Abstract
Introduction:
Patellofemoral pain syndrome (PFPS) is characterized by anterior knee pain, which may limit the performance of functional activities. The influence of hip joint motion on the development of this syndrome has already been documented in the literature. In this regard, studies have investigated the effectiveness of hip muscle strengthening in patients with PFPS.
Objectives:
The aims of this systematic review were (1) to summarize the literature related to the effects of hip muscle strengthening on pain intensity, muscle strength, and function in individuals with PFPS and (2) to evaluate the methodological quality of the selected studies.
Method:
A search for randomized controlled clinical trials was conducted using the following databases: Google Scholar, MEDLINE, PEDro, LILACS, and SciELO. The selected studies had to distinguish the effects of hip muscle strengthening in a group of patients with PFPS, as compared to non-intervention or other kinds of intervention, and had to investigate the following outcomes: pain, muscle strength, and function. The methodological quality of the selected studies was analyzed by means of the PEDro scale.
Results:
Seven studies were selected. These studies demonstrated that hip muscle strengthening was effective in reducing pain. However, the studies disagreed regarding the treatments' ability to improve muscle strength. Improvement in functional capabilities after hip muscle strengthening was found in five studies.
Conclusion:
Hip muscle strengthening is effective in reducing the intensity of pain and improving functional capabilities in patients with PFPS, despite the lack of evidence for its ability to increase muscle strength.
Keywords: patellofemoral pain syndrome, muscle strengthening, pain, function, hip, rehabilitation
Introduction
Patellofemoral pain syndrome (PFPS) is characterized by retro or peripatellar pain, mainly during weight-bearing activities, such as ascending and descending stairs1. In addition to pain, the clinical presentation of this syndrome includes muscular weakness and altered lower limb biomechanics2. PFPS is considered the most common overuse injury of the lower limb and is more prevalent in physically active individuals3 , 4. Physiotherapy is recommended for reducing the pain intensity and functional limitations associated with PFPS5. Traditional treatments aim at improving patellar alignment and strengthening the knee muscles6. However, several studies highlight the influence of other joints, such as hip, in the development of this syndrome.
In recent years, hip muscle strengthening has been proposed as a proper treatment for patients with PFPS. The rationale for this intervention is supported by the theoretical background hypothesizing that excessive hip motion, especially in frontal and transverse planes, places stress on the patellofemoral joint3. This excessive hip motion may be related to the weakness of muscles surrounding the hip joint7 - 11. In this case, patients with PFPS could benefit from hip muscle strengthening, since this intervention may reduce excessive hip motion and, as a consequence, excessive patellofemoral joint stress. As a result, hip muscle strengthening has been proposed as an effective treatment to reduce pain and improve function in PFPS patients.
In 2003, Mascal et al.12 suggested an intervention for PFPS that included strengthening of hip muscles and showed clinical improvement in two patients. After this initial study, other studies were performed to investigate the effects of hip muscle strengthening on the improvement of patients with PFPS13 - 19. However, results of these studies were equivocal and only a few were randomized controlled trials (RCT). RCT is considered the best study design to evaluate the effects of an intervention since the randomization protects against allocation bias20. In order to combine the evidence provided by these studies and reveal the true contribution of hip muscle strengthening to the treatment of patients with PFPS, a systematic review of this literature is needed. Thus, the aims of this systematic review were (1) to summarize the literature related to the effects of hip muscle strengthening on pain intensity, muscle strength, and function in individuals with PFPS and (2) to evaluate the methodological quality of the selected studies. The results of this review may help researchers to plan future studies since they can refine hypotheses, recognize and avoid pitfalls of previous studies, and estimate sample sizes21. Furthermore, this review may contribute to integrate existing knowledge about the effects of hip muscle strengthening on patellofemoral pain syndrome and provide data for clinical decision making21.
Method
A search was conducted among studies published in English, Portuguese, and Spanish using the databases Google Scholar, MEDLINE, PEDro, LILACS, and SciELO. The following keywords were used: patellofemoral pain syndrome, hip, strengthening, physical therapy, rehabilitation, and their correlates in Portuguese and Spanish. Furthermore, the reference lists of the selected studies were also investigated. There was no restriction as to the publication dates of the articles; the search was conducted between August, 2013 and September, 2014.
