Abstract
Purpose
Single-port laparoscopic splenectomy has been performed sporadically. The aim of this study is to assess our experience with single-port laparoscopic splenectomy compared to conventional multiport laparoscopic surgery for the usual treatment modality for various kinds of splenic disease.
Methods
Between October 2008 to February 2014, 29 patients underwent single-port laparoscopic splenectomy and 32 patients received multiport laparoscopic splenectomy. We retrospectively analyzed the clinical outcomes of single-port group and multiport group.
Results
The body mass index and disease profiles of the both groups were similar. The operative times of single-port and multiport group were 113.6 ± 39.9 and 95.9 ± 38.9 minutes, respectively (P = 0.946). The operative blood loss of the two groups were 295.8 ± 301.3 and 322.5 ± 254.5 mL (P = 0.582). Postoperative retrieved splenic weight of the single-port and multiport groups were 283.9 ± 300.7 and 362.3 ± 471.8 g, respectively (P = 0.261). One single-port partial splenectomy and 6 multiport partial splenectomies were performed in this study. There was one intraoperative gastric wall injury. It occurred in single-port group, which was successfully managed during the operation. Each case was converted to laparotomy in both groups due to bleeding. There was one mortality case in the multiport laparoscopic splenectomy group, which was not related to the splenectomy. Mean hospital stay of the single-port and multiport group was 5.8 ± 2.5 and 7.3 ± 5.2 days respectively (P = 0.140).
Conclusion
Single-port laparoscopic splenectomy seems to be a feasible approach for various kinds of splenic disease compared to multiport laparoscopic surgery.
Keywords: Splenectomy, Laparoscopy
INTRODUCTION
After Delaitre and Maignien [1] reported the first splenectomy case using laparoscopic approach in 1991, laparoscopic splenectomy (LS) has been performed by many surgeons for hematologic diseases such as idiopathic thrombocytopenic purpura and hereditary spherocytosis, and malignancies of spleen that are either primary or metastatic lesion [2,3,4,5,6]. Because surgeons have performed splenectomy by laparoscopic technique, this operation could be expected to achieve many improvements, such as reducing the length of abdominal incision, shortening of hospital stay, and less perioperative pain[7,8,9,10,11].
Over the course of time, the technique has advanced and several surgeons have introduced different kinds of laparoscopic procedures such as a single-port laparoscopic surgery, a hand assisted laparoscopic surgery, and a reduced port laparoscopic surgery [12,13,14,15]. The single-port laparoscopic surgery has been expected to satisfy patient demand of cosmesis or to decrease pain by reducing trocar incisions. As a result, single-port laparoscopic splenectomy (SPLS) has been preferred by some surgeons [15,16,17].
In the present study, we introduced our experience of SPLS and multiport laparoscopic splenectomy (MPLS). We compared SPLS with MPLS and evaluated the feasibility of SPLS from our experience.
METHODS
From October 2008 to February 2014, a total of 61 patients were selected to undergo SPLS (group 1, n = 29) or MPLS (group 2, n = 32). Without upper abdominal surgery and marked splenomegaly, in which caudal margin extends to umbilical level, all of the diseases needing splenectomy were indicative of LS. For multiport laparosocpic surgery, the patients requiring concomitant surgery were the primary candidates in general. Laparoscopic partial splenectomy was regarded as technically challenging so we have not yet established indication and one single-port laparoscopic trial was made in this report.
We started laparoscopic approach through a multiport at the first attempt at operation. For the introduction of SPLS, we made exclusion criteria; concomitant and partial. However, we were able to apply them by single-port, as we had experienced a large number of SPLS. Two procedures of LS were performed by two surgeons specialized in laparoscopic surgery. All patients agreed with the surgical technique of these operations. After Institutional Review Board approval and informed consent, all records and medical charts of patients were reviewed retrospectively.
