Abstract
Introduction:
The aim of this study was to evaluate the combination of intralesional verapamil injection (IVI) therapy with and tadalafil in men affected by Peyronie's disease (PD).
Materials and Methods:
In this study, 59 patients diagnosed with PD, were divided into three groups. Group A (GA) counted 23 patients treated with IVI; Group B (GB) treated 19 patients with tadalafil 5 mg once a day, and Group C (GC) treated 17 patients with IVI and tadalafil for 3 months. There were assessed at baseline and follow-up: Erectile function, presence and severity of painful erections, penile plaque size and penile curvature degree.
Results:
After 3 months pain resolved completely in 57% cases of GA, 61% of GB and 76% of GC; the final mean curvature degree further decreased in all groups without statistically significant differences; mean plaque size remained stable in GA: 1.57 versus 1.59 at baseline (P = 0.364) and GB: 1.51 versus 1.52 at baseline (P = 0,265), while a further decrease was evident in GC: 1.46 versus 1.58 at baseline (P = 0.03). Mean International Index of Erectile Function-5 score further improved significantly in the group treated with verapamil plus tadalafil: 23.1 versus 14.4 of GA and 18.2 of GB (P ≤ 0.01).
Conclusions:
The association of IVI and tadalafil showed better pain control while reducing penile curvature and erectile function, improving the quality of life.
Keywords: Erectile dysfunction, Peyronie's disease, phosphodiesterase type 5 inhibitors, verapamil
INTRODUCTION
Peyronie's disease (PD) is classified as fibrous, inelastic lesion of the tunica albuginea.
The tunica albuginea of the penis with fibroblast proliferation forms a thickened fibrous plaque that may cause penile pain, penile curvature and erectile dysfunction (ED).[1]
The aetiology of PD is considered to be multifactorial with the interplay of a genetic predisposition, trauma and tissue ischaemia.[2]
The prevalence of PD is estimated up to 7% among men in the general population, up to 8% of men with ED and >20% of men with comorbid diabetes and ED.[3] Importantly, this prevalence valuation may yet underestimate the true incidence of PD, because men may not present for treatment due to embarrassment or misbelieving that the disorder is not treatable.
Peyronie's disease natural evolution has two phases. First is an active (or acute) phase, characterized by inflammation and progressive deformity of the erect penis. During the acute disease phase, patients may experience painful erections and curvature deformity of the erect penis. However, not all patients have the experience penile pain or discomfort. The early phase generally lasts from 6 to 16 months, and after this phase, the majority of patients experience plaque's stabilization or disease progression.[4,5] The transition to the chronic phase is marked by resolution of pain and inflammation. The plaque size and the penis curvature become relatively stable with extensive fibrosis.
No reliable and effective nonsurgical therapy has emerged, in part because of the incomplete understanding of the pathophysiology disorders.[1]
Verapamil is a calcium channel blocker and therefore an intralesional verapamil injection (IVI) therapy inhibits calcium-dependent extracellular collagen transport and up-grade regulates collagenase activity at the plaque site.[6] Reports on the efficacy of IVI are varying. In vitro data demonstrate that the transport of extracellular matrix molecules, including collagen and fibronectin, is a calcium-dependent process. Therefore, a modification of the inflammatory response in the early phase of the disorder inhibits fibroblast proliferation in the plaques.[7] In the only randomized placebo-controlled study, no statistical significant differences were reported in plaque size, penile curvature and pain during erection.[8]
Phosphodiesterase type 5 inhibitors (PDE5i) have long been used in the treatment of ED. In PD, these agents are proposed to inhibit tissue remodeling after acute injuries by decreasing oxidative stress responsible for inflammation and fibrosis.[9]
The hypothesis of this study is that the combination of the mechanical effects of penile therapy with IVI and oral medications whit PDE5 (tadalafil) may have a synergistic effect on the tunica albuginea and plaque for men with PD.
MATERIALS AND METHODS
In this prospective, randomized study between April 2010 and May 2013, 59 consecutive patients diagnosed with PD, were treated as it follows: Group A (GA) consisted of 23 patients treated with verapamil 10 mg, 1 injection/week for a period of 12 weeks in the plaque ensuring uniformity of the injected drug; Group B (GB) counted 19 patients treated with oral medication: Tadalafil 5 mg once a day for a period of 3 months; Group C (GC) involved 17 patients treated with the association of two therapeutic agents (verapamil 10 mg and tadalafil 5 mg) for a period of 3 months. The group of patients underwent a comprehensive diagnostic protocol that included medical history, clinical examination, self-photography, penile Doppler ultrasound in patients associated ED. Patients with the following characteristics were included into the study protocol: disease not >12 months, a single penile plaque demonstrated by dynamic sonography, plaque's maximum size of 3.75 cm2 and penis recurvatum <30°. Patients receiving prior intralesional or surgical therapy for PD were excluded.
