Abstract
While outbreaks of infectious diseases have long presented a public health challenge, especially in developing countries like Nigeria; within recent years, the frequency of such outbreaks has risen tremendously. Furthermore, with the recent outbreaks of emerging and re-emerging infectious diseases such as Ebola virus disease and other epidemic prone diseases in Nigeria demanding immediate public health action, there is a need to strengthen the existing notifiable disease surveillance and notification system with increased clinicians’ involvement in timely reporting of notifiable diseases to designated public health authorities for prompt public health action. Hence, this paper provides the opportunity to increase awareness among clinicians on the importance of immediate reporting of notifiable diseases and intensify engagement of clinicians in disease notification activities by describing various notifiable diseases in Nigeria using their surveillance case definition, outlines the reporting channel for notifying these diseases and highlights the roles of clinicians in the current disease surveillance and notification network for early disease outbreak detection and public health response in Nigeria.
Keywords: Clinicians, disease outbreak, Nigeria, notifiable disease surveillance
INTRODUCTION
Disease surveillance is the continuous scrutiny of occurrence of diseases and health-related events to enable prompt intervention for the control of diseases.1 It involves the ongoing systematic collection, collation, analysis and interpretation of data on disease occurrence and public health related events and dissemination of the information obtained from such data for prompt public health action.2,3,4,5,6 However disease notification involves the official and timely reporting of the occurrence of specific diseases and conditions to designated public health authorities by clinicians and other health personnel for action using designated reporting tools.7 Disease notification is an important source of data collection for an effective and efficient disease surveillance system.7 Disease surveillance and notification (DSN) have been recognized as an effective strategy for the prevention and control of diseases most especially epidemic prone diseases. It is crucial to note that disease outbreak do not give notice before its occurrence neither do they respect the borders of nations. When they eventually occur, they are likely to spread like wildfire and often resulting in high morbidity and case fatality rate with consequent economic impact. An effective and efficient disease surveillance and notification system allows early detection of disease outbreaks that will prompt intervention for the reduction of morbidity and mortality that may result from the epidemics of these infectious diseases.8 Levels of disease surveillance and notification can be individual, local, national and international. National disease surveillance and notification system often depends on effective district/Local Government Area (LGA) disease monitoring and control mechanism with the clinicians’ actively involved.1,8
In Nigeria, surveillance and notification of diseases involve the immediate notification of epidemic prone diseases, diseases targeted for elimination and eradication and monthly notification of other diseases of public health importance.2 For a disease surveillance and notification system at the district/LGA level to be functional and effective in early detection of epidemic-prone diseases, clinicians remain indispensable to effective reporting because they can detect unusual disease manifestations and conditions that rely on clinical signs not related to laboratory testing, clusters of illnesses through patient interview and clinical judgments.9
Presently in Nigeria, the collection, collation, analysis and interpretation of disease-related data in public health institutions are often incomplete and untimely partly because of poor awareness among clinicians of the importance of their role in disease surveillance and notification activities for the prevention of infectious disease outbreaks.7 Many outbreaks which have occurred in Nigeria over the years have been attributed to clinicians either not reporting or reporting late when the index cases of epidemic prone diseases present in the various health institutions across the country.10 From previous studies on disease surveillance and notification, it is pertinent to note that failure in mandatory reporting of notifiable diseases among clinicians have been attributed to lack of awareness of the existence of a surveillance network for notifiable diseases including the requirement for reporting, which diseases are notifiable, how, when and to whom reporting should be done.7,11,12,13
This paper therefore seeks to identify opportunities for an increased engagement of clinicians in disease notification activities by describing various notifiable diseases in Nigeria using their surveillance case definitions, outlining the reporting channel for notifiable diseases and highlighting the roles of clinicians in the current disease surveillance and notification network for early disease outbreak detection and public health response in Nigeria.
