Introduction
Uterine tumors resembling ovarian sex cord tumors (UTROSCTs) are a rare group of stromal neoplasms containing prominent sex cord-like elements. Since they were first described in 1945 by Morehead and Bowman [1], no more than 100 such tumors have been reported [2]. In a report by Clement and Scully [3], these neoplasms were divided into 2 groups on the basis of clinical and histologic patterns. The first group (group I) included endometrial stromal tumors with less than 50 % sex cord-like elements, and the second group (group II) included UTROSCTs exhibiting sex cord-like differentiation of more than 50 %. In the latest, according to the World Health Organization classification of uterine neoplasms, UTROSCTs were placed in a miscellaneous category of tumors of the uterine corpus because of their different morphology and benign clinical behaviors [4]. More recently, UTROSCTs have been suggested to be unusual neoplasms of uncertain malignancy with polyphenotypic immunohistochemical expression, characterized by positivity for sex cord, epithelial, and myoid markers [5, 6]. These tumors usually occur in premenopausal or menopausal women. Most patients have symptoms such as abnormal vaginal bleeding, abdominal pain, and enlarged uterus or a palpable uterine mass on physical examination [7]. In most cases, UTROSCT is diagnosed incidentally after hysterectomy for a clinical diagnosis of an endometrial polyp [8, 9] or sometimes leiomyoma [10].
We report a case of UTROSCT in a postmenopausal woman with vaginal bleeding who was diagnosed with uterine sarcoma at a local clinic.
Case Report
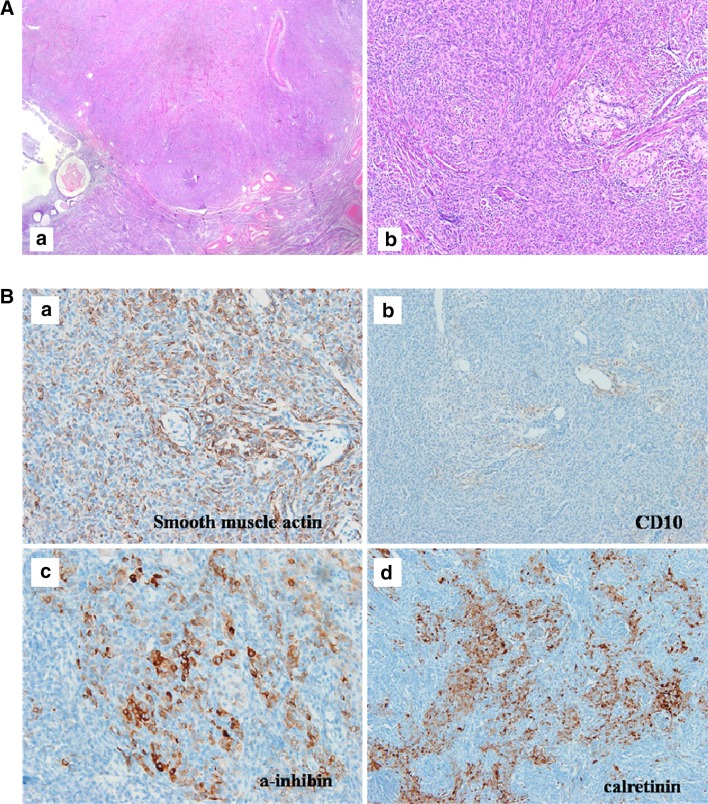
A 56-year-old woman, gravida 4, para 2, was admitted to our institute in August 2012 for management of abnormal vaginal bleeding and uterine malignancy tumor. She had reached menopause 2 years previously and had experienced irregular vaginal bleeding for 1 year. She visited a local gynecologic clinic underwent endometrial curettage. Pathology indicated malignant tumor with rhabdoid features, and the patient was referred to our clinic. Her body mass index was 20.5 kg/m2, and her medical history was unremarkable. Transvaginal ultrasonography examination revealed a lesion in the uterine fundus, which showed an irregular hyperechoic mass, and there was not clear margin between the myometrium and the mass. Fluid collection was noted in the endometrial cavity (Fig. 1). Computed tomography of the abdomen and pelvis showed a 2 cm mildly enhanced nodular mass, which was suspected to be malignant mixed Müllerian tumor or endometrial cancer with myometrial invasion, but no metastasis was noted (Fig. 2). Abdominal hysterectomy with bilateral salpingo-oophorectomy was performed, and the removed organs were submitted for pathologic examination. The removed uterus measured 7.5 × 5.0 × 3.0 cm and weighed 74.8 g. The cervix, fallopian tubes, and both ovaries were unremarkable on gross observation. Macroscopic examination, showed that the lesion was projecting into the uterine cavity. On section, the uterine mass was located submucosally with relatively good margination and yellowish color that was more intense than that for usual leiomyoma. The uterine mass measured 2.2 cm in diameter (Fig. 3). Microscopically, the tumor consisted of compactly packed, elongated, or rounded cells and irregular trabeculae, cords, or clusters of larger or foamy cells (Fig. 4a). Immunohistochemical stains were positive for smooth muscle actin and negative for CD10, a marker of endometrial stromal cells, and desmin in the elongated or rounded cells and positive for α-inhibin and calretinin in the larger cells (Fig 4b). Histologic and immunohistochemical findings indicated a mixture of smooth muscle elements and sex cord-like elements, suggesting a diagnosis of UTROSCT. The patient was discharged on the 8th postoperative day without complications. Follow-up based on clinical examination and imaging studies and laboratory tests was planned.