All patients gave their informed written consent. Subjects receive randomly IVI therapy or tadalafil 5 mg once daily or IVI plus tadalafil 5 mg for 3 months.
Erectile function, presence and severity of painful erections, penile plaque's size and penile curvature degree were assessed at baseline and follow-up evaluations by the same operator. ED was evaluated through the shortened version of the International Index of Erectile Function (IIEF-5) questionnaire. Severity of painful erection was assessed by means of VAS score ranging from 0 to 10, with 0 being no pain and 10 being severe pain. Plaque position was evaluated by palpation and plaque size was assessed by ultrasonography during an artificial erection induced by a standard injection of alprostadil (8 mcg). Plaque's size was measured as the product of length and width in square centimeters. The degree of penile curvature was determined with a goniometer during full artificial erection.
Statistical analysis of the mean values of continuous variables was performed using the Student's t-test and analysis of the significance of the categorical variables was performed using the Chi-square and Fisher tests. P <0.05 was considered to indicate statistical significance.
RESULTS
Patient's characteristics at inclusion are reported in Table 1. Not statistically significant differences emerged between the three groups at baseline. One patient of GB abandoned the study after 1-month of therapy because of drug intolerance (headache and flushing). There were no clinically hematomas requiring intervention reported after IVI. No patients reported new ED or changes in penile sensation. Four patients of GA (17%) and two of GB (2%) had a superficial hematoma at injection site, but there were no permanent adverse sequelae. However, adverse treatment effects are reported in Table 2. 3 months after the therapy in GA pain resolved completely or partially in 57% (13/23) of the patients, whereas in 61% (11/18) and 76% (13/17) cases of GB and GC, respectively. However, mean curvature degree decreased in all groups without statistically differences with baseline values.
Table 1.
Patients characteristics pretreatment

Table 2.
Adverse events reported during the treatments

Group A patients had a reduction from a mean of 21.4° at baseline to a mean of 19.8° after the 12 weeks protocol (P = 0.284). Patients in GB had a reduction from a mean of 22.03° at baseline to a mean of 20.05° after treatment (P = 0.34), while in GC a mean of 21.80° versus 19.6° after treatment, respectively (P = 0.87) [Figure 1].
Figure 1.

Mean curvature degree in Group A: (verapamil), Group B (tadalafil) and Group C (verapamil + tadalafil) at baseline and at follow-up after 12 weeks
Mean plaque size remained stable in GA: 1.57 versus 1.59 at baseline (P = 0.364) and GB: 1.51 versus 1.52 at baseline (P = 0.265), while a further decrease was evident in GC: 1.46 versus 1.58 at baseline (P = 0.03) [Figure 2]. Mean IIEF-5 score further improved significantly in the group treated with verapamil plus tadalafil: 23.1 versus 14.4 of GA and 18.2 of GB (P ≤ 0.01) [Figure 3].
Figure 2.
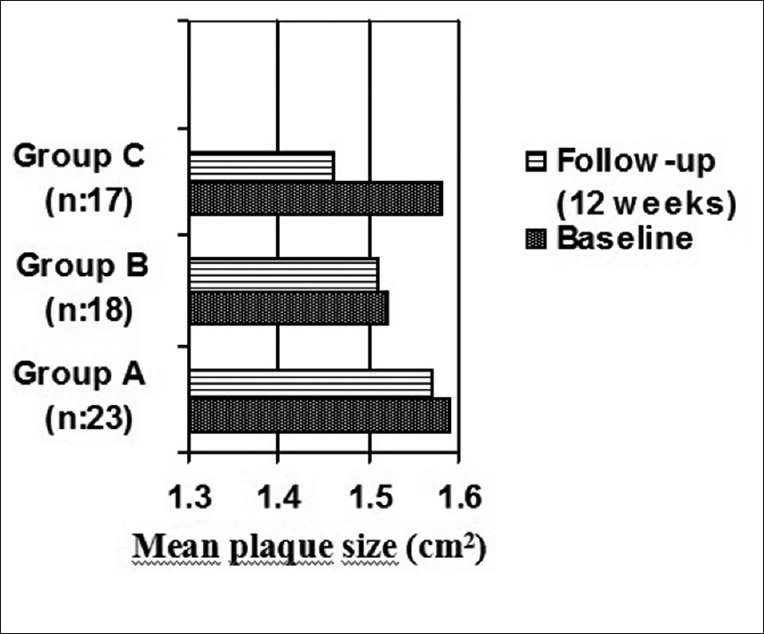
Mean plaque size in Group A: (verapamil), Group B (tadalafil) and Group C (verapamil + tadalafil: P = 0.03) at baseline and at follow-up after 12 weeks
Figure 3.

