Abstract
Background and Objective:
The safety of Mn2O3 nanoparticles (which are extensively used in industries) on male reproductive system is not known. Hence, we investigated the effects of Mn2O3 nanoparticles on male reproductive system.
Materials and Methods:
A total of 40 Wistar adult male rats were randomly assigned to four groups of 10 rats each. Three groups received Mn2O3 solution in concentrations of 100, 200, and 400 ppm orally for 14 days; the control group received equal volume of saline solution. Blood samples and testicles were collected for analysis.
Results:
Significant reduction in luteinizing hormone (LH), follicle-stimulating hormone (FSH), testosterone, spermatogonial cells, primary spermatocyte, spermatid and Leydig cell was observed in the Mn2O3 nanoparticles treated groups compared with controls.
Conclusion:
Mn2O3 nanoparticles significantly reduce FSH, LH, and testosterone levels resulting in a significant reduction in testicular cytology.
Keywords: Follicle-stimulating hormone, luteinizing hormone, Mn2O3 nanoparticles, testosterone, toxicity
INTRODUCTION
The advancement in nanotechnology and wide application of nanomaterials have collaterally increased the human exposure to these particles raising concerns on their potential health hazards.[1,2,3] Although a few studies have evaluated the systemic toxicity and distribution of the nanoparticles[4] the diversified nature of nanoparticles requires a through and system specific evaluation. Moreover, the nature of toxicity of nanoparticles, is significantly dose-dependent.[5] Various forms of Mn2O3 nanoparticles (tube, wire, plate, sphere and nanoshell shapes) are developed,[6,7] with varying toxic effects. The characteristics of these nanoparticles are influenced by their size.[8,9,10] Mn2O3 including MnO, MnO2, Mn3O4 are used as a composite in wastewater treatment, catalyzing, sensors, super capacitors, alkaline, and battery recharging.[11,12,13,14,15] However, in addition to the advantages of nanoparticles in today's industrial applications, the exposure and toxicity of these nanoparticles to human and animal health are collateral,[16] which necessitates understanding the system specific toxic effects of these nanoparticles. Hence the present study was designed to investigate the effects of Mn2O3 nanoparticles on the levels of testosterone (T), follicle-stimulating hormone (FSH), luteinizing hormone (LH), and the testicle cytology of male mice. Bar-shaped nanoparticles with an approximate diameter of 70 nm were used in our study. LH in males stimulates a specific type of Leydig cells in testicles for the production of testosterone. The LH level in the males is consistent after puberty. The increase in testosterone levels gives a negative feedback to the pituitary gland and hypothalamus glands, which results in a decrease of LH secretion. LH secretions and FSH levels for testosterone are the primary tests used for the work-up on infertility in males and females patients.[17]
MATERIALS AND METHODS
Materials
Mn (III) acetylacetonate, Acetone, ethanol, and chloroform were used to prepare nanoparticles. Saline, ketamine, Rat chow, hematoxylin eosin, and laboratory kit (DB52181, MercK. Co., of Germany) were used.
Equipments
X-ray diffraction (XRD), transmission electron microscopy (TEM) (JEM-200CX), ultraviolet (UV)-visible, optical microscope (OLYMPUS CX 21 FS1), and ELISA Reader (HumaReader HS by HUMAN Co., Germany) was used.
Preparation of Mn2O3
Mn2O3 nanoparticles were first synthesized by providing heat to Mn (III) acetylacetonate (1 mmol, 0.35 g) in 20 mL acetone or ethanol in a Teflon-lined Parr acid-digestion bomb at 200°C for 72 h. The resulting dark solution was distributed into chloroform and centrifuged for 10 min. The residual black solution obtained was isolated and dried under vacuum condition at room temperature for 12 h, following which the calcination process was conducted at 500°C for 4 h. The final product was analyzed by XRD, UV-visible, and TEM (JEM-200CX).
