Abstract
Introduction:
Prostate biopsy remains the gold standard for prostate cancer diagnosis. The field of prostate biopsy is undergoing a rapid change. This study aims to provide a snapshot of the current practice of prostate biopsy in the Urological Society of Australia and New Zealand (USANZ).
Materials and Methods:
A 31-question multiple-choice survey was constructed using a web-based provider and was distributed to 644 members of USANZ. The questionnaire addressed various aspects of prostate biopsy. Questionnaire results were collated and the data were analyzed statistically.
Results:
150 completed surveys were returned, with a response rate of 23.3%: 84.5% of those completing the survey were consultant urologists and 68% were working in a metropolitan setting. 98.6% of clinicians used prophylactic antibiotics before prostate biopsy, most commonly a quinolone. 30.6% had used intravenous (IV) carbapenems at least once. Peri-prostatic local anesthetic (LA) infiltration was used by 39.9% of clinicians with 73% using IV sedation or general anesthetic (GA). 38.4% of clinicians reported performing TPT biopsy of the prostate and 19.6% of clinicians had ordered a MRI of the prostate prior to an initial biopsy with 10.2% routinely ordering a MRI of the prostate before repeat biopsy.
Conclusion:
Frequent prophylactic use of carbapenems suggests concern amongst clinicians about sepsis with quinolone-resistant bacteria. Almost 75% of TRUS biopsies were performed under IV sedation or GA indicating a heavy demand of health resources. TPT biopsy was used commonly and there was significant use of multiparametric MRI prior to prostate biopsy.
Keywords: Antibiotics, magnetic resonance, prostate biopsy, prostate cancer, transperineal template biopsy, transrectal ultrasound-guided biopsy
INTRODUCTION
Prostate biopsy remains the gold standard for diagnosing prostate cancer.[1] The information obtained from a prostate biopsy is arguably the most important in clinical decision-making regarding further management options. In recent years, the field of prostate biopsy has undergone rapid change. Prostate biopsy is not only used for cancer diagnosis, but it is now routinely utilized for monitoring of disease in men undergoing active surveillance for low risk disease. Prostate biopsy is no longer just performed transrectally but also transperineally. The optimal number and location of cores are still unclear. Due to a lack of standardization of prostate biopsy,[2] a wide range of practices are thought to exist. This study aims to provide an insight into current practices of prostatic biopsy in the USANZ.
MATERIALS AND METHODS
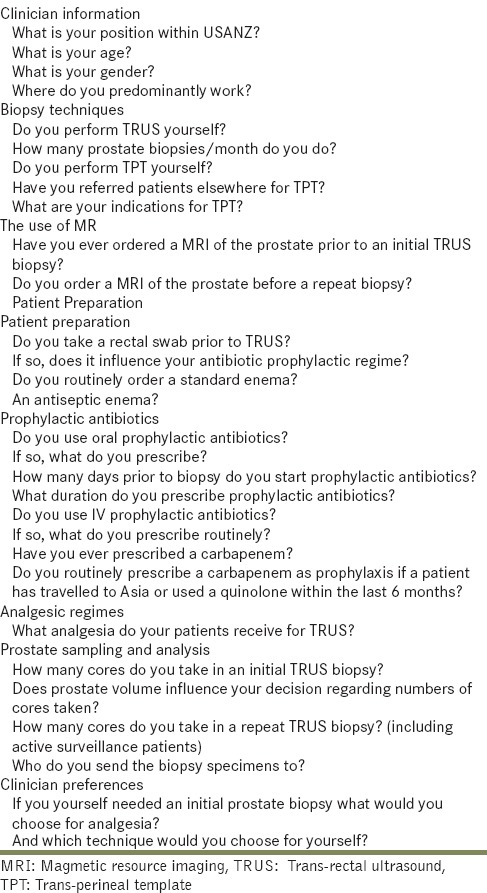
A 31-question multiple-choice survey was constructed using a web-based survey provider, freeonlinesurveys.com. The survey explored a range of issues regarding prostate biopsy. Multiple choices were provided for answering, wherever appropriate. Questions from the survey are outlined in Table 1.
Table 1.
