Abstract
Objectives
This article is a systematic review of the effectiveness of three practices for reducing blood culture contamination rates: venipuncture, phlebotomy teams, and prepackaged preparation/collection (prep) kits.
Design and methods
The CDC-funded Laboratory Medicine Best Practices Initiative systematic review methods for quality improvement practices were used.
Results
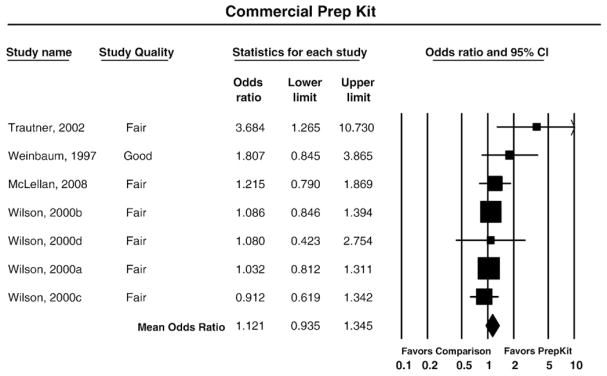
Studies included as evidence were: 9 venipuncture (vs. versus intravenous catheter), 5 phlebotomy team; and 7 prep kit. All studies for venipuncture and phlebotomy teams favored these practices, with meta-analysis mean odds ratios for venipuncture of 2.69 and phlebotomy teams of 2.58. For prep kits 6 studies’ effect sizes were not statistically significantly different from no effect (meta-analysis mean odds ratio 1.12).
Conclusions
Venipuncture and the use of phlebotomy teams are effective practices for reducing blood culture contamination rates in diverse hospital settings and are recommended as evidence-based “best practices” with high overall strength of evidence and substantial effect size ratings. No recommendation is made for or against prep kits based on uncertain improvement.
Keywords: Bacterial infections/diagnosis, Blood culture, Blood specimen collection/methods/standards, Comparative effectiveness research, Contamination, False positive reactions, Healthcare quality improvement, Laboratory medicine, Phlebotomy, Practice guideline
Introduction
A blood culture is the primary laboratory test for diagnosing serious blood stream infections, including septicemia or sepsis, and in directing appropriate antibiotic therapy [1–3]. Septicemia among hospitalized patients is widely prevalent and was the single most expensive condition treated in U.S. hospitals affecting nearly one of every 23 patients (4.2%) at an aggregate cost of nearly $15.4 billion (4.3% of all hospital costs) in 2009 [4]. The number of hospital stays for septicemia more than doubled between 2000 and 2009 [5], and it had an in-hospital mortality rate of about 16% in 2009, more than 8 times higher than other stays [4]. Accurate blood culture results are essential for providing safe, timely, effective and efficient care for patients with serious infections. These procedures also affect healthcare expenses as well as public health tracking and reporting of healthcare acquired infections and bloodstream infection rates for infection control activities [3].
Quality gap: blood culture contaminationa
False positive blood culture test results are common and are caused by contamination that occurs from the introduction of organisms outside the bloodstream (e.g., skin or environmental contaminants) into the sample of blood obtained for culture [6] that cannot be completely eliminated [7–9]. While a relatively small percentage of all blood cultures are contaminated, it represents a large proportion of all positive results and therefore has been recognized as an important quality problem for decades [3]. Although no definitive estimate is available, of all positive cultures, 20% to 50% are likely false positives [10–12]. According to the American Society for Microbiology (ASM) and the Clinical Laboratory Standards Institute (CLSI) overall blood culture contamination rates should not exceed 3% [1,2], however reported contamination rates in hospitals vary widely ranging from 0.6% to 12.5%, with the highest rates associated with emergency department settings [3,6–9,11,13–20]. One study reported a 26% contamination rate in pediatric outpatients [21]. False positive results can lead to inappropriate patient diagnosis, follow-up, and unnecessary treatment [3,9,11], creating substantial adverse consequences for patients and cost burdens for the healthcare system. This includes re-collection of blood cultures, other laboratory tests for reevaluation, incorrect or delayed diagnosis due to errors in clinical interpretation, inappropriate antibiotic treatment as well as unnecessary and longer hospital stays and costs associated with these outcomes [3,12,14,22,23].
To reduce this important quality gap and its consequences, it is essential to identify effective practices for reducing blood culture contamination rates. Other than the use of skin antiseptics [24] and changing needles prior to inoculation of blood culture bottles [25], no systematic reviews of quality improvement practice evidence of effectiveness have been conducted. The use of strict aseptic techniques by healthcare workers when obtaining blood culture specimens is an important factor in reducing contamination [9], and there is sufficient evidence to evaluate the effectiveness of three practices used to obtain blood culture specimens: venipuncture, phlebotomy teams and prepackaged prep kits. The purpose of this article is to evaluate evidence of these practices’ effectiveness at reducing blood culture contamination (false positive) rates by applying the CDC Laboratory Medicine Best Practices Initiative’s (LMBP) systematic review methods for quality improvement practices and translating the results into evidence-based guidance [26].
Methods
This evidence review followed the CDC’s Laboratory Medicine Best Practices Initiative’s (LMBP) “A-6 Cycle” systematic review methods for evaluating quality improvement practices and reported in detail elsewhere [26]. This approach is derived from previously validated methods, and is designed to transparently evaluate the results of studies of practice effectiveness to support evidence-based best practice recommendations. A review team conducts the systematic review including a review coordinator and staff specifically trained to apply the LMBP methods. Guidance on the conduct of the systematic review and draft recommendations is provided by an expert panel including individuals selected for their diverse perspectives and expertise in the review topic, laboratory management and evidence review methods.b The results of the evidence review are translated into an evidence-based best practice recommendation by the expert panel for approval by the LMBP Work-group, an independent, multi-disciplinary group composed of 15 members with expertise in laboratory medicine, clinical practice, health services research and health policy.
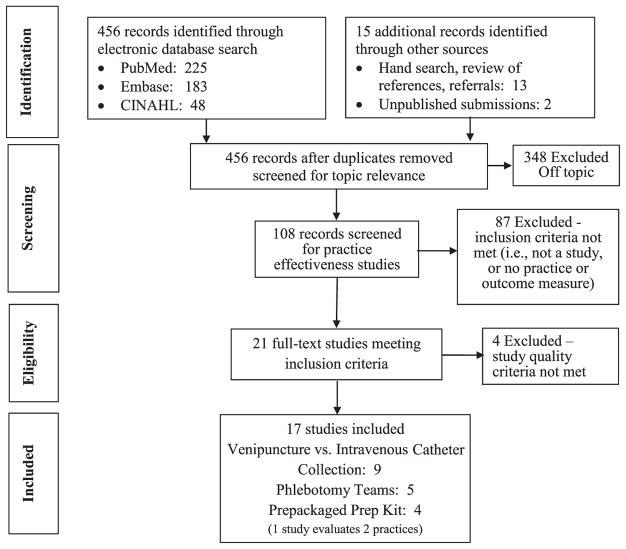
The question answered by this evidence review is: What practices are effective for reducing blood culture contamination? This review question is addressed in the context of an analytic framework for the quality issue of blood culture contamination depicted in Fig. 1. The relevant PICO elements are:
Fig. 1.
LMBP QI analytic framework: blood culture contamination.
Population: all patients in healthcare settings who have a blood culture specimens collected
-
Intervention (practice) versus Comparison:
venipuncture versus intravenous catheter collection
phlebotomy team versus non-phlebotomist staff collection
prepackaged prep kit versus no prep kit for venipuncture collection
Outcome: blood culture contamination rate is the direct outcome of interest
The three practices being evaluated in this review are venipuncture, puncture of a vein through the skin to withdraw blood as opposed to an indwelling catheter in the vein to withdraw blood (or other purposes such as delivery of antibiotics, pain medication, and saline solution); use of a phlebotomy team of certified or trained phlebotomists for specimen collection using venipuncture instead of other healthcare personnel (e.g., physicians, interns, nurses); and prepackaged prep kits of aseptic supplies for collection of blood specimens by venipuncture that are commercially purchased versus using usual disinfectant supplies that are not prepackaged.
