Abstract
Background:
Early detection of breast cancer plays an important role in decreasing its morbidity and mortality. This study therefore examines the factors influencing breast self-examination (BSE) awareness and practices among women in Ogun state, Western Nigeria.
Materials and Methods:
This analytical cross-sectional study was conducted between 22 April and 13 May 2013 using a semi- structured questionnaire. A multi-stage cluster sampling technique was used to select one participant per household into the study.
Results:
A total of 495 women were interviewed in this study, the mean age of the respondents was 36.45 ± 5.12 years. About half (58.2%) of respondents have heard of BSE and 24.4% have ever perform BSE. Only 5.3% of our respondents perform BSE regularly (monthly) as recommended. Barrier to non-performance of BSE were perception of not being at risk (47.6%), lack of knowledge of how to perform BSE (47.6%). Only 18.5% of respondents have ever had their breast examined by physicians for lump and all of them had continued to perform BSE afterwards. The only predictor of awareness and practice of breast self-examination was tertiary level of education [odds ratio (OR) = 1.43 cumulative incidence (CI) = 1.12-2.18].
Conclusion:
The study shows level of education, smoking habits and history of breast exam by health professional and were the factors found associated with BSE practice. Training on BSE should be given to women especially during antenatal care in order to increase the practice of BSE thus averting the severe morbidity and mortality of breast cancer in developing countries.
Keywords: Breast, Nigeria, reproductive age, rural, self-examination
INTRODUCTION
One of the best ways to early detection of breast cancer is screening.1 The best acceptable ways of screening for the breast cancer are breast self-examination (BSE), clinical examination by the physicians or healthcare providers (Clinical Breast Examination), mammography and magnetic resonance imaging.2 BSE from economical and human viewpoints has many benefits in comparison to two other methods, because it can be performed without any cost and is available everywhere.3 Surveys show that performing continuous BSE causes a decrease rate of 3.1% in breast cancer cases with interfacing axillary lymph.4 Breast cancer is the leading female malignancy in the world accounting for 19% of all female cancers and the leading cause of cancer-related death in women.5,6 In 2010, nearly 1.6 million women worldwide were diagnosed with breast cancer, accounting for approximately 14% of the cancer deaths in women and 35% of all cancer cases. Nowadays, the cancer is the second cause of death throughout the world.6,7 The breast cancer is the most organ cancer among the women and the first cause of death among the women in the age of 40-45 years.7
Early detection of breast cancer plays an important role in decreasing its morbidity and mortality. Though BSE is one of the screening methods for early detection of breast cancer,8 early diagnosis of breast cancer is known to be vital to the treatment of the disease and the reduction in cancer deaths. The efficacy of BSE is usually tested with the help of mammography.9 Also, in terms of feasibility, the mammography screening method is inaccessible for many countries for financial reasons. In contrast, BSE is a simple, low-priced, secure, effective, appropriate and feasible diagnostic procedure for developing countries when compared with mammography and clinical breast examination.10
MATERIALS AND METHODS
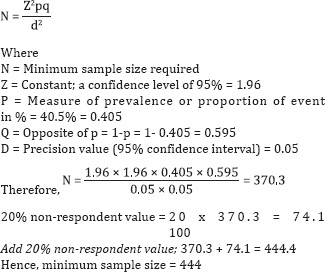
This was a stratified randomised, questionnaire-based study on mammography awareness among women in a rural set-up in southwestern Nigeria, between 22 April and 13 May 2013. Using the formula below, the estimated sample size was 444. Sample size estimation was based on the formula:
Ethical clearance was duly obtained and only participants who gave informed consent were recruited in the study. The data were processed and analysed using statistical package of social sciences (SPSS) 15 statistical software. Percentages or means and standard deviation were computed for baseline characteristics of women interviewed. The data analysis focused on univariate frequency table and bivariate cross tabulations that identify important relationships between variables.
The relationships between variables were examined through bivariate analysis, by computing odds ratio at 95% confidence level and chi squared and t-tests where appropriate. Predictor variables were restricted to outcome measures that were statistically significant. A P-value ≤ 0.05 or confidence limits which did not embrace unity (1) was considered as statistical significance.
