |||
| Personal use of CAM | .477 | .458 | .124 | ||||||||||||||
| No | 258 | 66 | 146 | 59 | 100 | 41 | 72 | 29 | 179 | 71 | 194 | 75 | 63 | 25 | |||
| Yes | 134 | 34 | 74 | 63 | 43 | 37 | 43 | 32 | 90 | 68 | 90 | 68 | 42 | 32 | |||
| Involved in clinical trial enrollment | .305 | .088 | .972 | ||||||||||||||
| No | 30 | 8 | 19 | 70 | 8 | 30 | 5 | 17 | 25 | 83 | 22 | 73 | 8 | 27 | |||
| Yes | 356 | 91 | 201 | 60 | 132 | 40 | 110 | 32 | 238 | 68 | 260 | 73 | 96 | 27 | |||
| Has enough knowledge to answer questions about HS‡ | < .001 | .189 | .572 | ||||||||||||||
| No | 249 | 64 | 159 | 69 | 70 | 31 | 68 | 28 | 176 | 72 | 184 | 74 | 64 | 26 | |||
| Yes | 138 | 35 | 59 | 45 | 71 | 55 | 47 | 34 | 90 | 66 | 98 | 72 | 39 | 28 | |||
| Prior education | .610 | < .001 | .188 | ||||||||||||||
| No | 226 | 58 | 133 | 62 | 83 | 38 | 52 | 23 | 170 | 77 | 159 | 70 | 67 | 30 | |||
| Yes | 161 | 41 | 86 | 59 | 60 | 41 | 63 | 40 | 94 | 60 | 123 | 76 | 38 | 24 | |||
| Correct knowledge of HS§ | .041 | .130 | .844 | ||||||||||||||
| No | 186 | 47 | 114 | 66 | 58 | 34 | 48 | 27 | 133 | 73 | 137 | 74 | 49 | 26 | |||
| Yes | 202 | 52 | 106 | 56 | 84 | 44 | 67 | 34 | 132 | 66 | 147 | 73 | 55 | 27 | |||
| Oncologists' estimate of patient HS use, % | .398 | < .001 | .289 | ||||||||||||||
| < 40 | 230 | 59 | 124 | 59 | 87 | 41 | 30 | 13 | 196 | 87 | 161 | 71 | 66 | 29 | |||
| ≥ 40 | 161 | 41 | 96 | 63 | 56 | 37 | 85 | 54 | 73 | 46 | 122 | 76 | 39 | 24 | |||
Abbreviations: CAM, complementary and alternative medicine; HS, herbs and supplements.
Percentages may not add up to 100% because of missing values.
χ2 test of association.
From Likert-scale type of statement: “I know enough to answer patients' questions about HS,” where response of strongly agree or agree meant enough knowledge.
Correct knowledge of what HS not to combine with cancer treatment was derived from four multiple-choice questions; yes was assigned if at least two questions were answered correctly.
Footnotes
Supported by an American Society of Clinical Oncology Cancer Foundation Young Investigator Award (R.T.L.) and by Grant No. T32 CA009566 from the National Cancer Institute.
Presented at the 46th Annual Meeting of the American Society of Clinical Oncology, Chicago, IL, June 4-8, 2010, and the Seventh Annual International Conference of the Society for Integrative Oncology, New York, NY, November 11-13, 2010.
Authors' disclosures of potential conflicts of interest are found in the article online at www.jco.org. Author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Disclosures provided by the authors are available with this article at www.jco.org.
AUTHOR CONTRIBUTIONS
Conception and design: Richard T. Lee, Olufunmilayo I. Olopade, Farr A. Curlin
Administrative support: Olufunmilayo I. Olopade
Collection and assembly of data: Richard T. Lee, Farr A. Curlin
Data analysis and interpretation: Richard T. Lee, Andrea Barbo, Gabriel Lopez, Amal Melhem-Bertrandt, Heather Lin, Farr A. Curlin
Manuscript writing: All authors
Final approval of manuscript: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
National Survey of US Oncologists' Knowledge, Attitudes, and Practice Patterns Regarding Herb and Supplement Use by Patients With Cancer
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or jco.ascopubs.org/site/ifc.
