Abstract
Structural equation modeling was used to examine the effects of cultural factors (ethnic identity, perceived discrimination), family relations, and child problem type on mental health service utilization in a community sample of 1,480 adolescent girls (860 African American, 620 European American) between ages 15 and 17 years enrolled in the Pittsburgh Girls Study. Results revealed ethnic identity, caregiver attachment, and conduct disorder were related to service use among African American girls. Among European American girls, correlate patterns differed by clinical need. Findings highlight the need for research on health disparities to examine racially specific influences on service utilization.
Keywords: Service utilization, Ethnic identity, Perceived discrimination, Problem type, Ethnic minority youth
Introduction
Although evidence shows a high prevalence of emotional and behavioral problems among children and youth in the United States (Brauner and Stephens 2006), only a portion of children and adolescents with clinically significant emotional or behavioral problems receive mental health care (Kataoka et al. 2002). Failure to participate in treatment may have long-term sequelae—children exhibiting emotional and behavioral problems earlier in development are more likely to evidence problematic behaviors later in life, such as engagement with deviant peers, involvement with violent crime, school dropout, drug and alcohol abuse, practicing unsafe sex, and unemployment (Lochman and Salekin 2003; Moffitt et al. 2002). The poor prognosis of children with untreated emotional and behavioral problems posits an even more serious concern among ethnic minority families that often face challenges associated with minority status, including discrimination, poverty, and acculturation (Nyborg and Curry 2003; Wong et al. 2003).
Research indicates that African American children and their families are less engaged in mental health services (Garland et al. 2005; Miller et al. 2008) and attend fewer treatment sessions (Harpaz-Rotem et al. 2004) than European American children do. Ethnic and racial differences in service utilization persist across gender (e.g., Herz 2001) and after controlling for other factors including socioeconomic status (SES), mental health needs, maltreatment exposure, parent mental health, and social support (Leslie et al. 2005; Coker et al. 2009). Further, African American youth are more likely than European American youth to be triaged to social welfare or juvenile justice systems for psychological problems instead of receiving appropriate services in mental health care (Chabra et al. 1999).
These studies highlight how urgent it is to examine factors that contribute to racial health disparities in mental health service use among ethnic minority youth. We attempted to untangle individual, cultural, and contextual factors that affect African American and European American girls’ engagement in mental health services. We examined how service use is influenced by the type of presenting problem, ethnic identity, perceived discrimination, and family relationships.
Presenting Problems and Service Use
The severity and type of presenting problem are predictors of service utilization (Garland et al. 1996; Leslie et al. 2000), and recent evidence suggests that these effects vary by race or ethnicity. For example, Martinez et al. (2013) found that the presenting problem type (internalizing, externalizing) predicted specialty services use for European American youth but did not for Latinos, and only externalizing problems predicted service use among African Americans. Gudiño et al. (2009) reported that African American youth were overall less likely to receive mental health services than European American youth were, but among those exhibiting greater externalizing behavior problems, African American and European American youth received services at similar rates. In contrast, or internalizing problems, European American youth used services at higher rates compared with African American and Latino youth. This pattern of less service utilization for depression and anxiety among racial minorities is reported in other studies (Cummings and Druss 2011; Merikangas et al. 2011).
Ethnocultural Influences on Service Use
Despite the long-standing evidence of racial disparities in service use, limited research has examined how ethnocultural factors influence service use among ethnic minority youth. Ethnic minority youth often experience discrimination, which is associated with behavior problems (Wong et al. 2003) and internalizing problems (Simons et al. 2002). Few researchers, however, have examined the direct effect of perceived discrimination on help-seeking behaviors, including service utilization. A handful of studies indicate that perceived discrimination is related to less service utilization across races (Casagrande et al. 2007; Lamkaddem et al. 2011).
In contrast to discrimination, evidence shows that ethnic identity, defined as an aspect of an individual’s self-conception derived from his or her knowledge of membership in a social group, together with the value and emotional significance attached to that membership (Phinney 1992), has a protective effect from poor psychological adjustment among racial minority youth (Yasui et al. 2004). However, results from studies examining the association between ethnic identity and help-seeking have been mixed. Longshore (1999) examined help-seeking behaviors among adult African American substance users and found that although ethnic identity had no main effect on help-seeking, an interaction effect was found in which individuals reporting higher ethnic identity and higher problem recognition engaged in more help-seeking behaviors. Chen et al. (2013) reported that higher ethnic identity predicted lower levels of stigma in seeking psychological help among African American adults. In contrast, Richman et al. (2007) found an opposite effect of racial identity: African American adults with stronger racial identities were less likely to use mental health services than were those with weaker racial identities, and these effects differed with levels of perceived discrimination.
Family Factors and Service Use
An important yet understudied correlate of mental health service use is family factors. In the general population, poorer family functioning (Verhulst and van der Ende 1997), family conflict (Horwitz et al. 2003), and attachment to caregiver (Bauman et al. 2001) predict increased service utilization.
Findings on the influence of family on service utilization among minorities have been mixed. For example, Chang et al. (2013) found that family cultural conflict predicted mental health service use among Asian and Latinos, whereas high family cohesion was related to underuse among Latinos even after adjusting for the effects of lifetime mental health disorder, perceived mental health need, immigration status, and participant demographics. Gorman-Smith et al. (2002) found no effect of family relationships on participation in a family-focused prevention intervention among African American and Latino first graders and their families. In contrast, Perrino et al. (2001) found that higher family organization, communication, and cohesion independently predicted initial intervention engagement among African American and Latino families.
Present Study
We tested the collective effects of the presenting problem type (i.e., symptom severity, diagnosis of conduct disorder [CD], major depressive disorder [MDD]) and ethnocultural (i.e., ethnic identity, perceived discrimination) and family factors (i.e., caregiver attachment) on service utilization among African American and European American girls. The aforementioned studies have examined the independent effects of these dimensions on service use among ethnic minorities; however, no single study has tested and compared the unique and combined influence of these factors on service utilization among racial groups.
We proposed that for African American girls, increased symptoms and diagnoses of CD but not MDD would be associated with more service utilization, and higher levels of ethnic identity and perceived discrimination would be associated with less service utilization. For European American girls, we hypothesized that increased symptoms and diagnoses of CD and MDD would be associated with more service utilization. Because empirical evidence is lacking on the centrality of ethnic identity for European American girls, we had no hypotheses concerning the relationship between ethnic identity and perceived discrimination with service utilization. We hypothesized that stronger caregiver attachment was directly related to less service utilization among all girls. Finally, we explored the indirect effects of these independent variables on service utilization. All analyses were controlled for socioeconomic disadvantage.
