Abstract
Background:
Cervical cancer is the most common cancer among Indian women of reproductive age. Unfortunately, despite the evidence of methods for prevention, most of the women remain unscreened. The reported barriers to screening include unawareness of risk factors, symptoms and prevention; stigma and misconceptions about gynecological diseases and lack of national cervical cancer screening guidelines and policies. This study attempts to assess the knowledge, attitude, and practices related to cervical cancer and its screening among women of reproductive age (15-45 years).
Materials and Methods:
A facility-based cross-sectional study was done on 400 females of reproductive age who presented to out-patient-department of All India Institute of Medical Sciences Bhopal. Structured questionnaire consisting 20 knowledge items and 7-items for attitude and history of pap smear for practices were administered by one of the investigators after informed consent. Data were entered and analyzed using Epi-Info version 7. Qualitative variables were summarized as counts and percentages while quantitative variables as mean and standard deviation. Predictors of better knowledge, attitude, and practices were identified by binary logistic regression analysis.
Results:
A total of 442 women were approached for interview of which 400 responded of which two-third (65.5%) had heard of cervical cancer. At least one symptom and one risk factor were known to 35.25% and 39.75% participants. Only 34.5% participants had heard, and 9.5% actually underwent screening test, however, 76.25% of the participants expressed a favorable attitude for screening. Binary logistic regression analysis revealed that education age and income were independent predictors of better knowledge. Education level influences attitude toward screening and actual practice depends on age, income, and marital status. This study shows that despite the fact that women had suboptimal level of knowledge regarding cervical cancer, their attitude is favorable for screening. However, uptake is low in actual practice. Strategic communication targeting eligible women may increase the uptake of screening.
Keywords: Awareness, cervical cancer, pap smear, screening
INTRODUCTION
Cervical cancer is a malignant neoplasm arising from cells originating in cervix uteri. It may be completely asymptomatic in early stages.[1] In advanced stages, it may present as persistent pelvic pain, unexplained weight loss, bleeding between periods, unusual vaginal discharge, bleeding, and pain after sexual intercourse.[2] Infection with human papillomavirus (HPV) types 16 and 18 cause 75% of cervical cancer globally.[3] Other risk factors include tobacco consumption, multiple sexual partners, early age of sexual intercourse, increasing parity, prolonged use of oral contraceptive pills, and sexually transmitted diseases.[4]
With access to HPV vaccine and early detection, most cases of cervical cancer are preventable. Pap smear test has been credited with dramatically reducing the number of cases of cervical cancer in developed countries.[5] Unfortunately, despite the availability of methods for prevention, >95% of women in India have never been screened for cervical cancer.[6] There are several barriers to cervical cancer screening uptake for women in low resource areas like India that include-low level of awareness and knowledge[7,8] of risk factors and early signs and symptoms of disease, prevention services, stigma and misconceptions about female cancer and gynecological diseases, socioeconomic limitations, and an overall lack of national cervical cancer screening guidelines and policies.[9]
Cervical cancer is the fourth most common cancer affecting women worldwide with an estimate of 5, 28,000 cases every year.[10] A large majority (85%) of the global burden occurs in less developed regions.[10] Cervical cancer is the 2nd most common cancer among Indian women aged 15-44 years with an estimate of 123,000 incident cases and 67,000 deaths in 2013.[10] In the light of India's rapidly growing population, the overall burden of incidence and mortality of cervical cancer in India is projected to increase by 68 and 78%, respectively, by the year 2030.[10] Within India, the age-adjusted incidence rate of 19.5/100,000 of cervical cancer was reported among women in Bhopal.[11]
The success and benefits of screening at a national level as a public health program to control and prevent cervical cancer depend to a great extent on the level of awareness of the potential beneficiaries. There is scanty information regarding knowledge, attitude, and practices related to cervical cancer and its screening; hence, this study was conducted. The outcome measurement of this study may provide inputs toward designing suitable information, education, and communication strategies to address various health issues of women of reproductive age group.