Methods
Totally 40 male Wistar rats weighing 230 ± 20 g were housed at appropriate temperature/light conditions, and were fed standard prepared food consisting of 20% protein, 50% carbohydrate, 10% cellulose, 15% fat and vitamins. The study was approved by the Institute Ethics Committee. Rats were procured from the Isfahan University of Medical Sciences. The rodents were randomly assigned to four groups consisting of 10 rats each. The test-groups 1, 2, 3 received Mn2O3 nanoparticle solution in 100, 200, and 400 ppm concentrations respectively for 14 days by orally (gavage), and group 4 as the control-group, which received an oral saline placebo. Applied Mn2O3 Nps in this research were of 70 nm diameter. At the end of the trial, the mice were first anesthetized by ketamine and autopsied. For hormone evaluation, the arterial blood samples were collected from the heart and analyzed by commercial ELISA kits (pars azmon). The testicles together with epididymis were dissected and removed and transferred into a physiological saline for further investigation on cellular modifications using an optical microscope. Five different sites from any section were selected and in any field a cross-section of seminiferous tubules was studied. Investigative measurements and cell numerations (spermatogonial cells, primary spermatocyte, spermatid, and Leydig cell) were performed. The raw data were analyzed by SPSS.19 statistical analysis software using ANOVA and Dunnett tests. Statistically, variation of results among observed groups was considered significant at P < 0.05.
Tissue processing
Five different sites from each section with a thickness of 2 mm were selected and in any field, and a cross-section of seminiferous tubules was studied. The tissue was fixed in 10% Formalin and processed in various grades of ethanol, xylene, chloroform, toluene eventually for paraffin embedding. The paraffin embedded tissue was sectioned using a microtome, and the tissue section was mounted on a glass slide for staining using hematoxylin and eosin.[18]
RESULTS
X-ray diffraction of Mn2O3 nanoparticles
The XRD pattern for Mn2O3 is illustrated Figure 1, and diffraction peaks absorbance is at 2θ values. Dominant peaks are used to estimate grain size of sample contributed by Scherrer equation,[19] D = Kλ/ (β cos θ) where K is constant (0.9), λ is the wavelength (λ = 1.5418 A°) (Cu Kα), β is the full width at the half-maximum of the line and θ is the diffraction angle. Estimated grain size were found to be ±70 nM using relative intensity peak for Mn2O3 nanoparticles and increase in sharpness of XRD peaks implies that particles are crystal shape in nature. All peaks in Figure 1 are associated with Mn2O3 nanoparticles and consistent with Joint Committee for Powder Diffraction Studies.[19]
Figure 1.
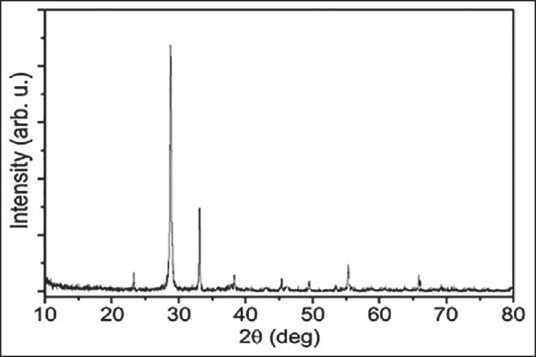
X-ray diffraction pattern for Mn2O3 nanoparticles
Size distribution and microscopic characterization of Mn2O3 nanoparticles
A particle size analyzer was applied to determine the area of sizes of the Mn2O3 nanoparticles. Figure 2 demonstrates the size dispersion of one of the arranged Mn2O3 nanoparticles. The mean size of the Mn2O3 nanoparticles was around 70 ± 5 nm.
Figure 2.