Most patients were injected with vaccines against Haemophilus influenzae type B, pneumococcus and meningococcus at least two weeks before the elective splenectomy and the remainders vaccinated postoperatively. All patients were evaluated for age, gender, body mass index (BMI), radiologic dimension of spleen. The radiologic dimension of spleen was evaluated by CT. The dimension was recorded by the maximum length which was measured as the greatest overall dimension in the coronal and axial planes. The factors related to the operation (operation time, the length of incision, estimated blood loss (EBL), spleen weight, number of trocars, the length of postoperative hospital stay) were also evaluated in the current study for analysis. The operation time was recorded between the skin incision to closure and the length of postoperative hospital stay was defined as the length of days between the operation and the discharge or transfer to other departments, which were department of hematology or infection. The length of skin incision in SPLS was measured after closing the skin.
Surgical procedure
The procedures of both groups were similar excepting the number of trocars. All patients were positioned in right lateral decubitus and bent at the waist to increase the space between the iliac crest and subcostal margin. The surgeon and the assistant stood on the right side of the patient. The insertion site of the single-port trocar was made at the left upper quadrant site (umbilicus level of left anterior axillary line) through a 4-cm transverse skin incision. We used two kinds of multichannel trocars for single-port insertion. One of them was surgical glove with extrasmall wound retractor (ALEXIS wound retractor XS, Applied Medical, Rancho Santa, CA, USA). The glove was attached with two 5-mm trocars and one 10-mm trocar. The other trocar was a Glove port (Nelis, Seoul, Korea), which was composed of 4 trocar channels and 2 rings with gas insufflation and exsufflation gates. For the 2-port procedure, an additional 5-mm trocar (Excel Endopath, Ethicon Endo-Surgery, Cincinnati, OH, USA) was inserted at the subxiphoid area accompanied with a multichannel single-port device. In cases of 3-port or 4-port, single-channel trocars (Excel Endopath, Ethicon Endo-Surgery) were used for operation, not multichannel trocars. Basically, one 12-mm incision at the midepigastric area, one 10-mm transumbilical incision for the scope, and other additional 5-mm incisions for the instruments at the left upper quadrant, below the costal margin, were used in MPLS.
For the 5-mm and 10-mm, a 30-degree rigid telescope (Olympus, Center Valley, PA, USA) was used as laparoscopic camera in MPLS and a flexible tip 10-mm scope was used in SPLS (Olympus). The 5-mm laparoscopic graspers, dissectors and scissors were used as laparoscopic instruments. The ultrasonic scalpel (Harmonic ACE, Ethicon Endo-Surgery) and the 12-mm endovascular stapler (Echelon Flex 69 Endopath stapler with white cartilage, Ethicon Endo-surgery) were used for ligating and dissecting vessels and tissues of patients. Sometimes 5-mm or 10-mm laparoscopic endo-clips (Ethicon Endo-Surgery) were used for ligating splenic vessels.
After insertion of trocar, we dissected the gastrocolic and gastrosplenic ligaments to access the lesser sac by using the ultrasonic scalpel or monopolar hook (Endopath Probe Plus II, Ethicon Endo-Surgery). The short gastric vessels were dissected by using endo-clips or ultrasonic scalpel, if needed. And then, by dividing splenorenal and splenophrenic ligaments, the spleen could be moved medially. After mobilization of spleen was finished, the splenic hilum was exposed and splenic vessels were ligated with one or two 12-mm endovascular staplers or endo-clips. Once the spleen was detached freely, the specimen was placed in the endo-bag and taken out through the trocar site in SPLS. For specimen retrieval in MPLS, the 12-mm incision site had to be extended in 3- or 4-port LS, and main trocar site was used in 2-port procedure. The ring forceps were used to morcellate the spleen in the endo-bag. If we needed, a closed drain was inserted via the single trocar site in SPLS and via the 5-mm trocar site in MPLS.
Statistical analyses
Data were expressed as mean ± standard deviation. Outcomes using continuous variables were compared by the t-test and categorical data using frequency distributions were compared by the chi-square. All statistical analyses were evaluated by PASW Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA). The statistical significance was set at 0.05.
RESULTS
The characteristics of patients and comparison between the two groups are shown in Table 1. Both groups had similar results with respect to the mean age in the current study. No significant differences were observed between the two procedures with regard to the mean BMI. There was also no significant difference in the radiologic dimension of spleen between the two groups, axial section and coronal section.