The search for studies of practice effectiveness included a systematic search of multiple electronic databases, hand searching of bibliographies from relevant information sources, consultation with and references from experts in the field including members of the expert panel (Appendix A), and by solicitation of unpublished quality improvement studies resulting in direct submissions to the Laboratory Medicine Best Practices Initiative.c The literature search strategy and terms were developed with the assistance of a research librarian and included a systematic search in September 2011 of three electronic databases (PubMed, Embase and CINAHL) for English language articles from 1995 to 2012 about human subjects. The search contained the following Medical Subject Headings: allied health personnel, blood, blood specimen collection, catheterization, disinfectants, health personnel, laboratory personnel, phlebotomy as well as these keywords: anti-infective agent, local; antisepsis; blood sampling; blood culture; catheter; contaminants; contamination; costs; disinfection; health care cost(s); healthcare personnel; intravenous catheter; microbiology; paramedical personnel; phlebotomists; phlebotomy team; skin; skin decontamination; quality; and venipuncture.
Included studies were considered to provide valid and useful information addressing the review question, with findings for at least one blood culture contamination rate outcome measure. To reduce subjectivity and the potential for bias, all screening, abstraction and evaluation was conducted by at least two independent reviewers, and all differences were resolved through consensus. The effect size for each study was standardized using its reported data and results to calculate an odds ratio (OR)d since the outcome of interest is dichotomous (i.e., blood culture is contaminated or is not contaminated) and the findings for these practices are typically expressed in terms of rates or percentages. The OR compares the intervention practice to the comparison practice, or comparator, in terms of the relative odds of a successful outcome (i.e., no contamination versus contamination). Each study is assigned one of three quality ratings (Good, Fair, Poor) and one of three effect size ratings (Substantial, Moderate or Minimal/None).e
The results from the individual effectiveness studies are aggregated into a practice body of evidence that is analyzed to produce the systematic review results for translation into an evidence-based recommendation (Recommend, No recommendation for or against, Recommend against). Both qualitative and quantitative analyses are used to assess the effect size consistency and patterns of results across studies [27], and to rate the overall strength of the body of evidence for practice effectiveness (High, Moderate, Suggestive, Insufficient). Criteria for these ratings are described in greater detail elsewhere [26,28]. The qualitative analysis synthesizes the individual studies to convey key study characteristics, results and evaluation findings summarized in a body of evidence table. The quantitative analysis is provided using meta-analysis of results from similar individual studies to provide a weighted average effect size and 95% confidence interval (CI) estimated using a random-effects modelf and presented in a forest plot [29,30] with the individual studies’ and overall mean odds ratios along with their respective 95% confidence interval upper and lower limits. The I2 statistic is used to estimate the percent of variability associated with between-study differences [31,32].
Evidence review synthesis and results
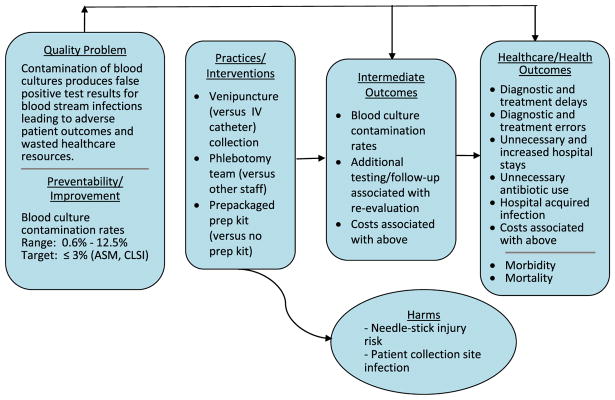
The search identified 456 separate bibliographic records that were screened for eligibility to contribute evidence of effectiveness for the three practices (venipuncture, phlebotomy teams, and prepackaged prep kits) with respect to blood culture contamination rate outcomes. After initial screening, 348 of these records were excluded as off-topic, and 87 were excluded for not meeting effectiveness study inclusion criteria (i.e., a study using data evaluating a practice of interest with at least one finding for a relevant blood culture contamination rate outcome measure). A total of 21 full-text studies met the review inclusion criteria. A systematic review flow diagram in Fig. 2 provides a breakdown of the search results. The full-text review and evaluation of the 21 eligible studies (10 venipuncture; 6 phlebotomy team; 6 prep kits), with one evaluating two practices, resulted in excluding 4 studies (1 venipuncture; 1 phlebotomy team; 2 prep kit) for not meeting the minimum required LMBP study quality inclusion criteria. Appendix C provides a Body of Evidence table for each practice, as well as abstracted and standardized information and study quality ratings in evidence summary tables for each of the 21 eligible studies. Appendix B provides bibliographic reference information for these studies. A total of 17 studies are included in this review as evidence of practice effectiveness (9 venipuncture; 5 phlebotomy team; 4 prep kits). One published study contained data evaluating 2 practices (Weinbaum [19]) and another published study (Wilson et al., 2000, Appendix B) contains 4 studies at separate sites resulting in a total of 7 prep kit studies.
Fig. 2.
Systematic review flow diagram.
Venipuncture practice effectiveness evidence
Information on the nine published studies that comprise the practice effectiveness body of evidence comparing venipuncture to catheter blood sample collection with respect to blood culture contamination rates is summarized in Table 1. The publication dates for these studies range from 1999 (DesJardin [34]) to 2011 (Weddle [18]), with the earliest study time periods beginning in 1994 (DesJardin [34]; Martinez [39]). Of the nine studies, seven were rated “Good” study quality and two were rated “Fair.” Paired blood cultures from the same patient (one collected by venipuncture and one by catheter) were used as the study samples in five studies (Beutz [35], DesJardin [34], Everts [40], Martinez [39], Mcbryde et al., 2005, Appendix B), ranging from 300 (Beutz [35]) to 1408 pairs (Everts [40]). The four non-paired study samples (Norberg [38], Qamruddin et al., 2007, Appendix B, Ramsook et al., 2000, Appendix B, Weddle [18]) ranged in size from 1138 (Qamruddin et al., 2007, Appendix B) to 4108 total blood cultures (Norberg [38]). These studies all involve hospital patients and include a range of settings as follows: all patients (adult and pediatric), (Everts [40]), all adult patients, (Qamruddin et al., 2007, Appendix B) intensive care units (Beutz [35], Martinez [39]), an oncology ward (DesJardin [34]), and pediatric emergency departments (Norberg [38], Ramsook et al., 2000, Appendix B, Weddle [18]). Seven studies were conducted in U.S. hospitals, two in the same hospital (DesJardin [34] and Martinez [39]), one in the UK (Qamruddin et al., 2007, Appendix B), and one in Australia (Mcbryde et al., 2005, Appendix B).
Table 1.
Body of evidence summary table: venipuncture (versus catheter).
| Study (Quality and Effect Size Ratings) | Population/Sample | Setting | Time period | Results (Blood Culture Contamination Rates) |
|---|---|---|---|---|
| Beutz 2003 - Good - Moderate |
300 paired blood cultures from 119 patients - medical ICU | Barnes - Jewish Hospital, St. Louis, MO: 1,000 bed university - affiliated teaching hospital | 9 months (02/2001 – 10/2001) | Venipuncture: 3.7% Catheter: 6.7% OR = 1.88 (CI: 0.88 – 3.99) |
| DesJardin 1999 - Good - Moderate |
551 paired blood cultures from 185 patients – oncology ward | New England Medical Cente, Boston, MA; 300 - bed tertiary care university - affiliated hospital | 22 months (08/1994 – 06/1996) | Venipuncture: 2.4% Catheter: 4.4% OR = 1.88 (CI: 0.95 – 3.74) |
| Everts 2001 - Good - Substantial |
1,408 pairs of concurrent catheter-drawn and venipuncture samples | Tertiary - care medical setting; Duke University School of Medicine, Durham, NC | 24 months (01/1997 – 12/1998) | Venipuncture: 1.8% Catheter: 3.8% OR = 2.12 (CI: 1.32 – 3.41) |
| Martinez 2002 - Good - Substantial |
499 paired blood cultures from 271 patients - surgical and cardiothoracic ICUs | New England Medical Center, Boston, MA; 300 - bed tertiary care university - affiliated hospital | 34 months (11/1994 – 08/1997) | Venipuncture: 1.6% Catheter: 4.0% OR = 2.57 (CI: 1.13 – 5.89) |
| Mcbryde et al. (2005) - Good - Substantial |
962 paired venipuncture and catheter - drawn blood cultures from same patient – multiple wards | Mater Misericordiae Hospital, Brisbane, Queensland Australia; 280 beds; Teaching hospital | 44 months (01/1998 - 08/2002) | Venipuncture: 2.6% Catheter: 13% OR = 5.60 (CI: 3.61 – 8.69) |
| Norberg 2003 - Good - Substantial |
4,108 total blood cultures – pediatric emergency department Catheter: 2108 Venipuncture: 2000 |
Children’s Hospital Medical Center of Akron, Akron, OH | 12 months (01/1999 - 12/1999) | Venipuncture: 2.8% Catheter: 9.1% OR = 3.46 (CI: 2.55 – 4.69) |
| Qamruddin et al. (2007) - Fair - Moderate |
1,138 total blood culture samples – adult patients from multiple wards Venipuncture: 979 Catheter: 159 |
Manchester Royal Infirmary, Manchester, UK. | 2 months (02/2006 - 04/2006) | Peripheral vein: 7.3% Catheter: 10.7% OR = 1.53 (CI: 0.88 – 2.68) |
| Ramsook et al. (2000) - Fair - Substantial |
1,722 total blood cultures – pediatric emergency room Venipuncture: 427 Catheter: 1295 |
Texas Children’s Hospital; Houston University - affiliated Houston, Texas | 6 months (02/1999 - 07/1999) | Venipuncture: 1.2% Catheter: 3.4% OR = 2.97 (CI: 1.17 – 7.54) |
| Weddle 2011 - Good - Substantial |
3,025 total blood cultures - pediatric emergency department Venipuncture: 1229 Catheter: 1796 |
Children’s Mercy Hospitals and Clinics, Kansas City, MO. 263-bed tertiary children’s hospital. | 12 months (9/2008 - 8/2009) | Venipuncture: 2.4 (29/1229) Catheter: 6.7% (120/1796) OR = 2.96 (CI 1.96 – 4.47) |
| BODY OF EVIDENCE RATINGS |
# Studies by Quality and Effect Size Ratings 5 Good/Substantial 1 Fair/Substantial 2 Good/Moderate 1 Fair/Moderate |
|||
| Consistency | YES | |||
| Overall Strength | HIGH | |||
Bibliographic information for all studies is provided in Appendix C.