Aims and objectives
To assess the level of knowledge, attitude, and practice related to cervical cancer and its screening among women of reproductive age attending outpatient department (OPD) of All India Institute of Medical Sciences (AIIMS) Bhopal.
To find the association between sociodemographic characters and knowledge, attitude, and practice related to cervical cancer.
MATERIALS AND METHODS
Facility-based cross-sectional study was conducted in an OPD of AIIMS Bhopal during months of March/April 2014. All patients are subjected to anthropometric and blood pressure assessment at central measurement station before visiting respective departments. Every third women aged 15-45 reporting to this measurement station was approached for participation in the study, and verbal informed consent was obtained. Consenting women were included in the study and further interview with pretested structured questionnaire was conducted by one of the investigators. The questionnaire was comprised of four sections to gather information regarding the sociodemographic characteristics of the participants, knowledge, attitude, and practice regarding cervical cancer and its screening. The sociodemographic characteristics included age, educational status, occupation, marital status, age of marriage, and per capita family monthly income.
The knowledge was assessed using a 20 points scale which had dichotomous response, that is, correct and incorrect. Each correct response was scored as 1 and incorrect as 0. A score 50% (≥10 correct responses) was considered as optimal. Attitude was assessed by 7 statements regarding cervical cancer screening and risk factors responses to which were categorized as 3-point scale Disagree, Neutral, and Agree. Attitude was considered as favorable for screening if four or more “Agree” responses were obtained. Those who had been screened for cervical cancer through pap-smear were regarded as having good practice.
Sample size estimations were based on assumption that 50% women will have optimal knowledge score (>50%). Therefore, required sample size to estimate the proportion of women with optimum knowledge score with 95% confidence interval (CI) of 50% (95% CI 45-55%) 384. Final sample size with 5% nonresponse rate was 400.
Data analysis
Data were entered into Epi-info version 7 (CDC, Atlanta). Qualitative variables were summarized as counts and proportions and numerical variables as mean and standard deviation. Univariate analysis using Chi-square test and t-test as appropriately was done to compare sociodemographic and other factors among optimal knowledge versus sub-optimal knowledge group, favorable attitude versus nonfavorable attitude group and takers of the screening test versus nontakers. We considered P < 0.05 as statistically significant. We performed binary logistic regression analysis separately to identify predictors of optimal knowledge, favorable attitude, and good practices. Independent factors for these three models were statistically significant variables of optimal knowledge, favorable attitude, and good practices groups on univariate analysis.
Ethics issues
A verbal informed consent was obtained from the participants at the time of interview. The Institute Human Ethical Committee of AIIMS Bhopal reviewed and approved study protocol vide letter dated, 1st August 2014.
RESULTS
Of 442 women to whom the questionnaire was administered, 400 responded resulting in response rate of 89%. The sociodemographic profiles of the participants are presented in Table 1. The mean age of the respondents was 32.3 years. Majority of the study participants had secondary or higher level of education (65%). About two-third (64.8%) women were homemakers. Table 2 depicts the distribution of study participants having optimum knowledge score, favorable attitude and practices. Details of responses for knowledge and attitude are shown in Table 3. The knowledge regarding the early symptoms of cervical cancer was limited as 64% (n = 256) of the total participants were not aware of even a single symptom. Furthermore, there was little knowledge about the risk factors as only 39% (156) were aware of at least a single risk factor. About one-third women had heard of cervical cancer screening (34.5%).
Table 1.
Sociodemographic profile of participants (n = 400)
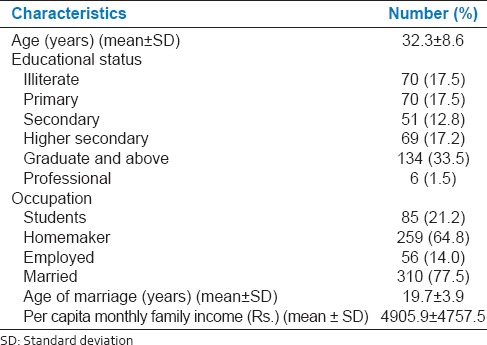
Table 2.
