Abstract
Sellar masses are frequently adenomatous pituitary tumors. Metastatic disease is unusual, often mimicking the presentations of adenomas. Hepatocellular carcinoma (HCC) is the most common primary hepatic malignancy but unusual to have a pituitary metastasis (PM). A 65-year-old man presented with headache, diplopia, ptosis, decreased vision in the right eye and unintentional weight loss of 32lbs. Preliminary out-patient work-up revealed a mass in the pituitary region. Cranial imaging showed 3.1 cm × 3.2 cm × 4.4 cm lesion. Abdominal imaging (computed tomography and magnetic resonance imaging) demonstrated a lobulated, nodular and heterogeneous right lobe of the liver. Trans-sphenoidal resection of the sellar mass favored metastatic HCC on histology. Liver biopsy confirmed HCC. We recommend maintaining an increased clinical suspicion upon evaluation of nonclassical clinical and radiological presentations of suspected PM/malignancy; as well as pursuing additional investigations in all early cases.
Keywords: Hepatocellular carcinoma, metastasis, pituitary gland
INTRODUCTION
Sellar masses are most frequently primary pituitary tumors of the adenomatous type. Metastatic malignancies are an unusual clinical presentation.[1] However, metastatic disease (including isolated pituitary metastasis [PM]) may mimic the clinical, endocrinological and radio graphical presentations of primary pituitary adenomas (PA)[2] which are much more common. Differentiating between these lesions may be difficult. Hence, any unusual presentation or clinical course of a PA must raise suspicion for the possibility of PM and scull base metastasis with an undiagnosed primary tumor.[3,4]
Almost all types of malignancies can be detected in sellar masses, though most derive from primaries in the breast and lung cancer. PM account for about 1% of operative pituitary lesions. The prognosis of patients with PM is poor, with a mean survival of 6-7 months, due to the aggressiveness of the primary neoplasm. Of note, most pituitary metastases appear to be asymptomatic and therefore, metastatic involvement of the pituitary gland is most frequently found on autopsy specimens versus recognized clinically. In symptomatic/operative cases, metastases are initially suspected during surgery because of the atypical appearance of the tumor and confirmation of the diagnosis relies on the histological study.[5,6]
The clinical presentation of the sellar mass may help the differential diagnosis because visual field defects and anterior pituitary dysfunction are mostly found in pituitary macroadenomas. Although symptomatic metastases commonly present with diabetes insipidus, headache, hypopituitary syndromes, visual fields and extraocular palsies have also been reported. The clinical features of metastases correlate well with published reports showing that tumor metastases are more often found in the posterior lobe than in the anterior lobe, due to the different blood supplies.[2,3,4,5,6]
CASE REPORT
A 65-year-old Hispanic male with a pertinent medical history of hypertension, obesity, dyslipidemia, and diabetes mellitus who presented with progressive frontal and biparietal headache. The headache was associated with photophobia, diplopia, decreased visual acuity and ptosis of the right eye as well as, nausea and vomiting for 1-month. In addition, he reported an unintentional weight loss of 32 pounds over a 2-month period. On physical examination, he was found to have internuclear opthalmoplegia and pupil-sparing right third nerve palsy. He was unable to abduct his left eye past the midline laterally and had difficulty with upward as well as downward gaze, suggesting a sixth cranial nerve palsy. No additional cranial nerve deficits were present. He denied any personal or family history of malignancy or liver disease. He admitted to a 20-pack year history of smoking and alcohol use.
Prior to presenting at our facility for worsening of symptoms, the patient underwent an magnetic resonance imaging (MRI) of the brain [Figures 1, 2a and b], which showed a mass in the pituitary region involving the sella as well as the clivus. Further diagnostic work-up, showed no abnormality in prolactin, thyroid-stimulating hormone, follicle-stimulating hormone, luteinizing hormone, or adrenocorticotropic hormone. In view of this hormonal inactivity, the patient's intracranial mass was unlikely to be a PA and alternate diagnoses including meningoma, chordoma, and metastasis were considered. The patient was placed on decadron to decrease intracranial pressure and underwent further evaluation for tumor diagnosis. His work-up included a coagulation profile demonstrating PT 14.0, international normalized ratio 1.1. Liver function studies reflected an albumin of 3.9, total bilirubin of 1.1, total protein 7.6, alkaline phosphatase 156, aspartate aminotranferase 113, and alanine aminotransferase 186. Hepatitis panel was uniformly negative for active hepatitis A, B and C, but did show evidence of prior exposure to hepatitis A and B. An extensive autoimmune work-up for cirrhosis were all within normal limits except antismooth muscle antibodies was borderline positive. Tumor marker screening including alpha-fetoprotein, prostate-specific antigen, CA 19-9, and carcinoembryonic antigen exhibited no abnormalities.