Table 1. Patient demographics.
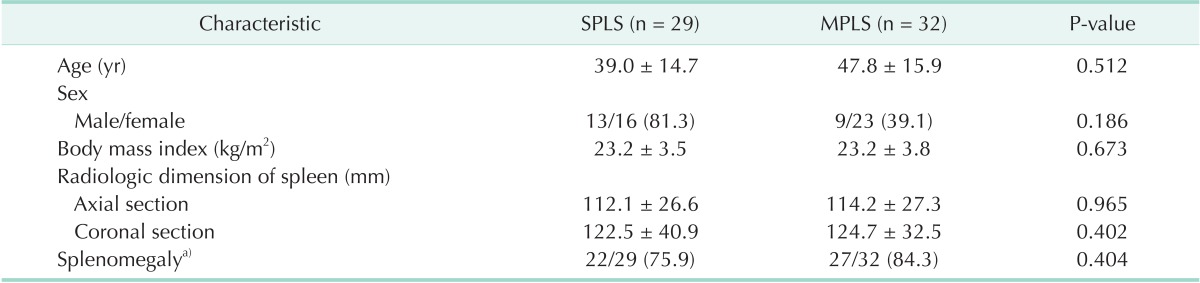
Values are presented as mean±standard deviation or number (%). SPLS, single-port laparoscopic splenectomy; MPLS, multiport laparoscopic splenectomy.
a)Splenomegaly was defined as the spleen having length greater than 9.76 cm by using CT [28].
*P < 0.050, statistically significance.
Diagnosis for splenectomy and types of operation are described in Table 2. Preoperative diagnosis varied from idiopathic thrombocytopenic purpura to benign splenic tumor. The most common indication of SPLS was idiopathic thrombocytopenic purpura and benign splenic tumors were mostly treated by MPLS. Several patients underwent concomitant operation with SPLS and MPLS. One patient underwent cholecystectomy with SPLS and three patients underwent cholecystectomy with MPLS. Gastric varix ligation, gynecologic procedure, pancreatectomy, nephrectomy and lymph node biopsy were carried out concomitantly with MPLS. The rate of partial splenectomy and concomitant operation were significantly higher in MPLS than SPLS.