Richard T. Lee
No relationship to disclose
Andrea Barbo
No relationship to disclose
Gabriel Lopez
No relationship to disclose
Amal Melhem-Bertrandt
No relationship to disclose
Heather Lin
No relationship to disclose
Olufunmilayo I. Olopade
No relationship to disclose
Farr A. Curlin
No relationship to disclose
REFERENCES
- 1.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;12:1–23. [PubMed] [Google Scholar]
- 2.Dy GK, Bekele L, Hanson LJ, et al. Complementary and alternative medicine use by patients enrolled onto phase I clinical trials. J Clin Oncol. 2004;22:4810–4815. doi: 10.1200/JCO.2004.03.121. [DOI] [PubMed] [Google Scholar]
- 3.Richardson MA, Sanders T, Palmer JL, et al. Complementary/alternative medicine use in a comprehensive cancer center and the implications for oncology. J Clin Oncol. 2000;18:2505–2514. doi: 10.1200/JCO.2000.18.13.2505. [DOI] [PubMed] [Google Scholar]
- 4.Bishop FL, Prescott P, Chan YK, et al. Prevalence of complementary medicine use in pediatric cancer: A systematic review. Pediatrics. 2010;125:768–776. doi: 10.1542/peds.2009-1775. [DOI] [PubMed] [Google Scholar]
- 5.Richardson MA, Mâsse LC, Nanny K, et al. Discrepant views of oncologists and cancer patients on complementary/alternative medicine. Support Care Cancer. 2004;12:797–804. doi: 10.1007/s00520-004-0677-3. [DOI] [PubMed] [Google Scholar]
- 6.Lee RT, Hlubocky FJ, Hu JJ, et al. An international pilot study of oncology physicians' opinions and practices on complementary and alternative medicine (CAM) Integr Cancer Ther. 2008;7:70–75. doi: 10.1177/1534735408319059. [DOI] [PubMed] [Google Scholar]
- 7.Sparreboom A, Cox MC, Acharya MR, et al. Herbal remedies in the United States: Potential adverse interactions with anticancer agents. J Clin Oncol. 2004;22:2489–2503. doi: 10.1200/JCO.2004.08.182. [DOI] [PubMed] [Google Scholar]
- 8.Frye RF, Fitzgerald SM, Lagattuta TF, et al. Effect of St John's wort on imatinib mesylate pharmacokinetics. Clin Pharmacol Ther. 2004;76:323–329. doi: 10.1016/j.clpt.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 9.Golden EB, Lam PY, Kardosh A, et al. Green tea polyphenols block the anticancer effects of bortezomib and other boronic acid-based proteasome inhibitors. Blood. 2009;113:5927–5937. doi: 10.1182/blood-2008-07-171389. [DOI] [PubMed] [Google Scholar]
- 10.Mazzanti G, Menniti-Ippolito F, Moro PA, et al. Hepatotoxicity from green tea: A review of the literature and two unpublished cases. Eur J Clin Pharmacol. 2009;65:331–341. doi: 10.1007/s00228-008-0610-7. [DOI] [PubMed] [Google Scholar]
- 11.McCune JS, Hatfield AJ, Blackburn AA, et al. Potential of chemotherapy-herb interactions in adult cancer patients. Support Care Cancer. 2004;12:454–462. doi: 10.1007/s00520-004-0598-1. [DOI] [PubMed] [Google Scholar]
- 12.Andersen MR, Sweet E, Lowe KA, et al. Dangerous combinations: Ingestible CAM supplement use during chemotherapy in patients with ovarian cancer. J Altern Complement Med. 2013;19:714–720. doi: 10.1089/acm.2012.0295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McCaffrey AM, Pugh GF, O'Connor BB. Understanding patient preference for integrative medical care: Results from patient focus groups. J Gen Intern Med. 2007;22:1500–1505. doi: 10.1007/s11606-007-0302-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Siegel S, Castellan NJ. Nonparametric Statistics for the Behavioral Sciences (ed 2) New York, NY: McGraw-Hill; 1988. [Google Scholar]
- 15.Woolson RF, Clarke WR. Statistical Methods for the Analysis of Biomedical Data (ed 2) New York, NY: Wiley-Interscience; 2002. [Google Scholar]
- 16.Hosmer DW, Lemeshow S. Applied Logistic Regression (ed 2) New York, NY: Wiley; 2000. [Google Scholar]
- 17.Rhode JM, Patel DA, Sen A, et al. Perception and use of complementary and alternative medicine among gynecologic oncology care providers. Int J Gynaecol Obstet. 2008;103:111–115. doi: 10.1016/j.ijgo.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 18.Roth M, Lin J, Kim M, et al. Pediatric oncologists' views toward the use of complementary and alternative medicine in children with cancer. J Pediatr Hematol Oncol. 2009;31:177–182. doi: 10.1097/MPH.0b013e3181984f5a. [DOI] [PubMed] [Google Scholar]
- 19.Richardson MA, Straus SE. Complementary and alternative medicine: Opportunities and challenges for cancer management and research. Semin Oncol. 2002;29:531–545. doi: 10.1053/sonc.2002.50002. [DOI] [PubMed] [Google Scholar]