Figure 1.
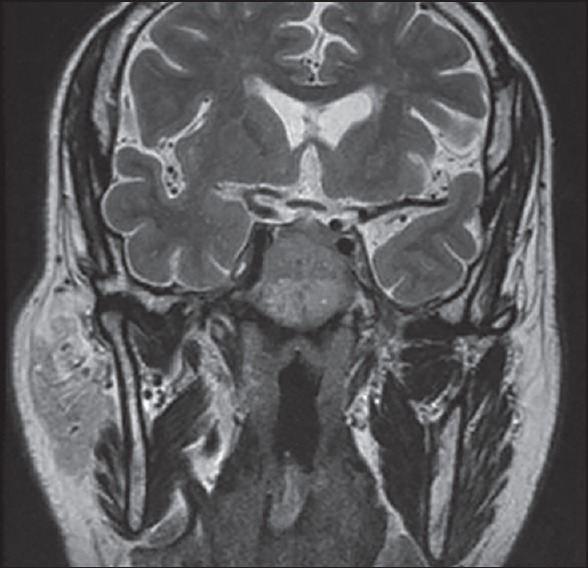
Magnetic resonance imaging pitutary coronal T2-weighted sequence demonstrating an iso-intense mass of the clivus displacing the normal pituitary gland cephalad. The mass does not extend to the level of the optic chiasm but does displace the infundibulum slightly leftward
Figure 2.
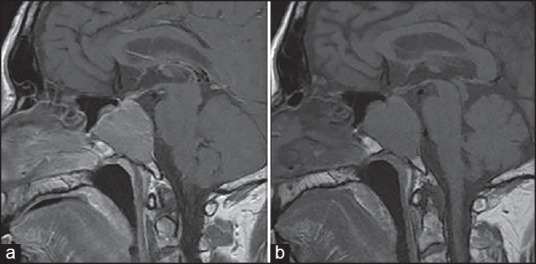
Magnetic resonance imaging pituitary with and without contrast post (a) and pre-contrast (b) (respectively) sagittal T1-weighed images without fat suppression showing a large heterogeneous 3.1 cm × 3.2 cm × 4.4 cm enhancing mass expanding the clivus and displacing the normal pituitary gland. The mass does have some pituitary extension displacing the normal pituitary gland cephalad, but is likely separate from the pituitary gland
A repeat MRI revealed the mass measured 3.1 cm × 3.2 cm × 4.4 cm and originated from the clivus extending into the pituitary gland and displacing it cephalad, but with no extension to the optic chiasm. It affected the infundibulum pushing it leftward, with slight insinuation at the cavernous sinus. Heterogeneous enhancement with a central vascular area was seen, and there was effacement of the undersurface of the sphenoid sinuses, but no noted hydrocephalus. Subsequent computed tomography (CT) scan of the chest, abdomen, and pelvis performed with intravenous contrast, showed a nodular contour of the right side of the liver with multiple ill-defined hypodense lesions, which was highly suspicious for a multifocal hepatocellular carcinoma (HCC). An abdominal MRI [Figure 3a and b] was performed with contrast, which showed a lobulated, nodular and heterogeneous appearance of the entire right lobe of the liver, which demonstrated abnormal contrast enhancement during the arterial phase. The left lobe of the liver was relatively unaffected.
Figure 3.
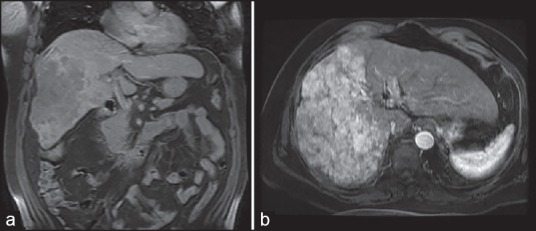
(a) Magnetic resonance imaging of the abdomen Coronal Single Shot Fast Spin Echo T2-weighted sequences showing a heterogeneous large bright T2 signal mass occupying most of the right lobe of the liver, (b) Magnetic resonance imaging of the abdomen coronal spoiled gradient T1-weighted post contrast image showing large mass with nodular heterogeneous boarders. The mass is hypointense relative to liver parenchyma
In the light of the patients sellar mass associated with liver disease, metastatic hepatic etiologies rose to the top of the differential and HCC in particular, was strongly suspected. Subsequently, the patient underwent the trans-sphenoidal resection of the sellar mass using neuronavigation, with significant tumor debulking. Grossly, the tumor was consistent with a soft macroadenoma and consisted of delicate tan-pink and friable tissue. Intraoperative frozen sections [Figures 4, 5a and b] confirmed metastatic HCC. Subsequently, a liver biopsy of the affected area was obtained and was consistent with HCC. This confirmed the suspected clinicopathologic diagnosis of PM from HCC.