Methods
Sample Description
Data for the current study were drawn from the Pittsburgh Girls Study (PGS), a community-wide longitudinal study examining the development of behavioral problems, internalizing problems, and substance use among 2,450 adolescent girls. The PGS sample was identified from 103,238 city households in 1999. All households in the poorest one-third of the city neighborhoods and 50 % of the households in the remaining neighborhoods were sampled (for more details, see Hipwell et al. 2002; Keenan et al. 2010). We used child and parent data from the 11th annual assessment (during years 2011–2012) from three PGS sample cohorts (5, 6, and 7) consisting of 1,480 adolescent girls (860 African American, 620 European American) between ages 15 and 17 years (M = 16.01). This allowed us to focus on service use during adolescence with data from both the adolescent and the caregiver. The three cohorts included girls ages 5, 6, and 7 years at the first PGS assessment. The 1,480 girls represented 60.4 % of the original sample (N = 2,450). Data from Cohort 8 were excluded because there were no instances of parent-reported service use (n = 622). Data from girls who were not African American or European American were also excluded (n = 113). In addition, girls with missing data on one or more of the measures used in the present study were excluded (n = 235). We found no significant correlations in the cases with missing data, suggesting an absence of patterns of missing data that would affect the analyses.
Procedure
Informed consent from the caregivers and verbal assent from the adolescent girls were obtained prior to data collection. In-home interviews were conducted separately for the adolescent girls and caretakers by trained interviewers using a laptop computer. All study procedures were approved by the University of Pittsburgh Institutional Review Board. All families were financially reimbursed for their participation.
Measures
Mental Health Service Utilization
We used the Health Questionnaire to assess girls’ mental health service utilization. The questionnaire, developed for the PGS, assesses help-seeking behaviors and service use for mental health and physical health problems as reported by the parent. We derived mental health service use from binary scores on service use from three items asking whether the adolescent (1) sought help from a mental health professional (psychiatrist, psychologist, therapist, social worker, or counselor); (2) sought help from a community service (counseling service, social service agency, family doctor, pediatrician, community program, crisis center, or hotline); or (3) was admitted to a hospital or inpatient clinic for emotional or behavioral problems in the past year. For all three items, only participants’ service use was coded (1 for any use of services, 0 for no service use), not the specific service type (i.e., for mental health professional, specific provider types used were not recorded). Participants’ responses to each of these items were not mutually exclusive, so it was impossible to determine whether participants responded to more than one item based on a service they sought (e.g., sought help from a counselor [Item 1] in a community counseling service [Item 2]). Therefore, we decided to code for overall mental health service use (1 = use of any of the services; 0 = no service use).
Ethnic Identity (Affirmation and Belonging)
The Multigroup Ethnic Identity Measure (MEIM; Phinney 1992) is a 14-item measure assessing an individual’s affirmation of and belonging to an ethnic group and his or her identification with an ethnic group (i.e., ethnic identity) on the basis of exploration and commitment. We used the affirmation and belonging subscale, which assesses the youth’s sense of belonging and membership to an ethnic group. Items were rated on a 4-point scale ranging from 1 (strongly disagree) to 4 (strongly agree). Higher scores indicated a higher degree of affirmation to one’s ethnic group. Internal consistency was .94 for all girls (.95 for European American girls, .94 for African American girls).
Daily Experiences of Discrimination
We assessed experience of discrimination using a 9-item scale of global perceptions of everyday unfair treatment by youth report (Williams et al. 1997). Responses were recorded using a 5-point Likert scale ranging from 1 (never) to 5 (very often). For the current study, we used the mean, with a higher score indicating more experiences of discrimination. Internal consistency was .84 for both European American and African American girls.
Conduct Disorder and Depression
Child reports on the Child Symptom Inventory-fourth edition (CSI-4; Gadow and Sprafkin, 1994/1997) were used to assess symptom severity and CD and MDD diagnoses. For CD, 13 DSM-IV CD symptoms were scored on 4-point scales ranging from 0 (never) to 3 (very often). For MDD, seven symptoms of major depression were assessed on a 4-point scale and five symptoms as present or absent. For the current analyses, we used continuous severity scores because they provided the greatest variability. The CD subscale of the CSI has good sensitivity and specificity in distinguishing youth with clinical diagnoses from healthy controls (Gadow and Sprafkin, 1994/1997). Internal consistency for the current sample was .80 for CD and .84 for MDD.
Past-year CD diagnosis consisted of endorsing three or more CD symptoms. Past-year MDD diagnosis included five or more of the nine DSM-IV MDD symptoms, of which one was depressed mood or anhedonia. Presence or absence of a CD or MDD diagnosis was coded using a binary scale (1 = positive diagnosis; 0 = negative diagnosis).
Caregiver Attachment
Quality of attachment to the caregiver was assessed using the trust subscale of the Revised Inventory of Parent and Peer Attachment (IPPA-R), which assesses adolescent trust and the quality of the relationship the caregiver (Gullone and Robinson 2005). For this study, nine items assessing parent trust were rated using a 5-point scale. Higher scores indicated stronger caregiver attachment. Internal consistency was .92 (.93 for European American girls, .92 for African American girls).
Socioeconomic Disadvantage
To control for the effect of low income on service use, we used a single item indicating household receipt of public assistance (1 = received; 0 = not received).
Analysis Plan
Descriptive analyses, odds ratio (OR), and 95 % confidence interval (CI) were calculated for psychological outcomes, cultural factors, caregiver attachment, and service use.
We used structural equation modeling to test relationships among the hypothesized correlates and service use among 1,480 African American and European American girls. We conducted multigroup path analysis to examine the moderating effects of race. To examine whether interrelations differed by girls’ level of clinical need, we first ran the multigroup path analysis using continuous clinical severity scores of CD and MDD. We then reran it using CD and MDD diagnostic scores. The rationale for conducting the multigroup models separately with clinical severity and diagnostic scores was the variability in range of clinical symptoms, particularly those below the diagnostic threshold reported by our community sample. To test for partial measurement invariance across groups, we compared (1) the Chi square value generated from a model in which all parameters were allowed to be unequal across groups with (2) the Chi square value generated from a model in which the parameters were constrained to be equal across groups. No means or intercepts were estimated in these models. Predictors were centered at the mean for each ethnic group (Cohen et al. 2003). All path analyses were estimated using Mplus software (Muthén and Muthén 2011), with weighted least square mean and variance (WLSMV) adjusted Chi square estimation. The WLSMV is the optimal method because it does not assume normally distributed variables, thereby providing the best approach for categorical or non-normal item responses or unbalanced data, which was appropriate given our unbalanced data on service use and clinical diagnoses (Brown 2006; Flora and Curran 2004). The comparative fit between the two models was estimated using standard weighted least square (WLS) estimation and associated Chi square difference tests (Muthén and Asparouhov 2002). All models estimated direct and indirect paths, and we analyzed the significance of the indirect paths using the indirect effect test in Mplus.