Mean International Index of Erectile Function-5 scores in Group A: (verapamil), Group B (tadalafil) and Group C (verapamil + tadalafil: P < 0.001) at baseline and at follow-up after 12 weeks
DISCUSSION
Peyronie's disease is first described in 1743 by Francois Gigot de La Peyronie.[10] The best therapy of PD remains controversial, in part because both etiology and natural history of the disease are not sufficiently known.
While severe deformities and ED are best treated surgically, for light and medium curvatures, pain and slow disease progression is preferred a conservative approach by oral and intralesional therapy.[11] Candidates for PD medical treatment are patients with early stage disease, those with progressive deformity and unstable plaque and those with painful erections.
The implication of chronic inflammation as the common pathway leading to PD has spurred various treatment strategies to reverse the associated fibrosis and attempt to restore normal tunica elasticity.[12]
In order to treat PD numerous treatment strategies exist and include the early efforts using steroids to suppress the inflammatory process. This leads to efforts using more sophisticated intralesional injection to suppress the fibrosis plaque. Other options for treatment include the use of pentoxyphyline, tamoxifen and Vitamin E as antiinflammatory reagents.[13]
Several products that are delivered as injections into the penile plaque have been tested as PD treatments. Treatment with injectable agents is typically performed by a specialist. Verapamil, a calcium anatagonist, has been used to treat PD based on its ability to alter fibroblast production of extracellular matrix macromolecules and collagenases.[14]
Reports on the efficacy of IVI are varying. In 1994, Levine et al.[6] published a small nonrandomized study of escalating IVI that demonstrated the drug's safety and the efficacy in reducing plaque volumes and penile curvature. A subsequent randomized, placebo-controlled trial showed a decrease in plaque volume and a trend towards improved curvature (nonstatistically significant) when compared to saline IVI alone.[15]
An uncontrolled trial in 2007 showed statistically significant improvement in penile rigidity in 94 patients,[16] while a 2009 randomized, placebo-controlled trial with 80 patients showed no statistical significance with Verapamil treatment in any of the primary outcomes (plaque size, degree of curvature, and erectile function).[8]
Since then, IVI has been used in a great number of trials both alone[17] and in combination with other treatment modalities (dexamethasone administered via trans-dermal electromotive administration,[18] testosterone supplementation in low-testosterone patients with PD,[19] and pentoxifylline and L-arginine given orally with or without penile traction.[20] PDE5i have long been used in the ED treatment. PDE5i enhances smooth muscle relaxation of the corpus cavernosum, thereby promoting blood flow to the penis.[21]
A current research of PDE5i use in regulating penile erectile response has revealed an alternative role for PDE5i in decreasing oxidative stress-associated inflammatory change by reducing the collagen/smooth muscle and collagen. Long-term use of PDE5i as an antifibrotic agent by maintaining or increasing the NO and cGMP levels in the target tissues has been promising and provides a much needed armamentarium in the PD medical therapy. The apoptotic effect on penile myofibroblast with PDE5i has been shown in sildenafil,[22] vardenafil,[23] and tadalafil.[24] Ferrini et al.[23] have reported that long-term oral treatment with vardenafil slows down and reverses the early stages of an experimental PD-like plaque in rats and potentially might play a role to ameliorate a more advanced plaque. A retrospective chart review of 65 PD patients showed a statistically significant improvement in the IIEF score in patients taking a low dose of tadalafil daily for 6 months when compared with those who did not take tadalafil.[9]
Finally, Palmieri et al.[25] published that tadalafil therapy in combination with ESWT was superior then ESWT alone in both IIEF and quality of life scores.
There are no studies in the literature that have compared the therapeutic efficacy of Verapamil and PDE5i association of in PD treatment.
