Abstract
Background:
Breast imaging plays a vital role in the multidisciplinary approach to management of breast disease. A baseline data is apt and necessary for collaborative studies.
Materials and Methods:
This is a prospective descriptive study carried out between January 2009 and December 2013 at our institution. Patients who had breast imaging were recruited into the study. Film-screen mammograms were acquired with a General Electric (GE) Senographe DMR machine. Breast ultrasound done using an Aloka Prosound SSD-350+ ultrasound machine equipped with linear and curvilinear 7.5–10 MHz transducer. Findings were categorized using the ACR-BIRADS (American college of Radiologists-Breast imaging reporting and data system). Data was collated and analysed using social statistical package (SPSS) version 17.
Result:
The mammograms of 824 patients were evaluated during this study period. Their age ranged from 40–85 years with a mean age of 50.9 ± 8.1 years. Eight hundred and sixteen (99%) were females and eight (1%) were males. The commonest clinical indication was breast lump (23.9%). The commonest density pattern was BIRADS 2-scattered fibroglandular pattern (43.9%). Mammograms were normal in 266 (32.3%) and positive in 558 (67.7%). The final BIRADS assessment showed BIRADS 0, 1, 2, 3, 4, 5 and 6 constituted 6.6%, 30.1%, 29.7%, 22.2%, 5.9%, 5.0% and 0.5% respectively.
Conclusion:
The level of awareness of breast cancer is quite high with the positive mammographic yield emphasizing the value of a multidisciplinary approach in the management of breast diseases.
Keywords: Audit, mammography findings, north central Nigeria
INTRODUCTION
Imaging has an important role to play in the management of breast diseases, which often present as breast mass, breast pain and the likes. Breast imaging has only come of age in the twenteith century, beginning with the introduction of mammography, which stemmed from the discoveries of X-rays and radiation in the late nineteenth century with breast ultrasound scan as an adjunct imaging modality.
In a developing country like ours, mammography and breast ultrasound scan still remain the key modalities for imaging the breast. Mammography is highly sensitive for early detection of cancer and thus remains the goal standard in breast cancer screening1 However, its sensitivity in cancer detection is reduced in mammographically dense breast which is a reflection of the amount of radiographic dense epithelium and stroma in the breast.2 In older women on hormone replacement therapy (HRT) or other medications and younger ones with naturally dense breast, ultrasound is useful in diagnosing breast lesions.3 There are various documentations on findings in breast cancer screening programmes,4,5,6,7 mostly from countries with established screening programmes with relatively scanty reports from developing countries. Increased awareness of breast cancer and recent establishment of breast imaging units has led to high turnout of patients. Generally, benign breast diseases are commoner than their malignant counterpart worldwide.3,8,9,10,11 This premier study documents our findings and analysis using the ACR-BIRADS.12,13
MATERIALS AND METHODS
The hospital ethics and research requirements were met before commencing this prospective study which was carried out among all consecutive patients that came for screening and diagnostic mammography in the breast imaging unit of our institution during a 5-year period, January 2009-December 2013.
The patients were made to complete a self administered questionnaire on getting to the breast imaging unit with or without a request form. This contained basic bio data information like age, sex, occupation, level of education; reproductive history such as age of menarche, menopause, first childbirth, parity and use of oral contraceptives; family history of breast cancer and other medical history. For patients that came in for follow up imaging during the period of study, the latest findings were used for the study. Data from these were collated and analysed using social statistical package (SPSS) version 17.
Mammography was routinely done as the first line of investigation in women 40 years and above and ultrasound scan in those with equivocal mammographic findings. The film-screen mammograms were acquired with a General Electric (GE) Senographe DMR machine using two standard views (cranio-caudal (CC) and mediolateral oblique (MLO) and additional views such as spot compression magnification view, cleavage view and exaggerated CC view where necessary. Breast ultrasound scan was done using an Aloka Prosound SSD-350 + ultrasound machine equipped with linear and curvilinear 7.5–10 MHz transducer in longitudinal, transverse, radial and anti-radial planes.