Results
Descriptive Statistics
Descriptive statistics of youth psychological outcomes, cultural factors, caregiver attachment, and service use are presented in Table 1. We tested race differences with socioeconomic disadvantage as a covariate. Univariate tests revealed no differences in service utilization and in reports of perceived discrimination among racial groups; however, African American girls reported higher ethnic identity compared with European American girls, F(21,473) = 30.22, p < .01. No group differences were found for MDD severity. However, CD severity was higher for African American girls, F (21,476) = 9.81, p < .01. Logistic regressions revealed no race differences in the presence of CD diagnosis, B = −.38, Wald = 2.46, p = .12, and MDD diagnosis, B = −.37, Wald = 1.55, p = .22. Caregiver attachment was significantly stronger among European American girls, F(2, 1474) = 4.80, p < .01. Public assistance use was significantly higher for African American girls, B = −1.52, Wald = 163.24, p<. 05.
Table 1.
Descriptives and odds ratio
| European American | African American | Race differences | Odds ratio of service utilization | 95 % CI | |||
|---|---|---|---|---|---|---|---|
| Service utilization | Yes | 142 (9.6 %) | 171 (11.5 %) | n.s.a | |||
| No | 478 (32.3 %) | 689 (46.6 %) | |||||
| Ethnic identity | 3.29 (.56) | 3.43 (.51) | AA > EAa | .65 | p < .001 | .51–.82 | |
| Discrimination | 13.07 (3.85) | 13.02 (4.15) | n.s.a | 1.12 | p < .001 | 1.09–1.15 | |
| Caregiver attachment | 24.17 (3.57) | 23.63 (3.80) | EA > AAa | .89 | p < .001 | .86–.92 | |
| CD severity | 3.07 (1.68) | 3.45 (2.11) | AA > EAa | 1.22 | p < .001 | 1.15–1.30 | |
| MDD severity | 6.64 (4.71) | 6.93 (5.05) | n.s.a | 1.10 | p < .001 | 1.07–1.12 | |
| CD diagnosis | Yes | 29 (1.9 %) | 65 (4.4 %) | n.s.a | 3.18 | p < .001 | 2.07–4.88 |
| No | 591 (40.0 %) | 794 (53.7 %) | |||||
| MDD diagnosis | Yes | 39 (2.6 %) | 46 (3.1 %) | n.s.a | 2.98 | p < .001 | 1.90–4.68 |
| No | 580 (39.3 %) | 812 (55.0 %) | |||||
| Race | .77 | n.s. | |||||
| Public assistance | Yes | 135 (9.1 %) | 482 (32.6 %) | AA>EA | 1.15 | n.s. | |
| No | 485 (32.8 %) | 378 (25.5 %) | |||||
Controlled for public assistance
To examine the extent to which each factor increased or decreased the probability of mental health service use among adolescent girls, OR and 95 % CI were calculated using logistic regressions (Table 1). ORs provide information on the occurrence of the outcome (i.e., service utilization) given exposure to the variable of interest. All variables except for adolescent race and socioeconomic disadvantage indicated a statistically significant increase or decrease in odds of service utilization.
Testing the Group Models
A series of multigroup path analyses was conducted in which all paths were allowed to vary freely between groups, using WLSMV-adjusted Chi square (Muthén and Asparouhov 2002). To examine whether correlates of service utilization differed by clinical symptom levels, two multigroup path models were run: the first using continuous CD and MDD severity scores and second using CD and MDD diagnostic scores.
Model with Severity Scores
The multigroup path analysis model in which all paths were allowed to vary freely using WLSMV-adjusted Chi square fit the data well, χ2 (12) = 36.70, p < .05, CFI = .98, TLI = .94, RMSEA = .053, WRMR = 1.14. The partial invariance model with loadings constrained to be equal across groups using WLSMV estimation fit significantly worse, χ2 (30) = 146.47, p < .001, CFI = .922, TLI = .89, RMSEA = .07, WRMR = 2.30.
To perform Chi square difference tests, the models were re-estimated using the WLS estimator, because WLSMV-adjusted Chi square cannot be compared across models (Muthén and Asparouhov 2002). The WLS-generated model fit for the model in which paths were allowed to vary freely was χ2 (12) = 30.63, p = < .05, CFI = .98, TLI = .94, RMSEA = .05, compared with the alternate model (equal constraints across groups), χ2 (30) = 117.40, p < .001, CFI = .91, TLI = .88, RMSEA = .07. The resulting difference in fit, Δχ2 (18) = 86.77, p < .001, suggested that the two models were significantly different, with the model in which paths were allowed to vary providing the better fit to the sample data.