Table 2. Diagnosis for splenectomy and types of operation.
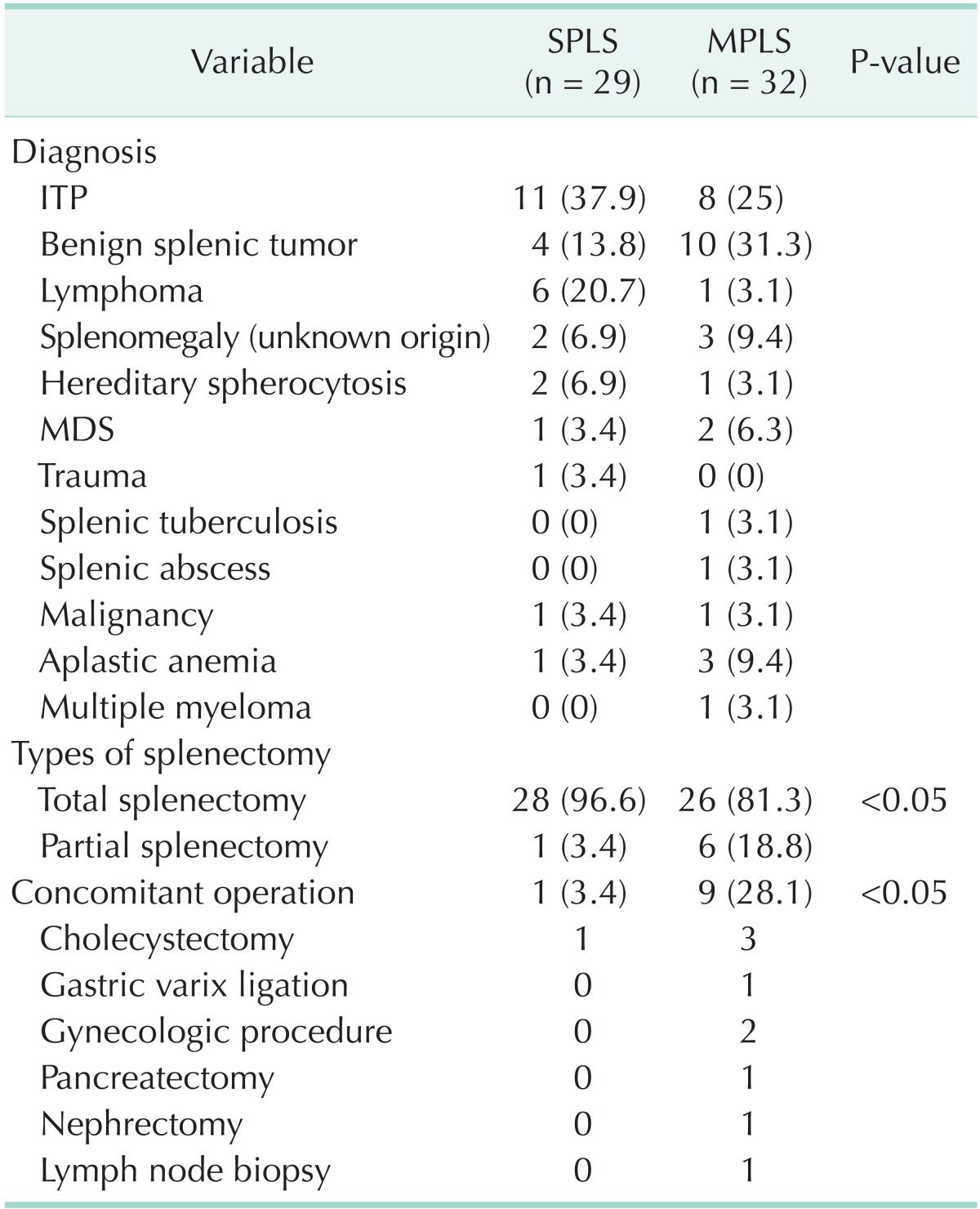
Values are presented as number (%).
SPLS, single-port laparoscopic splenectomy; MPLS, multiport laparoscopic splenectomy; ITP, idiopathic thrombocytopenic purpura; MDS, myelodysplastic syndrome.
The operative outcomes are described in the Table 3. The mean operating time was not longer in SPLS than MPLS. In terms of the mean EBL, the result of SPLS was comparable with the outcomes of MPLS. The length of hospital stay was not significantly different between the SPLS and MPLS groups. We had experienced two cases of adding trocars during SPLS, because of enlarged spleen. And laparotomic conversion took place in each case in both groups due to bleeding.
Table 3. Operative outcomes of SPLS and MPLS.
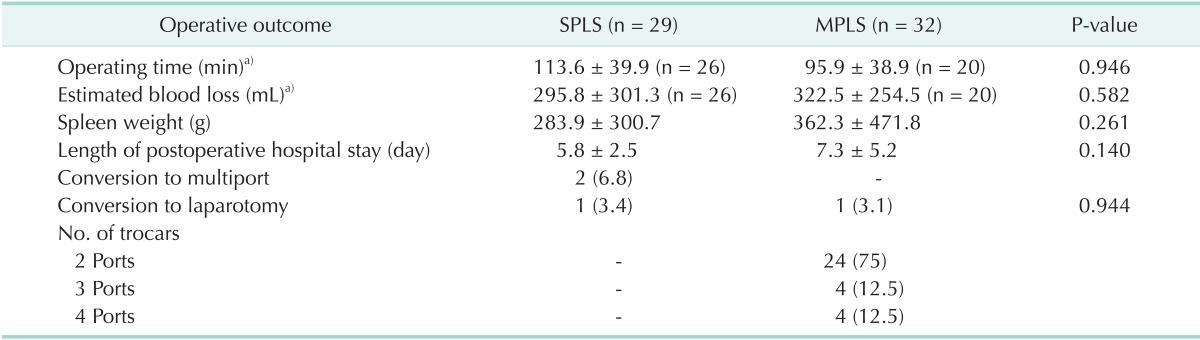
Values are presented as mean±standard deviation or number (%).