Adequacy of knowledge, attitude, and practice regarding cervical cancer and its screening
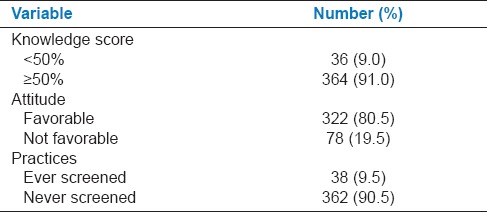
Table 3.
Knowledge of cervical cancer among respondents (n = 400)
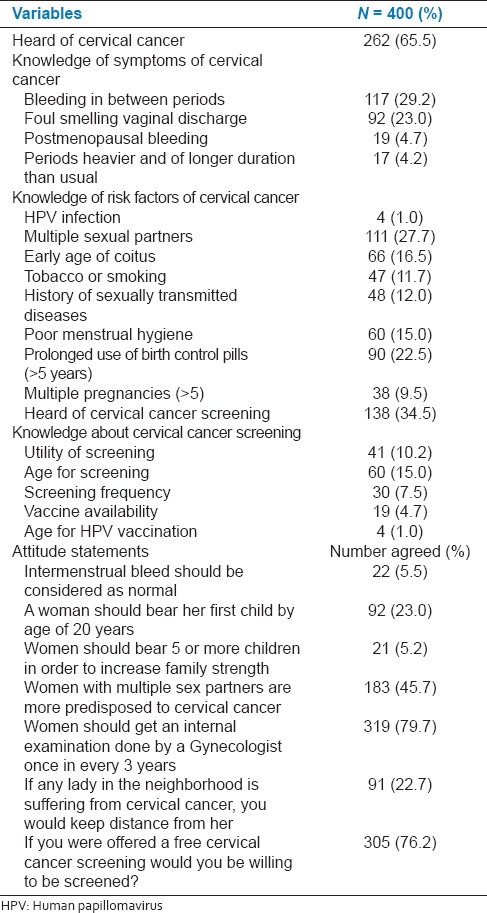
Despite the poor knowledge, majority participants expressed a positive attitude toward cervical cancer [Table 3]. About three-fourth (76.2%) women were willing to be screened if offered free of cost. However, the practice of screening for cervical cancer was poor as only 38 participants, that is, 9.5% women had ever been screened for cervical cancer [Table 2]. When enquired as to the major reason for nonscreening, majority of the participants responded that they were unaware of the screening test (65%) for cervical cancer. Furthermore, more than half of the respondents (58%) mentioned that they were asymptomatic, so it was pointless going for screening.
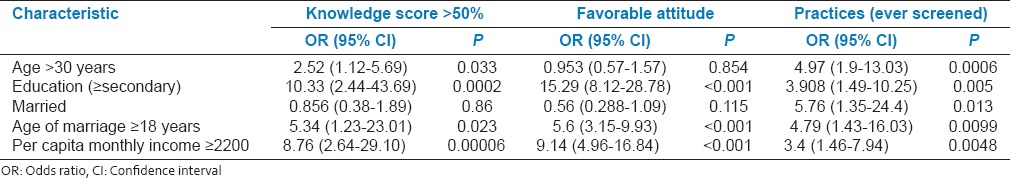
Results of binary logistic regression to identify predictors of optimum knowledge, favorable attitude, and practice (ever screened) are depicted in Table 4. Education, age, and income were independent predictors of better knowledge. Education level influences attitude towards screening and actual practice depends on age, income, and marital status.
Table 4.
Binary logistic regression for association of sociodemographic factors with optimal knowledge, favorable attitude, and practice
DISCUSSION
Our study shows suboptimal level of knowledge regarding cervical cancer but favorable attitude for screening. In our study, 65.5% women had “heard” about cervical cancer. Similar results were reported by Tran et al. and Shrestha et al. in Korea and Nepal respectively.[12,13] Only 11% women had adequate knowledge about carcinoma cervix and screening. The findings are similar to studies done in Cameroon by Tebeu et al.[14] and in Ethiopia by Yifru and Asheber.[15] However, the level of knowledge is far less than in developed countries (Study done in Kuwait[16] −52% had good knowledge and in London[17] −76% had adequate knowledge). The lack of knowledge is mainly due to lack of population-based screening programs, inefficient mass media campaigns, and cultural barriers wherein women in India feel shy to discuss the diseases affecting the sexual organs.