DISEASE URVEILLANCE AND NOTIFICATION IN NIGERIA: AN OVERVIEW
Disease surveillance and notification was introduced in Nigeria in 1988 following a major outbreak of yellow fever in 1986/87 which claimed many lives in the country and also affected ten out of the then 19 states of the country.7 Prior to that time, there was no coordinated system of disease reporting and surveillance in the country, as some states were sending weekly, some were sending annual report and others not sending at all. This became a major cause for concern as it resulted in denied access to health information needed for timely response to disease outbreaks.7 As a result, the National Task Force on Epidemic control was set up to find a lasting solution to disease notification in the country. The National Task Force identified poor disease surveillance and notification as a major national problem and as an important constraint to effective disease control in Nigeria.7 At the onset of its establishment, 42 diseases were officially designated as notifiable for routinely monthly reporting which was later reviewed to 22 in 1998.2 The current DSN system in Nigeria was approved for adoption by the Nigerian National Council on Health in 1989.1 In September 1998, the 48[th] World Health Organization Regional Committee for Africa met in Harare, Zimbabwe with the resolution of all member States (Reference document; AFRO/RC48/R2) adopting the Integrated Disease Surveillance and Response (IDSR) as a regional strategy for strengthening the weak national disease surveillance system in the African region. The aim of the scheme is to integrate multiple surveillance system for enhance early detection of outbreaks of diseases in the Africa so that human and other resources can be used more efficiently and effectively.14,15,16,17
INTEGRATED DISEASE SURVEILLANCE AND RESPONSE AND NOTIFIABLE DISEASES IN NIGERIA
Integrated Disease Surveillance and Response (IDSR) is a strategy and a tool to promote rational use of resources by integrating and streamlining common disease surveillance activities. Prior to the adoption and implementation of IDSR system in Nigeria, many disease control and intervention programmes still rely on their own disease surveillance system making efforts to improve their ability to obtain reliable and timely data in order to use information for taking action.2 But, it is paramount to note that disease control and prevention objectives are successfully achieved when available resources are dedicated to improving the ability of health officials to detect the targeted diseases, obtain laboratory confirmation of these diseases and use threshold to initiate action.2 After the adoption by the World Health Organization (WHO), African region of the Integrated Disease Surveillance and Response (IDSR) strategy as a regional strategy for disease control in 1998, Nigeria, commenced efforts towards implementation of the IDSR strategy in June 2000 with an orientation workshop held to sensitize national programme managers of vertical programs and partners on IDSR. In January 2001, a steering committee on IDSR was inaugurated to steer the implementation process. All the 36 states in the Federation, including the Federal Capital Territory are currently implementing IDSR.17
The Integrated Disease Surveillance system seeks to ensure that effective and functional IDSR system is available at each level of the health system, from health facilities to Local Government Areas (LGAs), states and at the national level. IDSR focuses on the LGA level where information generated is used for timely action consequently leading to reduction of morbidity, disability and mortality.2,18 A country where IDSR is functional is expected to use standard IDSR case definitions to identify and report notifiable diseases; collect and use surveillance data to alert higher levels and trigger local action; investigate and confirm suspected outbreaks or public health events using laboratory confirmation, when indicated; analyze and interpret data collected in outbreak investigation and from routine monitoring of other notifiable diseases; use information from the data analysis to implement an appropriate response; provide feedback within and across levels of the health care system and evaluate and improve the performance of surveillance and response system.2,19 The present IDSR strategy in Nigeria is well coordinated and combines available resources to collect information on notifiable diseases from a single focal point at each level (Community, health facilities, LGA, State and Federal) compared to the previous vertical disease surveillance system where scarce resources are divided among several disease control programmes.2 Also, it is important to note that the LGA level is the main focus in the IDSR system in Nigeria because it is the first level in the Nigerian health system with full time staff dedicated to all aspect of the health of the public such as monitoring health events in the community, mobilizing community action and accessing regional resources to protect the health of communities.2
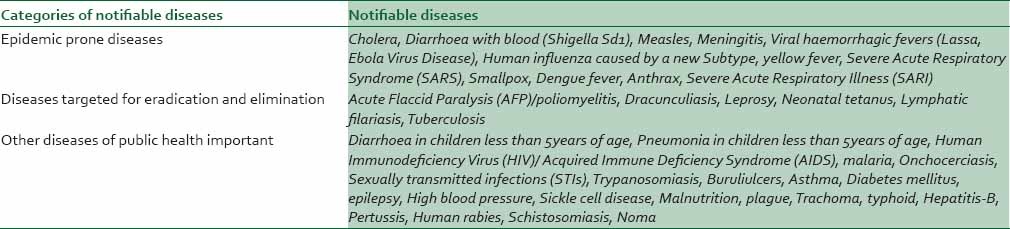
The Federal Ministry of Health (FMoH) have selected 40 communicable and non-communicable diseases and public health related conditions for the IDSR system in Nigeria. These diseases were selected based on the following; top cause of high morbidity and mortality in the country, have epidemic potential, surveillance required internationally, availability of effective control and preventive intervention for addressing the public health problem they pose, could be easily identified using simple case definition and have intervention programmes supported by the WHO for prevention and control, eradication or elimination of the diseases.2 These diseases have been grouped into three categories; epidemic prone diseases, diseases targeted for eradication and elimination and other diseases of public health importance as shown in Table 1. However, it is crucial to note that this current list of the Nigeria IDSR notifiable diseases, conditions and public health events are subjected to review hence clinicians are encouraged to look out for the revised IDSR guidelines which when published are expected to be circulated to all health institutions and parastatals in the country.