Questions regarding prostate biopsy practices that were distributed to the USANZ community
Permission to distribute the survey was obtained from the USANZ directorate. The survey was then linked to the weekly USANZ e-newsletter which is sent to 644 members. The survey was launched in November 2012. A link to the survey was also broadcast in posts on the USANZ e-forum, Netwit.
The completed survey results were collated automatically by the survey website's software. Data for various groups were then gathered and comparisons were made between these groups. Groups that were compared included consultants and trainees, clinicians aged 50 years or greater and those less than 50 years, clinicians working in regional settings and those in metropolitan settings as well as those clinicians who perform TPT biopsy and those who do not perform TPT biopsy.
Statistical comparisons were made using the Chi-Square Test for equal proportions or Fisher's exact test where the numbers were small. A two-sided P value less than 0.05 was considered statistically significant.
RESULTS
General demographics
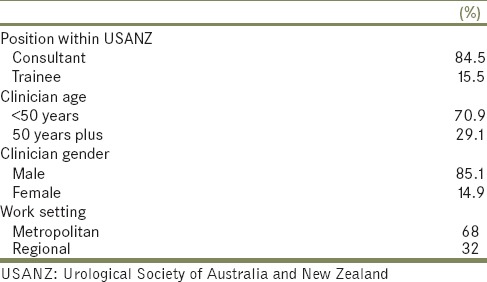
Of the 644 USANZ members to whom the survey was distributed, 150 completed surveys were received, for a response rate of 23.3%. Table 2 provides some additional demographic data.
Table 2.
General demographics of the USANZ responders
95.2% of those clinicians that responded to the survey were performing TRUS biopsy themselves, 85.7% were performing 1 to 20 TRUS biopsies each month.
Use of MR
19.6% of respondents had ordered a MR of prostate prior to an initial biopsy and 10.2% routinely used MR prerepeat biopsy with a further 46.9% occasionally having used MRI pre repeat biopsy. MR was used more commonly preinitial biopsy amongst those who perform TPT biopsy compared to those who do not perform TPT biopsy (33.9% vs. 11.1%; P = 0.001).
Patient preparation methods
Only 2% of clinicians routinely took a rectal swab prior to prostate biopsy. 9.5% of clinicians used rectal swabs if the patient had recently traveled to Asia or used a quinolone. 29.9% ordered a standard enema prior to prostate biopsy and 10.8% ordered an antiseptic enema prior to prostate biopsy.
Antibiotic prophylaxis
98.6% used prophylactic antibiotics prior to prostate biopsy. Figure 1 shows the most commonly prescribed prophylactic antibiotics. Most commonly prophylactic antibiotics were started the day prior to procedure (52.7%) or the day of the procedure (37.2%). 56.8% of clinicians prescribed a three day course of prophylactic antibiotics, 22.3% a one day course and 11.5% a five day course.
Figure 1.
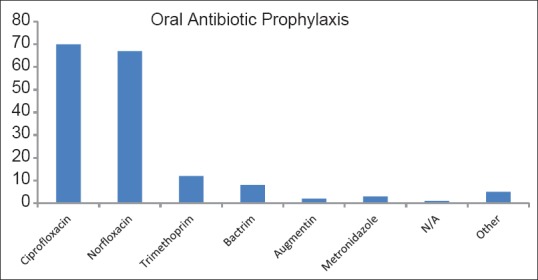
Most commonly prescribed oral antibiotic prophylaxis (Y-axis – number of clinicians who use these agents)
69.4% of clinicians used IV prophylactic antibiotics. Figure 2 highlights the most commonly used IV antibiotic prophylaxis. 30.6% of clinicians have used IV carbapenems and 27.7% routinely used them if the patient had travelled to Asia or used quinolones within six months of the planned biopsy date. The use of carbapenems was more common in metropolitan areas compared to regional areas (40.2% vs. 8.7%; P < 0.001).
Figure 2.