Only randomized controlled clinical trials (RCT) that included volunteers with PFPS were selected. In order to be included in the final review, the studies had to allow discrimination of the effects of hip muscle strengthening in a group of patients with PFPS, as compared to non-intervention or another kind of intervention. In addition, the articles had to investigate at least one of the following outcomes: pain, muscle strength, and function. In this review, the experimental group was identified as that in which the intervention activities contained at least hip muscle strengthening. On the other hand, the control group was the one in which no intervention or any other type of treatment was applied.
In order to identify and characterize the variables applicable to the present study, the following information was extracted from the selected studies: type and characteristics of the intervention, applicable variables, and evaluation instruments used. Furthermore, the methodological quality of the studies was analyzed based on the score in the Physiotherapy Evidence Database (PEDro) scale provided by PEDro database. If the selected study was not scored in this database, the authors would rank using the Portuguese (Brazilian) version of the scale22. In that case, the analysis would be performed independently by two evaluators and disagreements resolved by discussion and consensus.
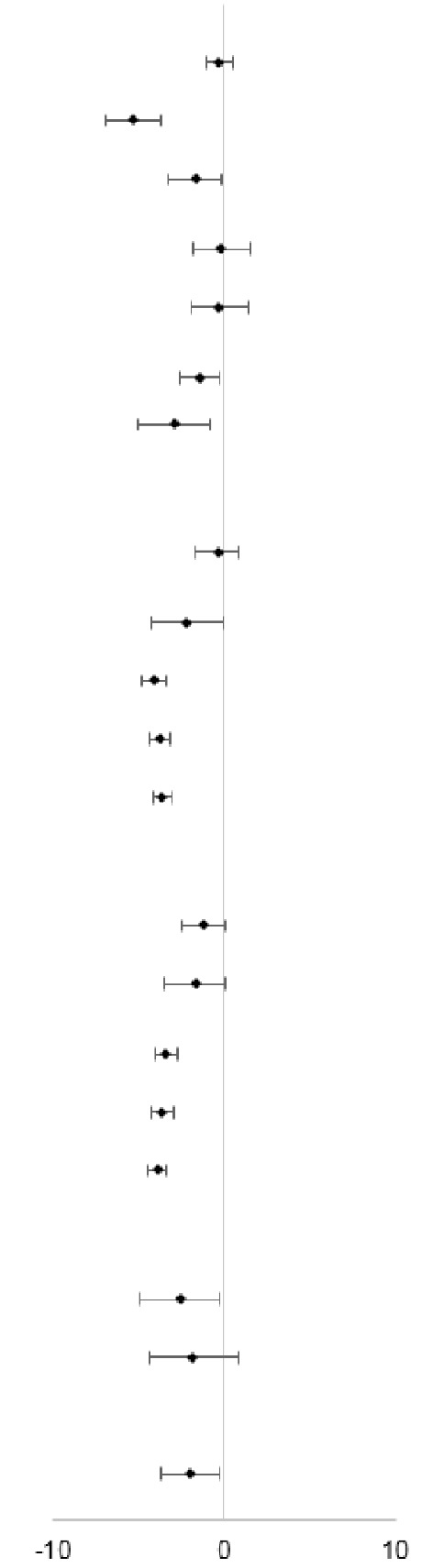
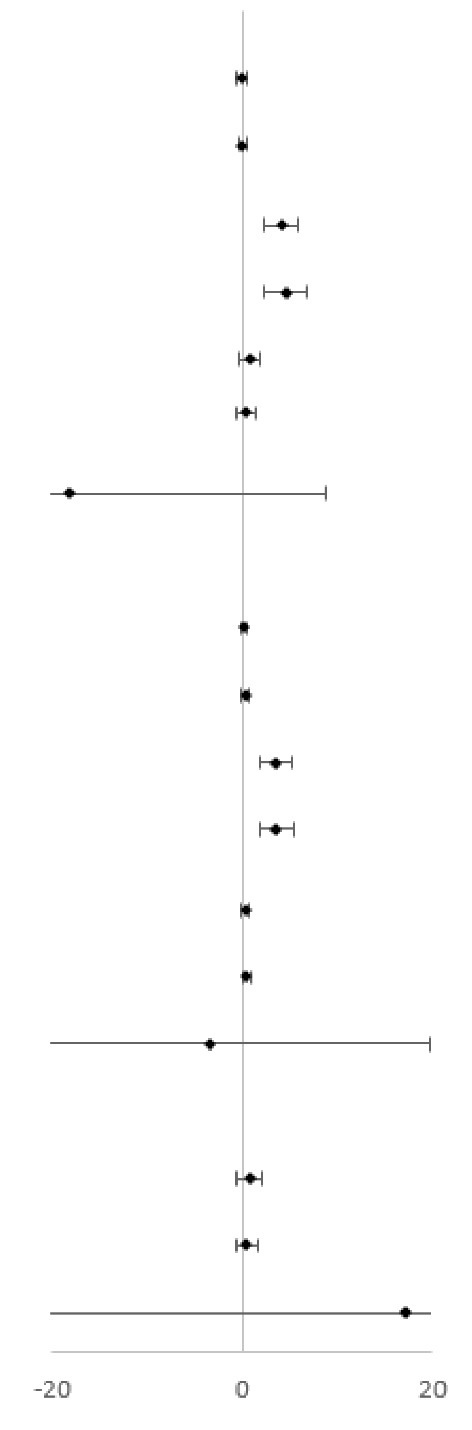
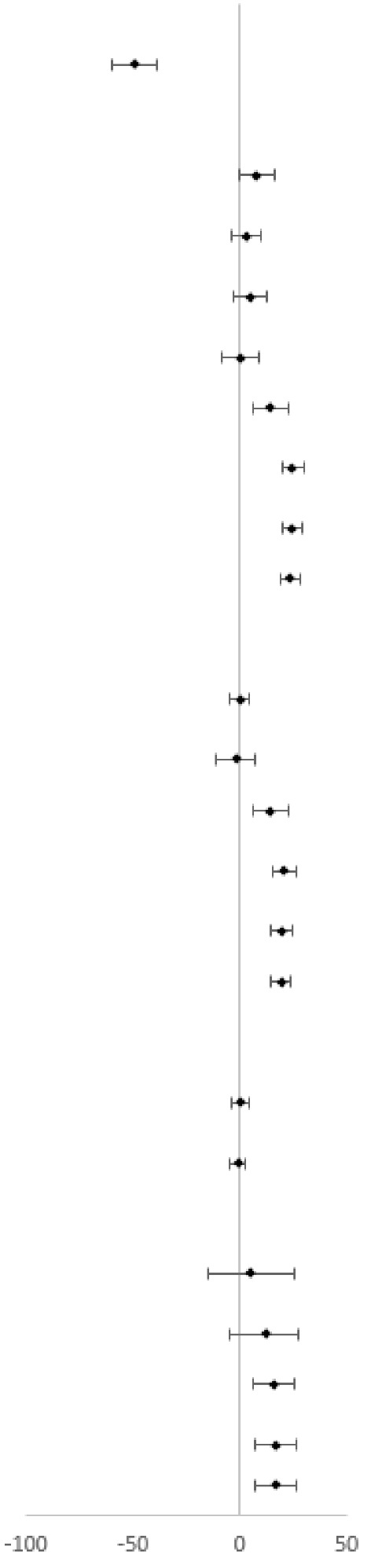
The quantitative synthesis of the results of the studies was shown using forest plots. Since the variables were treated as continuous by the studies, the intervention effect was analyzed using the mean difference between groups after intervention, with a 95% confidence interval, calculated using Cochrane Collaboration's RevMan 5.2 software.
Results
The search strategy yielded 2381 studies (Google Scholar = 1904, MEDLINE = 299, PEDro = 100, LILACS = 34, SciELO = 44), of which 2265 were excluded after reading the title and 20 were duplicates. Of the remaining 96 studies identified for possible inclusion, 78 were excluded after reading the abstracts. Thus, 18 studies were selected. Of these 18 studies, 12 were excluded after full reading, since they did not apply hip muscle strengthening intervention or did not investigate at least one of the clinical outcomes considered in this review. Additionally, one study was included following a search of the reference lists of the selected studies. Thus, seven studies were included in this review. Table 1 demonstrates the details of the intervention of the selected studies, as well as the clinical outcomes investigated therein. All selected studies were scored in the PEDro database and the results for each item are shown in Table 2.