Fig. 1.
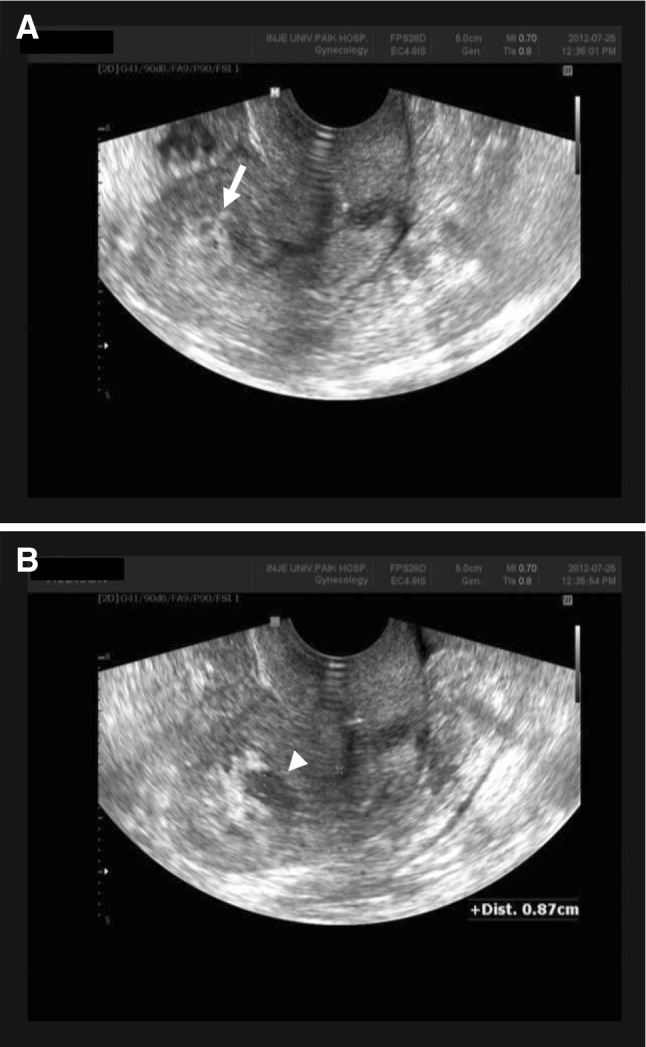
Transvaginal ultrasonography. a Irregularly shaped 2 cm mass with hyperechoic pattern is seen in the uterine fundus (white arrow), and b some of the fluid collection is shown in the endometrial cavity (arrow head)
Fig. 2.