RESULTS
A total of 495 women were interviewed in this study. The mean age of the respondents were 36.45 ± 5.12 years. Half [57.5%] of the respondents had tertiary education, 5.4% had no formal education, 12.8% had only primary education, while 24.3% had secondary education.
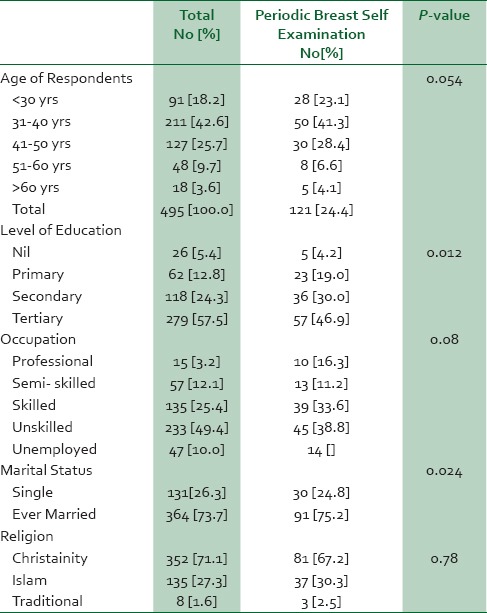
Those employed in unskilled settings were 49.4%, semi-skilled 12.1%, skilled 25.4%, unemployed 10.0% and 3.2% of respondents were professionals. Majority [68.0%] were married, 26.3% were never married, 1.0% were divorced and 4.7% were separated. Furthermore, 85.3% were in a monogamous marriage while 14.7% in a polygamous marriage. Most [71.1%] of the respondents were Christians, 27.3% were Muslims while 1.6% were traditional religion worshippers. Multi-parous women made up 48.1% of the respondents, primiparous women 35.2% and nulliparous women 16.8%. This is shown in Table 1 below.
Table 1.
Socio-dermographic characteristics and breast self examination
The mean age of menarche of our respondents was 15.53 ± 7.64 years. The mean age of first birth was 24.4 ± 4.53 years. The mean number of children given birth to was 3.3 ± 2.1 years. The mean duration of breastfeeding among respondents was 1.42 ± 3.16 years.
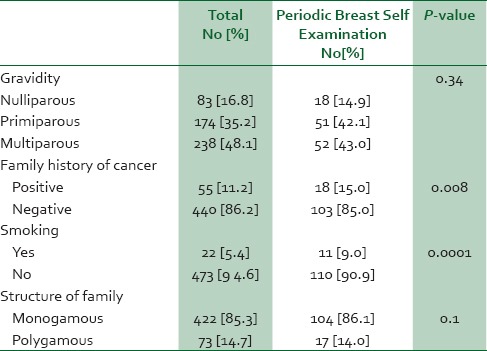
Majority (95.6%) were non-smokers, with only 4.4% as smokers. Of the 4.4% of smokers, the average pack year was 2 pack years. Only 24.5% used contraceptives while 75.5% did not acknowledge any oestrogen-containing contraceptive use. Majority at 85.7% have no family history of breast lesions while only 14.3% had a family history of such. Of those that had a family history of breast lesions, 50% were to second degree relatives, 28.6% to third-degree relatives while 21.4% were to first-degree relatives. This is shown in Table 2.
Table 2.
Other factors influencing breast self examination
About half (58.2%) of respondents have heard of self-breast examination while 41.8% have not heard of it. Of those aware of BSE, 36.1% responded that only women should perform it, 36.1% responded both men and women should perform it while 27.8% did not know. And, 44.1% did not know at what age BSE should be performed, 36.4% replied as above 19 years of age while 19.5% replied as below 19 years of age.
Few (24.4%) of the respondents have ever perform BSE. Only 5.3% of our respondents perform BSE regularly (monthly) as recommended. Of those that were aware of BSE, barrier to non performance of BSE were perception of not being at risk (47.6%), lack of knowledge of how to perform BSE (47.6%) while 2.4% did not because of a lack of time and 2.4% did not because they were too old.
Only 18.5% of respondents have ever had their breast examined by physicians for lump and all of them had continued to perform BSE. This is 75.8% of those that have ever performed BSE. Of those that had their breast examined, 100% had a clinical examination and not a mammographic examination.