Table 1.
List of Nigeria Integrated Disease Surveillance and Response (IDSR) notifiable diseases, conditions and public health events
FLOW OF IDSR DATA, IDSR REPORTING FORMS AND NOTIFIABLE DISEASES REPORTING PROCEDURE IN NIGERIA
The flow of information in the IDSR system in Nigeria is from the health facility, where diseases that have epidemic potential and those which are targeted for eradication and elimination, are reported immediately to the focal persons in the health facility and thereafter to the LGA using designated IDSR reporting forms [Figures 1 and 2]. The LGA receive data from the health facilities, collate and send to the next level which is the State Ministry of Health (SMoH).2,19
Figure 1.
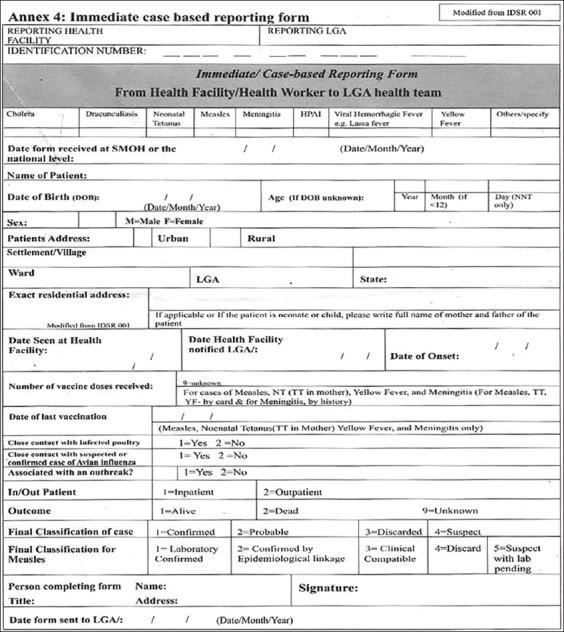
The Integrated Disease Surveillance and Response (IDSR) 001A form-immediate case-based reporting form for immediate reporting of notifiable diseases (it should be noted that this form is sent immediately to the Local Government Area (LGA) Disease Surveillance and Notification Officer at the LGA Primary Health Care Department) after completion for prompt action2
Figure 2.
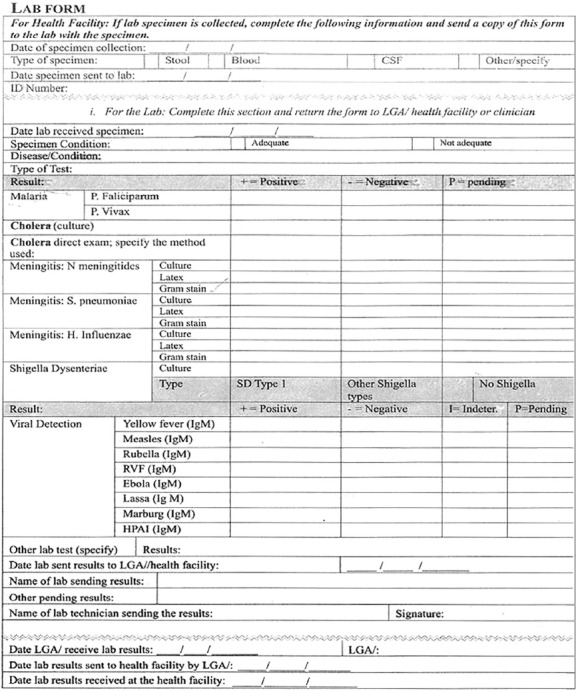
The Integrated Disease Surveillance and Response (IDSR) 001B form-Lab request form for immediate reporting of notifiablediseases2
At the LGA level, analysis and feedback to health facilities is expected to be done. The Epidemiology unit of the SMoH collates data from the LGAs and forwards it to the Epidemiology Division of the Federal Ministry of Health (FMoH).2,19 At the SMoH, analysis and feedback to the health facilities and public is done as well as planning appropriate operations and strategies for disease control.2,19
At the FMoH, data is collated and forwarded to the statistics division, analysis and feedback is carried out, as well as planning for appropriate intervention based upon the results of analysis [Figure 3].