SPLS, single-port laparoscopic splenectomy; MPLS, multiport laparoscopic splenectomy.
a)Partial splenectomy and concomitant operative cases are excluded in the operating time and estimated blood loss.
The complications of both groups are given in Table 4. There was no intraoperative complication in the MPLS group but one gastric tearing was encountered in the SPLS group, which was successfully treated with endovascular stapler (gastrointestinal anastomosis [GIA]) stapling during the operation. Postoperative complications occurred in one patient after SPLS compared with three patients in the MPLS. Atelectasis was observed in one case in the SPLS group. In the MPLS group, central intravenous line infection in the postoperative period took place in one patient. Postoperative bleeding occurred in one patient who underwent MPLS and this patient received nephrectomy concomitantly and expired due to bleeding of nephrectomy site. This patient was admitted to Urology and received postoperative care by a urologist. This was the only mortality case among both groups. One patient of the MPLS group suffered from pleural effusion that was successfully managed with transpleural catheter drainage.
Table 4. Comparison of complications.
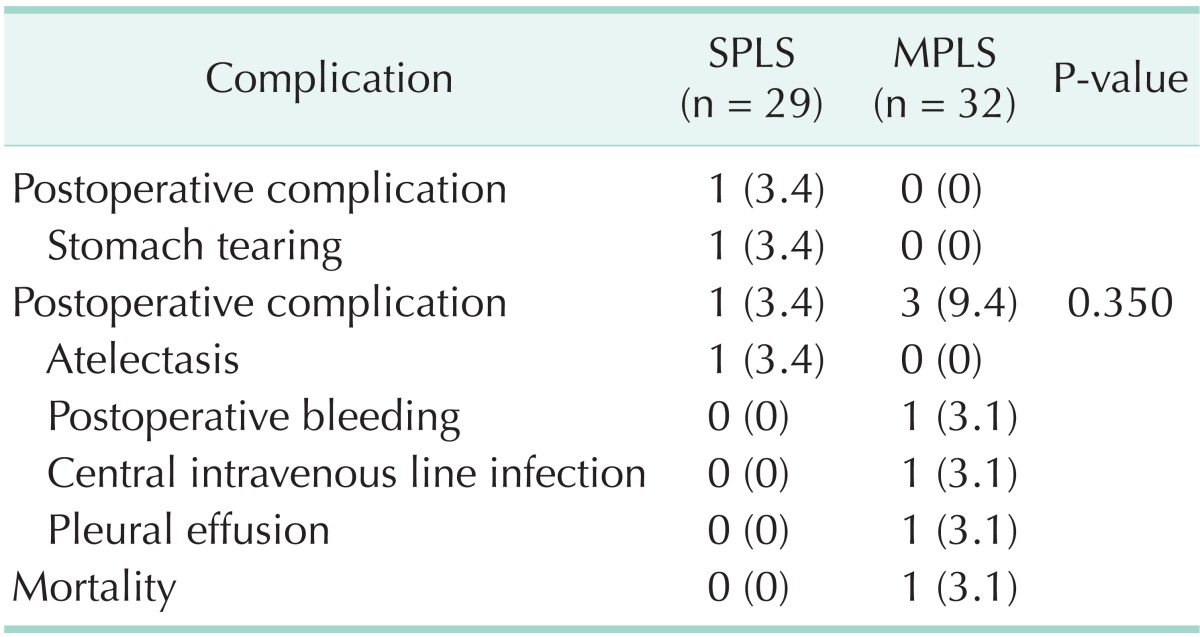
Values are presented as number (%).
SPLS, single-port laparoscopic splenectomy; MPLS, multiport laparoscopic splenectomy.
DISCUSSION
Recently, laparoscopic surgery aiming for minimally invasive technique has increased with some surgeons [18,19,20]. As the techniques and instruments have developed, more surgeons have performed laparoscopic surgery with less numbers of trocars for better postoperative outcomes such as cosmesis, economic advantage, and less pain [21,22]. On the basis of these advantages, some surgeons have attempted to apply laparoscopic single-port surgery for various types of abdominal surgery [23,24,25].