There was a statistically significant difference in the awareness and practice of BSE among respondents with high educational level [X2 = 16.25, P = 0.012], family history of breast cancer [X2 = 13.87, P = 0.008], marital status [X2 = 17.71, P = 0.024] and smoking habit of respondents [X2 = 20.82, P = 0.0001]. The gravidity of the respondent [X2 = 4.57, P = 0.34], age [X2 = 7.52, P = 0.68], religion [X2 = 1.78, P = 0.78] and type of marriage background [X2 = 7.75, p = 0.10] were not statistically significantly associated with the awareness and practice of BSE. This is as shown in Tables 1 and 2 below.
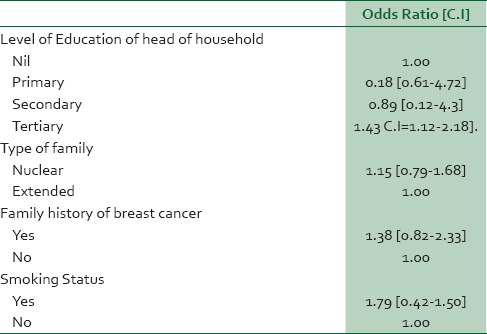
In the multiple logistic regression models, four measures that were statistically significantly associated with awareness and practice of breast self examination were entered into the model. The only predictor of awareness and practice of breast self examination was tertiary level of education (OR = 1.43 CI = 1.12-2.18]. This is shown in Table 3 below.
Table 3.
Multivariate logistic regression
DISCUSSION
This study has revealed poor awareness and practice of BSE. Only 24.4% of respondents have ever performed BSE and 5.3% of the respondents performed BSE on monthly basis. Studies on female healthcare staff have reported regular BSE performance rates of 6-83%.11,12,13,14,15 However, different studies show that the development of level of knowledge and the society's attitude about BSE can play a positive role on screening performances of the society's women.16,17 In order to raise awareness, it is advised for women to have a regular breast examination every month and to report any abnormalities found through observation.
This study reported that higher level of education was statistically significant associated with BSE practice. In many findings, practice of BSE was determined by the awareness of women or their having of information about diagnostic methods of breast cancer.18,19,20 Investments should be made in improving women's awareness of and access to BSE. Public education and awareness programs should be developed to promote earlier diagnosis using a multi-pronged approach that includes simple, cost-effective ways of disseminating the relevant information (such as through the mass media). The participation of non-governmental and charitable organizations in creating awareness about breast cancer will also be helpful in improving the practice of BSE.
This study shows that family history is statistically significantly associated with BSE and low personal perception of risk of developing breast cancer was a major factor for non-performance of BSE. Several studies have reported similar findings that family history of cancer significantly influenced the practice of the BSE.12,20,21,22 One of the most important factors that increase the risk of developing breast cancer among women is family history.23,24 The perception that most of the young women do not consider themselves at risk for developing breast cancer can discourage them from doing BSE. Identification of barriers regarding BSE is very essential and can be used to design appropriate educational interventions which promote this preventive behaviour.
The study shows an association between clinical examination of breast by the physicians and continual BSE by respondents. All of those examined by the clinicians had continued BSE though not regularly. Several studies have shown that acquiring information on BSE from health professional, discussion with families on the importance of BSE, and history of breast exam by health professional were the factors found associated with BSE practice.17,18 Therefore, training on BSE should be given to increase the practice of BSE which in turn would have the impact to avert the severe morbidity and mortality of breast. Moreover, giving training on the techniques of BSE for health extension workers is the way of reaching the wider community and the best opportunity to tackle the problem at wider perspective. Evidences suggest that BSE is a reliable screening tool when used as an adjunct to clinical breast examination and imaging studies.25,26 In addition, early diagnosis of breast cancer has been related to the frequency of BSE.27 Early diagnosis is an important strategy, particularly in low- and middle-income countries where the diseases is diagnosed in late stages and resources are very limited. There is some evidence that this strategy can produce “down staging” of the disease to stages that are more amenable to curative treatment.28 Breast cancer deaths can be reduced significantly if the tumor is discovered at an early stage.29
Keeping in mind that most breast cancers are diagnosed by women themselves, the importance of regular self-breast examination becomes obvious. Therefore, women should be encouraged to perform BSE, due to its importance in the early diagnosis of breast cancer. It is of the utmost importance to raise awareness and knowledge regarding the early diagnosis of breast cancer at an early age, and to teach the appropriate techniques. BSE is significant only when performed at regular intervals and conscientiously. If discovered early, breast cancer can usually be cured; however, early detection through screening is the only way to reduce mortality.