Figure 3.
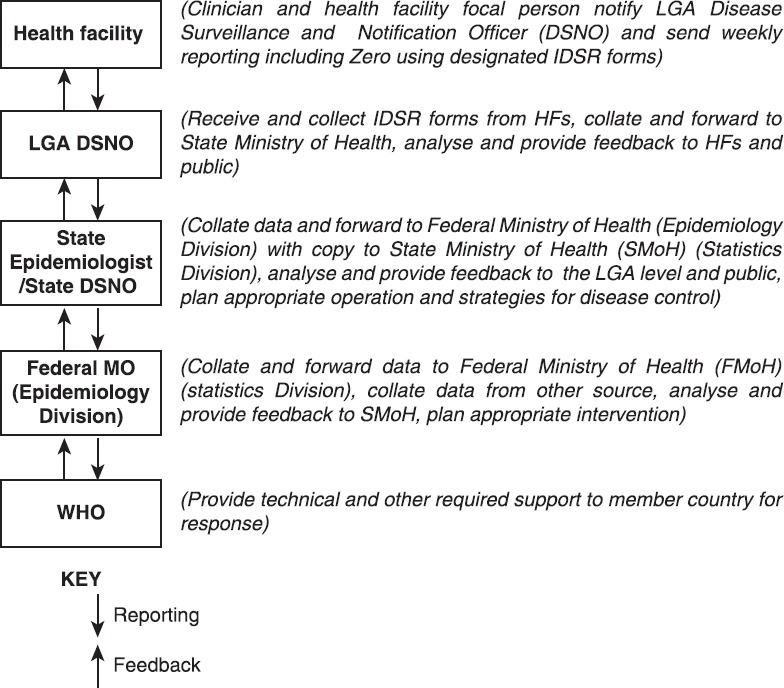
Flow of Integrated Disease Surveillance and Response (IDSR) data in Nigeria2
The flow of data in the IDSR system begins with the detection and immediate notification of notifiable diseases seen at the health facility by clinicians to the LGA Disease Surveillance and Notification Officers (DSNO) at the LGA Department of Primary Health Care (PHC) which serves as a link between the health facility/communities and other levels of the IDSR network in Nigeria.2,20
The current IDSR guideline which has been published and widely circulated in the country mandates clinicians to immediately notify suspected cases of epidemic prone diseases and diseases targeted for eradication and elimination using surveillance case definition and the designated IDSR reporting forms [Table 2] to the LGA Disease Surveillance and Notification Officers (DSNO) at the Primary Health Care Department of each LGA in the country [Figure 3] for onward reporting to State and Federal public health authorities for prompt action.2,20
Table 2.
The Integrated Disease Surveillance and Response (IDSR) reporting forms and their uses2
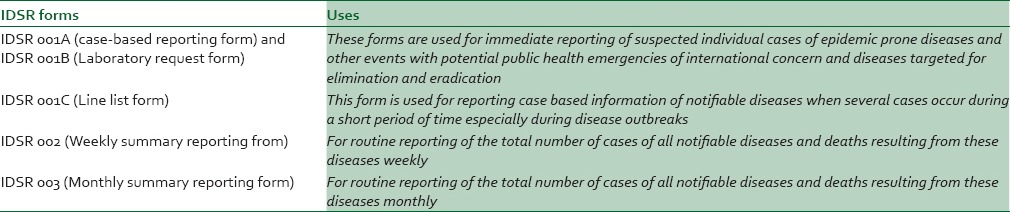
For timely and accurate information to be collected from suspected cases of notifiable diseases in order to achieve surveillance objectives, reporting forms have been simplified under the IDSR system to aid clinicians in the notification of these diseases. The IDSR forms [Figures 1 and 2] and their uses are presented in Table 2 below.
