Abstract
A case of a 42-year-old man with back pain associated with left radiculopathy and infiltrative mass involving the T12 and L5 vertebrae is described. Magnetic resonance imaging (MRI) and computed tomography indicated aggressive hemangiomas involving the T12 and L5 vertebrae. Three-year follow-up by imaging indicated minimally increased aggressiveness of the L5 lesion without any significant change in appearance of the T12 lesion thus, confirming the initial diagnosis of multiple aggressive vertebral hemangiomas.
Keywords: Aggressive hemangioma, computed tomography, magnetic resonance, spine, vertebral hemangioma
INTRODUCTION
Vertebral hemangiomas, which are usually considered to be benign, are very commonly encountered lesions on spinal radiographs, computed tomography (CT), and magnetic resonance imaging (MRI). A very rare subtype of vertebral hemangiomas can extend outside bony margins leading to the expansion of the bone, disturbance of blood flow, and occasionally compression fractures and are hence classified as aggressive hemangiomas.
CASE REPORT
A 42-year-old Arab man presented with severe mid and low back pain and left radiculopathy of 5-months duration, which worsened rapidly during the two weeks prior to admission. History of multilevel cervical laminectomies and discectomies for disc herniation was observed. On presentation, neurologic examination was unremarkable with no ataxia, dysmetria, or dysdiadochokinesia.
Pre- and post-contrast MRI of the thoracic and lumbar spine performed, as the initial study based on the clinical signs, suggested multiple typical vertebral hemangiomas including at T12 and L5 levels. A T2 and STIR hyperintense, T1 hypointense, enhancing and expansile bony lesion with accompanying trabecular thickening was observed involving the entire T12 vertebral body extending into its posterior elements on the left side. In addition, the mass lesion extended into the bony spinal canal and left posterolateral paraspinal musculature causing compression of the thecal sac and the thoracic spinal cord at this level [Figure 1]. Marrow edema and enhancement of the L5 vertebral body and the left posterior elements with minimal extension of the enhancing soft tissue in the left spinal canal and the left paraspinal soft tissue was also observed [Figure 1]. Aggressive hemangiomas of T12 and L5 vertebrae were diagnosed based on these characteristic findings and follow-up with MRI was advised to exclude the less likely possibility of spinal metastases.
Figure 1.
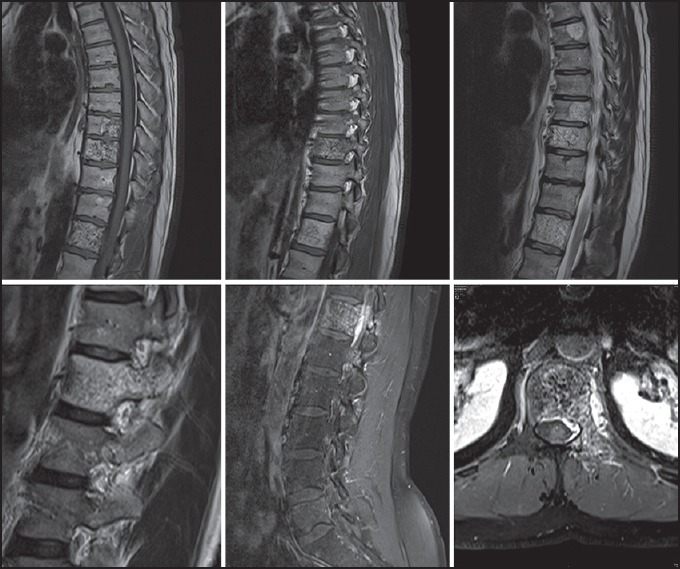
Magnetic resonance images demonstrating aggressive hemangiomas of T12 and L5 vertebral bodies
Non-contrast CT scan was performed 3 years after the initial presentation, which showed vertical and thick trabeculae involving the T12 and L5 vertebral bodies and the left posterior elements with expansion and irregularity of the bony cortex. Epidural soft tissue masses were also noticed at these vertebral levels. Peculiar “polka dot” appearance was seen on axial CT images and “corduroy cloth or jail bar” appearance was seen on sagittal and coronal reformatted CT images [Figure 2].
Figure 2.