The mammograms were evaluated by two trained radiologists under well lit viewing box and mammographic breast density pattern and findings assigned and categorized using BIRADS classification method. The density classifications are: BIRADS 1: Breast almost entirely fatty; BIRADS 2: Scattered fibroglandular pattern; BIRADS 3: Heterogeneous dense pattern and BIRDAS 4: Homogenous dense pattern. The assessment categories of findings are as follows: BIRADS 0: Inconclusive study; BIRADS 1: Normal study, BIRADS 2: Benign findings, BIRADS 3: Probably benign findings; BIRADS 4: Suspicious lesion, BIRADS 5: Highly suspicious lesion and BIRADS 6: Known biopsy.
RESULTS
The mammograms of 824 patients were evaluated during this study period. Their age ranged from 40–85 years with a mean age of 50.9 ± 8.1 years. The 40–49 age groups constituted the largest group (48.2%) with the least in the 80–90 groups (0.5%) [Table 1]. Eight hundred and sixteen (99%) were females and eight (1%) were males.
Table 1.
Age distribution of patients

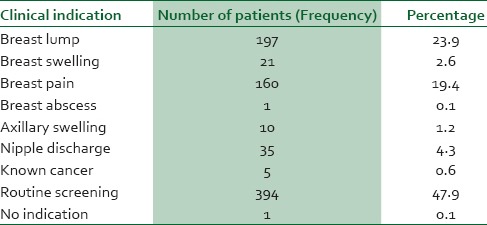
Of these patients, three hundred and ninety four (47.8%) came for routine screening, 52.1% had clinical indication and one patient (0.1%) had no documented clinical indication. Table 2 shows the frequency of the various clinical indications. The commonest clinical indication was breast lump (23.9%), closely followed by breast pain (19.4%) and just one patient with breast abscess (0.1%). These findings were slightly commoner on the right side; also four of the five cases of known cancer had their tumors on the right side. Fifty (6.1%) and 38 (4.6%) patients had history of mastectomy and lumpectomy respectively. There was positive history of breast cancer in first degree relatives in 46 (5.6%) patients including one of those with known cancer. In a patient with known cancer as the clinical indication, the cancer was already fungating hence mammography of the unaffected breast alone was done and re-categorized based on our finding.
Table 2.
Clinical indication distribution pattern
Mammographic density patterns were classified in the 816 females as shown in Table 3.
Table 3.
Distribution of mammographic density pattern

This showed that the ACR-BIRADS 2 (scattered fibroglandular pattern) had the highest frequency of 43.9%, followed by the fatty replaced pattern with 38.2%, then heterogeneous dense with 16.4% and least proportion was extremely dense pattern with 0.5%.
Mammograms were normal in 266 (32.3%) of the study population while 558 (67.7%) showed positive findings, Table 4. Of the positive findings, circumscribed opacity with regular margin were 371 in number, constituting 66.5% of the positive findings, this included opacity seen within breast parenchyma and axillary region irrespective of their sizes. Opacity with irregular, angular or speculated margin accounted for (53) 16.7%. Calcifications of various types were seen in 149 (17.8%), of these, 80.3% were benign looking and 19.7% suspicious. Areas of focal glandular asymmetry were noted in twenty-eight (5%) mammograms while tubular shaped, soft tissue opacity mainly in the retroareola region were seen in eighteen (3.2%) mammograms. Two (0.4%) of the male patients had diffuse increase in breast tissue without a focal opacity. Some patients however had combination of findings.
Table 4.
Distribution of mammographic findings

The final BIRADS assessment distribution is as shown in Table 5. Inconclusive study (BIRADS 0), Normal study (BIRADS 1), Benign findings (BIRADS 2), Probably Benign findings (BIRADS 3), Suspicious findings (BIRADS 4), Highly suspicious findings (BIRADS 5) and Known Cancer (BIRADS 6) constituted 6.6%, 30.1%, 29.7%, 22.2%, 5.9%, 5.0% and 0.5% respectively.
Table 5.