Table 1. Details of the intervention and outcomes of the included studies.
| Study | Intervention | Outcomes |
|---|---|---|
| Ismail et al.13 | EG: HABD and HLR strengthening. EG and CG: CKC (mini wall squat, forward step up, lateral step up, and terminal knee extension), stretching (HS, ITB, GN and QUADS). Duration: 6wks, 3 supervised sessions per wk. | Pain (Average pain in the previous week): 10-cm VAS; Function: AKPS; Strength: Concentric and eccentric HABD and HLR. |
| Fukuda et al.14 | EG: HABD, HEXT and HLR strengthening. EG and CG: KEXT, KFLX and APF strengthening; squatting; stretching (HS, TS, QUADS and ITB). Duration: 3 supervised sessions per wk for 6 wks. | Pain (Ascending and descending stairs): NPRS. Function: LEFS, AKPS and single-hop test. |
| Khayambashi et al.15 | EG: 5-min warm up (walking at self-selected pace); 20 min of bilateral HABD and HLR strengthening; 5-min cool down (walking at self-selected pace). Duration: 8wks, 3 supervised sessions per wk. CG: Omega-3 and calcium daily for 8 wks. | Pain (Average pain while performing activities that aggravated symptoms during the previous week): 10-cm VAS; Function: WOMAC; Strength: Isometric HABD and HLR. |
| Dolak et al.16 | EG: HABD and HLR strengthening. EG and CG:Stretching (HS, QUADS and TS); orientations; functional weight-bearing resistance exercises and balance; QUADS strengthening. Duration: 8wks, 3 times per wk, 1 supervision session per wk. | Pain (Worst pain in the previous wk): VAS; Function: LEFS, step-down task; Strength: Isometric HABD and HLR. |
| Razeghi et al.17 | EG: HFLX, HEXT, HABD, HADD, HMR, HLR strengthening. EG and CG: QUADS strengthening. Duration: 4 wks; supervision was not informed. | Pain: 10-cm VAS. |
| Fukuda et al.18 | EG: HABD, HLR strengthening. EG and CGa:Stretching (HS, TS, QUADS and ITB); QUADS and IP strengthening; squatting. Duration: 4wks, 3 supervised sessions per wk. CGb: No intervention. | Pain (Ascending and descending stairs): NPRS; Function: LEFS, AKPS and single-limb single hop test. |
| Nakagawa et al.19 | EG: Strengthening and functional training exercises focused on the TA, HABD and HLR. EG and CG: Patellar mobilization; stretching (QUADS, GN, ITB and HS); QUADS strengthening. Duration: 6 wks, 5 times per wk, 1 supervision session per wk. | Pain (Worst and usual pain in the last week; pain during stair-climbing, descending stair, squatting and prolonged sitting): 10-cm VAS; Strength: Eccentric KEXT, HABD and HLR. |
wk = week; wks = weeks; EG = Experimental Group; CG, CGa and CGb = Control Group; PFPS = Patellofemoral Pain Syndrome; GN = Gastrocnemius; HABD = Hip abductors; HADD = Hip adductors; HEXT = Hip extensors; HFLX = Hip flexors; HLR = Hip lateral rotators; HMR = Hip medial rotators; HS = Hamstrings; ITB = Iliotibial band; IP = Iliopsoas; KEXT = Knee extensors; KFLX = Knee flexors; APF = Ankle plantar flexors; QUADS = Quadriceps; TA = Transversus abdominis; TS = Triceps surae; CKC= Closed Kinetic Chain; NPRS = Numeric Pain Rating Scale; VAS = Visual Analogue Scale; LEFS = Lower Extremity Functional Scale; AKPS = Anterior Knee Pain Scale; WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index.
Table 2. PEDro scores of included studies.
| Study | Items | Total | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | ||
| Ismail et al.13 | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | 8 |
| Fukuda et al.14 | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | 8 |
| Khayambashi et al.15 | Yes | Yes | No | Yes | No | No | No | Yes | No | Yes | Yes | 5 |
| Dolak et al.16 | Yes | Yes | No | Yes | No | No | Yes | No | Yes | Yes | Yes | 6 |
| Razeghi et al.17 | Yes | Yes | No | No | No | No | No | Yes | No | Yes | Yes | 4 |
| Fukuda et al.18 | Yes | Yes | Yes | Yes | No | No | Yes | Yes | No | Yes | Yes | 7 |
| Nakagawa et al.19 | No | Yes | Yes | Yes | No | No | Yes | Yes | Yes | No | Yes | 7 |
The total represents the score in the PEDro scale. Item 1 is not included in this score22.
Means and standard deviations of pain, function, and muscle strength after the intervention are shown according to the group (experimental and control) for each analyzed study in Tables 3, 4, and 5. Furthermore, these tables present the sample size in each group and the 95% confidence interval of the mean difference between groups, which is also shown in the Forest plots.