Figure 4.
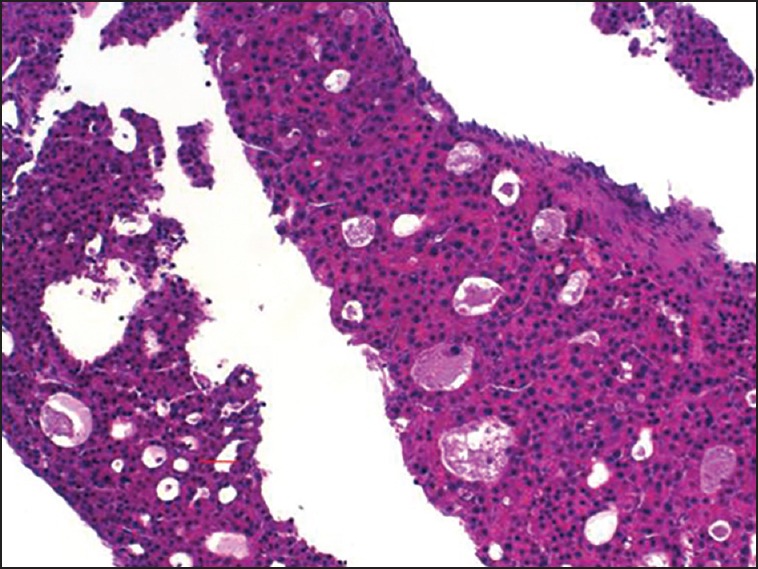
Liver biopsy of the affected area showing hepatoid cells with pseudoglandular pattern consistent with hepatocellular carcinoma
Figure 5.
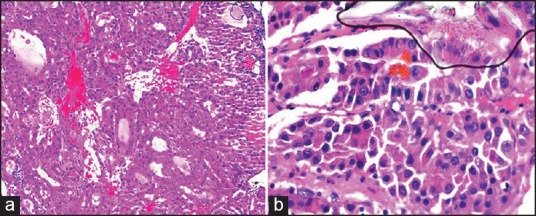
Permanent section of pituitary lesion showing hepatoid appearance and pseudoglandular pattern (a) and also showing bile pigment. (b) The morphology of the tumor is similar to patientæs liver biopsy which favors the diagnosis of metastatic hepatocellular carcinoma
DISCUSSION
Our patient is a 65-year-old Hispanic gentleman who presented with multiple cranial neuropathies and a newly diagnosed sellar mass. A sellar mass was initially suspected due to his constellation of neurologic symptoms. He was found to have pupil-sparing partial third nerve palsy, most likely from extension of the mass and compression of the third nerve along its course into the cavernous sinus. He also had left sided cranial nerve six palsy. The sixth nerve travels through the subarachnoid space where it ascends the clivus and enters the cavernous sinus. Within the subarachnoid space, the sixth nerve may be stretched or compressed against the clivus leading to a sixth nerve palsy. Upon admission to our institution, his CT scan showed a large lesion involving the sella with an anterior expansion towards the nasopharynx than would generally not be expected in a PA. In addition, on the sagittal bony reconstructions of the CT scan, there appeared to be erosion of the clivus, something that is quite uncommon with PA. Though the patient's presentation was suggestive of a sellar mass it's imaging was not consistent with a PA, but rather a lesion of the skull base involving the clivus, sella, sphenoid sinus, and nasopharyngeal space. Additionally, as our patient had no findings consistent with panhypopituitarism or other endocrinopathies. This led to an expansion of the differential diagnosis to primarily include metastatic lesions.