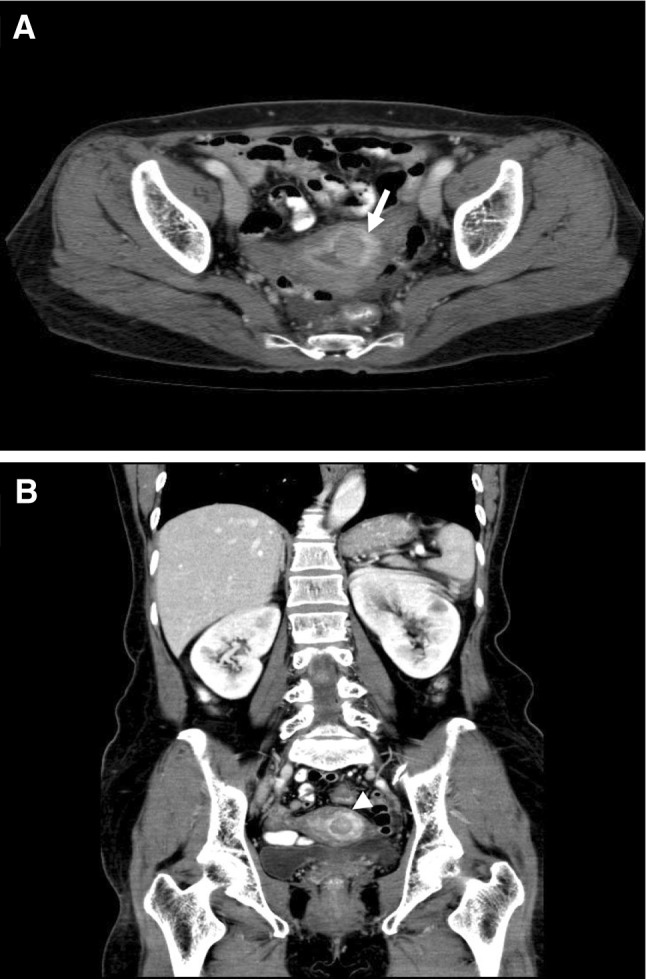
Computed tomography (CT) of the abdomen and pelvis. a Axial view of abdominal and pelvic CT. A small (2 cm) mass which was mildly enhanced nodular mass with myometrial invasion was shown (white arrow). The mass was suspected to be a malignant mixed Müllerian tumor (MMMT) or endometrial cancer. b Coronary view abdominal and pelvic CT (arrow head). No metastatic lesions are noted
Fig. 3.
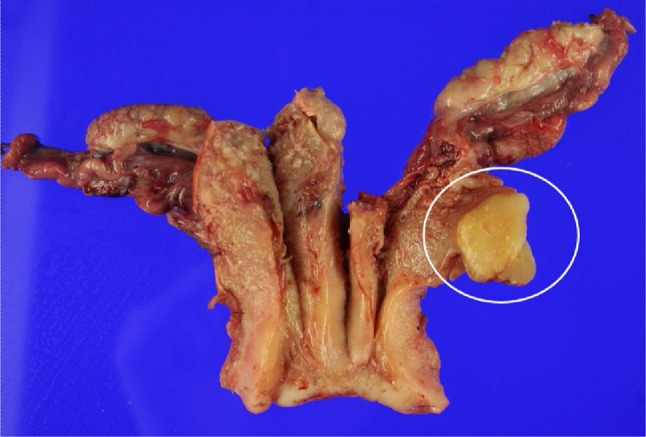
Macroscopic examination. The 2.2-cm uterine mass is located in the submucosal portion with good margination and a yellowish color that is more intense than that for usual leiomyoma
Fig. 4.
a Microscopic view. The mass is located submucosally and is relatively well delineated. Compactly packed elongated or rounded tumor cells with scattered larger cell clusters are seen. a Hematoxylin and eosin staining : low-power view (×10). b Hematoxylin and eosin staining : high-power view (×100). b Immunohistochemical analysis. The elongated tumor cells are positive for a smooth muscle actin; negative for b CD10, a marker of endometrial stromal cells; and focal positive for c α-inhibin and d calretinin, markers of sex cord differentiation
Discussion
UTROSCTs are considered as neoplasms and show benign behavior: they are different from endometrial stromal tumors with sex cord-like elements (ESTSCLEs or group I), which are associated with metastasis and recurrence. The clinical behavior of ESTSCLEs is similar to that of low-grade endometrial stromal sarcoma, which has a locoregional or distant relapsing rate of approximately 50 % [3, 11]. Although most UTROSCTs follow a benign course, some cases have shown recurrence, with omental, retroperitoneal extension, or subcutaneous suprapubic and abdominal metastases [12–14]. These neoplasms usually occur in middle-aged women with an average age of 50 years who are premenopausal or menopausal [7]. Clinical manifestations include abnormal uterine bleeding, enlarged uterus, palpable mass, or pelvic pain [7–9]. Therefore, most patients undergo hysterectomy with or without bilateral salpingo-oophorectomy. Because of the low recurrence rate, conservative management with fertility-sparing tumor resection has been suggested as an alternative to hysterectomy [10].