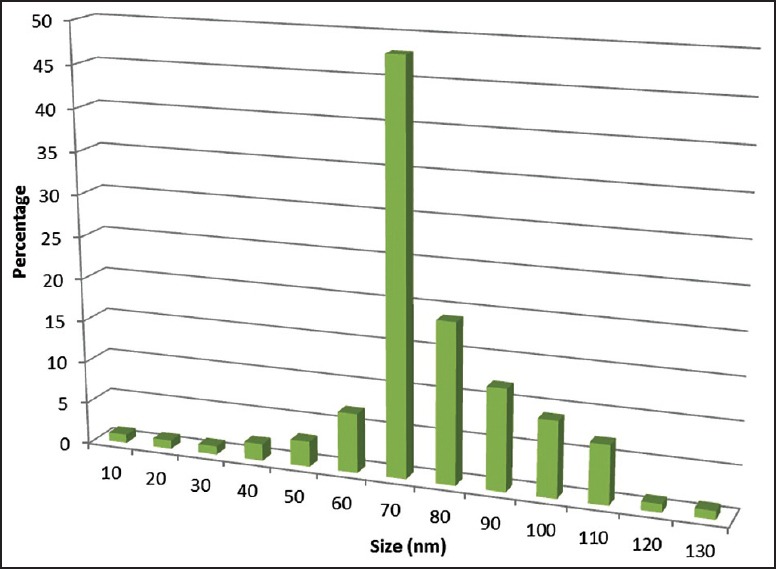
Size distribution of Mn2O3 nanoparticles
The properties of a wide variety of materials and function of many devices highly depend on their surface characteristics.[20] The morphology of Mn2O3 nanoparticles was studied by applying TEM). Figure 3 show the images of sample by TEM.
Figure 3.
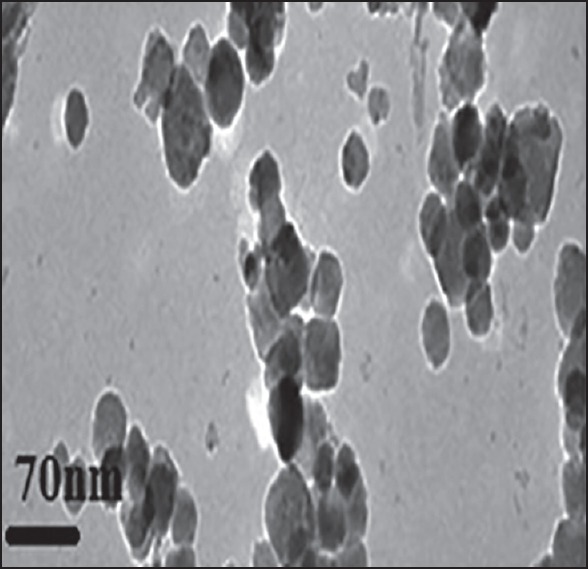
Transmission electron microscopy image of Mn2O3 nanoparticles
Mn2O3 nanoparticles caused a in the testosterone (P = 0.001), LH (P = 0.004) and FSH (P = 0.01) levels in-group receiving 400 ppm of Mn2O3 [Figure 4a–c].