ACKNOWLEDGEMENTS
We hereby acknowledge all the Hospital staff of CMPC Dept of OOUTH Sagamu and Medical students rotating through the department during the study period for their contribution during the design and conduct of the study.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Banaian SH, Kazemian A, Soleiman KH. Knowledge, attitude, practice among women referred to health centers in Broojen about screening methods of breast cancer. J Shahrekord Univ Med Sci. 2005;7:28–34. [Google Scholar]
- 2.Harris DM, Miller JE, Davis DM. Racial differences in breast cancer screening, knowledge and compliance. J Natl Med Assoc. 2003;95:693–701. [PMC free article] [PubMed] [Google Scholar]
- 3.Baxter N. Canadian Task Force on Preventive Health Care. Preventive health care, 2001 update: Should women be routinely taught breast self-examination to screen for breast cancer? CMAJ. 2001;164:1837–46. [PMC free article] [PubMed] [Google Scholar]
- 4.Carelli I, Pompei LM, Mattos CS, Ferreira HG, Pescuma R, Fernandes CE, et al. Knowledge, attitude and practice of breast self-examination in a female population of metropolitan São Paulo. Breast. 2008;17:270–4. doi: 10.1016/j.breast.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 5.Parkin DM, Fernandez LM. Use of statistics to assess the global burden of breast cancer. Breast J. 2006;12:S70–80. doi: 10.1111/j.1075-122X.2006.00205.x. [DOI] [PubMed] [Google Scholar]
- 6.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63:11–30. doi: 10.3322/caac.21166. [DOI] [PubMed] [Google Scholar]
- 7.Dundar PE, Ozmen D, Ozturk B, Haspolat G, Akyildiz F, Coban S, et al. The knowledge and attitudes of breast self-examination and mammography in a group of women in a rural area in western Turkey. BMC Cancer. 2006;6:43. doi: 10.1186/1471-2407-6-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Danesh A, Amiri M, Ramezani A, Tazhibi M, Ganji F. Knowledge, attitude, practice among female workers in shahrekord education organization about breast self examination. J Shahrekord Univ Med Sci. 2002;4:47–52. [Google Scholar]
- 9.Green BB, Taplin SH. Breast cancer screening controversies. J Am Board Fam Pract. 2003;16:233–41. doi: 10.3122/jabfm.16.3.233. [DOI] [PubMed] [Google Scholar]
- 10.Nakhichevan NO, Secginli S. Health belief related to breast self-examination in a sample of Turkish women. Oncol Nurs Forum. 2007;34:425–32. doi: 10.1188/07.ONF.425-432. [DOI] [PubMed] [Google Scholar]
- 11.Agboola AO, Deji-Agboola AM, Oritogun KS, Musa AA, Oyebadejo TY, Ayoade BA. Knowledge, attitude and practice of breast self examination in female health workers in Olabisi Onabanjo University teaching hospital, Sagamu, Nigeria. Int Med J. 2007;8:5–10. [Google Scholar]
- 12.Akhigbe AO, Omuemu VO. Knowledge, attitudes and practice of breast cancer screening among female health workers in a Nigerian urban city. BMC Cancer. 2009;9:203. doi: 10.1186/1471-2407-9-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alkhasawneh LM, Akhu-Zaheya LM, Suleiman SM. Knowledge and practice of breast self-examination. J Adv Nurs. 2009;65:412–6. doi: 10.1111/j.1365-2648.2008.04891.x. [DOI] [PubMed] [Google Scholar]
- 14.Ibrahim NA, Odusanya OO. Knowledge of risk factors, beliefs and practices of female healthcare professionals towards breast cancer in a tertiary institution in Lagos, Nigeria. BMC Cancer. 2009;9:76. doi: 10.1186/1471-2407-9-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Odusanya OO, Tayo OO. Tayo breast cancer knowledge, attitudes and practice among nurses in Lagos, Nigeria. Acta Oncol. 2001;40:844–8. doi: 10.1080/02841860152703472. [DOI] [PubMed] [Google Scholar]