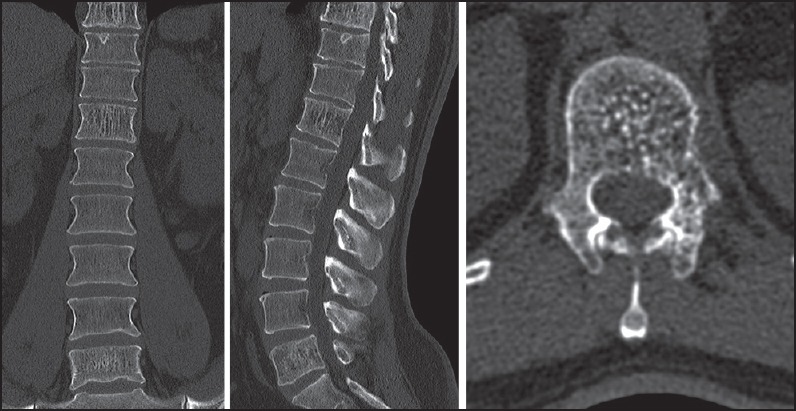
Computed tomography images demonstrating typical features of vertebral hemangiomas including at T12 and L5 levels
Follow-up MRI performed after one and 3 years, respectively, revealed no significant change in findings at the T12 vertebral level, however, minimally increased marrow edema and enhancement was observed at the L5 vertebral level, thus confirming the initial diagnosis of multiple aggressive vertebral hemangiomas [Figure 3a and b].
Figure 3.
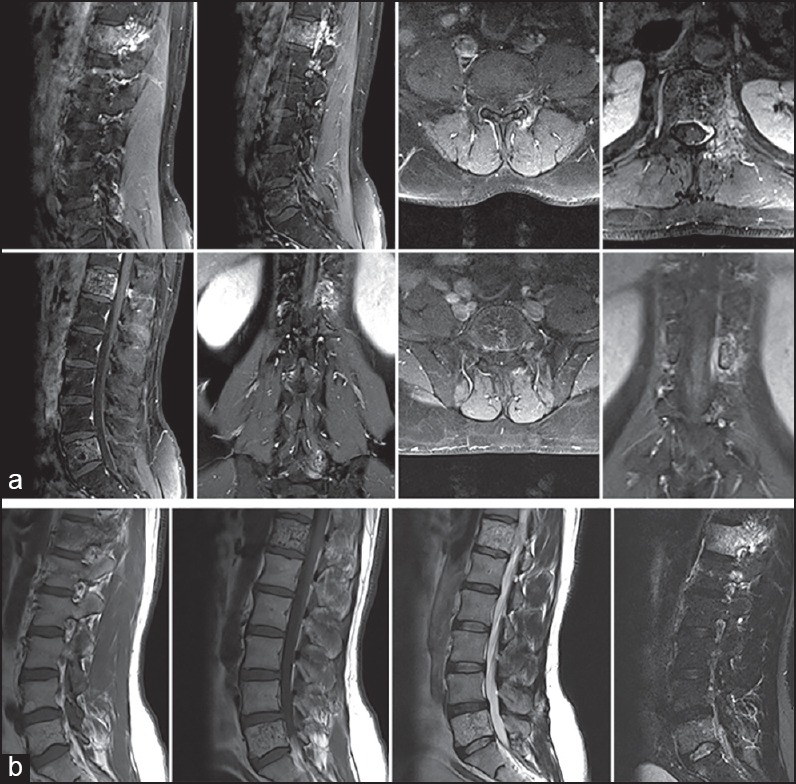
Follow-up magnetic resonance images (MRI) 3a (top two rows of images) done after 1 year and 3b (bottom row of images) done after 3 years of initial MRI reveal no significant interval change in T12 lesion and minimally increased severity of L5 lesion
DISCUSSION
Vertebral hemangiomas are common benign lesions of the spine. They are found in approximately 10-12% of autopsies and radiographs of the spine. Characteristically, the vertebral hemangiomas are incidentally observed in imaging studies. They are, however, symptomatic in almost 1% of adults[1,2] and are very rare in children.[2] These rare type of symptomatic lesions are known as aggressive hemangiomas and are characterized by expansion of the bone, extension outside bony margins, disturbance of local blood flow, and rarely vertebral compression fractures.[1,3] Approximately 45% of patients with aggressive vertebral hemangiomas have neurologic deficits, the rest suffer only from back pain.[3] Our case also had back pain only without any neurological deficits.