Figure 4.
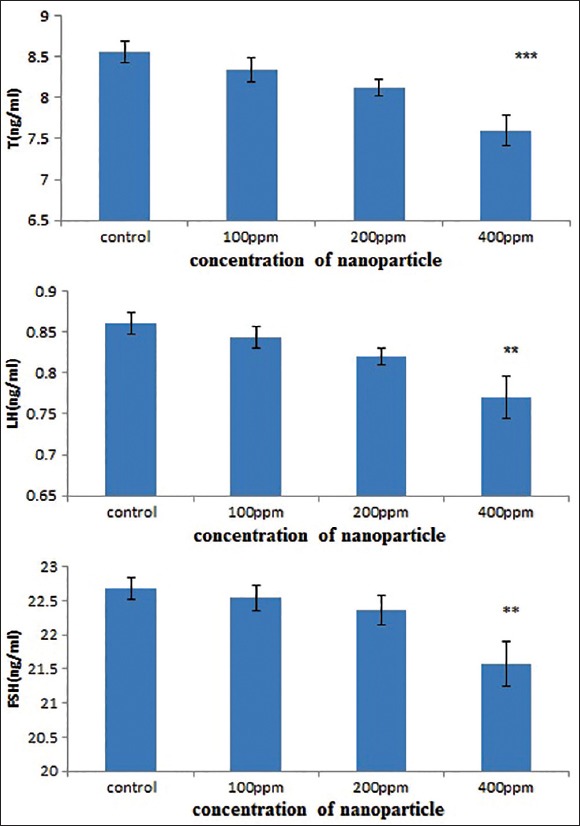
Mn2O3 nanoparticles effect on sex hormones
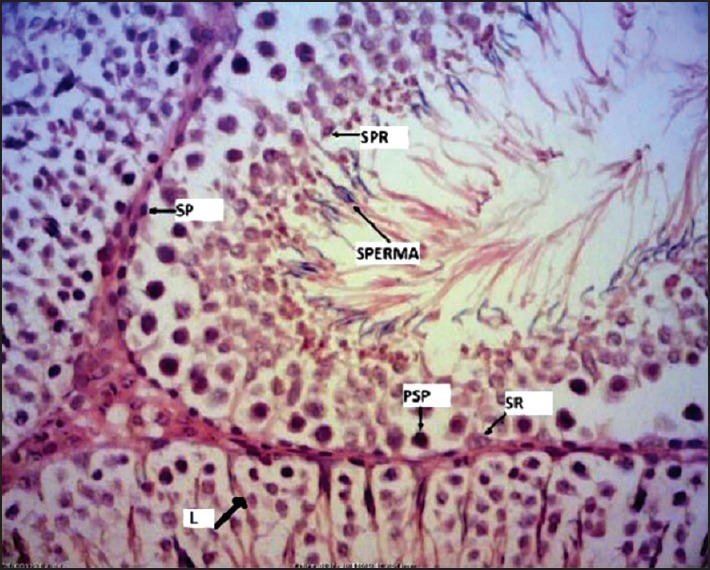
Significant reduction in the number of spermatogonial cells (P = 0.007), primary spermatocyte cells (P = 0.000) and spermatid cells (P = 0.002) was observed receiving 400 ppm Mn2O3 nanoparticles [Figures 5a–c and 6].
Figure 5.
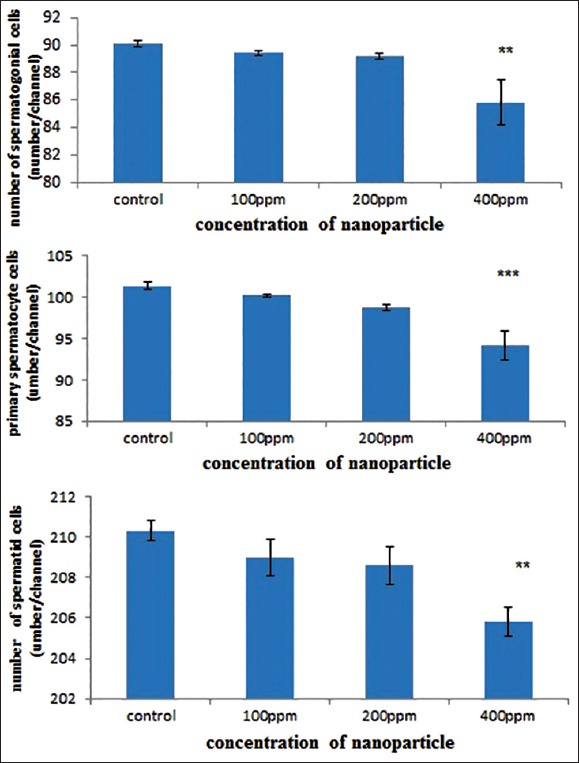
Mn2O3 nanoparticles, effect on testicle cell number
Figure 6.