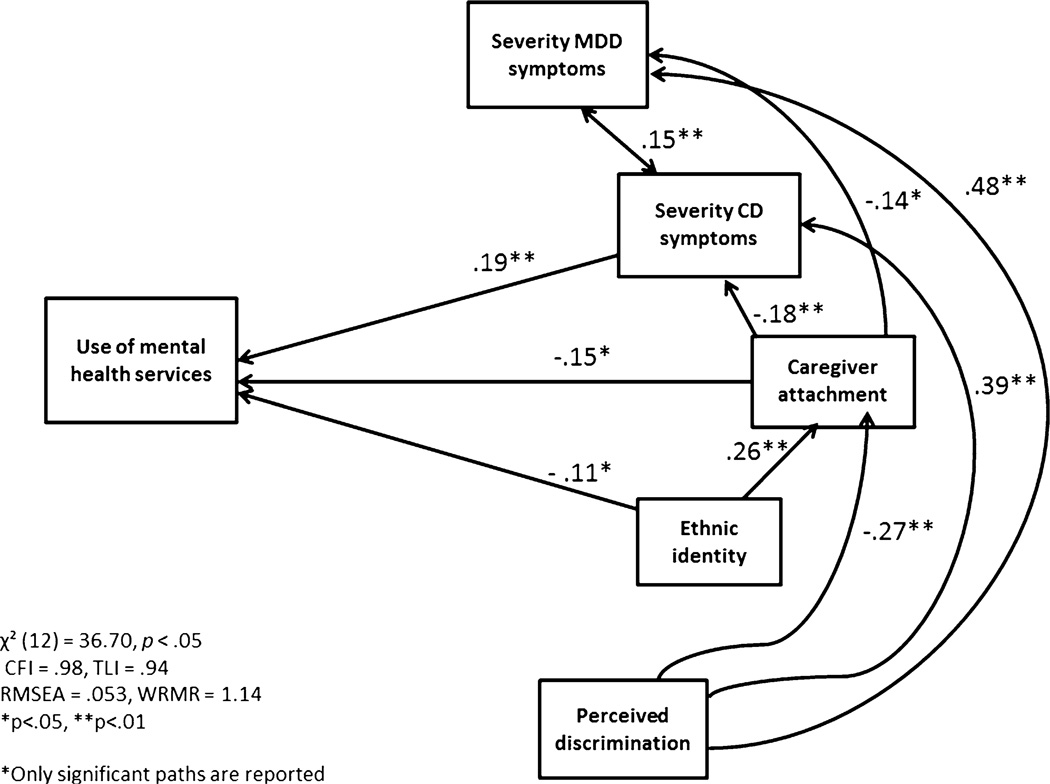
The model for African American girls is presented in Fig. 1. As we hypothesized, CD severity was negatively associated with mental health service use, whereas ethnic identity and caregiver attachment were positively related to mental health service use. Perceived discrimination was unrelated to service utilization but negatively related to caregiver attachment, and positively related to CD and MDD severity. Caregiver attachment was negatively related to CD and MDD severity and positively related to ethnic identity. As we expected, MDD severity was unrelated to service utilization. CD and MDD severity were positively related. Examination of indirect effects showed an effect of ethnic identity, via caregiver attachment, on service utilization (β = −.04, p < .05). In addition, indirect effects of perceived discrimination (β = .07, p < .05) and caregiver attachment (β = .04, p < .05), via CD severity, on service utilization were found.
Fig. 1.
Path model for African American girls (with clinical severity scores). Fit indices χ2 (12) = 36.70, p < .05 CFI = .98, TLI = .94, RMSEA = .053. Path coefficients are standardized, † p < .06, *p < .05; **p < .01
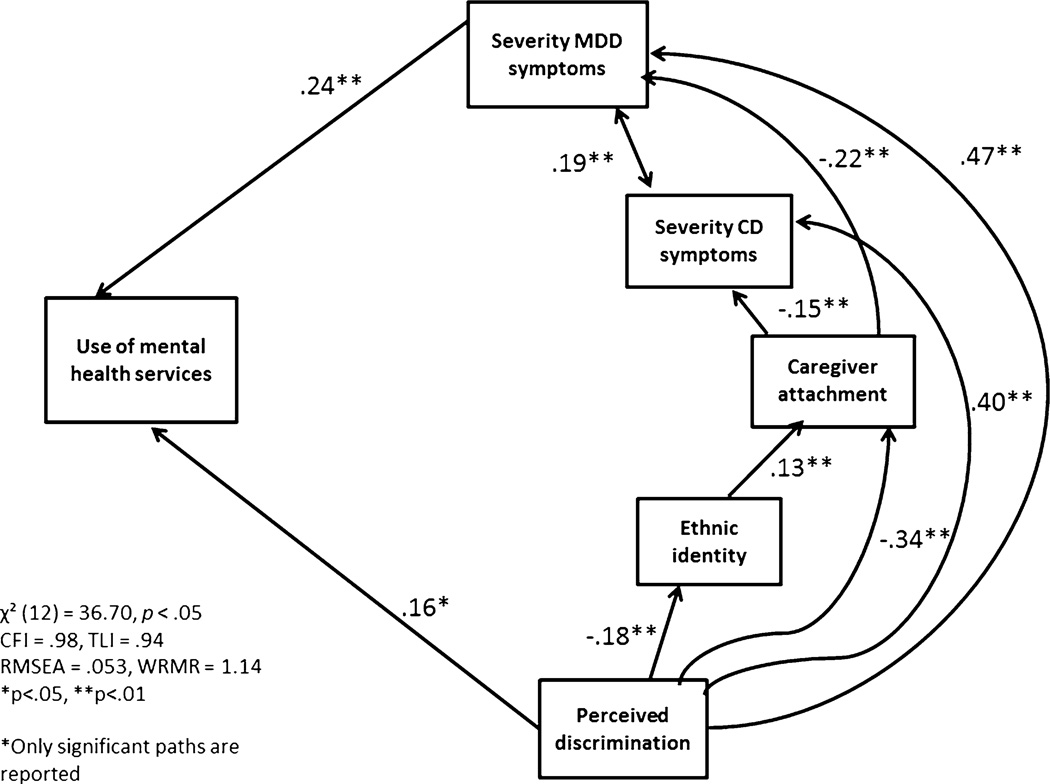
For European American girls (Fig. 2), MDD severity and perceived discrimination were positively related to service utilization. Perceived discrimination was negatively related to ethnic identity and caregiver attachment but positively related to CD and MDD severity. Caregiver attachment was negatively related to CD and MDD severity but positively associated with ethnic identity. CD and MDD severity were positively associated. Tests of indirect effects indicated an effect of perceived discrimination, via MDD severity, on service utilization (β = .11, p < .05), suggesting that psychological distress arising from discriminatory experiences were exhibited via MDD severity, which was related to service use. Ethnic identity had no direct effect on service utilization but was related to caregiver attachment. CD severity and caregiver attachment were unrelated to service utilization.
Fig. 2.
Path model for European American girls (with clinical severity scores). Fit indices χ2 (12) = 36.70, p < .05 CFI = .98, TLI = .94, RMSEA = .053. Path coefficients are standardized, †p < .06, *p < .05; **p < .01
Model with Diagnostic Scores
The multigroup model with diagnostic scores using WLSMV in which paths were allowed to vary fit the data well, χ2 (12) = 19.91, p = .07, CFI = .98, TLI = .94, RMSEA = .03 WRMR = .86. The model with loadings constrained to be equal across groups fit significantly worse, χ2 (31) = 153.27, p < .001, CFI = .702, TLI = .62, RMSEA = .07, WRMR = 2.43.