DISEASE SURVEILLANCE AND NOTIFICATION AS A TOOL FOR DISEASE OUTBREAK PREVENTION AND CONTROL IN NIGERIA
Early detection of outbreaks is necessary for effective and rapid control.21 One of the primary goals of a functional disease surveillance and notification system among others is to detect and monitor diseases and other events with potential threat to the health of the public with respect to source, time, person, population and place in order to provide rationale for public health action. This key goal of disease surveillance and notification has made it an effective tool for disease outbreak prevention and control. The fundamental objective of a functional national disease surveillance and notification system is early recognition and detection of infectious diseases as it provides the opportunity for timely public health action and minimises the number of people infected with the disease.22
Prompt reporting of cases of infectious diseases and other events of potential public health threat could prevent potential outbreaks which would result in high rate of morbidity and mortality. For example, the few cases and deaths from Ebola virus disease (EVD) recorded in Nigeria during the EVD outbreak from July to September, 2014 could be attributed to the prompt reporting of the imported case of EVD by the attending clinicians in Lagos-Nigeria to designated public health authorities which sprang up appropriate response that led to the quick containment of the outbreak.
In order to illustrate the importance of immediate reporting of notifiable diseases for outbreak prevention and control, let's consider two scenarios; the first scenario involving delayed reporting of an infectious disease [Figure 4] and the other scenario early reporting of an infectious disease [Figure 5]. From Figure 4, it is clear that when the reporting of suspected cases of infectious diseases and other events of potential threats to the health of the public are delayed by clinicians, the opportunity of spread is high while the opportunity to institute an effective control measure is minimal with few incident cases and deaths likely to be averted. On the other hand, Figure 5 illustrates the impact of early and immediate reporting of infectious diseases on disease outbreak prevention and control where a higher proportion of potential cases and deaths are likely to be averted.
Figure 4.
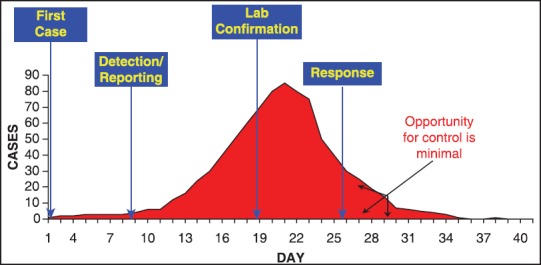
Impact of delayed reporting of infectious diseases by clinicians on disease outbreak control and prevention
Figure 5.
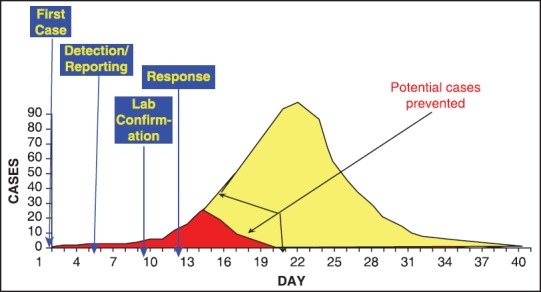
Impact of early reporting of infectious diseases by clinicians on disease outbreak control and prevention
THE ROLES OF CLINICIANS IN NOTIFIABLE DISEASE REPORTING
For the existing disease surveillance and notification system in Nigeria to be effective for infectious disease outbreak prevention and control, especially at the LGA level, clinicians remains indispensable to the system because they can detect unusual disease manifestations and conditions that rely on clinical signs through patient interview and clinical diagnosis.9 The roles of clinicians in ensuring a functional and responsive disease surveillance and notification system in Nigeria are outlined as follows:
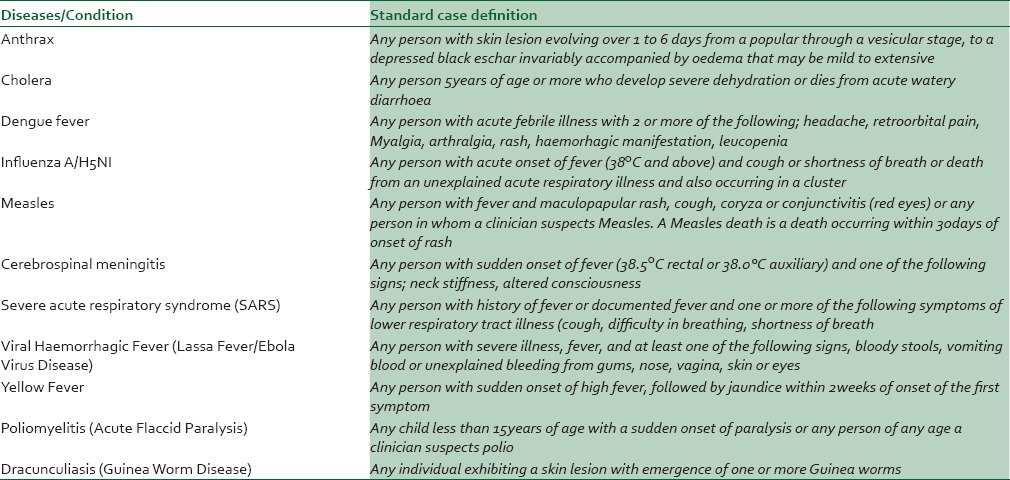
Detection of suspected cases of notifiable diseases for laboratory confirmation using the epidemiological surveillance standard case definition and differential diagnosis as stipulated in the national technical guideline [Table 3].