With the above-mentioned advantages, SPLS might provide patients with early recovery and ambulation and, thus, is expected to reduce the length of hospital stay. In this report, the hospital stay in the SPLS group was shorter than that in the MPLS group even there was no statistical significance. Hospital stay was influenced by concomitant surgical procedures and number of partial splenectomies in the current study. It is controversial that total days of hospital stay were considered a result of surgical outcome. This is because influential factors, such as medical insurance, differ from country to country.
On the contrary, the disadvantage of SPLS can be thought to be the difficulty in the use of operational techniques due to a clash among operational instruments in the multichannel port. It is deemed that MPLS can overcome this defect since two hands are free to use in this surgery with more than 2 ports. Despite the theoretical disadvantage, we did not observe any difference in operation time between the two groups. And EBL was lower in SPLS than MPLS, but not statistically significant. According to these results, we could anticipate that surgical difficulties of SPLS would not have a significant effect on the operative results.
In addition, in the comparison of complications, there was 1 case of stomach tearing in SPLS while no such complication was reported during the operation in MPLS. This injury occurred in the first case of SPLS. It was a perforation of the gastric fundus area during GIA stapling of splenic hilum. And it was treated immediately by additional GIA stapling without problems. For postoperative complication, in SPLS, there was 1 case of atelectasis, whereas in MPLS, we observed 3 cases of complications with postoperative bleeding, central venous catheter infection, and pleural effusion for each case. Among them, postoperative bleeding was from nephrectomy rather than from splenectomy. Unfortunately, the number of patients was so small that these results had no statistical significance. We should enroll more patients for the next studies to make conclusions about the comparison of complications between the procedures.
In the comparison of characteristics between the groups with two different surgeries, there was no statistical difference in BMI, spleen size, and spleen weights. Although this study was not a random trial, we could expect that SPLS could be applied to patients regardless of characteristics or spleen size. Of course, randomly prospective studies are required to prove this hypothesis.
Comparing the results of this thesis on 3 cases of early SPLS performed in our center and this study [26], duration of operation was reduced to 113.6 ± 39.9 minutes and there was no intraoperative complication except the first case in the above journal. As mentioned in the preceding journal, there was difficulty in the operation because there was no proper angle for the instruments during the dissection of uppermost part of spleen in SPLS. However, because of the flexible GIA stapler and greater dissecting curvature of the stomach, the SPLS was conducted effectively with no complication and was applied to cholecystectomy or partial splenectomy without any other problems. This implies that SPLS has enough safety and feasibility as a result of development of techniques and instruments.
We could see that a majority of MPLS operations were conducted in 2 ports. The operational difference between 2-port LS and SPLS is whether there is an additional 5-mm trocar. According to the results of comparison study between single port laparoscopic surgery and multiport laparoscopic surgery [27], we could conclude that single-port has a shorter total incision length and offers more aesthetic and economic benefits than multiport. Based on above grounds, SPLS offers better economic and aesthetic effects than 2-port LS since it has one less (number of) trocar.
The limitation of this study is as follows; Firstly, this is a retrospective, nonrandomized study based on a small number of patients. If we collect randomized prospective data over a long period of time in the direction we predicted in the discussion, a more obvious result can be drawn out. Secondly, this study did not conduct research on aesthetic satisfaction and pain, which are subjective results of patients. Thus, comparison of subjective results between the method of MPLS and SPLS is required by conducting both prospective study and questionnaire survey on patients after the operations. Lastly, there was no difference in the operative results between SPLS and MPLS since the operators of this study are from a highly experienced group in laparoscopic surgery. Therefore, in order to compare the technical difficulty of the two operations for beginners in laparoscopic surgery, acomparison should be made on the splenectomies of less experienced operators in the center in order to draw conclusion on the hypothesis.