Table 3. Quantitative synthesis of the results for pain intensity.
| Study | Experimental | Control | Mean Difference 95% CI | Forest plot | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| X | SD | N | X | SD | N | |||||
| Usual pain intensity |
|
|||||||||
| Ismail et al.13 | 2 | 1.1 | 16 | 2.3 | 1.1 | 16 | -0.3 [-1.1, 0.5] | |||
| Khayambashi et al.15 | 1.4 | 1.9 | 14 | 6.7 | 2.4 | 14 | -5.3 [-6.9, -3.7] | |||
| Dolak et al.16 (1) | 2.4 | 2 | 17 | 4.1 | 2.5 | 16 | -1.7 [-3.3, -0.2] | |||
| Dolak et al.16 (2) | 2.4 | 2.8 | 17 | 2.6 | 2 | 16 | -0.2 [-1.9, 1.5] | |||
| Dolak et al.16 (3) | 2.1 | 2.5 | 17 | 2.4 | 2.3 | 16 | -0.3 [-1.9, 1.3] | |||
| Razeghi et al.17 | 3.4 | 1.5 | 16 | 4.8 | 1.8 | 16 | -1.4 [-2.6, -0.3] | |||
| Nakagawa et al.19 | 1.1 | 1.2 | 7 | 4 | 2.6 | 7 | -2.9 [-5.0, -0.8] | |||
| Pain intensity in ascending stairs | ||||||||||
| Fukuda et al.18 | 3 | 1.8 | 21 | 3.4 | 2.3 | 20 | -0.4 [-1.7, 0.9] | |||
| Nakagawa et al.19 | 0.4 | 0.6 | 7 | 2.6 | 2.8 | 7 | -2.2 [-4.3, -0.1] | |||
| Fukuda et al.14 (4) | 1.2 | 1.1 | 25 | 5.3 | 1.3 | 24 | -4.1 [-4.8, -3.4] | |||
| Fukuda et al.14 (5) | 1.7 | 1 | 25 | 5.5 | 1.2 | 24 | -3.8 [-4.4, -3.2] | |||
| Fukuda et al.14 (6) | 2.9 | 0.8 | 25 | 6.5 | 1 | 24 | -3.6 [-4.1, -3.1] | |||
| Pain intensity in descending stairs | ||||||||||
| Fukuda et al.18 | 2.3 | 1.5 | 21 | 3.5 | 2.5 | 20 | -1.2 [-2.5, 0.1] | |||
| Nakagawa et al.19 | 0.3 | 0.4 | 7 | 2 | 2.4 | 7 | -1.7 [-3.5, 0.1] | |||
| Fukuda et al.14 (4) | 1.6 | 1.1 | 25 | 5 | 1.2 | 24 | -3.4 [-4.1, -2.8] | |||
| Fukuda et al.14 (5) | 2 | 0.8 | 25 | 5.6 | 1.4 | 24 | -3.6 [-4.2, -3.0] | |||
| Fukuda et al.14 (6) | 2.5 | 0.9 | 25 | 6.4 | 1.1 | 24 | -3.9 [-4.5, -3.3] | |||
| Pain intensity in other activities | ||||||||||
| Nakagawa et al.19 (7) | 0.4 | 0.6 | 7 | 3 | 3.1 | 7 | -2.6 [-4.9, -0.3] | |||
| Nakagawa et al.19 (8) | 1.1 | 1.6 | 7 | 2.9 | 3.1 | 7 | -1.8 [-4.4, 0.8] | |||
| Worst pain intensity | ||||||||||
| Nakagawa et al.19 | 1.4 | 1.3 | 7 | 3.4 | 1.9 | 7 | -2 [-3.7, -0.3] | |||
| Favors Experimental | Favors Control | |||||||||
X = Mean; SD = Standard deviation; N = Sample size; 95% CI = 95% Confidence Interval; (1) = 4 weeks; (2) = 8 weeks; (3) = 12 weeks; (4) = 3 months; (5) = 6 months; (6) = 12 months; (7) = Squatting; (8) = Sitting for prolonged time.