Body of evidence qualitative analysis
Evidence of practice effectiveness for reducing blood culture contamination rates by using venipuncture indicates consistent and substantially lower rates compared to catheter collection with a high strength of evidence in hospital settings (Table 1). The venipuncture odds ratios for all nine studies included in the body of evidence (with >1.0 favoring venipuncture over catheter blood draws) ranged from 1.53 (95% CI: 0.88–2.68) to 5.60 (95% CI: 3.61–8.69). The odds ratio for six of the nine studies exceeded 2.0 for a “Substantial” effect size rating. For the remaining three studies, the lower limit of their odds ratios’ 95% confidence interval is less than 1.0, with the lowest at 0.88. The odds ratio results of the five studies using paired blood cultures provide more reliable evidence and ranged from 1.88 (95% CI: 0.88–3.99) to 5.60 (95% CI: 3.61–8.69), offering greater support overall for the effectiveness of venipuncture compared to those of the four less suitable study designs ranging from 1.53 (95% CI: 0.88–2.68) to 3.46 (95% CI: 2.55–4.69). All three studies in the pediatric emergency department setting have similar high odds ratios ranging from 2.96 (95% CI: 1.96–4.47) to 3.46 (95% CI: 2.55–4.69).
Meta-analysis
The forest plot in Fig. 3 presents the meta-analysis effect size results for venipuncture compared to catheter blood culture contamination rates for the body of evidence estimated using a random effects model. The odds ratios for all nine studies included in the body of evidence favor venipuncture over catheter blood draws with a mean odds ratio of 2.69 (95% CI: 2.03–3.57), strongly favoring venipuncture over catheter blood collection for reducing blood culture contamination rates. The meta-analysis results show moderate statistical heterogeneity (Q=19.5, p=0.012), with approximately 60% of the variability in results attributable to between-study differences. (I2=59.0) [33].
Fig. 3.
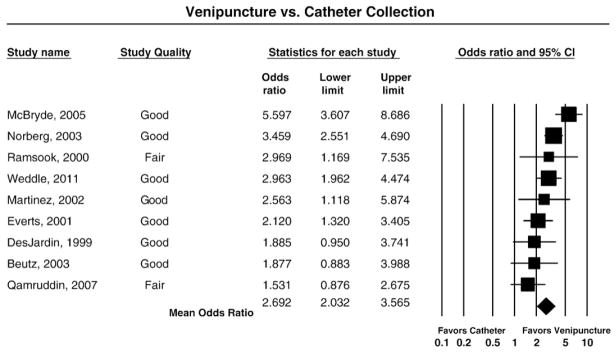
Meta-analysis forest plot: venipuncture versus catheter collection.
Phlebotomy team practice effectiveness evidence
Of the five studies included in the body of evidence for phlebotomy team practice effectiveness (Table 2), all were conducted in large U.S. hospitals, two in emergency departments only (Gander [41], Sheppard [13]). One of the studies is unpublished (Geisinger Wyoming Valley, 2009, Appendix B) and four are rated “Good” study quality and one is rated “Fair.” Of the included studies, three had phlebotomy team comparison groups using only venipuncture for blood draws (Gander [41], Surdulescu [16], Weinbaum [19]) which provide more reliable evidence for estimating phlebotomy team practice effectiveness than the two studies which include both venipuncture and catheter draws in their comparison groups. The earliest reported study time period began in 1993 (Surdulescu [16]) and the most recent began in 2009 (Geisinger Wyoming Valley, 2009, Appendix B). All of the studies had large sample sizes exceeding 1000 blood cultures, and overall appear to represent a broad and diverse hospital patient population.
Table 2.
Body of evidence summary table: phlebotomy teams.
| Study (Quality and Effect Size Ratings) | Population/Sample | Setting | Time period | Results (Blood Culture Contamination Rates) |
|---|---|---|---|---|
| Gander 2009 - Good - Substantial |
3,662 total venipuncture blood cultaaures - Emergency Dept (West): Phlebotomists: 2,012 Non -phlebotomists: 1,650 |
Parkland Memorial Hospital, Dallas, TX; 968 bed tertiary care teaching hospital | 12/2006–12/2007; 5mos. of a 13-mo. period | Phlebotomists: 3.1% Non-phlebotomists: 7.4% OR = 2.51 (CI: 1.84 –3.43) |
| Sheppard 2008 - Good - Substantial |
2,854 total blood cultures-Emergency Dept.: Phlebotomists: 278 Non-phlebotomists: 2,576 (include venipuncture and catheter) |
Emory Crawford Long Hospita, Atlanta, GA; Academic Medical Center | 3 months– no dates reported | Phlebotomists: 1.1% Non-phlebotomists: 5.0% OR = 4.83 (CI: 1.53 –15.28) |
| Surdulescu 1998 - Fair - Substantial |
Venipuncture blood draws with prep kits; Sample size not reported;~6,900 total for 1995; from 1/93–10/93 approx. ½ phlebotomy team draws | St. Luke’s Medical Center, Case Western Reserve University, Cleveland, OH; teaching hospital. | 10 months 01/1993–10/1993 | Phlebotomists: 2.6% Non-phlebotomists: 5.6% (p= 0.003) OR = 2.09 (CI: 1.68 –2.61) |
| Weinbaum 1997 -Good - Substantial |
1,164 total blood culture venipuncture draws with prep kits; adult general medical and surgical care Phlebotomists: 956 Non-phlebotomists: 208 |
New York Medical Center Hospital of Queens, Flushing, NY; 487-bed community hospital | No dates reported. Baseline: 3mos.; Intervention: 6 mos. | Phlebotomists: 1.2% Non-phlebotomists: 4.8%, OR = 4.34 (CI: 1.82 –10.36) |
| Unpublished | ||||
| Geisinger Wyoming Valley Hospital 2009 - Good - Substantial |
~7020 total blood cultures; 73% by phlebotomists; non-phlebotomist blood collections include venipuncture and catheter | Geisinger Wyoming Valley Hospital; Wilkes-Barre PA | 9 months (01/2009–09/2009) | Phlebotomists: 1.5% Non-phlebotomists: 4.3% OR = 2.93 (CI: 2.13 –4.02) |
| BODY OF EVIDENCE RATINGS |
# Studies by Quality and Effect Size Ratings 4 Good/Substantial 1 Fair/Substantial |
|||
| Consistency | YES | |||
| Overall Strength | HIGH | |||
Bibliographic information for all studies is provided in Appendix C.