Footnotes
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Delaitre B, Maignien B. Splenectomy by the laparoscopic approach: report of a case. Presse Med. 1991;20:2263. [PubMed] [Google Scholar]
- 2.Habermalz B, Sauerland S, Decker G, Delaitre B, Gigot JF, Leandros E, et al. Laparoscopic splenectomy: the clinical practice guidelines of the European Association for Endoscopic Surgery (EAES) Surg Endosc. 2008;22:821–848. doi: 10.1007/s00464-007-9735-5. [DOI] [PubMed] [Google Scholar]
- 3.Knauer EM, Ailawadi G, Yahanda A, Obermeyer RJ, Millie MP, Ojeda H, et al. 101 laparoscopic splenectomies for the treatment of benign and malignant hematologic disorders. Am J Surg. 2003;186:500–504. doi: 10.1016/j.amjsurg.2003.07.026. [DOI] [PubMed] [Google Scholar]
- 4.Schlachta CM, Poulin EC, Mamazza J. Laparoscopic splenectomy for hematologic malignancies. Surg Endosc. 1999;13:865–868. doi: 10.1007/s004649901121. [DOI] [PubMed] [Google Scholar]
- 5.Sharma D, Shukla VK. Laparoscopic splenectomy: 16 years since Delaitre with review of current literature. Surg Laparosc Endosc Percutan Tech. 2009;19:190–194. doi: 10.1097/SLE.0b013e3181a5a911. [DOI] [PubMed] [Google Scholar]
- 6.Feldman LS. Laparoscopic splenectomy: standardized approach. World J Surg. 2011;35:1487–1495. doi: 10.1007/s00268-011-1059-x. [DOI] [PubMed] [Google Scholar]
- 7.Carroll BJ, Phillips EH, Semel CJ, Fallas M, Morgenstern L. Laparoscopic splenectomy. Surg Endosc. 1992;6:183–185. doi: 10.1007/BF02210877. [DOI] [PubMed] [Google Scholar]
- 8.Katkhouda N, Hurwitz MB, Rivera RT, Chandra M, Waldrep DJ, Gugenheim J, et al. Laparoscopic splenectomy: outcome and efficacy in 103 consecutive patients. Ann Surg. 1998;228:568–578. doi: 10.1097/00000658-199810000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sampath S, Meneghetti AT, MacFarlane JK, Nguyen NH, Benny WB, Panton ON. An 18-year review of open and laparoscopic splenectomy for idiopathic thrombocytopenic purpura. Am J Surg. 2007;193:580–583. doi: 10.1016/j.amjsurg.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 10.Brunt LM, Langer JC, Quasebarth MA, Whitman ED. Comparative analysis of laparoscopic versus open splenectomy. Am J Surg. 1996;172:596–599. doi: 10.1016/s0002-9610(96)00241-3. [DOI] [PubMed] [Google Scholar]
- 11.Kercher KW, Matthews BD, Walsh RM, Sing RF, Backus CL, Heniford BT. Laparoscopic splenectomy for massive splenomegaly. Am J Surg. 2002;183:192–196. doi: 10.1016/s0002-9610(01)00874-1. [DOI] [PubMed] [Google Scholar]
- 12.Rosen M, Brody F, Walsh RM, Ponsky J. Hand-assisted laparoscopic splenectomy vs conventional laparoscopic splenectomy in cases of splenomegaly. Arch Surg. 2002;137:1348–1352. doi: 10.1001/archsurg.137.12.1348. [DOI] [PubMed] [Google Scholar]
- 13.Ailawadi G, Yahanda A, Dimick JB, Bedi A, Mulholland MW, Colletti L, et al. Hand-assisted laparoscopic splenectomy in patients with splenomegaly or prior upper abdominal operation. Surgery. 2002;132:689–694. doi: 10.1067/msy.2002.127686. [DOI] [PubMed] [Google Scholar]
- 14.Vatansev C, Ece I., Jr Single incision laparoscopic splenectomy with double port. Surg Laparosc Endosc Percutan Tech. 2009;19:e225–e227. doi: 10.1097/SLE.0b013e3181c4efab. [DOI] [PubMed] [Google Scholar]
- 15.Barbaros U, Dinccag A. Single incision laparoscopic splenectomy: the first two cases. J Gastrointest Surg. 2009;13:1520–1523. doi: 10.1007/s11605-009-0869-8. [DOI] [PubMed] [Google Scholar]