Immediate reporting of detected cases to designated local public health surveillance officers (LGA DSNO) for investigation including the collection of specimen for laboratory analysis.2,20
Provide support to designated LGA surveillance officers during case investigation to ensure adequate samples are collected from the reported cases to ensure accurate laboratory analysis.
Case management using the recommended treatment protocol especially as specified in the national technical guideline.2,23,24
Table 3.
World Health Organization and Federal Ministry of Health recommended surveillance case definition for immediate reporting of selected notifiable diseases2
CONCLUSION
Clinicians who are frequently the first contact a patient has with the healthcare system, may find themselves identifying the presence of infectious diseases, tracking and identifying cases and notifying designated public health authorities. Also, implementing disease containment programs as the first line of detection of an infectious disease agent in a population reside with a clinician who diagnoses an individual with signs and symptoms of that disease. Hence, in remaining vigilant for the presence of these infectious diseases, clinicians must function as ‘disease detectives’ in the present IDSR system in Nigeria. Most importantly, clinicians must understand they are critical component of the national notifiable disease and public health surveillance system in Nigeria. In this view, clinicians in Nigeria should be familiar with basic concepts of the IDSR system in order to be prepared to recognize and respond to all disease outbreaks in a timely manner.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Buehler JW, Hopkins RS, Overhage JM, Sosin DM, Tong V. CDC Working Group. Framework for evaluating public health surveillance systems for early detection of outbreaks. Recommendations from the Centre for Disease Control and Prevention Working Group. MMWR Recomm Rep. 2004;53:1–11. [PubMed] [Google Scholar]
- 2.Federal Ministry of Health. National technical guidelines for integrated diseases surveillance and response. Abuja: Federal Ministry of Health; 2009. pp. 2–69. [Google Scholar]
- 3.Eylenbosch WJ, Noah ND. Historical aspects. In: Eylenbosch WJ, Noah ND, editors. Surveillance in Health and Disease. Oxford: Oxford University Press; 1988. pp. 1–3. [Google Scholar]
- 4.Heymann DL, editor. Control of Communicable Diseases Manual. 18th ed. Washington: America Public Health Association; 2004. pp. 103–14. [Google Scholar]
- 5.Last JM, editor. A Dictionary of Epidemiology. 4th ed. Oxford: Oxford University Press; 2001. p. 61. [Google Scholar]
- 6.Bonita R, Beaglhole T, Kjellström T, editors. Basic epidemiology. 2nd ed. Geneva: World Health Organization press; 2006. pp. 127–31. [Google Scholar]
- 7.Abdulraheem IS, Monehin OJ, Akanbi AA, Onajole AT, Bamgbala AO. Disease notification among physicians in a Nigerian Tertiary Health Institution. Niger Med Pract. 2004;45:111–5. [Google Scholar]
- 8.Dairo MD, Bamidele JO, Adebimpe WO. Disease surveillance and reporting in two Southwestern States in Nigeria; Logistic challenges and prospect. J Public Health Epidemiol. 2010;2:126–9. [Google Scholar]
- 9.McClean CM, Silk BJ, Buehler JM, Berkelman RL. Disease reporting among Georgiaphysicians and laboratories. J Public Health Manag Pract. 2010;16:535–43. doi: 10.1097/PHH.0b013e3181cb4324. [DOI] [PubMed] [Google Scholar]