Intermenstrual bleeding was the commonly mentioned symptom among study participants. This finding is similar to study done in Kerala[6] and Ahmedabad.[18] The most common risk factor mentioned was multiple sexual partners. James John and Robin Marie Beining have reported similar findings in his dissertation submitted to the Muhimbili University of Health and Allied Sciences, Songea in 2011 and The University of Iowa in 2012, respectively.[19,20]
Our study has reported poor knowledge of cervical cancer screening similar results was shown by Shrestha et al. in Nepal.[13]
When attitude on cervical cancer and its screening was studied, 80.5% expressed a positive attitude toward cervical cancer and screening. Majority of women expressed willingness for screening if provided free of cost. These findings are consistent with studies done by Al Sairafi and Mohamed in Kuwait.[16] This is an advantage as we do not have to convince the women. One of the women is made aware of the disease and screening services offered free of cost, we would get a marked rise in screening coverage.
Only 9.5% of women had undergone screening. These results are comparable with the study by Shrestha et al. in Nepal.[13] This was slightly higher than the rest of India probably due to study being conducted in a tertiary care hospital and also about 65% women had secondary or higher level of education. Lack of awareness of screening test and absence of symptoms were the most common reasons for not undergoing screening. This is similar to a study done in Kerala[6] and Ethiopia.[15]
Further association was found between sociodemographic characteristics and knowledge, attitude, and practice. On multivariate analysis, it was found that women with age >30, secondary or higher level of education and those who were either employed or students were more likely to have adequate knowledge. This may be because with advancing age women are more exposed to health centers hence they get to know more about the disease from the health care providers. Also women who are employed or students have a greater opportunity for social interaction hence they get to know more about the disease.
The study participants with higher per capita family monthly income and those with higher education level were more likely to have a positive attitude toward cervical cancer.
Women with age >30 and education level >secondary are more likely to execute positive practice of screening for cervical cancer. This may be because as the age advances women are more likely to approach health care facility for different types of reproductive morbidities when opportunistic screening is also done. Also women with higher education level are more likely to know about the benefits of screening and hence better practice.
CONCLUSION AND RECOMMENDATIONS
This study shows that despite the fact that women had suboptimal level of knowledge regarding cervical cancer, their attitude is favorable for screening. However, uptake is low in actual practice. Strategic communication targeting eligible women, universal availability of screening facilities in public health facilities may increase the uptake of screening.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Kumar V, Abbas AK, Fausto N, Mitchell RN, editors. 8th ed. Philadelphia: Saunders Elsevier; 2007. Robbins Basic Pathology. [Google Scholar]
- 2.Kaku M, Mathew A, Rajan B. Impact of socio-economic factors in delayed reporting and late-stage presentation among patients with cervix cancer in a major cancer hospital in South India. Asian Pac J Cancer Prev. 2008;9:589–94. [PubMed] [Google Scholar]