Although the exact pathogenesis of UTROSCTs has not yet been established, some researchers have hypothesized that UTROSCTs originate from an uncommitted stem cell enabling both epithelial and sex cord differentiation, whereas others have postulated that UTROSCTs can be considered a variant of endometrial stromal neoplasm [6, 15]. In most cases, UTROSCTs were diagnosed incidentally after hysterectomy for a treatment after clinical diagnosis of an endometrial polyp [8, 9] or a leiomyoma [10]. In our case, the patient was a menopausal woman diagnosed with uterine sarcoma by biopsy at a local clinic. However, she was diagnosed with UTROSCT on final pathology after hysterectomy in our hospital. UTROSCT can present some diagnostic difficulties when healthcare practitioners examine a small biopsy specimen, because this neoplasm can be similar to other benign or malignant lesions with mesenchymal or epithelial structures. Because UTROSCT shows a large variety of histological features, it is necessary to differentiate it from a large number of neoplasms. Epithelioid leiomyomas, stromal tumors, perivascular epithelioid cell tumors, melanoma, and endometrioid carcinoma should be differentiated from UTROSCT [7]. Therefore, immunohistochemical analysis is useful for differentiating UTROSCT from leiomyoma, ESTSCLE, and other malignant epithelial neoplasms such as endometrioid adenocarcinoma and uterine mesonephric carcinoma. According to Irving et al. [5], reliable histochemical markers for UTROSCT are calretinin, inhibin, CD99, and Melan-A, and positivity for calretinin and at least one of the other 3 markers is suggestive of UTROSCT. In our case, tumor cells were positive for calretinin and α-inhibin.
UTROSCTs are usually benign [3] and have low recurrence rates, and they are generally treated with hysterectomy alone. If patients desire to have children, fertility-sparing tumor resection can be suggested [10]. Few cases of recurrence of UTROSCT have been reported [14]. Therefore, close long-term follow-up with imaging studies such as vaginal ultrasonography, computed tomography, pelvic magnetic resonance image, and chest X-ray is required [16].
In our case, the patient received total abdominal hysterectomy with bilateral salpingo-oophorectomy in August 2012 and has been followed-up thereafter. This patient was initially diagnosed with uterine sarcoma by endometrial biopsy, at a local clinic, and her symptom was abnormal vaginal bleeding in a menopausal state. Therefore, we had good reason to be suspicious of a malignancy, but her final diagnosis was confirmed as UTROSCT by immunohistochemical analysis. UTROSCT is a rare tumor, and it can sometimes be misdiagnosed as malignancy in postmenopausal women. Furthermore, radical surgery or overtreatment can be performed after misdiagnosis. UTROSCT is diagnosed using immunohistochemical analysis, which is justified because it prevents overtreatment and the need for long-term follow-up.
Acknowledgments
Conflict of interest
The authors have no conflicts of interest to declare.
Jung Mi Byun
, MD is an Assistant Professor of Obstetrics and Gynecology at Inje University, School of Medicine. Dr. Byun received her medical degree from the Inje University in 2004 and completed her residency training in Obstetrics & Gynecology at Busan Paik Hospital, Inje University in Busan from 2005 to 2009. She continued with subspecialty training as a fellow in Gynecology Oncology at the Inje University. She is an expert in laparoscopic operation and management of gynecologic cancer. Her clinical research interests include management and epidemiology of gynecologic cancer. Dr. Byun is a member of the International Gynecological Cancer Society (IGCS) and Korean Cancer Association for gynecologic oncology.