The number of cells in seminiferous tubules. The structure of rat testis tissue controls (H and E, ×40). SP: spermatogonial cells, PSP: primary spermatocyte cells, SPR: Spermatid cells, L: Leydig cells, SPERMA: spermatozoide, SR: Sertoli cell
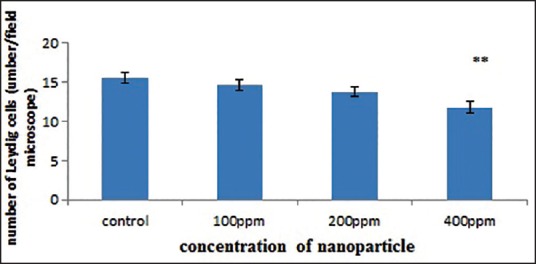
The number of Leydig cells in all groups decreased but were significant in the group receiving 400 ppm dosage (P = 0.003) [Figures 6 and 7].
Figure 7.
Mn2O3 nanoparticles, effect on number of Leydig cells
In this investigation, the pathological studies demonstrated 400 ppm dosage leads to
An increase in cellular disruption in the seminiferous tubules,
Interstitial edema of seminiferous tubules,
Appearance of vacuoles in epithelium and
A reduction in cell regulation, as shown in Figure 6a.
Irregularities were discovered in germinal cells levels, seminiferous tubules, and thickness reduction of epithelium was observed [Figure 8c]. In the group receiving 200 ppm Mn2O3 nanoparticles, the elevation in cellular disruption of seminiferous tubules was partially obvious. These comparisons were made with the control group [Figure 8d].
Figure 8.
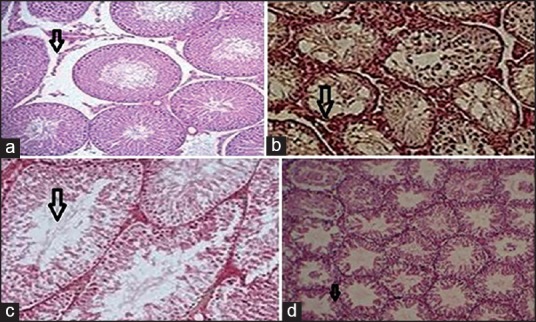
Effects of Mn2O3 nanoparticles over the damage of testis. (a) Arrows show elevation in cellular disruption of seminiferous tubules, interstitial edema, and decline in cell regulation were observed by H and E (×10). (b) Arrows show chaos in the germinal cells level in seminiferous tubules, increased in the gap between seminiferous tubular, and vacuoles seen in epithelium by H and E (×10). (c) Arrows indicate elevation in diameter of seminiferous tubules and decline in epithelium diameter were observed, H and E (×10). (d) Arrows indicate images of seminiferous tubules in the control-group demonstrated uniformity of the seminiferous tubules were seen, H and E (×10)
DISCUSSION
The effect of oral intake of Mn2O3 nanoparticles in 100, 200, and 400 ppm concentrations on testosterone, LH, FSH, spermatogonial cells, primary spermatocyte, spermatid, Leydig and pathological modifications in the testicle tissue were evaluated. Mn2O3 nanoparticles caused malignancies in the testicular tissue, a decrease in the levels of the sex hormones, and spermatogonial cells, primary spermatocyte, spermatid, and Leydig cells at the dose of 400 ppm. Mn2O3 in nanoscale may produce active oxygen that results in toxicity via oxidative stress, producing a variety of active oxygen is the dominant mechanism of toxicity raised from Mn2O3 nanoparticles. Several studies have demonstrated that cells exposed to Mn2O3 nanoparticles, have a lower mitochondrial activity, leading to severe tissue damage.[21,22,23,24] Nanoparticles have severe toxic effects on the male reproduction system by trespassing the blood barrier in the testicular tissue and damage the sperm cells.[25] Nanoparticles have also been shown to be toxic on stem cells in vitro and can interference with male reproduction system.[26] Nanoparticles may also react with DNA and may lead to inflammation, oxidative stress and impairment in cell function.[27] Titanium nanoparticles were shown to result in infertile sperm, and abnormal Leydig cell[28] while other nanoparticles can accumulate in testicular tissue, including Leydig cell, sertoli cells, and spermatid.[17] The effects of Mn2O3 nanoparticles on sex hormone reduction observed in our study could be due to the above factors including direct toxic effects on testicular cytology.