The WLS-generated model in which paths were allowed to vary freely was χ2 (12) = 18.51, p = .107, CFI = .98, TLI = .94, RMSEA = .03, compared with the model with equal constraints across groups, χ2 (31) = 140.04, p < .001, CFI = .67, TLI = .57, RMSEA = .07. The Chi square difference, Δχ2 (19) = 121.53, p < .001, suggested that the model with paths allowed to vary had a better fit to the data.
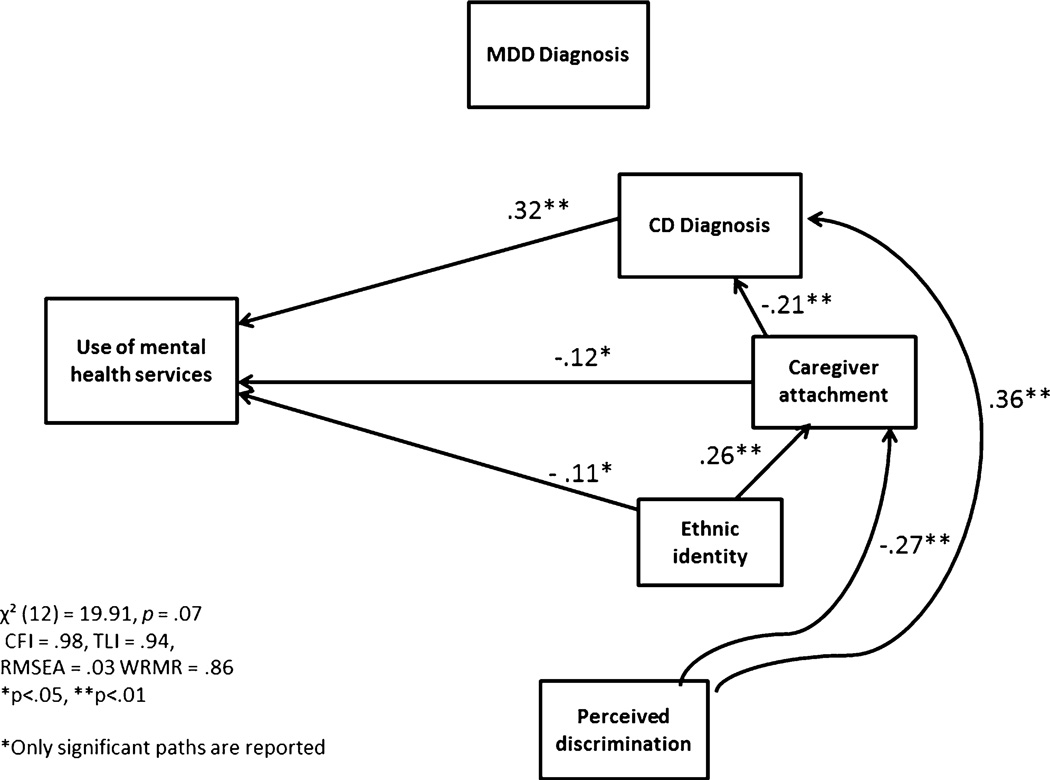
Results for African American girls paralleled the model with severity scores. Service utilization was positively related to CD diagnosis and negatively related to ethnic identity and caregiver attachment. MDD diagnosis and perceived discrimination were unrelated to service utilization. Perceived discrimination was positively related to CD diagnosis and negatively related to caregiver attachment. Caregiver attachment was negatively related to CD diagnosis. Ethnic identity was positively associated with caregiver attachment (Fig. 3). Indirect effects indicated effects of perceived discrimination on service utilization via CD diagnosis (β = .12, p < .05), ethnic identity via caregiver attachment (β = −.03, p < .05), and caregiver attachment via CD diagnosis (β = −.02, p < .05).
Fig. 3.
Path model for African American girls (with clinical diagnosis scores). Fit indices: χ2 (12) = 19.91, p = .07, CFI = .98, TLI = .94, RMSEA = .03 WRMR = .86. Path coefficients are standardized, †p < .06, *p < .05; **p < .01
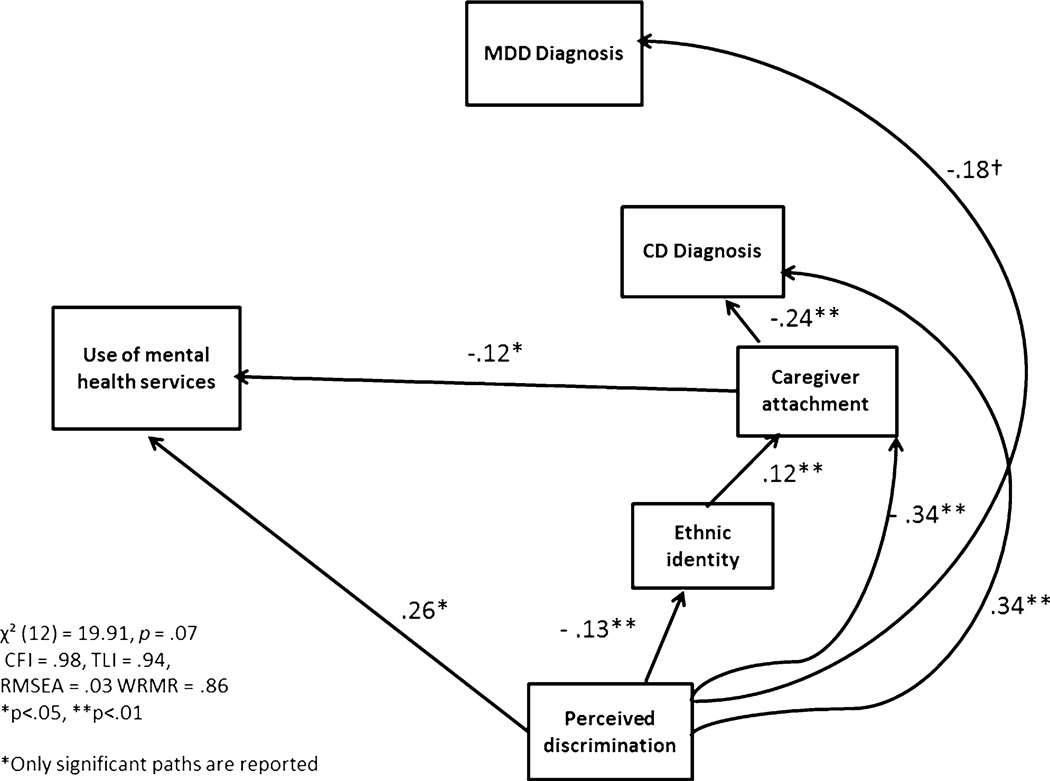
The model for European American girls using diagnostic scores differed from the previous model with severity scores (Fig. 4). In this model, both CD and MDD diagnoses were unrelated to service use. However, service utilization was positively associated with perceived discrimination and negatively associated with caregiver attachment. Perceived discrimination was negatively associated with ethnic identity and caregiver attachment but positively related to CD diagnosis. A marginal association was found for perceived discrimination and MDD diagnosis. Caregiver attachment was negatively related to CD diagnosis. As expected, ethnic identity was unrelated to service utilization but was associated with caregiver attachment. Indirect effects revealed the effect of perceived discrimination via caregiver attachment on service utilization (β = 0.03, p = .06).