Most commonly prescribed intravenous antibiotic prophylaxis (Y-axis – number of clinicians who use these agents)
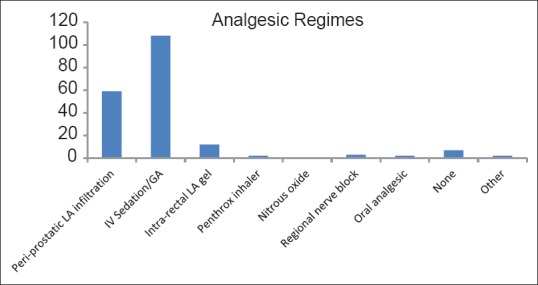
Analgesia regimes
73% of clinicians used IV sedation or GA for analgesia in prostatic biopsy. 39.9% used peri-prostatic LA infiltration while 8.1% used intrarectal LA gel. The use of IV sedation or GA was more frequent in metropolitan areas than regional areas (79% vs. 59.6%; P = 0.01); See Figure 3.
Figure 3.

Most commonly used analgesic regimes (Y-axis – number of clinicians who use these regimes)
Prostatic biopsy sampling and analysis
For an initial prostate biopsy 54.1% clinicians took 10-12 prostate cores while 38.4% took 14-16 cores. Prostatic volume influenced the decision as to how many cores were taken in 59.4% of clinicians. 71.4% of those clinicians who perform TPT biopsy were influenced by prostatic volume compared to 51.8% of those who do not perform TPT biopsy (P = 0.02). For repeat biopsy, including patients having a repeat biopsy as part of active surveillance, 55.5% clinicians took greater than 20 cores. General pathologists were used to analyze the specimens by 27.2% of clinicians while 72.8% utilized expert uro-pathologists. General pathologists were used more commonly in regional areas (38.3% vs. 21.2%; P = 0.03). Consultants used specialist uro-pathologists more commonly than trainees (77.3% vs. 17.7%; P < 0.001).
Trans-perineal biopsy of the prostate
38.4% of clinicians had performed TPT biopsy of the prostate. 49.3% of clinicians had referred patients on for TPT biopsy of the prostate. The main indications for TPT biopsy were a rising PSA after negative TRUS prostate biopsy and as part of active surveillance. TPT biopsy was performed less frequently amongst clinicians in regional settings compared to those in metropolitan settings (26.1% vs. 44.4%; P = 0.04).
Urologist preferences
Overall 78.4% of clinicians would prefer a TRUS biopsy of the prostate if they needed a biopsy. Most trainees also preferred to undergo a TRUS biopsy rather than TPT biopsy. However, the proportion of trainees preferring TPT biopsy (36.4%) was higher than that for consultant urologists at 18.4% (P = 0.09), although this did not reach statistical significance. Also clinicians who performed TPT biopsy were more likely to want a TPT biopsy if they needed a biopsy than those clinicians who do not perform TPT biopsy (35.7% vs. 13.3%; P = 0.001).
DISCUSSION
Prostate biopsy remains the mainstay of diagnosing prostate cancer. It is standard of care for prostate biopsy to be performed with ultrasound guidance.[1] Most commonly, prostate biopsy is performed transrectally. Between July 2011 and June 2012, 27,352 TRUS biopsies were performed in Australia.[3] However the transperineal approach, with comparable cancer detection rates to TRUS biopsy, appears to be gaining momentum.
No clear standard exists regarding other aspects of prostate biopsy. As such, practices of prostate biopsy vary amongst urologists. This is not limited to the biopsy technique but extends to patient preparation, antibiotic prophylaxis, analgesic regimes, prostatic sampling and analysis as well as the use of MRI.[2]
Although a significant limitation of this study is the response rate to the distributed survey, clear trends in the practice of prostate biopsy in our region were apparent.
Antibiotic prophylaxis
When performing a TRUS biopsy of the prostate, rectal flora may be inoculated into the prostate and thereon into the bloodstream. Common organisms include Escherichia coli, Streptococcus faecalis and Bacteroides.[4] Several studies have demonstrated the efficacy of prophylactic antibiotics in TRUS biopsy[5,6] such that it is standard of care.
According to current EUA guidelines, quinolones are the antibiotic of choice in TRUS biopsy as they are well-absorbed orally and have good prostatic tissue penetration.[1,6,7] Our data suggest that quinolones in the form of ciprofloxacin and norfloxacin are being most commonly used as prophylaxis in the region.