CONCLUSION
We conclude that the Mn2O3 nanoparticles at a dose of 400 ppm can reduce sex hormones, sperm production and damage the testicular cytology.
ACKNOWLEDGMENT
We would like to thank Mr. Sadeghi for helping us in this study.
Footnotes
Source of Support: Expenses of this work were discharged by authors.
Conflict of Interest: None declared.
REFERENCES
- 1.Mirkovic B, Turnsek TL, Kos J. Nanotechnology in the treatment of cancer. Zdravniski Vestnik. 2010;79(2) [Google Scholar]
- 2.Gupta AK, Gupta M. Synthesis and surface engineering of iron oxide nanoparticles for biomedical applications. Biomaterials. 2005;26:3995–4021. doi: 10.1016/j.biomaterials.2004.10.012. [DOI] [PubMed] [Google Scholar]
- 3.Pankhurst QA, Connolly J, Jones S, Dobson J. Applications of magnetic nanoparticles in biomedicine. J Phys D Appl Phys. 2003;36:167–81. [Google Scholar]
- 4.Almeida JP, Chen AL, Foster A, Drezek R. In vivo biodistribution of nanoparticles. Nanomedicine (Lond) 2011;6:815–35. doi: 10.2217/nnm.11.79. [DOI] [PubMed] [Google Scholar]
- 5.Kong B, Seog JH, Graham LM, Lee SB. Experimental considerations on the cytotoxicity of nanoparticles. Nanomedicine (Lond) 2011;6:929–41. doi: 10.2217/nnm.11.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ghosh M, Biswas K, Sundaresan A, Rao C. MnO and NiO nanoparticles: Synthesis and magnetic properties. J Mater Chem. 2006;16:106–11. [Google Scholar]
- 7.Liu R, Duay J, Lee SB. Redox exchange induced MnO2 nanoparticle enrichment in poly (3, 4-ethylenedioxythiophene) nanowires for electrochemical energy storage. ACS Nano. 2010;4:4299–307. doi: 10.1021/nn1010182. [DOI] [PubMed] [Google Scholar]
- 8.Shumakova AA, Trushina ÉN, Mustaphina OK, Soto SKh, Gmoshinskii IV, Khotimchenko SA. Influence of titanium dioxide and silica nanoparticles on accumulation and toxicity of lead in experiments with intragastric co-administration. Vopr Pitan. 2014;83:57–63. [PubMed] [Google Scholar]
- 9.Lee GH, Huh SH, Jeong JW, Choi BJ, Kim SH, Ri HC. Anomalous magnetic properties of MnO nanoclusters. J Am Chem Soc. 2002;124:12094–5. doi: 10.1021/ja027558m. [DOI] [PubMed] [Google Scholar]
- 10.Yin M, O’Brien S. Synthesis of monodisperse nanocrystals of manganese oxides. J Am Chem Soc. 2003;125:10180–1. doi: 10.1021/ja0362656. [DOI] [PubMed] [Google Scholar]
- 11.Seo WS, Jo HH, Lee K, Kim B, Oh SJ, Park JT. Size-dependent magnetic properties of colloidal Mn(3)O(4) and MnO nanoparticles. Angew Chem Int Ed Engl. 2004;43:1115–7. doi: 10.1002/anie.200352400. [DOI] [PubMed] [Google Scholar]
- 12.Park J, Kang E, Bae CJ, Park JG, Noh HJ, Kim JY, et al. Synthesis, characterization, and magnetic properties of uniform-sized MnO nanospheres and nanorods. J Phys Chem B. 2004;108:13594–8. [Google Scholar]
- 13.Park J, An K, Hwang Y, Park JG, Noh HJ, Kim JY, et al. Ultra-large-scale syntheses of monodisperse nanocrystals. Nat Mater. 2004;3:891–5. doi: 10.1038/nmat1251. [DOI] [PubMed] [Google Scholar]
- 14.Richardson J, Yiagas D, Turk B, Forster K, Twigg M. Origin of superparamagnetism in nickel oxide. J Appl Phys. 1991;70:6977–82. [Google Scholar]