During his work-up he was found to have a large lesion of the right side of the liver, which was confirmed on biopsy to be HCC that is the most common primary malignant hepatic neoplasm. The reported incidence of HCC has risen in developed countries in recent years, possibly owing to the introduction of more sensitive diagnostic tools.[7] In the majority of cases, HCC arises in the background of cirrhosis/liver disease due to viral hepatitis or alcoholism; in only 20% of patients there is no serological evidence of viral hepatitis. Extrahepatic spread of HCC in the central nervous systemic uncommon. The most common sites of distant metastases of HCC are lung and bones. Pituitary metastases from HCC have only rarely been reported in literature.[1,8,9]
Similarly to our patient, Hirsch et al. described a patient in whom headache and left external opthalmoplegia were the only presenting signs of a clinically silent HCC. However, unlike our case, the HCC was radiologically undetectable. Likely, secondary to the small size of the malignant liver nodules, CT imaging of the liver failed to reveal hepatic lesions. Overall, HCC presenting with signs and symptoms related to distant metastases without abdominal discomfort or palpable liver masses is quite uncommon, representing <5% of cases. Liver tumors rarely metastasize to the pituitary, accounting for just 21% of all PM. The mean survival decreases to 5-month among patients with PM from HCC. There have been a number of case reports and published series with identified pituitary metastases.[5,8,9,10,11]
CONCLUSION
Our patient's unique presentation and scarcity of related published data make this case an unusual diagnostic challenge. Lack of concomitant presenting complaints or previous history suspicious for underlying malignancy combined with a classical presentation of sellar mass likely led to the initial outpatient diagnostic presumption of PA. However, increased clinical suspicion upon evaluation of nonclassical inpatient imaging led to appropriate further investigations and elucidated the distant primary malignancy.
ACKNOLEDGMENT
We would like to thank Drs. Ann Elizabeth Doniguian (pathologist), Edward Milman (Radiologist), Beth Stein (Neurologist) for their invaluable contribution to our work.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Hirsch D, Benbassat CA, Drozd T, Okon E, Blum I. Pituitary and bilateral adrenal enlargement: an unusual presentation of hepatocellular carcinoma. J Endocrinol Invest. 2005;28:454–8. doi: 10.1007/BF03347227. [DOI] [PubMed] [Google Scholar]
- 2.Freda PU, Post KD. Differential diagnosis of sellar masses. Endocrinol Metab Clin North Am. 1999;28:81–117. doi: 10.1016/s0889-8529(05)70058-x. vi. [DOI] [PubMed] [Google Scholar]
- 3.Buonaguidi R, Ferdeghini M, Faggionato F, Tusini G. Intrasellar metastasis mimicking a pituitary adenoma. Surg Neurol. 1983;20:373–8. doi: 10.1016/0090-3019(83)90005-8. [DOI] [PubMed] [Google Scholar]
- 4.Moreno-Perez O, Peiró FM, López P, Boix E, Meoro A, Serna-Candel C, et al. An isolated pituitary metastasis as presentation of a differentiated hepatocellular carcinoma mimicking a nonfunctioning macroadenoma. J Endocrinol Invest. 2007;30:428–33. doi: 10.1007/BF03346322. [DOI] [PubMed] [Google Scholar]
- 5.Karamouzis MV, Melachrinou M, Fratzoglou M, Labropoulou-Karatza CH, Kalofonos HP. Hepatocellular carcinoma metastasis in the pituitary gland: Case report and review of the literature. J Neurooncol. 2003;63:173–7. doi: 10.1023/a:1023994604919. [DOI] [PubMed] [Google Scholar]
- 6.Ruelle A, Palladino M, Andrioli GC. Pituitary metastases as presenting lesions of malignancy. J Neurosurg Sci. 1992;36:51–4. [PubMed] [Google Scholar]
- 7.El-Serag HB, Mason AC. Rising incidence of hepatocellular carcinoma in the United States. N Engl J Med. 1999;340:745–50. doi: 10.1056/NEJM199903113401001. [DOI] [PubMed] [Google Scholar]
- 8.Chang SS, Luo JC, Chao Y, Chao JY, Chi KH, Wang SS, et al. The clinical features and prognostic factors of hepatocellular carcinoma patients with spinal metastasis. Eur J Gastroenterol Hepatol. 2001;13:1341–5. doi: 10.1097/00042737-200111000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Aung TH, Po YC, Wong WK. Hepatocellular carcinoma with metastasis to the skull base, pituitary gland, sphenoid sinus, and cavernous sinus. Hong Kong Med J. 2002;8:48–51. [PubMed] [Google Scholar]
- 10.Komninos J, Vlassopoulou V, Protopapa D, Korfias S, Kontogeorgos G, Sakas DE, et al. Tumors metastatic to the pituitary gland: Case report and literature review. J Clin Endocrinol Metab. 2004;89:574–80. doi: 10.1210/jc.2003-030395. [DOI] [PubMed] [Google Scholar]
- 11.Branch CL, Jr, Laws ER., Jr Metastatic tumors of the sella turcica masquerading as primary pituitary tumors. J Clin Endocrinol Metab. 1987;65:469–74. doi: 10.1210/jcem-65-3-469. [DOI] [PubMed] [Google Scholar]