Body of evidence qualitative analysis
The evidence of practice effectiveness for phlebotomy teams at reducing blood culture contamination rates indicates consistent and substantial improvement compared to collections by non-phlebotomist staff with a high strength of evidence in hospital settings (Table 2). For all five studies in the practice body of evidence, the phlebotomy team odds ratio exceeded 2.0 (favoring phlebotomy teams over non-phlebotomist staff), ranging from 2.09 (95% CI: 1.68–2.61) to 4.83 (95% CI: 1.53–15.28), and were all statistically significantly different from 1.0, exceeding the threshold criteria for a “Substantial” effect size rating. The phlebotomy practice odds ratio effective size for the three studies with a venipuncture only comparison group ranged from 2.09 (95% CI: 1.68–2.61) to 4.34 (95% CI: 1.82–10.36), which is slightly lower and potentially more representative of the true effect than the range for the two other studies that included catheter draws with odds ratios of 2.93 (95% CI: 2.13–4.02) and 4.83 (95% CI: 1.53–15.28). There is not a notable difference in the effect sizes of the two studies conducted in emergency departments with odds ratios 2.51 (95% CI: 1.84–3.43) and 4.83 (95% CI: 1.53–15.28) compared to the three studies conducted hospital-wide.
Meta-analysis
The forest plot in Fig. 4 presents the meta-analysis effect size results for the phlebotomy team compared to non-phlebotomist collection blood culture contamination rates for the body of evidence estimated using a random effects model. The odds ratios for all five included studies favor phlebotomy teams over non-phlebotomists, with a mean odds ratio of 2.58 (95% CI: 2.07–3.20) strongly favoring phlebotomy teams for reducing blood culture contamination rates. The meta-analysis results are homogeneous (Q=6.2, p=0.182) with moderate variability attributed to between study differences (I2=35.8%) [33].
Fig. 4.
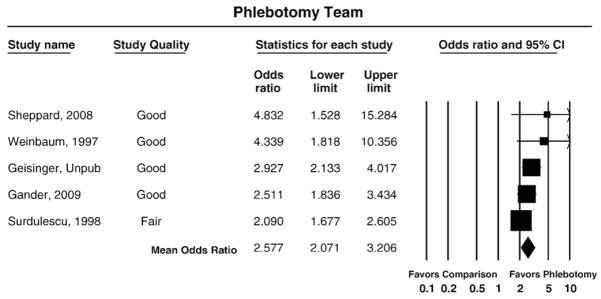
Meta-analysis forest plot: phlebotomy teams.
Prepackaged prep kit practice effectiveness evidence
Of the four published studies included in the prepackaged prep kit practice effectiveness body of evidence (Table 3), one (Wilson et al., 2000, Appendix B) contains four separate trials, each at a different hospital, yielding a total of seven studies. All seven studies were conducted in hospitals, six in the U.S. and one in the UK (McLellan [6]), and involved venipuncture blood collections in a broad range of hospital settings by multiple types of staff (i.e., phlebotomists, healthcare technicians, staff physicians and interns). One of the studies was rated “Good” study quality and six were rated “Fair.” The study time periods for five of the seven studies began prior to 2000 (Wilson et al., 2000, Appendix B, Weinbaum [19]), with only one study period occurring in the last five years (McLellan [6]). The study sample sizes ranged from 495 (Weinbaum [19]) to 6,460 total blood cultures (Wilson et al., 2000, Appendix B).
Table 3.
Body of evidence summary table: prepackaged prep kits.
| Study (Quality and Effect Size Ratings) | Population/Sample | Setting | Time period | Results (Blood Culture Contamination Rates) |
|---|---|---|---|---|
| McLellan 2008 -Fair -Minimal/None |
1,115 total blood cultures collected by Doctor Support Workers (DSWs), junior and on call doctors No prep kit (Pre): 563 Prep kit (Post): 552 (2% chlorhexidine gluconate in 70% isopropyl alcohol) |
Northern General Hospital, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, South Yorkshire, UK Academic Medical Center; 2 units; accident/emergency and general practice | Pre: 5/2007- 7/2007 Post: 8/2007–10/2007 |
Overall: No prep kit (Pre): 8.88% Prep kit (Post): 7.43 % OR= 1.22 (CI: 0.79 –1.87) |
| Trautner 2002 -Fair -Substantial |
813 total blood cultures collected by phlebotomists, house staff (medical students/residents) and healthcare technicians No prep kit:383 Prep kits: 430 paired sets from 215 patients-2 separate sites (chlorhexidine and tincture of iodine) |
VA Medical Center, Houston, TX; Tertiary-care teaching hospital, inpatient service wards (telemetry, oncology, geriatric), medical and cardiac ICU. | 11/2000–5/2001 | No prep kit: 6.5% Prep kits: 0.9% OR = 3.68 (CI: 1.27 –10.73) |
| Weinbaum 1997 -Good -Moderate |
495 total blood culture specimens collected by house staff (interns & residents No prep kit: 287 Prep kits: 208 (isopropanol and tincture of iodine) |
New York Medica Center Hospital of Queens Flushing, NY.; 487-bed community hospital); general medical unit | 3 months (1995); dates not reported | No prep kit: 6.5% Prep kits: 0.9% OR = 1.81 (CI: 0.85 –3.87) |
| Wilson et al. (2000) -Fair -Minimal/None (4 studies) |
12,367 total blood samples; 6,362 with alcohol pledgets; 6005 with prep kits (70% isopropyl alcohol & 2% iodine tincture on separate sterile applicators). By site: Site a: No kit: 3536; Prep kit 2924; Site b: No kit: 1632; Prep kit 1801; Site c: No kit: 1007; Prep kit 906; Site d: No Kit: 187; Prep kit 374; collected by house staff physicians/medical students except phlebotomy teams at Site c. |
4 Academic medical centers: Duke Univ. Med. Ctr., Durham, NC (Site a), Robert Wood Johnson Univ. Hosp., New Brunswick, NJ (Site b), Denver Health Med. Ctr., Denver, CO (Site c), and Salt Lake Veterans Affairs Med. Ctr., Salt Lake City, UT (Site d) | Dates not reported; prior to 2000 | Overall: No prep kit: 5.5% Prep kits:* 5.5% By site: Conventional; Prep kit Site a: 4.4%; 4.3% OR = 1.03 (CI: 0.81–1.31) Site b: 8.1%; 7.5% OR = 1.09 (CI: 0.85–1.39) Site c: 5.5%; 6.0% OR = 0.91 (CI: 0.62–1.34) Site d: 3.7%; 3.5% OR = 1.08 (CI: 0.42 –2.75) |
| BODY OF EVIDENCE RATINGS |
# Studies by Quality and Effect Size Ratings 1 Fair/Substantial 1 Good/Moderate 5 Fair/Minimal/None |
|||
| Consistency | NO | |||
| Overall Strength | INSUFFICIENT | |||
Bibliographic information for all studies is provided in Appendix C.
Body of evidence qualitative analysis
The evidence of practice effectiveness for prepackaged prep kits at reducing blood culture contamination rates often indicated either minimal or no improvement compared to venipuncture collections without prep kits in hospital settings (Table 3). For six of the seven studies in the practice body of evidence, the prep kit odds ratio was not statistically significantly different from 1.0. (i.e., no difference between blood culture contamination rates for prep kits versus no prep kits) with one study showing substantial improvement. The odds ratios for the seven individual studies ranged from 0.91 (95% CI: 0.62–1.34) to 3.68 (95% CI: 1.27–10.73). Five of the studies received a “Minimal/None” effect size rating with odds ratios ranging from 0.91 (95% CI: 0.62–1.34) to 1.22 (95% CI: 0.79–1.87), one was rated “Moderate,” and only one study exceeded the threshold criteria for a “Substantial” effect size rating.
Meta-analysis
The forest plot in Fig. 5 presents the meta-analysis blood culture contamination rate effect size results for venipuncture collections with prepackaged prep kits compared to without prep kits for the practice body of evidence estimated using a random effects model. The mean odds ratio of 1.12 (95% CI: 0.94–1.35) is homogeneous (Q=7.9, p=0.242) and does not favor prepackaged prep kits for reducing blood culture contamination rates. The meta-analysis results show low between-study variability with an I2 statistic of 24.4% [33].
Fig. 5.
Meta-analysis forest plot: prepackaged prep kits.
Discussion
Additional considerations
This section addresses additional considerations for evaluating venipuncture and phlebotomy teams, the two practices identified as effective at reducing blood culture contamination rates.