Table 4. Quantitative synthesis of the results for muscle strength.
| Study | Experimental | Control | Mean Difference 95% CI | Forest Plot | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| X | SD | N | X | SD | N | |||||
| Hip abductors |
|
|||||||||
| Ismail et al.13 (1) | 2.4 | 0.8 | 16 | 2.5 | 0.7 | 16 | -0.1 [-0.6, 0.4] | |||
| Ismail et al.13 (2) | 2.4 | 0.8 | 16 | 2.4 | 0.5 | 16 | 0 [-0.5, 0.5] | |||
| Khayambashi et al.15 (3) | 15.3 | 2.5 | 14 | 11.2 | 2.5 | 14 | 4.1 [2.3, 6.0] | |||
| Khayambashi et al.15 (4) | 15.9 | 3.1 | 14 | 11.4 | 3.1 | 14 | 4.5 [2.2, 6.8] | |||
| Dolak et al.16 (5) | 6.2 | 1.1 | 17 | 5.5 | 1.9 | 16 | 0.7 [-0.4, 1.8] | |||
| Dolak et al.16 (6) | 6.6 | 0.9 | 17 | 6.2 | 1.8 | 16 | 0.4 [-0.6, 1.4] | |||
| Nakagawa et al.19 | 102.2 | 19.8 | 7 | 120.4 | 30.4 | 7 | -18.2 [-45.1, 8.7] | |||
| Hip lateral rotators | ||||||||||
| Ismail et al.13 (1) | 1.3 | 0.6 | 16 | 1.2 | 0.4 | 16 | 0.1 [-0.3, 0.5] | |||
| Ismail et al.13 (2) | 1.8 | 0.8 | 16 | 1.6 | 0.3 | 16 | 0.2 [-0.2, 0.6] | |||
| Khayambashi et al.15 (3) | 11.8 | 2.2 | 14 | 8.3 | 2.3 | 14 | 3.5 [1.8, 5.2] | |||
| Khayambashi et al.15 (4) | 10.9 | 2.6 | 14 | 7.3 | 1.9 | 14 | 3.6 [1.9, 5.3] | |||
| Dolak et al.16 (5) | 2.5 | 0.7 | 17 | 2.2 | 0.8 | 16 | 0.3 [-0.2, 0.8] | |||
| Dolak et al.16 (6) | 2.7 | 0.7 | 17 | 2.2 | 0.7 | 16 | 0.5 [0.02, 1.0] | |||
| Nakagawa et al.19 | 59.4 | 18.9 | 7 | 62.9 | 24.9 | 7 | -3.5 [-26.7, 19.7] | |||
| Knee extensors | ||||||||||
| Dolak et al.16 (5) | 6.8 | 1.9 | 17 | 6.1 | 1.9 | 16 | 0.7 [-0.6, 2.0] | |||
| Dolak et al.16 (6) | 7 | 1.4 | 17 | 6.6 | 1.9 | 16 | 0.4 [-0.7, 1.5] | |||
| Nakagawa et al.19 | 318.9 | 96.8 | 7 | 301.9 | 63.4 | 7 | 17.0 [-68.7, 102.7] | |||
| Favors Control | Favors Experimental | |||||||||
X = Mean; SD = Standard deviation; N = Sample size; 95% CI = 95% Confidence Interval; (1) = Concentric; (2) = Eccentric; (3) Right side; (4) = Left side; (5) = 4 weeks; (6) = 8 weeks. Ismail et al.13 measured concentric and eccentric strength (peak torque in Nm/body mass index in Kg/m2); Khayambashi et al.15 measured isometric strength (force in N/body weight in N x 100); Dolak et al.16 measured isometric strength [(torque in Nm/body weight in N) x (participant height in m x 100)]; Nakagawa et al.19 measured eccentric strength (peak torque in Nm/body mass in Kg). The upper and lower limits from Nakagawa et al.19 data are not showed in the Forest Plot because of the differences in strength units among studies in order to show the data from the other studies in a better scale.
Table 5. Quantitative synthesis of the results for function.