- 15.Bødker F, Hansen MF, Koch CB, Lefmann K, Mørup S. Magnetic properties of hematite nanoparticles. Phys Rev B. 2000;61:6826. [Google Scholar]
- 16.Dobrzynska MM, Gajowik A, Radzikowska J, Lankoff A, Dušinská M, Kruszewski M. Genotoxicity of silver and titanium dioxide nanoparticles in bone marrow cells of rats in vivo. Toxicology. 2014;315:86–91. doi: 10.1016/j.tox.2013.11.012. [DOI] [PubMed] [Google Scholar]
- 17.Fartkhooni FM, Noori A, Momayez M, Sadeghi L, Shirani K, Babadi VY. The effects of nano titanium dioxide (TiO 2) in spermatogenesis in wistar rat. Eur J Exp Biol. 2013;3:145–9. [Google Scholar]
- 18.Ayala E, Enghardt MH, Horton M. Cost effective, environmentally safe tissue processing method with paraffin oil. J Histotechnol. 1997;20:133–7. [Google Scholar]
- 19.Monico L, Van der Snickt G, Janssens K, De Nolf W, Miliani C, Verbeeck J, et al. Degradation process of lead chromate in paintings by Vincent van Gogh studied by means of synchrotron X-ray spectromicroscopy and related methods 1. Artificially aged model samples. Anal Chem. 2011;83:1214–23. doi: 10.1021/ac102424h. [DOI] [PubMed] [Google Scholar]
- 20.Van Ruitenbeek J, Alvarez A, Pineyro I, Grahmann C, Joyez P, Devoret M, et al. Adjustable nanofabricated atomic size contacts. Rev Sci Instrum. 1996;67:108–11. [Google Scholar]
- 21.Erikson KM, Dobson AW, Dorman DC, Aschner M. Manganese exposure and induced oxidative stress in the rat brain. Sci Total Environ. 2004;334-335:409–16. doi: 10.1016/j.scitotenv.2004.04.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stokes AH, Lewis DY, Lash LH, Jerome WG, 3rd, Grant KW, Aschner M, et al. Dopamine toxicity in neuroblastoma cells: Role of glutathione depletion by L-BSO and apoptosis. Brain Res. 2000;858:1–8. doi: 10.1016/s0006-8993(99)02329-x. [DOI] [PubMed] [Google Scholar]
- 23.Calne DB, Chu NS, Huang CC, Lu CS, Olanow W. Manganism and idiopathic parkinsonism: Similarities and differences. Neurology. 1994;44:1583–6. doi: 10.1212/wnl.44.9.1583. [DOI] [PubMed] [Google Scholar]
- 24.Cohen G, Spina MB. Deprenyl suppresses the oxidant stress associated with increased dopamine turnover. Ann Neurol. 1989;26:689–90. doi: 10.1002/ana.410260518. [DOI] [PubMed] [Google Scholar]
- 25.McAuliffe ME, Perry MJ. Are nanoparticles potential male reproductive toxicants? A literature review. Nanotoxicology. 2007;1:204–10. [Google Scholar]
- 26.Braydich-Stolle L, Hussain S, Schlager JJ, Hofmann MC. In vitro cytotoxicity of nanoparticles in mammalian germline stem cells. Toxicol Sci. 2005;88:412–9. doi: 10.1093/toxsci/kfi256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nel A, Xia T, Mädler L, Li N. Toxic potential of materials at the nanolevel. Science. 2006;311:622–7. doi: 10.1126/science.1114397. [DOI] [PubMed] [Google Scholar]
- 28.Ema M, Kobayashi N, Naya M, Hanai S, Nakanishi J. Reproductive and developmental toxicity studies of manufactured nanomaterials. Reprod Toxicol. 2010;30:343–52. doi: 10.1016/j.reprotox.2010.06.002. [DOI] [PubMed] [Google Scholar]