Applicability
While venipuncture is demonstrated to be more effective at reducing blood culture contamination than intravenous catheter for blood culture collection, venipuncture and its effect size results are not necessarily equally applicable in all hospital settings and populations (e.g., pediatric units, hematology-oncology patients and other settings where patients are critically ill and may have in-dwelling catheters in place) [18,34–38]. Catheter blood collection may remain a secondary source of blood specimens for blood culture or other laboratory tests when there are problems with venipuncture due to poor peripheral access, since it is convenient and prevents trauma to the veins when blood is needed frequently [34] (e.g., for ruling out infection in critically ill patients in surgical intensive care units [39]). In addition, catheter blood collections are required to identify or rule out catheter colonization with bacteria, in which case catheters may need to be removed and replaced. As indicated by the higher contamination rates from this systematic review, interpretation of positive blood culture results from catheter drawn samples must be exercised with care [3,40].
Phlebotomy teams are applicable to a variety of hospital environments such as tertiary care, community and academic medical centers, emergency departments, adult general medical and surgical care settings [13,16,19,41]. Based on the included studies, phlebotomy team results are highly applicable across several patient groups in hospital settings, but less so in special cases where venipuncture may be less applicable such as neonatal intensive care units and critically ill patients in long term care. It is important to note that well-trained and experienced non-phlebotomist staff can potentially achieve comparable blood culture contamination rates when using the same collection techniques as phlebotomists.
Harms
Venipuncture procedures should be performed using universal precautions [1], as there are needle stick injuries [42] and pathogen exposure risks for the phlebotomists or other healthcare staff drawing patient blood samples [1]. Patients are at risk for needle insertion site injury from multiple attempts to obtain blood specimens [42].
Additional benefits
Studies reviewed report beneficial outcomes associated with venipuncture performed by phlebotomists in addition to reducing blood culture contamination rates. These benefits include decreased turnaround time for laboratory test results on specimens other than blood cultures [13]; reduced frequency of misidentified and mislabeled specimens [43,44]; decrease in patient needle-stick bruises; improved quality of specimens; improved working relationships between phlebotomists and nurses; and higher levels of patient satisfaction [42,45].
Economic evaluation
Venipuncture, like catheter collection, is a primary means of blood sample collection for blood cultures; however the cost of this practice has not been evaluated. Four studies of phlebotomy teams included estimated and projected labor costs and healthcare savings (e.g., reduced hospital length of stay, pharmacy and laboratory services) associated with reduced blood culture contamination rates or false positives [13,16,19,41]. Some studies’ estimated savings were associated with either a general reduction in blood culture contamination rates or relied on other sources for key cost-related assumptions [13,16,19]. All four studies concluded that the healthcare cost savings from reduced contaminated blood cultures exceeded total phlebotomist labor costs, however they did not compare phlebotomist to non-phlebotomist costs (i.e., implies $0 cost for non-phlebotomist labor). Nonetheless, these studies all support a conclusion that phlebotomy teams are not only cost-effective but cost-saving solely based on reduction in blood culture contamination.
Feasibility of implementation
Venipuncture is feasible in all settings and patient populations with some special patient case exceptions as noted in the applicability section. The evidence reviewed clearly demonstrates the feasibility of adopting phlebotomy teams in a variety of hospital settings [13,16,41]. Implementing phlebotomy teams for blood culture collection may require assessment of the availability of currently trained phlebotomist staff in various areas of the hospital settings and possible reorganization of resources. In settings where phlebotomy has been decentralized or eliminated, changes may be instituted to achieve workforce goals. Selected environments where high volumes of blood cultures are initiated at specific hours of the workday may be an excellent starting point for implementation [41]. Phlebotomist salaries and training costs may be perceived as initial barriers to adoption of phlebotomy teams, therefore an assessment of blood culture contamination rates and associated costs within an institution may be helpful to support perceived additional costs for implementing phlebotomy teams compared to using non-phlebotomist staff. Involvement from multiple, relevant departments and leaders within an organization to support implementation will likely be required [13,19,41].
Future research needs
Research is needed to identify and better clarify the impact of blood culture contamination on patient care and health outcomes and their associated costs. This can be accomplished in conjunction with new economic evaluation research to more rigorously and transparently demonstrate blood culture contamination clinical and economic outcomes as well as those associated with phlebotomy teams due to the limited cost-savings information in available studies. Given the evidence on higher blood culture contamination rates from catheter blood collections, more investigation is needed regarding practices to effectively reduce catheter use by non-phlebotomists (e.g., through educational interventions), and by clarifying the specific circumstances for its use (e.g., based on patient characteristics, only newly inserted catheters) to reduce contamination. More research is also needed, however, to determine blood culture contamination rates in patient subgroups, particularly pediatric patient subgroups, to refine guidance on catheter use. Research on the rate of blood culture contamination and quality improvement practices in relatively high volume non-hospital settings, such as in nursing homes and rehabilitation centers, is needed to evaluate and improve quality gaps in other important care settings.
Limitations
The LMBP systematic review methods are consistent with practice standards for systematic reviews [27], but all similar methods are imperfect and include subjective assessments at multiple points that may produce bias. Rating study quality depends on consensus assessments that may be affected by rater experience and the criteria used. Publication bias must be considered although this review contains unpublished studies which may help mitigate that bias. The restriction to English language studies to satisfy the requirement of multiple reviewers for each study may also introduce bias. Most of the evidence for this review is from quality improvement studies, thus the primary data have many limitations, including single institution site-specific differences which may affect study results. Many studies were missing information including actual study sample sizes, dates for relevant time periods, and practice implementation and setting characteristics. Several studies were conducted in specific settings within a hospital such as emergency departments, medical intensive care units and academic settings which may not be generalizable to other settings. Individual study comparison group settings were not always identical, therefore potential differences in practice patterns and patient clinical status could influence results.
As noted in the Results section, several studies included in this review have study periods that are more than ten years old, with three dating to the early 1990s; two for venipuncture (DesJardin [34] and Martinez [30]); one for phlebotomy teams (Surdulescu [16]); and six of the seven prep kit study periods began prior to or in 2000. As indicated in the venipuncture results section, five of the nine studies used a paired blood culture sample study design comparing venipuncture and catheter blood samples from the same patient within a pre-defined time limit, while the other four studies used group-wise comparisons. Although systematic differences are not observed and all nine included studies favored venipuncture, the non-paired design may yield less valid findings when blood culture contamination is affected by patient or setting characteristics. Three of the five phlebotomy team studies used comparison groups of non-phlebotomists performing only venipuncture collections, thereby controlling for the possibility of catheter contamination. Although systematic differences were not observed, it is likely that the results from these three studies were more representative of the practice’s true effect size. All five studies favored phlebotomy teams, but the two studies with non-phlebotomist catheter collections in the comparison group may have had a slight upward bias on the meta-analysis mean effect size estimate. Several studies in this review noted study design limitations in terms of phlebotomy teams and non-phlebotomist staff which may have introduced confounding results on reported blood culture contamination rates and effect sizes due to differences in the skill level and training of staff performing venipuncture.
Conclusions and recommendations
On the basis of a high overall strength of evidence of effectiveness, venipuncture is recommended as a best practice to reduce blood culture contamination (false positive) rates in all hospital settings. The high overall strength of evidence rating is due to sufficient evidence of practice effectiveness from nine individual studies, all favoring venipuncture over catheter blood collection and demonstrating consistent and substantial reductions in blood culture contamination rates (mean odds ratio of 2.69; 95% CI: 2.03–3.57).
On the basis of a high overall strength of evidence of effectiveness, phlebotomy teams are recommended as a best practice to reduce blood culture contamination (false positive) rates in all hospital settings. The high overall strength of evidence rating is due to sufficient evidence of practice effectiveness from five individual studies, all favoring phlebotomy team over non-phlebotomist staff collection and demonstrating consistent and substantial reductions in blood culture contamination rates (mean odds ratio of 2.58; 95% CI: 2.07–3.20).
On the basis of an insufficient overall strength of evidence of effectiveness, no recommendation is made for or against prepackaged prep kits. The overall insufficient strength of evidence rating is based on evidence that indicates inconsistent and unlikely improvement in blood culture (false positive) contamination rates compared to venipuncture collections without prep kits in hospital settings from the results of seven trials in a broad range of hospital settings by multiple types of staff. For six of the seven studies, the prep kit failed to significantly reduce blood culture contamination relative to a standard practice, and the overall effect size was homogeneous and not statistically significantly different from collections without prep kits (mean odds ratio of 1.12; 95% CI: 0.94–1.35).