In our study, curvature degree decreased in all groups without statistically differences from baseline values, while a further decrease of plaque size was evident in the group treated with the association of the two therapeutic agents (P = 0.03). This lower rate of deterioration in penile curvature could be explained by the short-term follow-up. However, tadalafil may play a role in stabilizing plaque's fibrosis of and penis curvature, as amply demonstrated in the literature. The increase in IIEF-5 scores in the tadalafil groups is to be expected. Certainly the limit of our study, in addition to a nonhigh number of patients treated in draw each group, was to have had a short period of follow-up. This prevents information on the natural course of the plaque or the possible long-term efficacy of tadalafil. Another limit of the present study is the low incidence of cardiovascular comorbidities (hypercholesterolemia, diabetes mellitus, ischemic heart disease and peripheral vascular disease) of significant severity, which likely reflects the excellent health status of the patients and then a rapid recovery of sexual function.
CONCLUSIONS
This study demonstrates an interesting therapeutic signal in which tadalafil used daily has a role on antifibrotic activity in PD and its treatment.
This action is valid when combined strategically to the synergistic action of verapamil injected directly into the plaque. Moreover, IVI was not able to improve alone plaque size and curvature degree in our subset of patients. However, larger studies with a longer follow-up are needed to determine the effectiveness of the proposed therapeutic strategy in PD.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Pryor J, Akkus E, Alter G, Jordan G, Lebret T, Levine L, et al. Peyronie's disease. J Sex Med. 2004;1:110–5. doi: 10.1111/j.1743-6109.2004.10116.x. [DOI] [PubMed] [Google Scholar]
- 2.Mulhall J, Anderson M, Parker M. A surgical algorithm for men with combined Peyronie's disease and erectile dysfunction: Functional and satisfaction outcomes. J Sex Med. 2005;2:132–8. doi: 10.1111/j.1743-6109.2005.20113.x. [DOI] [PubMed] [Google Scholar]
- 3.El-Sakka AI. Prevalence of Peyronie's disease among patients with erectile dysfunction. Eur Urol. 2006;49:564–9. doi: 10.1016/j.eururo.2005.10.026. [DOI] [PubMed] [Google Scholar]
- 4.Mulhall JP, Schiff J, Guhring P. An analysis of the natural history of Peyronie's disease. J Urol. 2006;175:2115–8. doi: 10.1016/S0022-5347(06)00270-9. [DOI] [PubMed] [Google Scholar]
- 5.Gelbard MK, Dorey F, James K. The natural history of Peyronie's disease. J Urol. 1990;144:1376–9. doi: 10.1016/s0022-5347(17)39746-x. [DOI] [PubMed] [Google Scholar]
- 6.Levine LA, Merrick PF, Lee RC. Intralesional verapamil injection for the treatment of Peyronie's disease. J Urol. 1994;151:1522–4. doi: 10.1016/s0022-5347(17)35291-6. [DOI] [PubMed] [Google Scholar]
- 7.Hatzimouratidis K, Eardley I, Giuliano F, Hatzichristou D, Moncada I, Salonia A, et al. EAU guidelines on penile curvature. Eur Urol. 2012;62:543–52. doi: 10.1016/j.eururo.2012.05.040. [DOI] [PubMed] [Google Scholar]
- 8.Shirazi M, Haghpanah AR, Badiee M, Afrasiabi MA, Haghpanah S. Effect of intralesional verapamil for treatment of Peyronie's disease: A randomized single-blind, placebo-controlled study. Int Urol Nephrol. 2009;41:467–71. doi: 10.1007/s11255-009-9522-4. [DOI] [PubMed] [Google Scholar]
- 9.Chung E, Deyoung L, Brock GB. The role of PDE5 inhibitors in penile septal scar remodeling: Assessment of clinical and radiological outcomes. J Sex Med. 2011;8:1472–7. doi: 10.1111/j.1743-6109.2011.02217.x. [DOI] [PubMed] [Google Scholar]
- 10.Musitelli S, Bossi M, Jallous H. A brief historical survey of “Peyronie's disease”. J Sex Med. 2008;5:1737–46. doi: 10.1111/j.1743-6109.2007.00692.x. [DOI] [PubMed] [Google Scholar]