Imaging of vertebral hemangiomas revealed thick and vertical bony trabeculae, thus preserving the functional ability of the vertebrae to withstand an axial load. This appearance is described on radiographs and CT as “polka-dot”, “jail bar”, “corduroy cloth”, “salt and pepper”, and “honeycomb” with reduced overall density of the affected vertebral body secondary to the presence of fatty bone marrow.[4,5,7] Fatty tissue present within the hemangiomas can lead to hyperintensity on T1-weighted MRI while increased water content leads to hyperintensity on T2-weighted images.[6] The T2-hyperintensity is often greater than that of fat, thereby differentiating hemangiomas from focal fat deposition.[3,7] Aggressive hemangiomas characteristically have reduced fat content and more vascular component causing hypointensity on T1-weighted MRI.[1,4,8] This appearance may resemble vertebral metastasis, however, metastatic foci commonly reveal hypointensity on T1-weighted images and hyperintensity on T2-weighted images.[7] In addition, the morphology, including the presence of coarsened trabeculae can be used for differentiation.[7] For indeterminate cases, CT is helpful since the modality is more sensitive to the characteristic osseous remodeling.[3,9] Paget's disease of the spine can have similar appearance but is usually distinguished by expansion of the vertebral body with peripheral cortical thickening which can be observed on CT, with characteristic “picture frame” vertebral body on radiographs.[3,10] Lymphoma may also have a similar appearance but is usually distinguished by homogeneous enhancement on contrast enhanced MRI.[3,11] Aggressive vertebral hemangiomas most often occur between T3 and T9 vertebral segments.[3,12] They generally occupy the entire vertebral body, extend into the neural arch, expand the osseous margins, and contain a soft tissue component.[12] Cord compression and subsequent myelopathy may result from either encroachment of extradural soft tissue, pathologic fracture or hemorrhage.[3,13] Vertebral hemangiomas may become symptomatic during pregnancy due to increased intra-abdominal pressure and vascular redistribution of flow in the vertebral venous plexus when the uterus enlarges.[14]
The histologic pattern of osseous hemangiomas is characterized by the proliferation of anomalous thin-walled blood vessels and sinuses lined by endothelium between the thickened, vertically oriented trabeculae of bone.[3] The dilated vascular channels are set in a stroma of fat.[7] The ratio of fat to vascular tissue wrapped between the pillars of bone determines the signal intensity on MRI.[4]
Treatment options for symptomatic or aggressive hemangiomas without cord compression include vertebroplasty,[3,14,15] embolization, and sclerotherapy.[16] Surgical resection is reported to be relatively safe method for treatment of compressive vertebral hemangiomas[17] while radiation therapy may be used in cases of subtotal resection.[8,17]
Vertebral hemangiomas are most often benign, incidentally imaged lesions with a good prognosis; however, a rare subset of them can be aggressive with devastating neurologic sequela.[3] It is important for the clinician to keep aggressive hemangioma as a differential diagnosis in any patient presenting with myelopathic symptoms and obtain early imaging, especially MRI, in order to guide proper treatment.[3] As aggressive hemangiomas often mimic other aggressive spinal lesions, additional imaging modalities such as CT, angiography, and radiography are usually needed to make a definitive diagnosis.[3] We present here, a very rare case of multiple aggressive vertebral hemangiomas. To our knowledge, this type of presentation has not been reported in the published literature before.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Chen HI, Heuer GG, Zaghloul K, Simon SL, Weigele JB, Grady MS. Lumbar vertebral hemangioma presenting with the acute onset of neurological symptoms. Case report. J Neurosurg Spine. 2007;7:80–5. doi: 10.3171/SPI-07/07/080. [DOI] [PubMed] [Google Scholar]
- 2.Cheung NK, Doorenbosch X, Christie JG. Rapid onset aggressive vertebral haemangioma. Childs Nerv Syst. 2011;27:469–72. doi: 10.1007/s00381-011-1391-3. [DOI] [PubMed] [Google Scholar]
- 3.Schrock WB, Wetzel RJ, Tanner SC, Khan MA. Aggressive hemangioma of the thoracic spine. J Radiol Case Rep. 2011;5:7–13. doi: 10.3941/jrcr.v5i10.828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Laredo JD, Assouline E, Gelbert F, Wybier M, Merland JJ, Tubiana JM. Vertebral hemangiomas: Fat content as a sign of aggressiveness. Radiology. 1990;177:467–72. doi: 10.1148/radiology.177.2.2217787. [DOI] [PubMed] [Google Scholar]
- 5.Grossman RI, Yousem DY. Neuroradiology. 3rd ed. Philadelphia: Mosby; 2003. Nondegenerative diseases of the spine; pp. 827–8. [Google Scholar]
- 6.Ross JS, Masaryk TJ, Modic MT, Carter JR, Mapstone T, Dengel FH. Vertebral hemangiomas: MR imaging. Radiology. 1987;165:165–9. doi: 10.1148/radiology.165.1.3628764. [DOI] [PubMed] [Google Scholar]
- 7.Quinn S. Case Report. Vertebral Hemangioma. MRI Web Clinic. 2006. [Last accessed on 2011 Mar 02]. Available from: http://www.radsource.us .