Infectious complications following prostatic biopsy are reported to occur in 1-6% of patients.[8] These range from life-threatening sepsis to fever, urinary tract infection, acute prostatitis and epididymo-orchitis.[9] Quinolone-resistant infections after prostate biopsy are becoming increasingly common worldwide. They represent a significant problem and have even been described as a public health emergency.[10]
The cause of this concerning trend is thought to be due to widespread inappropriate quinolone use.[11] The use of quinolones in the 6 months before biopsy has been associated with an increased risk of fecal carriage of quinolone-resistant bacteria.[12]
Quinolone-resistant bacteria are usually susceptible to carbapenems. In this survey, 30.6% of clinicians reported having used IV carbapenems as prophylaxis with 27.7% reporting that they routinely used carbapenems if the patient had traveled to Asia or used quinolones within 6 months of the proposed biopsy date. This prophylactic use of carbapenems highlights the concern about sepsis with quinolone-resistant bacteria in our region. Of even greater concern than quinolone-resistant pathogens is the emergence of carbapenem-resistant Enterobacter (CRE), deemed to be an “urgent threat” in the CDC's 2013 report. These strains are likely to be promoted by the increasing use of carbapenems as prophylaxis, as “use of antibiotics is the single most important factor leading to antibiotic resistance around the world.”[13] Treatment options for these organisms are very limited.
Transperineal biopsy of the prostate
Transperineal biopsy has an equivalent tumor detection rate and has been reported to improve cancer detection in the anterior zone.[14] TPT biopsy has an extremely low infection rate. This is particularly important, given the increasing rate of serious post-TRUS biopsy infections. A recent worldwide review found the post-TPT biopsy infection rate to be 0.07%.[15] Within our region, TPT was commonly used with 38.4% of clinicians performing TPT biopsy. It was more likely to be performed amongst clinicians working in metropolitan settings.
Of note, when clinicians were asked what technique of biopsy they themselves would choose if they were to need a prostate biopsy, trainees were more likely to choose a TPT biopsy of their prostate compared to consultants. This may translate to the increasing use of this approach in the future.
Use of MRI
Multiparametric MRI of the prostate is increasingly being used in the detection of prostate cancer. If suspicious areas are found they can be targeted with additional biopsies. Some centers are even performing MR-targeted biopsies only, although this remains controversial.
There was significant use of MRI by USANZ members with 19.6% having utilized MRI prior to an initial prostate biopsy. The use of MRI was most notable in those clinicians performing TPT biopsy of the prostate. 33.9% of clinicians performing TPT biopsy of the prostate had an MRI performed prior to initial biopsy. These results indicate a degree of acceptance of MRI as a useful tool in prostate cancer diagnosis by urologists in the region and correspond to the burgeoning literature in this field.
Analgesic regimes
In the EUA's guidelines on TRUS biopsy, peri-prostatic infiltration of LA (PILA) is described as state of the art analgesia.[1] Despite this, the majority of TRUS biopsies in our region were performed under IV sedation or GA at 73%. This suggests a degree of dissatisfaction amongst clinicians with PILA. It also highlights the significant resource allocation associated with prostate biopsy being performed under IV sedation and GA. Further research is warranted to determine a widely acceptable and efficacious method of analgesia that can be performed outside the operation theatre.
To conclude, this study provides an insight into the current practices of prostate biopsy by USANZ members. Although TRUS biopsy without additional imaging was still the most typical approach, use of MRI and TPT biopsy was common. Both of these diagnostic tools are likely to continue to increase in the future. Quinolone prophylaxis was widely used but selective use of prophylactic carbapenems was also common, suggesting concerns regarding quinolone-resistant pathogens and their infective complications. There was a lack of widespread use of PILA, the gold standard analgesic regime for prostate biopsy, indicating a lack of confidence in the efficacy of this method, and a heavy use of resources in our region for this minor diagnostic procedure.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Heidenreich A, Bastian P, Bellmunt J, Bolla M, Joniau S, Mason MD, et al. Guidelines on Prostate Cancer. Eur Assoc Urol. 2013 Mar;:154. [Google Scholar]
- 2.Djavan B, Rocco B. Optimising prostate biopsy. BMJ. 2012;344:D8201. doi: 10.1136/bmj.d8201. [DOI] [PubMed] [Google Scholar]
- 3.Medicare Benefits Schedule. Australian Government: Department of Health and Aging 2012. [Last accessed on 2014 June 01]. Available from: http://www.health.gov.au .