Acknowledgments
Melissa Gustafson of Battelle, Roberta Carey, Devery Howerton, Abrienne Patta and Barbara Zehnbauer of the Centers for Disease Control and Prevention, the LMBP Blood Culture Contamination Expert Panel and LMBP Workgroup members, and Submitters of unpublished studies.
Abbreviations
- CDC
U.S. Centers for Disease Control and Prevention
- CI
Confidence interval
- IV
Intravenous
- LMBP
Laboratory Medicine Best Practices Initiative
- QI
Quality improvement
Glossary
- Antiseptic
a substance that inhibits the growth and development of microorganisms without necessarily killing them.
- Bacteremia
the presence of bacteria in the bloodstream.
- Bias
systematic error; threats to validity; tendency to produce results that depart systematically from the ‘true’ results. Unbiased results are internally valid. Four types of bias are selection/allocation, performance, measurement/detection and attrition/exclusion.
- Blood culture
a specimen of blood that is submitted for bacterial or fungal culture [1].
- Blood culture contamination rate
the number of contaminated cultures per number of blood cultures received by the laboratory per month or per year. Contamination rates vary based on laboratory-specific definitions due to variation in the definition of contaminant (see Contaminant definition).
- Bloodstream infection
an infection associated with bacteremia or fungemia.
- Catheter
an indwelling device inserted into the vein for injection of medication or as an access for collection of blood samples using a thin flexible tube [35,36].
- Consistency
the degree to which estimates of effect for specific outcomes are similar across included studies.
- Contaminant
a microorganism isolated from a blood culture that was introduced into the culture during specimen collection or processing and that was not pathogenic for the patient from whom blood was collected (i.e., not present in the patient’s blood when the blood was sampled for culture). Organisms are most commonly coagulase-negative Staphylococci but also include other skin flora species such as viridans streptococci, Corynebacterium species other than C. jekieum; Bacillus species, Propioonibacterium acnes [1,2,11].
- Disinfectant
a substance used to reduce the concentration of bacteria, fungi, or viruses on a surface.
- External validity
generalizability, applicability — extent to which the effects observed in the study are applicable outside of the study to other populations and settings.
- Effect size
a value which reflects the magnitude of the difference in a study’s outcome measure between the group with the intervention/practice being evaluated and its control or comparison group.
- False positive blood culture
a culture with one or more contaminants producing a positive test result for a patient without a bloodstream infection. False positive rates are the percent of cultures contaminated relative to the total number of cultures positive.
- Fungemia
the presence of fungi (yeasts or molds) in the bloodstream.
- Internal validity
extent to which the design and conduct of the study are likely to prevent systematic error. Internal validity is a prerequisite for external validity.
- Meta-analysis
the process of using statistical methods to combine quantitatively the results of similar studies in an attempt to allow inferences to be made from the sample of studies and be applied to the population of interest.
- Non-phlebotomist staffs
hospital staff whose primary work responsibilities consist of duties other than collection of patient blood samples for laboratory tests by venipuncture [19,41].
- Odds ratio
-
the ratio of two odds of an event from two groups - a treatment or intervention group (a/c) versus a control group (b/d) where a and c represent the number of times the event occurs for the intervention and control group, respectively, using the formula below and the barcoding and comparison practice example table. An OR=1 means the two practices are equally successful (no difference in reducing risk with respect to the outcome evaluated); OR>1 means the barcoding practice is more successful; and OR<1 means the barcoding practice is less successful.
Odds ratio estimate formula: ;
Where pa = a/(a + b), pc = c/(c+d) and a, b, c, and d are proportions in the table below.
Frequencies
Proportions
Success Failure Success Failure Barcoding practice A B pa = a/(a + b) pb = b/(a + b) Comparison Practice C D pc = c/(c + d) pd = d/(c + d) - Phlebotomy team
a team of trained persons with primary responsibility for collecting blood for laboratory evaluation using sterile technique by puncture of a vein [19,41].
- Septicemia (also Bacteremia, Sepsis, Systemic inflammatory response syndrome (SIRS))
a serious systemic illness caused by bacteria and bacterial toxins circulating in the bloodstream.
- Systematic review
a scientific investigation that focuses on a specific question and that uses explicit, planned scientific methods to identify, select, assess, and summarize the findings of similar but separate studies. It may or may not include a quantitative synthesis of the results from separate studies (meta-analysis).
- Transparency
methods are explicitly defined, consistently applied, and available for public review so that observers can readily link judgments, decisions, or actions to the data on which they are based. Allows users to assess the strengths and weaknesses of the systematic review of the associated guidance and recommendations.
- Venipuncture
puncture of a vein. A method used to collect blood specimens for culture removed through a sterile needle inserted into a vein [1].
Appendix A. LMBP blood culture contamination expert panel members and LMBP Workgroup members
LMBP Blood Culture Contamination Expert Panel
Roberta Carey, PhD (Centers for Disease Control and Prevention)
Dennis Ernst, MT(ASCP) (Center for Phlebotomy Education)
Dana Grzybicki, MD, PhD (University of Colorado Denver)
Margret Oethinger, MD, PhD (Providence Portland Medical Center)
Stephen Raab, MD, PhDa (University of Washington)
Ronald Schifman, MD, MPH (Southern Arizona VA Healthcare System)
Ann Vannier, MDa (Kaiser-Permanente)
Melvin Weinstein, MD (University of Medicine, Dentistry of New Jersey-Robert Wood Johnson Medical School)
Laboratory Medicine Best Practices Work Group, 2008 – 2011
Raj Behal, MD, MPH (Rush University Medical Center)
Robert H. Christenson, PhD, DABCC, FACB (University of Maryland Medical Center)
John Fontanesi, PhD (University of California, San Diego)
Julie Gayken, MT (ASCP) (Regions Hospital)
Cyril (Kim) Hetsko, MD, FACP (University of Wisconsin-Madison, Chief Medical Officer, COLA and Trustee, American Medical Association)
Lee H. Hilborne, MD, MPH (UCLA David Geffen School of Medicine, President, American Society for Clinical Pathology, RAND, Quest Diagnostics)
James H. Nichols, PhD (Baystate Medical Center)
Mary Nix, MS, MT(ASCP)SBB (Agency for Healthcare Research and Quality)
Stephen S. Raab, MD (University of Colorado Denver School of Medicine)
Milenko Tanasijevic, MD, MBA (Brigham and Women’s Hospital, Dana Farber Cancer Institute, Harvard Medical School)
Ann M. Vannier, MD (Kaiser Permanente Southern California Regional Reference Laboratories)
Ann Watt, MBA, RHIA (The Joint Commission)
Ex-officio Members:
Sousan S. Altaie, PhD (Food and Drug Administration)
James Cometa (Centers for Medicaid and Medicare Services)
Appendix B. LMBP blood culture contamination systematic review eligible studies
Venipuncture vs. intravenous catheter collection
Included studies
Published
- Beutz M, Sherman G, Mayfield J, Fraser VJ, Kollef MH. Clinical utility of blood cultures drawn from central vein catheters and peripheral venipuncture in critically ill medical patients. Chest. 2003;123:854–61. doi: 10.1378/chest.123.3.854. [DOI] [PubMed] [Google Scholar]
- DesJardin JA, Falagas ME, Ruthazer R, Griffith J, Wawrose D, Schenkein D, et al. Clinical utility of blood cultures drawn from indwelling central venous catheters in hospitalized patients with cancer. Annals of Internal Medicine. 1999;131:641–7. doi: 10.7326/0003-4819-131-9-199911020-00002. [DOI] [PubMed] [Google Scholar]