- 20.Ge J, Fishman J, Vapiwala N, et al. Patient-physician communication about complementary and alternative medicine in a radiation oncology setting. Int J Radiat Oncol Biol Phys. 2013;85:e1–e6. doi: 10.1016/j.ijrobp.2012.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim do Y, Kim BS, Lee KH, et al. Discrepant views of Korean medical oncologists and cancer patients on complementary and alternative medicine. Cancer Res Treat. 2008;40:87–92. doi: 10.4143/crt.2008.40.2.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oh B, Butow P, Mullan B, et al. Patient-doctor communication: Use of complementary and alternative medicine by adult patients with cancer. J Soc Integr Oncol. 2010;8:56–64. [PubMed] [Google Scholar]
- 23.Chang KH, Brodie R, Choong MA, et al. Complementary and alternative medicine use in oncology: A questionnaire survey of patients and health care professionals. BMC Cancer. 2011;11:196. doi: 10.1186/1471-2407-11-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Crocetti E, Crotti N, Montella M, et al. Complementary medicine and oncologists' attitudes: A survey in Italy. Tumori. 1996;82:539–542. doi: 10.1177/030089169608200605. [DOI] [PubMed] [Google Scholar]
- 25.Hyodo I, Eguchi K, Nishina T, et al. Perceptions and attitudes of clinical oncologists on complementary and alternative medicine: A nationwide survey in Japan. Cancer. 2003;97:2861–2868. doi: 10.1002/cncr.11402. [DOI] [PubMed] [Google Scholar]
- 26.Al-Omari A, Al-Qudimat M, Abu Hmaidan A, et al. Perception and attitude of Jordanian physicians towards complementary and alternative medicine (CAM) use in oncology. Complement Ther Clin Pract. 2013;19:70–76. doi: 10.1016/j.ctcp.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 27.Boon H, Stewart M, Kennard MA, et al. Use of complementary/alternative medicine by breast cancer survivors in Ontario: Prevalence and perceptions. J Clin Oncol. 2000;18:2515–2521. doi: 10.1200/JCO.2000.18.13.2515. [DOI] [PubMed] [Google Scholar]
- 28.Swenson SL, Buell S, Zettler P, et al. Patient-centered communication: Do patients really prefer it? J Gen Intern Med. 2004;19:1069–1079. doi: 10.1111/j.1525-1497.2004.30384.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Söllner W, Zingg-Schir M, Rumpold G, et al. Attitude toward alternative therapy, compliance with standard treatment, and need for emotional support in patients with melanoma. Arch Dermatol. 1997;133:316–321. doi: 10.1001/archderm.1997.03890390054007. [DOI] [PubMed] [Google Scholar]
- 30.Burstein HJ, Gelber S, Guadagnoli E, et al. Use of alternative medicine by women with early-stage breast cancer. N Engl J Med. 1999;340:1733–1739. doi: 10.1056/NEJM199906033402206. [DOI] [PubMed] [Google Scholar]
- 31.Söllner W, Maislinger S, DeVries A, et al. Use of complementary and alternative medicine by cancer patients is not associated with perceived distress or poor compliance with standard treatment but with active coping behavior: A survey. Cancer. 2000;89:873–880. doi: 10.1002/1097-0142(20000815)89:4<873::aid-cncr21>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 32.Paltiel O, Avitzour M, Peretz T, et al. Determinants of the use of complementary therapies by patients with cancer. J Clin Oncol. 2001;19:2439–2448. doi: 10.1200/JCO.2001.19.9.2439. [DOI] [PubMed] [Google Scholar]
- 33.Shumay DM, Maskarinec G, Gotay CC, et al. Determinants of the degree of complementary and alternative medicine use among patients with cancer. J Altern Complement Med. 2002;8:661–671. doi: 10.1089/107555302320825183. [DOI] [PubMed] [Google Scholar]
- 34.Engdal S, Klepp O, Nilsen OG. Identification and exploration of herb-drug combinations used by cancer patients. Integr Cancer Ther. 2009;8:29–36. doi: 10.1177/1534735408330202. [DOI] [PubMed] [Google Scholar]
- 35.van Leeuwen RW, Swart EL, Boven E, et al. Potential drug interactions in cancer therapy: A prevalence study using an advanced screening method. Ann Oncol. 2011;22:2334–2341. doi: 10.1093/annonc/mdq761. [DOI] [PubMed] [Google Scholar]
- 36.Bairati I, Meyer F, Gélinas M, et al. A randomized trial of antioxidant vitamins to prevent second primary cancers in head and neck cancer patients. J Natl Cancer Inst. 2005;97:481–488. doi: 10.1093/jnci/dji095. [DOI] [PubMed] [Google Scholar]