- 11.Tunuguntla HS. Management of Peyronie's disease - a review. World J Urol. 2001;19:244–50. doi: 10.1007/s003450100209. [DOI] [PubMed] [Google Scholar]
- 12.Ralph DJ, Minhas S. The management of Peyronie's disease. BJU Int. 2004;93:208–15. doi: 10.1111/j.1464-410x.2004.04587.x. [DOI] [PubMed] [Google Scholar]
- 13.Shaw EJ, Mitchell GC, Tan RB, Sangkum P, Hellstrom WJ. The non-surgical treatment of peyronie disease: 2013 update. World J Mens Health. 2013;31:183–92. doi: 10.5534/wjmh.2013.31.3.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Levine LA, Goldman KE, Greenfield JM. Experience with intraplaque injection of verapamil for Peyronie's disease. J Urol. 2002;168:621–5. doi: 10.1016/s0022-5347(05)64691-5. [DOI] [PubMed] [Google Scholar]
- 15.Rehman J, Benet A, Melman A. Use of intralesional verapamil to dissolve Peyronie's disease plaque: A long-term single-blind study. Urology. 1998;51:620–6. doi: 10.1016/s0090-4295(97)00700-0. [DOI] [PubMed] [Google Scholar]
- 16.Bennett NE, Guhring P, Mulhall JP. Intralesional verapamil prevents the progression of Peyronie's disease. Urology. 2007;69:1181–4. doi: 10.1016/j.urology.2007.02.042. [DOI] [PubMed] [Google Scholar]
- 17.Moskovic DJ, Alex B, Choi JM, Nelson CJ, Mulhall JP. Defining predictors of response to intralesional verapamil injection therapy for Peyronie's disease. BJU Int. 2011;108:1485–9. doi: 10.1111/j.1464-410X.2010.10029.x. [DOI] [PubMed] [Google Scholar]
- 18.Mehrsai AR, Namdari F, Salavati A, Dehghani S, Allameh F, Pourmand G. Comparison of transdermal electromotive administration of verapamil and dexamethasone versus intra-lesional injection for Peyronie's disease. Andrology. 2013;1:129–32. doi: 10.1111/j.2047-2927.2012.00018.x. [DOI] [PubMed] [Google Scholar]
- 19.Cavallini G, Biagiotti G, Lo Giudice C. Association between Peyronie disease and low serum testosterone levels: Detection and therapeutic considerations. J Androl. 2012;33:381–8. doi: 10.2164/jandrol.111.012948. [DOI] [PubMed] [Google Scholar]
- 20.Abern MR, Larsen S, Levine LA. Combination of penile traction, intralesional verapamil, and oral therapies for Peyronie's disease. J Sex Med. 2012;9:288–95. doi: 10.1111/j.1743-6109.2011.02519.x. [DOI] [PubMed] [Google Scholar]
- 21.Boolell M, Allen MJ, Ballard SA, Gepi-Attee S, Muirhead GJ, Naylor AM, et al. Sildenafil: An orally active type 5 cyclic GMP-specific phosphodiesterase inhibitor for the treatment of penile erectile dysfunction. Int J Impot Res. 1996;8:47–52. [PubMed] [Google Scholar]
- 22.Kovanecz I, Rambhatla A, Ferrini M, Vernet D, Sanchez S, Rajfer J, et al. Long-term continuous sildenafil treatment ameliorates corporal veno-occlusive dysfunction (CVOD) induced by cavernosal nerve resection in rats. Int J Impot Res. 2008;20:202–12. doi: 10.1038/sj.ijir.3901612. [DOI] [PubMed] [Google Scholar]
- 23.Ferrini MG, Kovanecz I, Nolazco G, Rajfer J, Gonzalez-Cadavid NF. Effects of long-term vardenafil treatment on the development of fibrotic plaques in a rat model of Peyronie's disease. BJU Int. 2006;97:625–33. doi: 10.1111/j.1464-410X.2006.05955.x. [DOI] [PubMed] [Google Scholar]
- 24.Kovanecz I, Rambhatla A, Ferrini MG, Vernet D, Sanchez S, Rajfer J, et al. Chronic daily tadalafil prevents the corporal fibrosis and veno-occlusive dysfunction that occurs after cavernosal nerve resection. BJU Int. 2008;101:203–10. doi: 10.1111/j.1464-410X.2007.07223.x. [DOI] [PubMed] [Google Scholar]
- 25.Palmieri A, Imbimbo C, Creta M, Verze P, Fusco F, Mirone V. Tadalafil once daily and extracorporeal shock wave therapy in the management of patients with Peyronie's disease and erectile dysfunction: Results from a prospective randomized trial. Int J Androl. 2012;35:190–5. doi: 10.1111/j.1365-2605.2011.01226.x. [DOI] [PubMed] [Google Scholar]