- Everts RJ, Vinson EN, Adholla PO, Reller LB. Contamination of catheter-drawn blood cultures. Journal of Clinical Microbiology. 2001;39:3393–4. doi: 10.1128/JCM.39.9.3393-3394.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez JA, DesJardin JA, Aronoff M, Supran S, Nasraway SA, Snydman DR. Clinical utility of blood cultures drawn from central venous or arterial catheters in critically ill surgical patients. Critical Care Medicine. 2002;30:7–13. doi: 10.1097/00003246-200201000-00002. [DOI] [PubMed] [Google Scholar]
- McBryde ES, Tilse M, McCormack J. Comparison of contamination rates of catheter-drawn and peripheral blood cultures. The Journal of Hospital Infection. 2005;60:118–21. doi: 10.1016/j.jhin.2004.10.020. [DOI] [PubMed] [Google Scholar]
- Norberg A, Christopher NC, Ramundo ML, Bower JR, Berman SA. Contamination rates of blood cultures obtained by dedicated phlebotomy vs intravenous catheter. JAMA: the Journal of the American Medical Association. 2003;289:726–9. doi: 10.1001/jama.289.6.726. [DOI] [PubMed] [Google Scholar]
- Qamruddin A, Khanna N, Orr D. Peripheral blood culture contamination in adults and venepuncture technique: prospective cohort study. Journal of Clinical Pathology. 2008;61:509–13. doi: 10.1136/jcp.2007.047647. [DOI] [PubMed] [Google Scholar]
- Ramsook C, Childers K, Cron SG, Nirken M. Comparison of blood-culture contamination rates in a pediatric emergency room: newly inserted intravenous catheters versus venipuncture. Infection Control and Hospital Epidemiology: the Official Journal of the Society of Hospital Epidemiologists of America. 2000;21:649–51. doi: 10.1086/501708. [DOI] [PubMed] [Google Scholar]
- Weddle G, Jackson MA, Selvarangan R. Reducing blood culture contamination in a pediatric emergency department. Pediatric Emergency Care. 2011;27:179–81. doi: 10.1097/PEC.0b013e31820d652b. [DOI] [PubMed] [Google Scholar]
Excluded studies
Published
- Gonsalves WI, Cornish N, Moore M, Chen A, Varman M. Effects of volume and site of blood draw on blood culture results. Journal of Clinical Microbiology. 2009;47:3482–5. doi: 10.1128/JCM.02107-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
Phlebotomy teams
Included studies
Published
- Gander RM, Byrd L, DeCrescenzo M, Hirany S, Bowen M, Baughman J. Impact of blood cultures drawn by phlebotomy on contamination rates and health care costs in a hospital emergency department. Journal of Clinical Microbiology. 2009;47:1021–4. doi: 10.1128/JCM.02162-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheppard C, Franks N, Nolte F, Fantz C. Improving quality of patient care in an emergency department: a laboratory perspective. American Journal of Clinical Pathology. 2008;130:573–7. doi: 10.1309/DGXYTH0VNTTQRQHD. [DOI] [PubMed] [Google Scholar]
- Surdulescu S, Utamsingh D, Shekar R. Phlebotomy teams reduce blood-culture contamination rate and save money. Clinical Performance and Quality Health Care. 1998;6:60–2. [PubMed] [Google Scholar]
- Weinbaum FI, Lavie S, Danek M, Sixsmith D, Heinrich GF, Mills SS. Doing it right the first time: quality improvement and the contaminant blood culture. Journal of Clinical Microbiology. 1997;35:563–5. doi: 10.1128/jcm.35.3.563-565.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
Unpublished
- Geisinger Wyoming Valley Hospital; 2009.
Excluded
Unpublished
- Providence Regional Medical Center Everett, WA 2009
Prepackaged prep kit
Included studies
Published
- McLellan E, Townsend R, Parsons HK. Evaluation of chloraprep (2% chlorhexidine gluconate in 70% isopropyl alcohol) for skin antisepsis in preparation for blood culture collection. The Journal of Infection. 2008;57:459–63. doi: 10.1016/j.jinf.2008.08.012. [DOI] [PubMed] [Google Scholar]
- Trautner BW, Clarridge JE, Darouiche RO. Skin antisepsis kits containing alcohol and chlorhexidine gluconate or tincture of iodine are associated with low rates of blood culture contamination. Infection Control and Hospital Epidemiology: the Official Journal of the Society of Hospital Epidemiologists of America. 2002;23:397–401. doi: 10.1086/502073. [DOI] [PubMed] [Google Scholar]
- Weinbaum FI, Lavie S, Danek M, Sixsmith D, Heinrich GF, Mills SS. Doing it right the first time: quality improvement and the contaminant blood culture. Journal of Clinical Microbiology. 1997;35:563–5. doi: 10.1128/jcm.35.3.563-565.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson ML, Weinstein MP, Mirrett S, Reimer LG, Fernando C, Meredith FT, et al. Comparison of iodophor and alcohol pledgets with the medi-flex blood culture prep kit II for preventing contamination of blood cultures. Journal of Clinical Microbiology. 2000;38:4665–7. doi: 10.1128/jcm.38.12.4665-4667.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
Excluded studies
Published
- Madeo M, Davies D, Owen L, Wadsworth P, Johnson G, Martin CR. Reduction in the contamination rate of blood cultures collected by medical staff in the accident and emergency department. Clinical Effectiveness in Nursing. 2003;7:30–2. [Google Scholar]
Appendix C. Supplementary data
Supplementary data to this article can be found online at http://dx.doi.org/10.1016/j.clinbiochem.2012.06.007.
Footnotes
Funding source: CDC funding for the Laboratory Medicine Best Practices Initiative to Battelle Centers for Public Health Research and Evaluation under contract W911NF-07-D-0001/DO 0191/TCN 07235.
See Glossary for more information on the definition of blood culture contamination and other terms.
See Appendix A for the LMBP Blood Culture Contamination Expert Panel Members and LMBP Workgroup members. See Appendix Edits/Notes.
More information on submission of unpublished studies to the Laboratory Medicine Best Practices Initiative is available at www.futurelabmedicine.org.
See Glossary for more information on odds ratios.
The criteria for a substantial effect size rating: OR>2.0 and significantly different from OR=1.0 at p=0.05 (i.e., the lower limit of the 95% confidence interval is>1.0).
Random-effects model assumes there is no common population effect size for the included studies and the studies’ effect size variation follows a distribution with the studies representing a random sample. This is in contrast to the fixed-effects model which assumes a single population effect size for all studies and that observed differences reflect random variation.
Laboratory Medicine Best Practices Workgroup member.
Disclaimer
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention/the Agency for Toxic Substances and Disease Registry (CDC/ATSDR).
References
- 1.Wilson ML, Clinical I. Laboratory standards, principles and procedures for blood cultures: approved guideline. Wayne, Pa: Clinical and Laboratory Standards Institute; 2007. [Google Scholar]
- 2.Baron EJ, Weinstein MP, Dunne WM, Jr, Yagupsky P, Welch DF, Wilson DM. Cumitech 1C, blood cultures IV. Washington, D.C: ASM Press; 2005. [Google Scholar]
- 3.Hall KK, Lyman JA. Updated review of blood culture contamination. Clin Microbiol Rev. 2006;19:788–802. doi: 10.1128/CMR.00062-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elixhauser A, Friedman B, Stranges E. Septicemia in U.S. Hospitals, 2009, HCUP statistical brief #122. Rockville, MD: Agency for Healthcare Research and Quality; 2011. [PubMed] [Google Scholar]
- 5.Hall MJ, Williams SN, Defrances CJ, Golosinskiy A. Inpatient care for septicemia or sepsis: a challenge for patients and hospitals. NCHS Data Brief. 2011:1–8. [PubMed] [Google Scholar]
- 6.McLellan E, Townsend R, Parsons HK. Evaluation of ChloraPrep (2% chlorhexidine gluconate in 70% isopropyl alcohol) for skin antisepsis in preparation for blood culture collection. J Infect. 2008;57:459–63. doi: 10.1016/j.jinf.2008.08.012. [DOI] [PubMed] [Google Scholar]
- 7.Bekeris LG, Tworek JA, Walsh MK, Valenstein PN. Trends in blood culture contamination: a College of American Pathologists Q-Tracks study of 356 institutions. Arch Pathol Lab Med. 2005;129:1222–5. doi: 10.5858/2005-129-1222-TIBCCA. [DOI] [PubMed] [Google Scholar]
- 8.Robert RR. Reducing blood-culture contamination through an education program. J Infus Nurs. 2011;34:49–54. doi: 10.1097/NAN.0b013e31820219c1. [DOI] [PubMed] [Google Scholar]