References
- 1.Morehead RP, Bowman MC. Heterologous mesodermal tumors of the uterus: report of a neoplasm resembling a granulosa cell tumor. Am J Pathol. 1945;21:53–61. [PMC free article] [PubMed] [Google Scholar]
- 2.Garuti G, Gonfiantini C, Mirra M, et al. Uterine tumor resembling ovarian sex cord tumors treated by resectoscopic surgery. J Minim Invasive Gynecol. 2009;16:236–240. doi: 10.1016/j.jmig.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 3.Clement PB, Scully RE. Uterine tumors resembling ovarian sex-cord tumors. A clinicopathologic analysis of 14 cases. Am J Clin Pathol. 1976;66:512–525. doi: 10.1093/ajcp/66.3.512. [DOI] [PubMed] [Google Scholar]
- 4.Siverberg SG, Kurman RJ, Nogales F. Tumours of uterine corpus. In: Tavassoli FA, Devilee P, editors. Pathology and genetics of tumours of the breast and female genital organs. Lyon: IARC Press; 2003. pp. 217–257. [Google Scholar]
- 5.Irving JA, Carinelli S, Prat J. Uterine tumors resembling ovarian sex cord tumors are polyphenotypic neoplasms with true sex cord differentiation. Mod Pathol. 2006;19:17–24. doi: 10.1038/modpathol.3800475. [DOI] [PubMed] [Google Scholar]
- 6.Hurrell DP, McCluggage WG. Uterine tumour resembling ovarian sex cord tumour is an immunohistochemically polyphenotypic neoplasm which exhibits coexpression of epithelial, myoid and sex cord markers. J Clin Pathol. 2007;60:1148–1154. doi: 10.1136/jcp.2006.044842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Czernobilsky B. Uterine tumors resembling ovarian sex cord tumors: an update. Int J Gynecol Pathol. 2008;27:229–235. doi: 10.1097/PGP.0b013e3181569a21. [DOI] [PubMed] [Google Scholar]
- 8.Pang LC. Endometrial stromal sarcoma with sex cord-like differentiation associated with tamoxifen therapy. South Med J. 1998;91:592–594. doi: 10.1097/00007611-199806000-00018. [DOI] [PubMed] [Google Scholar]
- 9.Oliva E, Clement P, Young R. Mesenchymal tumours of the uterus: selected topics emphasizing diagnostic pitfalls. Curr Diagn Pathol. 2002;8:268–282. doi: 10.1054/cdip.2002.0126. [DOI] [Google Scholar]
- 10.Hillard JB, Malpica A, Ramirez PT. Conservative management of a uterine tumor resembling an ovarian sex cord-stromal tumor. Gynecol Oncol. 2004;92:347–352. doi: 10.1016/j.ygyno.2003.09.011. [DOI] [PubMed] [Google Scholar]
- 11.Al-Salam S, El-Terifi H, Ghazal-Aswad S. Low-grade endometrial stromal sarcoma with sex cord-like differentiation metastatic to the thoracic spines. APMIS. 2006;114:651–655. doi: 10.1111/j.1600-0463.2006.apm_409.x. [DOI] [PubMed] [Google Scholar]
- 12.Kantelip B, Cloup N, Dechelotte P. Uterine tumor resembling ovarian sex cord tumors: report of a case with ultrastructural study. Hum Pathol. 1986;17:91–94. doi: 10.1016/S0046-8177(86)80161-7. [DOI] [PubMed] [Google Scholar]
- 13.Horn LC, Stegner HE. Uterine stromal tumor with ovarian sex cord differentiation. Pathologe. 1995;16:421–425. doi: 10.1007/s002920050124. [DOI] [PubMed] [Google Scholar]
- 14.O’Meara AC, Giger OT, Kurrer M, et al. Case report: recurrence of a uterine tumor resembling ovarian sex-cord tumor. Gynecol Oncol. 2009;114:140–142. doi: 10.1016/j.ygyno.2009.03.021. [DOI] [PubMed] [Google Scholar]
- 15.Hauptmann S, Nadjari B, Kraus J, et al. Uterine tumor resembling ovarian sex-cord tumor—a case report and review of the literature. Virchows Arch. 2001;439:97–101. doi: 10.1007/s004280100455. [DOI] [PubMed] [Google Scholar]
- 16.Giordano G, Lombardi M, Brigati F, et al. Clinicopathologic features of 2 new cases of uterine tumors resembling ovarian sex cord tumors. Int J Gynecol Pathol. 2010;29:459–467. doi: 10.1097/PGP.0b013e3181dfcfdc. [DOI] [PubMed] [Google Scholar]