BIRADS assessment categories distribution

DISCUSSION
Imaging of the breast is assuming a vital role in the management of breast disease and breast cancer screening. Mammography has established its role in this direction. However, modifications like graduation from screen film mammography to digital mammography; contrast enhanced spectral mammography, breast tomosynthesis have evolved. Automated breast ultrasound scan, shear wave elastography are evolving. Magnetic resonance imaging (MRI) is also assuming a prominent role in breast imaging. Other modalities include computed tomography (CT), scintimammography, positron emission mammography (PEM) and single photon emission computed tomography (SPECT). In our centre, the film-screen mammography and conventional breast ultrasound are the available modalities used in this study.
The largest proportion of women in this study that had mammography was the 40–49 year age group which tallies with the commonest group from previous studies.14,15,16 Baseline mammography is usually started by the fifth decade of life and the increased health awareness and enthusiasm at this stage could probably explain this high percentage. Breast disease includes all non-malignant and malignant conditions of the breast, including lumps, swelling, trauma, mastalgia, mastitis, and nipple discharge. Breast lump accounted for the highest clinical indication for diagnostic mammography closely followed by breast pain. In some studies done locally, breast lumps has been shown to be the most prevalent clinical presentation and highest indication for diagnostic mammography.15,17,18 Mammographic breast density pattern is a reflection of the relative proportion of radiolucent fat to the radiodense glandular epithelium and connective tissue. It is a known independent risk factor for developing breast cancer and can be used to predict who will develop breast cancer.19,20,21 The most prevalent breast density pattern in this study is the scattered fibroglandular pattern (ACR-BIRADS 2) which accounted for 43.9%. This finding is similar to that of Akinola et al., and Pak et al.,15,22 but at variance with Obajimi et al.,14 whose study showed BIRADS 1 as the most prevalent breast pattern. The high risk breast density pattern, BIRADS 3 and 4 constituted a total of 16.9% and this is relatively lower than those from previous studies14,15,23 presumably due to the higher mean age of this study population as breast density pattern is known to be inversely proportional to age.21 These categories of breast density pattern have a lower sensitivity to mammography as an imaging tool as cancers can easily be obscured by the dense breast.24 It is worthy to mention here that of the BIRADS 4 breast pattern patients, one had previous left mastectomy and then presented with right breast swelling and after imaging, her final ultrasound and mammogram BIRADS assessment category was 5 (highly suspicious lesion) based on the presence of scattered clusters of pleomorphic calcifications and was one of those confirmed by histology.
In this study, abnormalities were detected in 67.7% of the population, which buttresses the high sensitivity of mammography in detection of breast diseases.16 In this group of patients with abnormal findings on mammograms, the commonest finding was circumscribed opacity with smooth margins constituting 66.5%. The differential diagnoses of such findings in this study were fibroadenoma, papilloma, cyst, phylloides tumor intramammary node and axillary lymph node as documented in many radiological texts.25,26 The mammographic features of these lesions and use of adjuvant imaging modality like breast ultrasound coupled with relevant clinical history was used in narrowing the differential diagnosis or clinch a diagnosis. For example, breast cysts were confirmed on ultrasound.
