Abstract
A 9-year-old girl presented to us, after failed perineal approach for vaginal atresia, with abdominal pain. She was thoroughly evaluated and contrast enhanced computed tomographic was done, which revealed absence of lower 1/3rd of vagina with normal uterus, fallopian tubes and ovaries. There was no associated anomaly. She was successfully managed by a combined robotic and perineal approach. Follow-up after 6 and 12 months revealed large capacious vagina with healthy mucocutaneous junction.
Keywords: Robotic vaginoplasty, vaginal agenesis, vaginal atresia
INTRODUCTION
Adolescent girls may present with cyclical abdominal pain. When such pain is progressive, vaginal atresia must be a differential diagnosis. In these cases clinical examination of the abdomen may not be contributory; however, examination of the perineum reveals absence of vaginal opening. An abdominal ultrasonography will confirm a large cystic mass of the pelvis secondary to cryptic menstruation. Vaginal atresia may have different grades, each having different surgical approach. We report an interesting case, which was referred to us after a failed perineal approach in a urology center. This was managed successfully by a combined robotic and perineal approach.
CASE REPORT
A 9-year-old girl was referred to us after failed perineal approach in a urology hospital in our neighboring country. She was in severe pain due to cryptic menstruation, demonstrated by contrast enhanced computed tomographic done in our place. Computed tomography showed normal uterus with cystic vagina and absence of lower 1/3rd of vagina [Figure 1]. Examination under anesthesia with genitoscopy revealed normal labia minor and majora with patulous urethral opening. Anal opening was normal but vaginal opening was not seen. Diagnostic laparoscopy showed normal bilateral ovaries and fallopian tubes with distended uterus. She underwent Robotic assisted vaginoplasty. Both the ureters were preoperatively stented. The intra-abdominal portion was performed entirely with Davinci SI robot (Intuitive Surgical, Sunnyvale, CA). The magnification and high resolution of the robot helped us to precisely dissect lower end of blind ending vagina from urethra/bladder and rectum. Uterine vessels were also preserved. This allowed caudal mobilization of vagina which allowed us to avoid bowel interposition for vaginal reconstruction. Perineal skin flaps were used to construct vagina from outside and mucocutaneous anastomosis was done with the help of robot. Time taken for the abdominal approach was approximately 135 min. There was minimal blood loss and no intraoperative or postoperative complications. Oral feeds were started after 24 h. She was discharged on the 7th postoperative day after endoscopic examination and stent removal, with Foley catheter in situ, which was later removed after 6 weeks. Follow-up was done after 6 and 12 months, which revealed large capacious vagina with healthy mucocutaneous junction and she was fully continent.
Figure 1.

Computed tomography (sagittal view) showing dilated upper 2/3rd vagina with atresia of lower 1/3rd
DISCUSSION
Vaginal atresia occurs when the urogenital sinus (UGS) fails to contribute to formation of the lower (distal) portion of the vagina. This differs from vaginal agenesis in that the Müllerian structures are usually not affected. As a result, the uterus, cervix, and upper portion of the vagina are normal. Vaginal agenesis is the absence the proximal portion of the vagina in an otherwise phenotypically, chromosomally and hormonally intact female. It occurs at an incidence of approximately 1 in 5000–10,000 live female births. This is usually associated with various syndromes like Mayer-Rokitansky-Kuster-Hauser syndrome, Bardet–Biedl syndrome, Kaufman–McKusick syndrome, Fraser syndrome, and Winters syndrome. These syndromes generally comprise of variable absence or hypoplasia of Mullerian structures with renal or skeletal anomalies. Rarely, vaginal agenesis is associated with abnormal development of the anus and rectum.
There are many classification systems for congenital utero-vaginal anomalies. These include:
Buttram and Gibbons classification
American Fertility Society (AFS) classification
Modified Rock and Adam - AFS classification.
All these classification are for Mullerian duct anomalies and as such there is no validated classification system for vaginal atresia. In AFS classification, complete vaginal atresia is categorized under agenesis or dysgenesis of the Müllerian ductal system. In our patient, both ovaries with fallopian ducts, uterus, upper 2/3rd of vagina and were normal with no associated anomaly in other system and hence we concluded it to be UGS anomaly. There are different grades of this anomaly ranging from imperforate hymen to vaginal atresia of lower portion.