- 3.Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189:12–9. doi: 10.1002/(SICI)1096-9896(199909)189:1<12::AID-PATH431>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 4.Gadducci A, Barsotti C, Cosio S, Domenici L, Riccardo Genazzani A. Smoking habit, immune suppression, oral contraceptive use, and hormone replacement therapy use and cervical carcinogenesis: A review of the literature. Gynecol Endocrinol. 2011;27:597–604. doi: 10.3109/09513590.2011.558953. [DOI] [PubMed] [Google Scholar]
- 5.Canavan TP, Doshi NR. Cervical cancer. Am Fam Physician. 2000;61:1369–76. [PubMed] [Google Scholar]
- 6.Aswathy S, Quereshi MA, Kurian B, Leelamoni K. Cervical cancer screening: Current knowledge & practice among women in a rural population of Kerala, India. Indian J Med Res. 2012;136:205–10. [PMC free article] [PubMed] [Google Scholar]
- 7.Fylan F. Screening for cervical cancer: A review of women's attitudes, knowledge, and behaviour. Br J Gen Pract. 1998;48:1509–14. [PMC free article] [PubMed] [Google Scholar]
- 8.Mosavel M, Simon C, Oakar C, Meyer S. Cervical cancer attitudes and beliefs-a Cape Town community responds on World Cancer Day. J Cancer Educ. 2009;24:114–9. doi: 10.1080/08858190902854590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rajkumar R, Sankaranarayanan R, Esmi A, Jayaraman R, Cherian J, Parkin DM. Leads to cancer control based on cancer patterns in a rural population in South India. Cancer Causes Control. 2000;11:433–9. doi: 10.1023/a:1008900425151. [DOI] [PubMed] [Google Scholar]
- 10.Lyon, France: IARC; 2013. [Last accessed on 2015 Feb 17]. International Agency for Research on Cancer. GLOBOCAN 2012: Estimated cancer incidence, mortality and prevalence worldwide in 2012. Available from: http://www.globocan.iarc.fr/ [Google Scholar]
- 11.Curado MP, Edwards B, Shin HR, Storm H, Ferlay J, Heanue M, et al., editors. IX. Lyon: IARC Scientific Publications; 2007. Cancer Incidence in Five Continents. [Google Scholar]
- 12.Tran NT, Choe SI, Taylor R, Ko WS, Pyo HS, So HC. Knowledge, attitude and practice (KAP) concerning cervical cancer and screening among rural and urban women in six provinces of the Democratic People's Republic of Korea. Asian Pac J Cancer Prev. 2011;12:3029–33. [PubMed] [Google Scholar]
- 13.Shrestha J, Saha R, Tripathi N. Knowledge, attitude and practice regarding cervical cancer screening amongst women visiting tertiary centre in Kathmandu, Nepal. Nepal J Med Sci. 2013;2:85–90. [Google Scholar]
- 14.Tebeu PM, Major AL, Rapiti E, Petignat P, Bouchardy C, Sando Z, et al. The attitude and knowledge of cervical cancer by Cameroonian women; a clinical survey conducted in Maroua, the capital of Far North Province of Cameroon. Int J Gynecol Cancer. 2008;18:761–5. doi: 10.1111/j.1525-1438.2007.01066.x. [DOI] [PubMed] [Google Scholar]
- 15.Yifru T, Asheber G. Knowledge, attitude and practice of screening for carcinoma of the cervix among reproductive health clients at three teaching hospitals, Addis Ababa, Ethiopia. Ethiop J Reprod Health. 2008:2. [Google Scholar]
- 16.Al Sairafi M, Mohamed FA. Knowledge, attitudes, and practice related to cervical cancer screening among Kuwaiti women. Med Princ Pract. 2009;18:35–42. doi: 10.1159/000163044. [DOI] [PubMed] [Google Scholar]
- 17.Yu CK, Rymer J. Women's attitudes to and awareness of smear testing and cervical cancer. Br J Fam Plann. 1998;23:127–33. [PubMed] [Google Scholar]
- 18.Goyal A, Gunvant V, Shrivastava A, Verma R, Modi A. Knowledge, attitude & practices about cervical cancer and screening among nursing staff in a teaching hospital. Int J Med Sci Public Health. 2013;2:249–53. [Google Scholar]
- 19.John J. The Knowledge, attitude, practice and perceived barriers towards screening for premalignant lesions among women aged 18 years and above in Songea Urban, Ruvama [dissertation] Muhimbili Univ Health Allied Sci. 2011 [Google Scholar]
- 20.Beining RM. Screening for cervical cancer: An exploratory study of urban women in Tamil Nadu, India [dissertation] University of Lowa. 2012 [Google Scholar]