- 16.Rosvold EO, Hjartåker A, Bjertness E, Lund E. Breast self-examination and cervical cancer testing among Norwegian female physicians. A nation-wide comparative study. Soc Sci Med. 2001;52:249–58. doi: 10.1016/s0277-9536(00)00225-2. [DOI] [PubMed] [Google Scholar]
- 17.Karayurt O, Dramali A. Adaptation of Champion's Health Belief Model Scale for Turkish women and evaluation of the selected variables associated with breast self-examination. Cancer Nurs. 2007;30:69–77. doi: 10.1097/00002820-200701000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Godazande GH, Khani H, Khalilian AR, Atarod Z, Firouzjai MA, Partoei A, et al. Knowledge and practice of women over 15 years about breast cancer in Sari. J Mazandaran Univ Med Sci. 2006;16:64–74. [Google Scholar]
- 19.Friedman LC, Moore A, Webb JA, Puryear LJ. Breast cancer screening among ethnically diverse low-income women in a general hospital psychiatry clinic. Gen Hosp Psychiatry. 1999;21:374–81. doi: 10.1016/s0163-8343(99)00036-5. [DOI] [PubMed] [Google Scholar]
- 20.Teferi S, Mezgebe T, Demissie M, Durgaprasada A. IOSR Journal of Pharmacy and Biological Sciences, Baywood Publishers. 13th ed. Vol. 2. Addis Ababa: Ethiopia; 2012. Knowledge about breast cancer risk-factors, breast screening method and practice of breast screening among female healthcare professionals working in governmental hospitals; pp. 5–12. [Google Scholar]
- 21.Karima FE, Ashraf MS. Knowledge and practice of breast cancer screening among Egyptian nurses. J Hematol Oncol. 2010;1:122–8. [Google Scholar]
- 22.Al-Naggar RA, Al-Naggar DH, Bobryshev YV, Chen R, Assabri A. Practice and barriers toward breast self-examination among young Malaysian women. Asian Pac J Cancer Prev. 2011;12:1173–8. [PubMed] [Google Scholar]
- 23.Bassey RB, Irurhe NK, Olowoyeye MA, Adeyomoye AA, Onajole AT. Knowledge, attitude and practice of breast self-examination among nursing students in Lagos University Teaching Hospital, Nigeria. Educ Res. 2011;2:1232–6. [Google Scholar]
- 24.Karayurt O, Ozmen D, Cetinkaya AC. Awareness of breast cancer risk factors and practice of breast self examination among high school students in Turkey. BMC Public Health. 2008;8:359. doi: 10.1186/1471-2458-8-359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Montgomery GH, Erblich J, DiLorenzo T, Bovbjerg DH. Family and friends with disease: Their impact on perceived risk. Prev Med. 2003;37:242–9. doi: 10.1016/s0091-7435(03)00120-8. [DOI] [PubMed] [Google Scholar]
- 26.Habib F, Salman S, Safwat M, Shalaby S. Awareness and knowledge of breast cancer Among University Students in Al Madina Al Munawara Region. Middle East J Cancer. 2010;1:159–66. [Google Scholar]
- 27.Chong PN, Krishnan M, Hong CY, Swash TS. Knowledge and practice of breast cancer screening amongst public health nurses in Singapore. Singapore Med J. 2002;43:509–16. [PubMed] [Google Scholar]
- 28.Loescher L. Nursing roles in cancer prevention position statements. Semin Oncol Nurs. 2004;20:111–20. doi: 10.1053/j.soncn.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 29.Abdel-Fattah M, Zaki A, Bassili A, El-Shazly M, Tognoni G. Breast self-examination practice and its impact on breast cancer diagnosis in Alexandria, Egypt. East Mediterr Health J. 2000;6:34–40. [PubMed] [Google Scholar]