- 9.Weinstein MP. Blood culture contamination: persisting problems and partial progress. J Clin Microbiol. 2003;41:2275–8. doi: 10.1128/JCM.41.6.2275-2278.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paxton A. Nipping contamination in the blood. CAP Today. 2000;14:1. [56, 58, 60 passim] [PubMed] [Google Scholar]
- 11.Schifman RB, Strand CL, Meier FA, Howanitz PJ. Blood culture contamination: a College of American Pathologists Q-Probes study involving 640 institutions and 497134 specimens from adult patients. Arch Pathol Lab Med. 1998;122:216–21. [PubMed] [Google Scholar]
- 12.Zwang O, Albert RK. Analysis of strategies to improve cost effectiveness of blood cultures. J Hosp Med. 2006;1:272–6. doi: 10.1002/jhm.115. [DOI] [PubMed] [Google Scholar]
- 13.Sheppard C, Franks N, Nolte F, Fantz C. Improving quality of patient care in an emergency department: a laboratory perspective. Am J Clin Pathol. 2008;130:573–7. doi: 10.1309/DGXYTH0VNTTQRQHD. [DOI] [PubMed] [Google Scholar]
- 14.Souvenir D, Anderson DE, Jr, Palpant S, Mroch H, Askin S, Anderson J, et al. Blood cultures positive for coagulase-negative staphylococci: antisepsis, pseudobacteremia, and therapy of patients. J Clin Microbiol. 1998;36:1923–6. doi: 10.1128/jcm.36.7.1923-1926.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stohl S, Benenson S, Sviri S, Avidan A, Block C, Sprung CL, et al. Blood cultures at central line insertion in the intensive care unit: comparison with peripheral venipuncture. J Clin Microbiol. 2011;49:2398–403. doi: 10.1128/JCM.02546-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Surdulescu S, Utamsingh D, Shekar R. Phlebotomy teams reduce blood-culture contamination rate and save money. Clin Perform Qual Health Care. 1998;6:60–2. [PubMed] [Google Scholar]
- 17.Suwanpimolkul G, Pongkumpai M, Suankratay C. A randomized trial of 2% chlor-hexidine tincture compared with 10% aqueous povidone-iodine for venipuncture site disinfection: effects on blood culture contamination rates. J Infect. 2008;56:354–9. doi: 10.1016/j.jinf.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 18.Weddle G, Jackson MA, Selvarangan R. Reducing blood culture contamination in a pediatric emergency department. Pediatr Emerg Care. 2011;27:179–81. doi: 10.1097/PEC.0b013e31820d652b. [DOI] [PubMed] [Google Scholar]
- 19.Weinbaum FI, Lavie S, Danek M, Sixsmith D, Heinrich GF, Mills SS. Doing it right the first time: quality improvement and the contaminant blood culture. J Clin Microbiol. 1997;35:563–5. doi: 10.1128/jcm.35.3.563-565.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim NH, Kim M, Lee S, Yun NR, Kim KH, Park SW, et al. Effect of routine sterile gloving on contamination rates in blood culture: a cluster randomized trial. Ann Intern Med. 2011;154:145–51. doi: 10.7326/0003-4819-154-3-201102010-00003. [DOI] [PubMed] [Google Scholar]
- 21.Thuler LC, Jenicek M, Turgeon JP, Rivard M, Lebel P, Lebel MH. Impact of a false positive blood culture result on the management of febrile children. Pediatr Infect Dis J. 1997;16:846–51. doi: 10.1097/00006454-199709000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Alahmadi YM, Aldeyab MA, McElnay JC, Scott MG, Darwish Elhajji FW, Magee FA, et al. Clinical and economic impact of contaminated blood cultures within the hospital setting. J Hosp Infect. 2011;77:233–6. doi: 10.1016/j.jhin.2010.09.033. [DOI] [PubMed] [Google Scholar]
- 23.Bates DW, Goldman L, Lee TH. Contaminant blood cultures and resource utilization. The true consequences of false-positive results. JAMA. 1991;265:365–9. [PubMed] [Google Scholar]
- 24.Caldeira D, David C, Sampaio C. Skin antiseptics in venous puncture-site disinfection for prevention of blood culture contamination: systematic review with meta-analysis. J Hosp Infect. 2011;77:223–32. doi: 10.1016/j.jhin.2010.10.015. [DOI] [PubMed] [Google Scholar]
- 25.Spitalnic SJ, Woolard RH, Mermel LA. The significance of changing needles when inoculating blood cultures: a meta-analysis. Clin Infect Dis. 1995;21:1103–6. doi: 10.1093/clinids/21.5.1103. [DOI] [PubMed] [Google Scholar]
- 26.Christenson RH, Snyder SR, Shaw CS, Derzon JH, Black RS, Mass D, et al. Laboratory medicine best practices: systematic evidence review and evaluation methods for quality improvement. Clin Chem. 2011;57:816–25. doi: 10.1373/clinchem.2010.157131. [DOI] [PubMed] [Google Scholar]
- 27.Institute of Medicine. Committee on standards for systematic reviews of comparative effectiveness research. Finding what works in health care: standards for systematic reviews. 2011 [Google Scholar]
- 28.CDC Laboratory Medicine Best Practices Team. Laboratory medicine best practices: developing systematic evidence review and evaluation methods for quality improvement — phase 3 final technical report. 2010 [Google Scholar]
- 29.Raudenbush SW. Random effects models. In: Cooper H, Hedges LV, editors. The handbook of research synthesis. New York: Russell Sage; 1994. pp. 301–21. [Google Scholar]
- 30.Hedges LV. A random effects model for effect sizes. Psychol Bull. 1983;93:388–95. [Google Scholar]
- 31.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 32.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Br Med J. 2003:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Borenstein M. Introduction to meta-analysis. Chichester, West Sussex, U.K.; Hoboken: John Wiley & Sons; 2009. [Google Scholar]
- 34.DesJardin JA, Falagas ME, Ruthazer R, Griffith J, Wawrose D, Schenkein D, et al. Clinical utility of blood cultures drawn from indwelling central venous catheters in hospitalized patients with cancer. Ann Intern Med. 1999;131:641–7. doi: 10.7326/0003-4819-131-9-199911020-00002. [DOI] [PubMed] [Google Scholar]
- 35.Beutz M, Sherman G, Mayfield J, Fraser VJ, Kollef MH. Clinical utility of blood cultures drawn from central vein catheters and peripheral venipuncture in critically ill medical patients. Chest. 2003;123:854–61. doi: 10.1378/chest.123.3.854. [DOI] [PubMed] [Google Scholar]
- 36.Ramsook C, Childers K, Cron SG, Nirken M. Comparison of blood-culture contamination rates in a pediatric emergency room: newly inserted intravenous catheters versus venipuncture. Infect Control Hosp Epidemiol. 2000;21:649–51. doi: 10.1086/501708. [DOI] [PubMed] [Google Scholar]
- 37.Qamruddin A, Khanna N, Orr D. Peripheral blood culture contamination in adults and venepuncture technique: prospective cohort study. J Clin Pathol. 2008;61:509–13. doi: 10.1136/jcp.2007.047647. [DOI] [PubMed] [Google Scholar]
- 38.Norberg A, Christopher NC, Ramundo ML, Bower JR, Berman SA. Contamination rates of blood cultures obtained by dedicated phlebotomy vs intravenous catheter. JAMA. 2003;289:726–9. doi: 10.1001/jama.289.6.726. [DOI] [PubMed] [Google Scholar]
- 39.Martinez JA, DesJardin JA, Aronoff M, Supran S, Nasraway SA, Snydman DR. Clinical utility of blood cultures drawn from central venous or arterial catheters in critically ill surgical patients. Crit Care Med. 2002;30:7–13. doi: 10.1097/00003246-200201000-00002. [DOI] [PubMed] [Google Scholar]
- 40.Everts RJ, Vinson EN, Adholla PO, Reller LB. Contamination of catheter-drawn blood cultures. J Clin Microbiol. 2001;39:3393–4. doi: 10.1128/JCM.39.9.3393-3394.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gander RM, Byrd L, DeCrescenzo M, Hirany S, Bowen M, Baughman J. Impact of blood cultures drawn by phlebotomy on contamination rates and health care costs in a hospital emergency department. J Clin Microbiol. 2009;47:1021–4. doi: 10.1128/JCM.02162-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Should non-phlebotomists be allowed to draw blood? Clin Leadersh Manag Rev. 2001;15:426–8. [PubMed] [Google Scholar]
- 43.Brown JE, Smith N, Sherfy BR. Decreasing mislabeled laboratory specimens using barcode technology and bedside printers. J Nurs Care Qual. 2011 Jan-Mar;26(1):13–21. doi: 10.1097/NCQ.0b013e3181e4e6dd. [DOI] [PubMed] [Google Scholar]
- 44.Bologna LJ, Mutter M. Life after phlebotomy deployment: reducing major patient and specimen identification errors. J Healthc Inf Manag. 2002;16:65–70. [PubMed] [Google Scholar]
- 45.Ernst DJ. Has decentralized phlebotomy run its course? MLO Med Lab Obs. 2009;41:20. [22] [PubMed] [Google Scholar]