- 10.Osibogun A, Jaekie Z, Idowu JA, Alausa OK, Oluwole FA. For better data, better utilized. World Health Forum. 1996;17:274–6. [PubMed] [Google Scholar]
- 11.Ofili AN, Ugwu EN, Ziregbe A, Richards R, Salami S. Knowledge of disease notification among doctors in government hospitals in Benin City, Edo State, Nigeria. Public Health. 2003;117:214–7. doi: 10.1016/S0033-3506(02)00021-5. [DOI] [PubMed] [Google Scholar]
- 12.AbdoolKarim SS, Dilray A. Reasons for underreporting of notifiable conditions. S Afr Med J. 1996;86:834–6. [PubMed] [Google Scholar]
- 13.Friedman SM, Sommersall LA, Mgardam MD, Arenovich T. Suboptimal reporting of notifiable diseases in Canadian emergency departments: A survey of emergency physicianknowledge, practices and perceived barriers. Can Commun Dis Rep. 2006;32:187–98. [PubMed] [Google Scholar]
- 14.Franco LM, Setzer J, Banke K. Improving performance of IDSR at district and facility levels: Experiences in Tanzania and Ghana in making IDSR operational. Bethesda, MD: The partners for reform plus project. Abt Associates; 2006. pp. 13–5. [Google Scholar]
- 15.Nsubuga P, Eseko N, Tadesse W, Ndayimirije N, Stella C, McNabb S. Structure and performance of infectious disease surveillance and response, United Republic of Tanzania,1998. Bull World Health Organ. 2002;80:196–203. [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization. An Integrated approach to communicable disease surveillance. [Last accessed on 2014 Oct 3];Wkly Epidemiol Rec. 2000 75:1–8. Available from: http://www.who.int/docstore/wer/pdf/2000/wer7501.pdf . [Google Scholar]
- 17.Federal Ministry of Health (FMoH) National policy on Integrated Disease Surveillance Response in Nigeria. Abuja: Federal Ministry of Health; 2005. [Last accessed on 2015 May 14]. pp. 1–7. Available from: http://cheld.org/wp-content/uploads/2012/04/National-Policy-on-Integrated-Disease-Surveillance-and-Response.pdf . [Google Scholar]
- 18.Kasolo F, Roungou JB, Perry H. Technical guidelines for Integrated Disease Surveillance and response in the African region. 2nd edition. 2010. [Last accessed on 2015 Feb 26]. Available from: http://www.cdc.gov/globalhealth/dphswd/idsr/pdf/Technical%20Guidelines/IDSR%20Technical%20Guidelines%202nd%20Edition_2010_English.pdf .
- 19.Abubakar AA, Sambo MN, Idris SH, Sabitu K, Nguku P. Assessment of integrated disease surveillance and response strategy implementation in selected Local Government Areas of Kaduna state. Ann Niger Med. 2013;7:14–9. [Google Scholar]
- 20.Isere EE, Fatiregun AA. Measles case-based surveillance and outbreak response in Nigeria; an update for clinicians and public health professionals. Ann Ib Postgrad Med. 2014;12:15–21. [PMC free article] [PubMed] [Google Scholar]
- 21.Duric P, Ilic S. Participation of infectious disease surveillance in primary health care. Sri Lanka J Infect Dis. 2012;2:37–46. [Google Scholar]
- 22.Veenema T, Tõke J. Early Detection and Surveillance for Biopreparedness and Emerging Infectious Diseases. Online J Issues Nurs. 2006. [Last accessed 2014 on Sept 24]. p. 11. Available from: http://www.nursingworld.org/mainmenucategorie . [PubMed]
- 23.Technical guideline for acute flaccid paralysis surveillance inNigeria. Abuja: Federal Ministry of Health; 2012. Federal Ministry of Health; pp. 35–37. [Google Scholar]
- 24.Guideline for measles surveillance and outbreak response in Nigeria. Abuja: Federal Ministry of Health; 2012. Federal Ministry of Health; pp. 10–11. [Google Scholar]