The most common presentation is primary amenorrhea but it may rarely present with cyclical abdominal pain caused by retention of menstrual blood in uterus. Differential diagnosis includes vaginal agenesis, androgen insensitivity syndrome, imperforate hymen, labial adhesions, transverse vaginal septum, and vaginal atresia. Incidence of congenital imperforate hymen in term infants has been reported to be 0.1%. There is no gold standard while choosing the surgical approach. Surgical correction via perineal approach can be successful for imperforate hymen, transverse vaginal septum and sometimes in vaginal atresia. If it fails then it has to be managed on same principles as done for vaginal agenesis. Intermittent self-dilatation, Vecchietti procedure, Williams vaginoplasty, McIndoe procedure, Davydov procedure and various other techniques have been described in the treatment of vaginal agenesis and all these could be employed in vaginal atresia also. Variety of tissues have been used in these surgical techniques to create a functional vaginal substitute, including split thickness skin grafts, full thickness skin grafts, myocutaneous flaps, buccal mucosa grafts, bladder mucosa, peritoneum, amnion, bowel substitution and tissue expansion.[1,2,3]
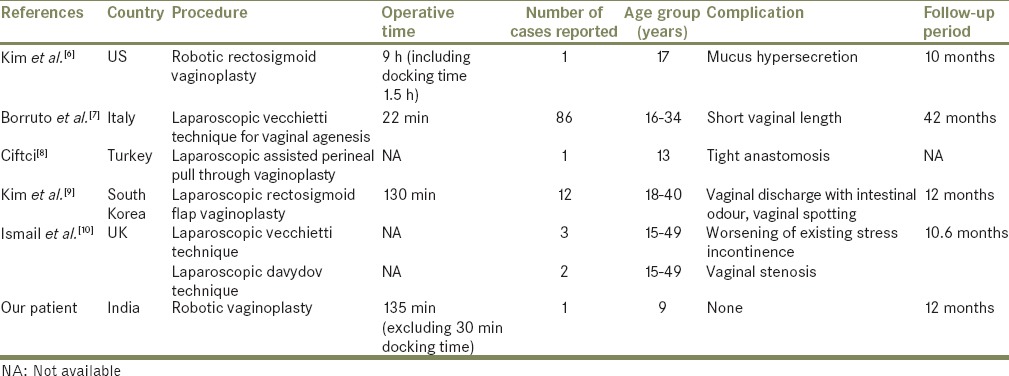
Compared with the traditional open procedure, laparoscopy makes this therapeutic procedure more attractive with advantages of no large abdominal incision, avoiding the exposure of the internal organs, reducing loss of blood and body fluid, quicker recovery of the intestine function, and less complications such as postoperative adhesion. Moreover, the laparoscopic technique allows a better view of the pelvic floor and rectal neovaginal space to avoid rectal injury. Minimally invasive techniques to create a neovagina have been developed gradually and some results have been published [Table 1].[4,5,6,7,8,9,10] Now days, these surgeries are increasingly being done with robotic assistance. The three-dimensional view with depth perception is remarkable. Images with increased resolution combined with the increased degrees of freedom and enhanced dexterity greatly enhances the surgeon's ability to identify and dissect anatomic structures.
Table 1.
Studies done on robotic/laparoscopic vaginoplasty
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Darai E, Toullalan O, Besse O, Potiron L, Delga P. Anatomic and functional results of laparoscopic-perineal neovagina construction by sigmoid colpoplasty in women with Rokitansky's syndrome. Hum Reprod. 2003;18:2454–9. doi: 10.1093/humrep/deg443. [DOI] [PubMed] [Google Scholar]
- 2.Tei E, Yamataka A, Segawa O, Kobayashi H, Lane GJ, Tobayama S, et al. Laparoscopically assisted anorectovaginoplasty for selected types of female anorectal malformations. J Pediatr Surg. 2003;38:1770–4. doi: 10.1016/j.jpedsurg.2003.08.018. [DOI] [PubMed] [Google Scholar]
- 3.Sheth NP, Chainani MS, Sheth SN. Vaginoplasty from peritoneal tube of Douglas’ pouch for congenital vaginal agenesis. Eur J Pediatr Surg. 2003;13:213–4. doi: 10.1055/s-2003-41259. [DOI] [PubMed] [Google Scholar]
- 4.Urbanowicz W, Starzyk J, Sulislawski J. Laparoscopic vaginal reconstruction using a sigmoid colon segment: A preliminary report. J Urol. 2004;171:2632–5. doi: 10.1097/01.ju.0000111342.92168.42. [DOI] [PubMed] [Google Scholar]
- 5.Maas SM, Eijsbouts QA, Hage JJ, Cuesta MA. Laparoscopic rectosigmoid colpopoiesis: Does it benefit our transsexual patients? Plast Reconstr Surg. 1999;103:518–24. doi: 10.1097/00006534-199902000-00023. [DOI] [PubMed] [Google Scholar]
- 6.Kim C, Campbell B, Ferrer F. Robotic sigmoid vaginoplasty: A novel technique. Urology. 2008;72:847–9. doi: 10.1016/j.urology.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 7.Borruto F, Camoglio FS, Zampieri N, Fedele L. The laparoscopic Vecchietti technique for vaginal agenesis. Int J Gynaecol Obstet. 2007;98:15–9. doi: 10.1016/j.ijgo.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 8.Ciftci I. Laparoscopic-assisted perineal pull-through vaginoplasty. J Pediatr Surg. 2012;47:e13–5. doi: 10.1016/j.jpedsurg.2011.11.070. [DOI] [PubMed] [Google Scholar]
- 9.Kim SK, Jeong JO, Kwon YS, Lee KC, Park KJ, Jung G. Laparoscopic rectosigmoid flap vaginoplasty. J Plast Surg Hand Surg. 2011;45:226–31. doi: 10.3109/2000656X.2011.613649. [DOI] [PubMed] [Google Scholar]
- 10.Ismail IS, Cutner AS, Creighton SM. Laparoscopic vaginoplasty: Alternative techniques in vaginal reconstruction. BJOG. 2006;113:340–3. doi: 10.1111/j.1471-0528.2005.00845.x. [DOI] [PubMed] [Google Scholar]