Fig. 4.
Path model for European American girls (with clinical diagnosis scores). Fit indices: χ2 (12) = 19.91, p = .07, CFI = .98, TLI = .94, RMSEA = .03 WRMR = .86. Path coefficients are standardized, †p < .06, *p < .05; **p < .01
Discussion
In the present study we tested the influences of presenting problem type (by symptom severity and clinical diagnoses), ethnocultural factors, and caregiver attachment on mental health service use in a community sample of African American and European American girls. First, we find no overall effects of race on service utilization, which is contrary to previous research (Coker et al. 2009; Garland et al. 2005). Second, consistent with previous research (Gudiño et al. 2009), we find that externalizing problems, as measured by CD severity scores and diagnosis, are associated with service utilization for African American girls.
For European American girls, the relationship between clinical symptoms and service utilization differs across models. Service utilization is significantly associated with MDD severity scores; however, when using diagnostic scores, the association no longer holds. Although these results are perplexing, the contrast in the association between MDD and service utilization between the two models suggests a tendency to seek help from mental health services for psychological distress among European American families in the community, and that this tendency is more pronounced among families with girls reporting lower levels of MDD symptoms.
In addition, among European American girls, CD severity or diagnosis is not related to service use. This lack of association between clinical diagnoses and service utilization contradicts prior research finding significant relationships in clinical samples. Future research should examine how varying levels of clinical severity moderates the correlates of service utilization and how these levels differ by racial groups.
We have found that higher levels of perceived discrimination are positively associated with service utilization for European American girls. For African American girls, the relationship between perceived discrimination is not significant for service utilization. Because prior studies report a negative relationship between discrimination and service use, these findings are surprising. However, it is encouraging that parents of girls experiencing more discrimination sought services, because it may suggest families’ inclination to use services in response to their daughter’s distress in general, not only in response to clinical need. Moreover, when the discrimination is experienced by the child, parents may react more proactively to seek support for their child’s distress compared with when the discrimination is targeted at parents, which can deter service use. Future research should examine whether youth and parents’ experiences of discrimination have differing effects on seeking services; prior studies have focused only on adult populations.
The indirect effects reveal interesting patterns for African American girls: The effect of perceived discrimination on service utilization is via youth CD, suggesting that the psychological effects of perceived discrimination are significant in propelling parents to connect their adolescent girls with mental health services. These findings support literature indicating the negative effect of discrimination on mental health outcomes among youth and underscore the need for health disparities research to examine discrimination’s salient role in service use among ethnic minority youth.
Ethnic identity is related to less service utilization only for African American girls. This parallels previous findings (Richman et al. 2007), suggesting that girls reporting a stronger sense of belonging to their ethnic group are less likely to use mental health services. The negative association between ethnic identity and service utilization may indicate that significant stigma is still associated with mental health problems in the African American community (e.g., Matthews et al. 2006; Thompson-Sanders et al. 2004). Therefore, the more one values his or her ethnic group membership, the less likely he or she is to seek professional services. Considering that the “Strong Black Woman” identity emphasizes self-reliance, affect regulation, and financial and emotional independence (Beauboeuf-Lafontant 2005), African American girls who strongly identify with their ethnic group may find that relying on mental health services may be incongruent with this identity, thereby deterring them from seeking services. Indirect effects of ethnic identity, via caregiver attachment, on service utilization for African American girls across models may suggest that a strong ethnic pride and sense of belonging to one’s group is closely related to African American girls’ connection within their family, and that these relationships influence whether girls utilize services. Although African American girls who have strong ethnic identities may be from families with stable relationships, thus lowering their risk for mental health problems and need for services, the lack of an indirect effect via CD may suggest otherwise. Future research should examine the central roles of ethnic identity and family socialization in how African American youth and families perceive the need for mental health services and how they contribution to service underutilization of services.
Caregiver attachment is associated with less service use for African American girls in both models and for European American girls in the model using diagnostic scores. A plausible explanation for the negative association is that girls with cohesive family relationships may have fewer mental health problems and, therefore, less mental health service use. The indirect effects of caregiver attachment via CD for African American girls may reflect this interpretation. Future research must disentangle whether family relationships are a proxy for mental health need or whether family relationships have a distinct role in help-seeking and utilization of mental health service.
Several limitations must be addressed when interpreting the present findings. First, we used a binary measure of mental health service utilization, which limits our understanding of the variability in professional service use among the girls. In addition, our measure of service utilization did not assess families’ responses to the specific type of service used, which limited our understanding of the distribution of specific types of services used in this sample. Further, the effect of service type variability was not examined. Although our measure of service utilization included broad categories of responses for professional mental health services, community services, and hospitals, only a small number of individuals reported hospital use and we were unable to accurately distinguish between participants’ mental health professional use and community service or hospital use (i.e., the listed professionals may be sought in these service settings). Second, much of the current literature examining mental health service utilization has focused on clinical samples that are in need of such services (e.g., Gudiño et al. 2009; Martinez et al. 2013), and this current study used a community sample in which the majority of youths did not meet diagnostic criteria for CD or MDD, which may affect need for services. A comparison of clinical and community samples in service utilization is an important future step to examine how the severity of problems affect actual service utilization, and how ethnicity and other factors mediate or moderate this relationship. Third, we were unable to control for health insurance status in our analyses because health insurance data available were only for Medicaid and not health insurance in general, thus leading to significant missing data on this variable in our sample. Therefore, we chose public assistance use as a measure to control for the availability of services among families. Fourth, our data are cross-sectional. Therefore, the results of the model do not confirm causality, and a model with all the prediction paths reversed may be equally plausible. Fifth, our measure of perceived discrimination captured experiences of discrimination in general, which may include various discriminatory experiences arising from complex peer relations rather than one’s race. Future research should examine how varying discrimination experiences (e.g., racial/ethnic discrimination, discrimination related to mental health problems) relate to service utilization. Sixth, we used the membership and belonging subscale of the MEIM (Phinney 1992), which did not include items on exploration or ethnic behaviors. Evidence suggests that a sense of belonging is also a significant aspect of one’s identity for not only minority but majority youth (Yasui et al. 2004), and that the exploration of one’s ethnic group may define the salience of one’s ethnic or racial group. Future studies should examine how different aspects of adolescents’ ethnic identity may inform attitudes and behaviors regarding seeking mental health services.