| Study | Experimental | Control | Mean Difference 95% CI | Forest plot | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| X | DP | N | X | DP | N | |||||
| WOMAC |
|
|||||||||
| Khayambashi et al.15 | 10.7 | 16.1 | 14 | 59.9 | 12.6 | 14 | -49.2 [-59.9, -38.5] | |||
| LEFS | ||||||||||
| Dolak et al.16 (1) | 67 | 11 | 17 | 59 | 14 | 16 | 8.0 [-0.6, 16.6] | |||
| Dolak et al.16 (2) | 70 | 10 | 17 | 67 | 11 | 16 | 3.0 [-4.2, 10.2] | |||
| Dolak et al.16 (3) | 70 | 10 | 17 | 65 | 13 | 5 | -5.0 [-3.0, 13.0] | |||
| Fukuda et al.18 (4) | 65.7 | 13.5 | 21 | 65.6 | 14.5 | 20 | 0.1 [-8.5, 8.7] | |||
| Fukuda et al.18 (5) | 65.7 | 13.5 | 21 | 51.2 | 15.1 | 23 | 14.5 [6.1, 23.0] | |||
| Fukuda et al.14 (6) | 74.1 | 5.6 | 25 | 49.4 | 11.2 | 24 | 24.7 [19.7, 29.7] | |||
| Fukuda et al.14 (7) | 72.4 | 6.1 | 25 | 47.7 | 10.5 | 24 | 24.7 [19.9, 29.5] | |||
| Fukuda et al.14 (8) | 69.6 | 5.2 | 25 | 46.1 | 10.9 | 24 | 23.5 [18.7, 28.3] | |||
| AKPS | ||||||||||
| Ismail et al.13 | 85.1 | 6.2 | 16 | 85 | 6.7 | 16 | 0.1 [-4.4, 4.6] | |||
| Fukuda et al.18 (4) | 78.9 | 16 | 21 | 80.6 | 13.9 | 20 | -1.7 [-10.9, 7.5] | |||
| Fukuda et al.18 (5) | 78.9 | 16 | 21 | 64.5 | 11.1 | 23 | 14.4 [6.2, 22.6] | |||
| Fukuda et al.14 (6) | 85.7 | 9 | 25 | 64.6 | 10.2 | 24 | 21.1 [15.7, 26.5] | |||
| Fukuda et al.14 (7) | 81.7 | 7.6 | 25 | 62 | 9.3 | 24 | 19.7 [14.9, 24.5] | |||
| Fukuda et al.14 (8) | 79 | 7.7 | 25 | 60 | 8.3 | 24 | 19.0 [14.5, 23.5] | |||
| Step-down test | ||||||||||
| Dolak et al.16 (1) | 17 | 5 | 17 | 17 | 7 | 16 | 0 [-4.2, 4.2] | |||
| Dolak et al.16 (2) | 19 | 5 | 17 | 20 | 6 | 16 | -1.0 [-4.8, 2.8] | |||
| Unilateral jump | ||||||||||
| Fukuda et al.18 (4) | 91.8 | 34.4 | 21 | 86.5 | 32 | 20 | 5.3 [-15.0, 25.6] | |||
| Fukuda et al.18 (5) | 91.8 | 34.4 | 21 | 80.3 | 16 | 23 | 11.5 [-4.6, 27.6] | |||
| Fukuda et al.14 (6) | 85.7 | 10.2 | 25 | 69.9 | 21.8 | 24 | 15.8 [6.2, 25.4] | |||
| Fukuda et al.14 (7) | 84 | 10.9 | 25 | 67.3 | 21.5 | 24 | 16.7 [7.1, 26.3] | |||
| Fukuda et al.14 (8) | 82.3 | 10.2 | 25 | 65.6 | 21.2 | 24 | 16.7 [7.3, 26.1] | |||
| Favors Experimental | Favors Control | |||||||||
X = Mean; SD = Standard deviation; N = Sample size; 95% CI = 95% Confidence Interval; (1) = 4 weeks; (2) = 8 weeks; (3) = 12 weeks; (4) = Comparison EG x CGa; (5) = Comparison EG x CGb (6) = 3 months; (7) = 6 months; (8) = 12 months.
One of the selected studies compared the hip muscle strengthening intervention group (i.e., experimental) against a control group that used Omega-3 and calcium for eight weeks as a placebo15. Only the experimental group showed reduction in pain intensity and improvement in function and in hip lateral rotator and abductor strength15 (Tables 3, 4, and 5). Another study compared an intervention that included hip muscle strengthening against an intervention that included knee extensor strengthening16. After this intervention was applied for four weeks, functional exercises were added for another four weeks in both groups16. The groups were reassessed at the end of the full eight weeks of intervention and again after four more weeks without intervention16. The experimental group had less pain after four weeks than the control group16 (Table 3). The groups did not differ in relation to function in any of the assessment moments16 (Table 5). In addition, the experimental group showed greater muscular strength than the control group only in hip lateral rotators16 (Table 4) and this difference was found only after the 8th week (Table 4).