- 8.Fox MW, Onofrio BM. The natural history and management of symptomatic and asymptomatic vertebral hemangiomas. J Neurosurg. 1993;78:36–45. doi: 10.3171/jns.1993.78.1.0036. [DOI] [PubMed] [Google Scholar]
- 9.Cross JJ, Antoun NM, Laing RJ, Xuereb J. Imaging of compressive vertebral haemangiomas. Eur Radiol. 2000;10:997–1002. doi: 10.1007/s003300051051. [DOI] [PubMed] [Google Scholar]
- 10.Smith SE, Murphey MD, Motamedi K, Mulligan ME, Resnik CS, Gannon FH. From the archives of the AFIP. Radiologic spectrum of Paget disease of bone and its complications with pathologic correlation. Radiographics. 2002;22:1191–216. doi: 10.1148/radiographics.22.5.g02se281191. [DOI] [PubMed] [Google Scholar]
- 11.Boukobza M, Mazel C, Touboul E. Primary vertebral and spinal epidural non-Hodgkin's lymphoma with spinal cord compression. Neuroradiology. 1996;38:333–7. doi: 10.1007/BF00596582. [DOI] [PubMed] [Google Scholar]
- 12.Laredo JD, Reizine D, Bard M, Merland JJ. Vertebral hemangiomas: Radiologic evaluation. Radiology. 1986;161:183–9. doi: 10.1148/radiology.161.1.3763864. [DOI] [PubMed] [Google Scholar]
- 13.Dickerman RD, Bennett MT. Acute spinal cord compression caused by vertebral hemangioma. Spine J. 2005;5:582–4. doi: 10.1016/j.spinee.2005.05.378. [DOI] [PubMed] [Google Scholar]
- 14.Guarnieri G, Ambrosanio G, Vassallo P, Pezzullo MG, Galasso R, Lavanga A, et al. Vertebroplasty as treatment of aggressive and symptomatic vertebral hemangiomas: Up to 4 years of follow-up. Neuroradiology. 2009;51:471–6. doi: 10.1007/s00234-009-0520-0. [DOI] [PubMed] [Google Scholar]
- 15.Galibert P, Déramond H. Percutaneous acrylic vertebroplasty as a treatment of vertebral angioma as well as painful and debilitating diseases. Chirurgie. 1990;116:326–34. [PubMed] [Google Scholar]
- 16.Doppman JL, Oldfield EH, Heiss JD. Symptomatic vertebral hemangiomas: Treatment by means of direct intralesional injection of ethanol. Radiology. 2000;214:341–8. doi: 10.1148/radiology.214.2.r00fe46341. [DOI] [PubMed] [Google Scholar]
- 17.Urrutia J, Postigo R, Larrondo R, Martin AS. Clinical and imaging findings in patients with aggressive spinal hemangioma requiring surgical treatment. J Clin Neurosci. 2011;18:209–12. doi: 10.1016/j.jocn.2010.05.022. [DOI] [PubMed] [Google Scholar]