In summary, this study is an initial attempt in uncovering the salience of cultural and contextual factors that influence racial disparities in mental health service utilization. Although the findings are not definitive, they are certainly suggestive. The significant relationship between service utilization and culturally anchored factors such as ethnic identity and perceived discrimination signals the need to examine ethnic specific patterns of engaging in mental health services. In light of the widespread movement of evidence-based treatments among more diverse populations, understanding the barriers to or positive influences on service utilization will be a critical endeavor, considering the ongoing dilemma of poorer service utilization among such groups.
Acknowledgments
This research was supported by Grants from the National Institute of Mental Health (MH056630), the National Institute on Drug Abuse (DA012237), the FISA Foundation, and the Falk Fund. The authors would like to thank the participants and their families for their many contributions to this study.
Contributor Information
Miwa Yasui, Email: myasui@uchicago.edu, University of Chicago, Chicago, USA.
Alison E. Hipwell, University of Pittsburgh, Pittsburgh, USA
Stephanie D. Stepp, University of Pittsburgh, Pittsburgh, USA
Kate Keenan, University of Chicago, Chicago, USA.
References
- Bauman KE, Ennett ST, Foshee VA, Pemberton M, Hicks K. Correlates of participation in a family-directed tobacco and alcohol prevention program for adolescents. Health Education and Behavior. 2001;28:440–461. doi: 10.1177/109019810102800406. [DOI] [PubMed] [Google Scholar]
- Beauboeuf-Lafontant T. Keeping up appearances, getting fed up: The embodiment of strength among African American women. Meridians: Feminism, Race, Transnationalism. 2005;5:104–123. [Google Scholar]
- Brauner C, Stephens CB. Estimating the prevalence of early childhood emotional/behavioral disorders: Issues and challenges. Public Health Reports. 2006;121(3):303–310. doi: 10.1177/003335490612100314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown T. Confirmatory factor analysis for applied research. New York: Guildford; 2006. [Google Scholar]
- Casagrande SS, Gary TL, LaVeist TA, Gaskin DJ, Cooper LA. Perceived discrimination and adherence to medical care in a racially integrated community. Journal of General Internal Medicine. 2007;22:389–395. doi: 10.1007/s11606-006-0057-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chabra A, Chavez GF, Harris ES, Shah R. Hospitalization for mental illness in adolescents: Risk groups and impact on the health care system. Journal of Adolescent Health. 1999;24:349–356. doi: 10.1016/s1054-139x(98)00116-5. [DOI] [PubMed] [Google Scholar]
- Chang J, Natsuaki MN, Chen C. The importance of family factors and generation status: Mental health service use among Latino and Asian Americans. Cultural Diversity and Ethnic Minority Psychology. 2013;19:236–247. doi: 10.1037/a0032901. [DOI] [PubMed] [Google Scholar]
- Chen HL, Kwan KKL, Sevig T. Racial and ethnic minority college students’ stigma associated with seeking psychological help: Examining psychocultural correlates. Journal of Counseling Psychology. 2013;60:98–111. doi: 10.1037/a0031169. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd ed. Mahwah, NJ: Erlbaum; 2003. [Google Scholar]
- Coker TR, Elliot MN, Kataoka SH, Schwebel DC, Mrug S, Grunbaum J, et al. Racial/ethnic disparities in the mental health care utilization of 5th-grade children. Academic Pediatrics. 2009;9:89–96. doi: 10.1016/j.acap.2008.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings JR, Druss BG. Racial/ethnic differences in mental health service use among adolescents with major depression. Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50:160–170. doi: 10.1016/j.jaac.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flora DB, Curran PJ. An empirical evaluation of alternative methods of estimation for confirmatory factor analysis with ordinal data. Psychological Methods. 2004;9:466–491. doi: 10.1037/1082-989X.9.4.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gadow K, Sprafkin J. Child/adolescent symptom inventories manual. Stony Brook, NY: Checkmate Plus; 1994/1997. [Google Scholar]
- Garland AF, Landsverk JL, Hough RL, Ellis-MacLeod E. Type of maltreatment as a predictor of mental health service use for children in foster care. Child Abuse and Neglect. 1996;20:675–688. doi: 10.1016/0145-2134(96)00056-7. [DOI] [PubMed] [Google Scholar]
- Garland AF, Lau AS, Yeh M, McCabe KM, Hough RL, Landsverk JA. Racial and ethnic differences in utilization of mental health services among high-risk youths. The American Journal of Psychiatry. 2005;162:1336–1343. doi: 10.1176/appi.ajp.162.7.1336. [DOI] [PubMed] [Google Scholar]
- Gorman-Smith D, Tolan PH, Henry DB, Leventhal A, Schoeny M, Lutovsky K, Quintana E. Predictors of participation in a family-focused preventive intervention for substance use. Psychology of Addictive Behaviors. 2002;16:S55–S64. doi: 10.1037/0893-164x.16.4s.s55. [DOI] [PubMed] [Google Scholar]
- Gudiño OG, Lau AS, McCabe KM, Hough RL. Understanding racial/ethnic disparities in youth mental health services: Do disparities vary by problem type? Journal of Emotional and Behavioral Disorders. 2009;17:3–16. [Google Scholar]
- Gullone E, Robinson K. The inventory of parent and peer attachment-revised (IPPA-R) for children: A psychometric investigation. Clinical Psychology and Psychotherapy. 2005;12:67–79. [Google Scholar]
- Harpaz-Rotem I, Leslie D, Rosenheck RA. Treatment retention among children entering a new episode of mental health care. Psychiatric Services. 2004;55:1022–1028. doi: 10.1176/appi.ps.55.9.1022. [DOI] [PubMed] [Google Scholar]
- Herz DC. Understanding the use of mental health placements by the juvenile justice system. Journal of Emotional and Behavioral Disorders. 2001;9:172–181. [Google Scholar]