Topmost on the differential diagnosis of circumscribed opacity in this study was fibroadenoma. Generally benign breast diseases are commoner than their malignant counterpart3,8,9,10,11 and fibroadenoma has been shown to be the commonest histological-proven benign breast disease8,10,27 while fibrocystic disease was the commonest in the study by Ochicha et al.9
Breast cancer is a common malignant disease estimated to affect approximately 12.15% of women born today over the course of their lifetime.28
A total of 16.7% opacity with irregular, speculated or angular margin was observed in this study. In addition patients had complimentary breast ultrasound and were categorized as suspicious or highly suspicious lesions. Also, 5% of the abnormalities showed as area of focal asymmetry, this could be benign as in cases of summated fibrous tissue, radial scar or perhaps malignant lesions. Tubular retroareola soft tissue opacity was seen in 3.2% of cases, this is higher than seen in Study of Akinola et al.,15 but slightly lower than that of Pak-art et al.22 Sonography showed these to be dilated ducts with or without intraductal masses. The common differentials for this were papillomatosis, malignant papilloma, ductal ectasia or ductal extension of a centrally located carcinoma. The suspicious and highly suspicious lesions are higher than in previous studies15,16,29 and this further emphases the need and value of cytology and histology as the final arbiter in confirming malignant lesions. We could only lay our hands on twenty-nine histology confirmed results during the course of this study. However, a multidisciplinary study to correlate our findings with clinico-pathological findings is being designed. Combination of mammography, breast ultrasound and palpation yields higher sensitivity as to when use alone and this would reduce unnecessary biopsies and its associated risks.30
Calcifications are of various types, shapes and density. They can be associated with benign or malignant diseases of the breast. It was seen in a total 17.8% of the mammograms with or without an associated opacity. This value varies for different studies but predominance of the vascular type tallies and a strong correlation of breast arterial calcification with age have been established in a study by Loberant N et al.31 The worrisome looking types such as pleomorphic and casting type constituted about 19.7% of the calcifications and this could be the earliest sign of breast cancer.32,33 This was a major finding in a case of histological confirmed breast cancer documented during a screening program in this centre previously.34 Two of the male patients had diffuse increased opacity of their breast tissue with no focal mass while the remaining six had focal masses. Fifty four of the patients that were asked to come for breast ultrasound scan based on their mammograms (BIRADS 0) defaulted, thus their studies were inconclusive. This could be due to logistics factors or resort to alternative treatment. The high proportions of the BIRADS 2 (benign) and BIRADS 3 (probably benign lesions) follow the trend of higher incidence of benign breast lesions generally.3,8,9,10,11 The BIRADS 4 and 5 lesions seen were slightly higher than previously documented locally15,29 but could be explained by the higher number of patients in this study. Four of the five cases of known cancer (BIRADS 6) were confirmed on imaging while one of them due to the ulcerating cancer had imaging of the contralateral breast and was classified accordingly.
CONCLUSION
The level of awareness of breast cancer is quite high as justified by almost half of the study population that came for screening mammography. The highest indication for diagnostic mammography was breast lump. The scattered fibroglandular breast pattern was most predominant. Majority of mammographic findings had benign features. Some of the suspicious-looking lesions were confirmed by histology. The high mammographic yield emphasizes the value of a multidisciplinary approach in the management of breast diseases.