- 16.Dutta S. Early experience with single incision laparoscopic surgery: eliminating the scar from abdominal operations. J Pediatr Surg. 2009;44:1741–1745. doi: 10.1016/j.jpedsurg.2008.12.024. [DOI] [PubMed] [Google Scholar]
- 17.Lagrand R, Kehdy F. Laparoendoscopic single site splenectomy. Am Surg. 2010;76:E158–E159. [PubMed] [Google Scholar]
- 18.Yaghoubian A, Kaji AH, Lee SL. Laparoscopic versus open appendectomy: outcomes analysis. Am Surg. 2012;78:1083–1086. [PubMed] [Google Scholar]
- 19.Steinert R, Nestler G, Sagynaliev E, Muller J, Lippert H, Reymond MA. Laparoscopic cholecystectomy and gallbladder cancer. J Surg Oncol. 2006;93:682–689. doi: 10.1002/jso.20536. [DOI] [PubMed] [Google Scholar]
- 20.Lian L, Kalady M, Geisler D, Kiran RP. Laparoscopic colectomy is safe and leads to a significantly shorter hospital stay for octogenarians. Surg Endosc. 2010;24:2039–2043. doi: 10.1007/s00464-010-0900-x. [DOI] [PubMed] [Google Scholar]
- 21.Kulaylat AN, Podany AB, Hollenbeak CS, Santos MC, Rocourt DV. Transumbilical laparoscopic-assisted appendectomy is associated with lower costs compared to multiport laparoscopic appendectomy. J Pediatr Surg. 2014;49:1508–1512. doi: 10.1016/j.jpedsurg.2014.03.016. [DOI] [PubMed] [Google Scholar]
- 22.Ahn SH, Son SY, Jung DH, Park DJ, Kim HH. Pure single-port laparoscopic distal gastrectomy for early gastric cancer: comparative study with multi-port laparoscopic distal gastrectomy. J Am Coll Surg. 2014;219:933–943. doi: 10.1016/j.jamcollsurg.2014.07.009. [DOI] [PubMed] [Google Scholar]
- 23.Marks JH, Montenegro GA, Shields MV, Frenkel JL, Marks GJ. Single-port laparoscopic colorectal surgery shows equivalent or better outcomes to standard laparoscopic surgery: results of a 190-patient, 7-criterion case-match study. Surg Endosc. 2015;29:1492–1499. doi: 10.1007/s00464-014-3830-1. [DOI] [PubMed] [Google Scholar]
- 24.Maluenda F, Leon J, Csendes A, Burdiles P, Giordano J, Molina M. Single-incision laparoscopic sleeve gastrectomy: initial experience in 20 patients and 2-year follow-up. Eur Surg. 2014;46:32–37. doi: 10.1007/s10353-013-0246-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shetty GS, You YK, Choi HJ, Na GH, Hong TH, Kim DG. Extending the limitations of liver surgery: outcomes of initial human experience in a high-volume center performing single-port laparoscopic liver resection for hepatocellular carcinoma. Surg Endosc. 2012;26:1602–1608. doi: 10.1007/s00464-011-2077-3. [DOI] [PubMed] [Google Scholar]
- 26.You YK, Lee SK, Hong TH, Kim JG. Singleport laparoscopic splenectomy: the first three cases. Asian J Endosc Surg. 2010;3:33–35. [Google Scholar]
- 27.Deie K, Uchida H, Kawashima H, Tanaka Y, Masuko T, Takazawa S. Single-incision laparoscopic-assisted appendectomy in children: exteriorization of the appendix is a key component of a simple and costeffective surgical technique. Pediatr Surg Int. 2013;29:1187–1191. doi: 10.1007/s00383-013-3373-x. [DOI] [PubMed] [Google Scholar]
- 28.Bezerra AS, D'Ippolito G, Faintuch S, Szejnfeld J, Ahmed M. Determination of splenomegaly by CT: is there a place for a single measurement? AJR Am J Roentgenol. 2005;184:1510–1513. doi: 10.2214/ajr.184.5.01841510. [DOI] [PubMed] [Google Scholar]