- 4.Patel U, Rickards D. London: Martin Dunitz; 2002. Handbook of Transrectal Ultrasound and Biopsy of the Prostate. [Google Scholar]
- 5.Kapoor DA, Klimberg IW, Malek GH, Wegenke JD, Cox CE, Patterson AL, et al. Single dose oral ciprofloxacin versus placebo for prophylaxis during transrectal prostate biopsy. Urology. 1998;52:552–8. doi: 10.1016/s0090-4295(98)00296-9. [DOI] [PubMed] [Google Scholar]
- 6.Aron M, Rajeev TP, Gupta NP. Antibiotic prophylaxis for transrectal needle biopsy of the prostate: A RCT. Br J Urol. 2000;85:682–5. doi: 10.1046/j.1464-410x.2000.00576.x. [DOI] [PubMed] [Google Scholar]
- 7.Naber KG. Use of quinolones in UTI and prostatitis. Rev Infect Dis. 1989;11:1321–7. doi: 10.1093/clinids/11.supplement_5.s1321. [DOI] [PubMed] [Google Scholar]
- 8.Adibi M, Pearle M, Lotan Y. Cost-effectiveness of standard vs intensive antibiotic regimens for transrectal ultrasonography-guided prostate biopsy prophylaxis. Br J Urol. 2011;110:86–91. doi: 10.1111/j.1464-410X.2011.10768.x. [DOI] [PubMed] [Google Scholar]
- 9.Steensels D, Slabbaert K, De Wever L, Vermeersch P, Van Poppel H, Verhaegen J. Fluoroquinolone resistant E. coli in intestinal flora of patients undergoing transrectal ultrasound-guided prostate biopsy – should we reassess our practices for antibiotic prophylaxis? Clin Microbiol Infect. 2012;18:575–81. doi: 10.1111/j.1469-0691.2011.03638.x. [DOI] [PubMed] [Google Scholar]
- 10.Bartoletti R, Cai T. Prostate biopsies should be performed according to a standard of care. Eur Urol. 2013;63:528–30. doi: 10.1016/j.eururo.2012.06.050. [DOI] [PubMed] [Google Scholar]
- 11.Ekici S, Cengiz M, Turan G, Alış EE. Fluoroquinolone-resistant acute prostatitis requiring hospitalization after transrectal prostate biopsy: Effect of previous fluoroquinolone use as prophylaxis or long-term treatment. Int Urol Nephrol. 2012;44:19–27. doi: 10.1007/s11255-011-9980-3. [DOI] [PubMed] [Google Scholar]
- 12.Baltaci S, Suer E, Haliloglu AH, Gokce M, Elhan A, Beduk Y. Effectiveness of antibiotics given to aymptomatic men for an increased PSA. J Urol. 2009;181:129–32. doi: 10.1016/j.juro.2008.09.020. [DOI] [PubMed] [Google Scholar]
- 13.Antibiotic Resistance Threats in the United States. US Department of Health and Human Services; Centers for Disease Control and Prevention. [Last accessed on 2014 Apr]. Available from http://www.cdc.gov/drugresistance/threat-report-2013 .
- 14.Grummet JP, Hossack T, Weerakoon M, Huang S, Lawrentschuk N, Frydenberg M, Moon DA, et al. Sepsis and superbugs: Should we favour the transperineal over transrectal approach for prostate biopsy? Br J Uro. 2013 doi: 10.1111/bju.12536. In Press. [DOI] [PubMed] [Google Scholar]
- 15.Dickinson L, Ahmed HU, Allen C, Barentsz JO, Carey B, Futterer JJ, et al. Magnetic resonance imaging for the detection, localisation, and characterisation of prostate cancer: Recommendations from a European Consensus Meeting. Eur Urol. 2011;59:477–94. doi: 10.1016/j.eururo.2010.12.009. [DOI] [PubMed] [Google Scholar]