ACKNOWLEDGEMENT
Breast Imaging Scientists in the department of Radiology, University of Ilorin Teaching Hospital, Ilorin, Kwara State.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Nandi RJ, Nandi AK, Rangayyan RM, Scutt D. Classification of breast masses in mammograms using genetic programming and feature selection. Med Biol Eng Comput. 2006;44:683–94. doi: 10.1007/s11517-006-0077-6. [DOI] [PubMed] [Google Scholar]
- 2.Heng D, Gao F, Jong R, Fishell E, Yaffe M, Martin L, et al. Risk factors for breast cancer associated with mammographic features in Singaporean Chinese women. Cancer Epidemiol Biomarkers Prev. 2004;13:1751–8. [PubMed] [Google Scholar]
- 3.Malik G, Waqar F, Buledi GQ. Sonomammography for evaluation of solid breast masses in young patients. J Ayub Med Coll Abbottabad. 2006;18:34–7. [PubMed] [Google Scholar]
- 4.Nystrom L, Rutqvist LE, Wall S, Lindgren A, Lindqvist M, Ryden S, et al. Breast cancer screening with mammography: Overview of Swedish randomized trials. Lancet. 1993;341:973–8. doi: 10.1016/0140-6736(93)91067-v. [DOI] [PubMed] [Google Scholar]
- 5.Poplack SP, Tosteson AN, Grove MR, Wells WA, Carney PA. Mammography in 53,803 women from the New Hampshire mammography network. Radiology. 2000;217:832–40. doi: 10.1148/radiology.217.3.r00dc33832. [DOI] [PubMed] [Google Scholar]
- 6.Roberts MM, Alexander FE, Anderson TJ, Chetty U, Donnan PT, Forrest P, et al. Edinburgh trail of screening for breast cancer: Mortality at seven years. Lancet. 1990;335:241–6. doi: 10.1016/0140-6736(90)90066-e. [DOI] [PubMed] [Google Scholar]
- 7.Frisell J, Eklund G, Hellstrom L, Lidbrink E, Rutqvist LE, Somell A. Randomized study of mammography screening - preliminary report on mortality in the Stockholm trial. Breast Cancer Res Treat. 1991;18:49–56. doi: 10.1007/BF01975443. [DOI] [PubMed] [Google Scholar]
- 8.Irabor AO, Okolo CA. An audit of 149 consecutive breast biopsies in Ibadan, Nigeria. Pak J Med Sci. 2008;24:257–62. [Google Scholar]
- 9.Ochicha O, Edino ST, Mohammed AZ, Amin SN. Benign breast lesions in Kano. Nig J Surg Res. 2002;4:1–5. [Google Scholar]
- 10.Adesunkanmi AR, Agbakwuru EA. Benign breast disease at Wesley Guild Hospital, Ilesha, Nigeria. West Afr J Med. 2001;20:146–51. [PubMed] [Google Scholar]
- 11.Starvos AT, Thickmen D, Rapp CL, Dennis MA, Parker SH, Sisney GA. Solid breast nodules: Use of sonography to distinguish between benign and malignant lesions. Radiology. 1995;196:123–34. doi: 10.1148/radiology.196.1.7784555. [DOI] [PubMed] [Google Scholar]
- 12.Sickles EA, Dorsi CJ, Bassette LW. Breast Imaging Reporting and Data System (BI-RADS) 3rd ed. Reston. Virginia: American College of Radiology; 1998. American College of Radiology (ACR) [Google Scholar]
- 13.Sickles EA, Dorsi CJ, Bassette LW. American College of Radiology: Breast imaging reporting and data system, breast Imaging atlas. 4th ed. Reston. Virginia: American College of Radiology; 2003. [Google Scholar]
- 14.Obajimi MO, Adeniji-Sofoluwe AT, Oluwasola AO, Adedokun BO, Soyemi TO, Olopade F, et al. Mammographic breast pattern in Nigerian women in Ibadan, Nigeria. Breast Dis. 2011;33:9–15. doi: 10.3233/BD-2010-0313. [DOI] [PubMed] [Google Scholar]
- 15.Akinola RA, Akinola OL, Shittu L, Balogun BO, Tayo AO. Appraisal of mammography in Nigeria women in a new teaching Hospital scientific. Res Essay. 2007;2:325–9. [Google Scholar]
- 16.Adeyomoye AA, Awosanya GO, Adesanya AA, Anunobi CC, Osibogun A. Medical audit of diagnostic mammographic examination at the Lagos university teaching hospital (luth), Nigeria. Niger Postgrad Med J. 2009;16:25–30. [PubMed] [Google Scholar]
- 17.Jeje EA, Mofikoya BO, Oku YE. Pattern of breast masses in Lagos: A private health facility review of 189 consecutive patients. Nig Q Hosp Med. 2010;20:38–41. doi: 10.4314/nqjhm.v20i1.58015. [DOI] [PubMed] [Google Scholar]