- Hipwell AE, Loeber R, Stouthamer-Loeber M, Keenan K, White H, Kroneman L. Characteristics of girls with early onset disruptive and antisocial behaviour. Criminal Behaviour and Mental Health. 2002;12:99–118. doi: 10.1002/cbm.489. [DOI] [PubMed] [Google Scholar]
- Horwitz SM, Gary LC, Briggs-Gowan MJ, Carter AS. Do needs drive services use in young children? Pediatrics. 2003;112:1373–1378. doi: 10.1542/peds.112.6.1373. [DOI] [PubMed] [Google Scholar]
- Kataoka S, Zhang L, Wells KB. Unmet need for mental health care among U.S. children: Variation by ethnicity and public assistance status. American Journal of Psychiatry. 2002;159(9):1548–1555. doi: 10.1176/appi.ajp.159.9.1548. [DOI] [PubMed] [Google Scholar]
- Keenan K, Hipwell A, Chung T, Stepp S, Stouthamer-Loeber M, Loeber R, et al. The Pittsburgh Girls Study: Overview and initial findings. Journal of Clinical Child and Adolescent Psychology. 2010;39:506–521. doi: 10.1080/15374416.2010.486320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamkaddem M, Essink-Bot ML, Deville W, Foets M, Stronks K. Perceived discrimination outside health care settings and health care utilization of Turkish and Moroccan GP patients in the Netherlands. European Journal of Public Health. 2011;22:472–478. doi: 10.1093/eurpub/ckr113. [DOI] [PubMed] [Google Scholar]
- Leslie LK, Hurlburt MS, James S, Landsverk J, Slymen DJ, Zhang J. Relationship between entry into and mental health service use. Psychiatric Services. 2005;56:981–987. doi: 10.1176/appi.ps.56.8.981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leslie LK, Landsverk J, Ezzet-Loftstrom R, Tschann JM, Slymen DJ, Garland AF. Children in foster care: Factors influencing outpatient mental health service use. Child Abuse and Neglect. 2000;24:465–476. doi: 10.1016/s0145-2134(00)00116-2. [DOI] [PubMed] [Google Scholar]
- Lochman JE, Salekin RT. Prevention and intervention with aggressive and disruptive children: Next steps in behavioral intervention research. Behavior Therapy. 2003;34:413–419. [Google Scholar]
- Longshore D. Help-seeking by African American drug users: A prospective analysis. Addictive Behaviors. 1999;24:683–686. doi: 10.1016/s0306-4603(98)00111-7. [DOI] [PubMed] [Google Scholar]
- Martinez JI, Gudino OG, Lau AS. Problem-specific racial/ethnic disparities in pathways from maltreatment exposure to specialty mental health service use for youth in child welfare. Child Maltreatment. 2013;18:98–107. doi: 10.1177/1077559513483549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews AK, Corrigan PW, Smith BM, Aranda F. A qualitative exploration of African Americans’ attitudes toward mental illness and mental illness treatment seeking. Rehabilitation Education. 2006;20:253–268. [Google Scholar]
- Merikangas KR, Jin R, He JP, Kessler RC, Lee S, Sampson NA, et al. Prevalence and correlates of bipolar spectrum disorder in the World Mental Health Survey Initiative. Archives of General Psychiatry. 2011;68:241–251. doi: 10.1001/archgenpsychiatry.2011.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller LM, Southam-Gerow MA, Allin RB. Who stays in treatment? Child and family predictors of youth client retention in a public mental health agency. Child & Youth Care Forum. 2008;37:153–170. doi: 10.1007/s10566-008-9058-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Harrington H, Milne BJ. Males on the life-course-persistent and adolescence-limited antisocial pathways: Follow-up at age 26 years. Development and Psychopathology. 2002;14:179–207. doi: 10.1017/s0954579402001104. [DOI] [PubMed] [Google Scholar]
- Muthén B, Asparouhov T. Latent variable analysis with categorical outcomes: Multiple-group and growth modeling in Mplus. 2002 [Version 5], December 9, 2002. [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. Los Angeles, CA: Muthen & Muthen; 2011. [Google Scholar]
- Nyborg VM, Curry JF. The impact of perceived racism: Psychological symptoms among African American boys. Journal of Clinical Child & Adolescent Psychology. 2003;32:258–266. doi: 10.1207/S15374424JCCP3202_11. [DOI] [PubMed] [Google Scholar]
- Perrino T, Coats worth JD, Briones E, Pantin H, Szapocznik J. Initial engagement to parent-centered prevention interventions: A family systems perspective. Journal of Primary Prevention. 2001;22:21–44. [Google Scholar]
- Phinney J. The multigroup ethnic identity measure: A new scale for use with adolescents and youth adults from diverse groups. Journal of Adolescent Research. 1992;7:156–176. [Google Scholar]
- Richman LS, Kohn-Wood LP, Williams DR. The role of discrimination and racial identity for mental health service utilization. Journal of Social and Clinical Psychology. 2007;26:960–981. [Google Scholar]
- Simons RL, Murry V, McLoyd V, Lin K, Cutrona C, Conger RD. Discrimination, crime, ethnic identity and parenting as correlates of depressive symptoms among African American children: A multilevel analysis. Developmental Psychopathology. 2002;14:371–393. doi: 10.1017/s0954579402002109. [DOI] [PubMed] [Google Scholar]
- Thompson-Sanders VL, Bazile A, Akbar M. African Americans’ perceptions of psychotherapy and psychotherapists. Professional Psychology: Research and Practice. 2004;35:19–26. [Google Scholar]
- Verhulst FC, van der Ende J. Factors associated with child mental health service use in the community. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:901–909. doi: 10.1097/00004583-199707000-00011. [DOI] [PubMed] [Google Scholar]
- Williams DR, Yu Y, Jackson J, Anderson N. Racial differences in physical and mental health: Socioeconomic status, stress, and discrimination. Journal of Health Psychology. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- Wong CA, Eccles JS, Sameroff A. The influence of ethnic discrimination and ethnic identification on African American adolescents’ school and socioemotional adjustment. Journal of Personality. 2003;71:1197–1232. doi: 10.1111/1467-6494.7106012. [DOI] [PubMed] [Google Scholar]
- Yasui M, Dorham CR, Dishion TJ. Ethnic identity and psychological adjustment: A validity analysis for European American and African American adolescents. Journal of Adolescent Research. 2004;19:807–825. [Google Scholar]