- 18.Ayoade BA, Tade AO, Salami BA. Clinical features and pattern of presentation of breast diseases in surgical outpatient clinic of a suburban tertiary hospital in South-west Nigeria. Niger J Surg. 2012;18:13–6. doi: 10.4103/1117-6806.95476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McCormack VA, dos Santos Silva I. Breast density and parenchymal patterns as markers of breast cancer risk: A meta-analysis. Cancer Epidemiol Biomarkers Prev. 2006;15:1159–69. doi: 10.1158/1055-9965.EPI-06-0034. [DOI] [PubMed] [Google Scholar]
- 20.Boyd NF, Martin LJ, Bronskill MJ, Yaffe MJ, Duric N, Minkin S. Breast tissue composition and susceptibility to breast cancer. J Natl Cancer Inst. 2010;102:1224–37. doi: 10.1093/jnci/djq239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wolfe JN. Breast patterns as an index of risk for developing breast cancer. AJR Am J Roentgenol. 1976;126:1130–7. doi: 10.2214/ajr.126.6.1130. [DOI] [PubMed] [Google Scholar]
- 22.Pak-art P, Bunjunwetwat D, Vajragupta L, Amomrattanapaijit W, Vajarapongse K, Sampatanukui P, et al. Abnormal findings in breast imaging: A hospital-based survey in 4264 Thai women. J Med Assoc Thai. 2004;87:5179–84. [PubMed] [Google Scholar]
- 23.Barlow WE, Lehhman CD, Zheng Y, Ballard-Barbash R, Yankaskas BC, Cutter GR, et al. Performance of diagnostic mammography for women with signs and symptoms of breast cancer. J Natl Cancer Inst. 2002;94:1151–9. doi: 10.1093/jnci/94.15.1151. [DOI] [PubMed] [Google Scholar]
- 24.Byrne C, Schairer C, Wolfe J, Parekh N, Salane M, Brinton LA, et al. Mammographic features and breast Cancer risks: Effects with time age and menopause status. J Natl Cancer Inst. 1995;87:1622–9. doi: 10.1093/jnci/87.21.1622. [DOI] [PubMed] [Google Scholar]
- 25.Michelle MJ, Lawinski C, The W, Vinnicombe S. The breast. In: David S, editor. Textbook of Radiology and Imaging. 7th ed. Vol. 2. 2003. pp. 1464–7. [Google Scholar]
- 26.Cardenosa G. Benign masses. In: McAllister L, Scheidt S, Rampertab R, editors. The Core Curriculum Breast Imaging. Philadelphia: Lippincott Williams and Wilkins; pp. 185–237. [Google Scholar]
- 27.Liberman L, Menell JH. Breast imaging reporting and data system (BI-RADS) Radiol Clin North Am. 2002;40:409–30. doi: 10.1016/s0033-8389(01)00017-3. [DOI] [PubMed] [Google Scholar]
- 28.National Cancer Institute. Surveillance Epidemiology and End Results (SEER) SEER Stat Fact Sheets: Breast. [Last accessed on 2014 Sep 26]. Available from: www.cancer.gov .
- 29.Danfulani M, Saidu SA, Ma’aji SM, Musa MA. Pattern of mammographic findings in Sokoto, Nigeria. Asian J Med Sci. 2014;5:79–83. [Google Scholar]
- 30.Varela C, Timp S, Karssemeijer N. Use of border information in the classification of mammographic masses. Phys Med Biol. 2006;51:425–41. doi: 10.1088/0031-9155/51/2/016. [DOI] [PubMed] [Google Scholar]
- 31.Loberant N, Salamon V, Carmi N, Chernihovsky A. Prevalence and degree of breast arterial calcifications on mammography: A cross-sectional analysis. J Clin Imaging Sci. 2013;3:36. doi: 10.4103/2156-7514.119013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ismail F, Holl J, Lockhat Z, Akande H. Unusual mammography findings of patients with ductal carcinoma in situ (DCIS) of the breast. South Afr J Radiol. 2008;12:97–9. [Google Scholar]
- 33.Gülsün M, Demirkazik FB, Ariyürek M. Evaluation of breast microcalcifications according to Breast Imaging Reporting and Data System criteria and Le Gal's classification. Eur J Radiol. 2003;47:227–31. doi: 10.1016/s0720-048x(02)00181-x. [DOI] [PubMed] [Google Scholar]
- 34.Akande HJ, Oyinloye OI, Olafimihan BB. Radiological findings of breast cancer screening in a newly equipped centre. [Last accessed on 2014 Nov 30];Int J Med Sci. 2011 3:294–8. Available from: http://www.academicjournals.org/ijmms . [Google Scholar]