Four studies14 , 15 , 17 , 18 compared an intervention that included hip muscle strengthening (experimental group) against another intervention that included only knee muscle strengthening (control group). These four studies also assessed pain intensity in different contexts. Two studies17 , 19 assessed daily pain intensity and both identified greater improvement in the experimental group (Table 3). Three studies investigated pain intensity when ascending and descending stairs14 , 18 , 19. Two studies identified14 , 19 greater reduction in pain intensity when ascending stairs in the experimental group, while the other study18 did not identify differences between groups (Table 3). One study14 identified greater reduction in pain when descending stairs while the other two studies18 , 19 did not identify differences between groups (Table 3). One study19 also investigated pain intensity when squatting and sitting for long periods and found that the experimental group reported less pain intensity only during the squatting task (Table 3). In addition, this study19 found that the experimental group presented less intensity of the worst experienced pain compared to the control group (Table 3).
Two studies14 , 18 investigated function and one study19 investigated eccentric muscle strength by comparing an intervention that included hip muscle strengthening to an intervention that included only knee muscle strengthening. Fukuda et al.18 observed no differences between groups when they used three tests to assess function (unilateral jump test, Lower Extremity Functional Scale-LEFS, and Anterior Knee Pain Scale-AKPS) (Table 5). In another study, Fukuda et al.14 observed that the experimental group had greater functional capacity when compared to the control group, when they used these same three tests three, six, and twelve months after intervention (Table 5). The study that assessed eccentric knee extension strength19 did not identify differences between the groups (Table 4).
Fukuda et al.18 compared an intervention that included hip muscle strengthening against no intervention. This study showed that after four weeks of intervention, the experimental group presented a reduction in pain intensity when ascending and descending stairs, as well as improved function when compared to the control group18 (Tables 3 and 5). No difference was observed between the groups in the unilateral jump test18 (Table 5).
One study13 compared a group that was submitted to closed kinetic chain (CKC) exercises and hip muscle strengthening (experimental group) against a group that was submitted exclusively to CKC exercises (control group). There were no differences between the groups related to pain intensity, hip muscle strength, and function after the intervention (Tables 3, 4, and 5).
Discussion
This systematic review showed that the majority of selected studies indicate that hip muscle strengthening is effective for reducing pain and improving function in individuals with PFPS. However, the studies disagreed regarding the treatments' ability to improve muscle strength. The review of the literature showed only a few studies with RCT design that compared hip muscle strengthening with other treatments. The selected studies included a variety of intervention protocols and outcome assessments making it difficult to compare the results among studies and prevented statistical grouping of the results to perform meta-analysis.
The selected studies showed good internal validity according to the PEDro scale since they satisfied the majority of the items from 2 to 11. Items 5 and 6 were not satisfied by any study. One point is earned for these items if there was blinding of the subjects (Item 5) and therapists (Item 6). Both procedures are difficult to be performed by studies that looked for the effect of physical therapy interventions because of the nature of these interventions. Apart from these criteria, the study of Razeghi et al.17 did not score other items related to internal validity and thus, presented the lowest score. Furthermore, the majority of the studies were rated on the external validity criterion (Item 1). Only one study was not awarded a point for this item because it did not describe the source of the subjects19. Considering the overall score in the PEDro scale, this review selected studies that presented good internal and external validity.
Pain intensity was evaluated by all the studies selected for this review13 - 19. Some studies used different scales to evaluate this variable, while others, despite using the same scale, asked the participants to report the mean pain intensity in different contexts. For example, the worst pain experienced in the previous week19, pain when ascending and descending stairs14 , 18 , 19, and pain while squatting or sitting for prolonged periods19. Regardless of the method of evaluation, the majority of studies showed greater reduction in pain in the hip-strengthening group as compared to the control group. It is noteworthy that three studies14 , 18 , 19 showed pain reduction in the experimental group, in ascending and descending stairs, indicating the positive impact of this intervention on daily activities. Furthermore, one study14 showed that those participants who strengthened both the hip and knee muscles presented less pain in ascending and descending stairs one year after treatment was discontinued when compared to those participants who strengthened only the knee muscles. This may indicate the long-term benefits of associating both muscle groups in the intervention. However, the investigation of benefits after such a long period (i.e. one year) was performed by only one study. Future studies may consider investigating the long-term effects of muscle strengthening in patients with PFPS.
Dolak et al.16 also showed that patients who strengthened the hip muscles had less pain intensity four weeks after treatment, when compared to those who strengthened only the knee muscles. However, these authors16 indicated that, following the intervention with functional exercises, both groups showed reduction in pain when compared to their initial measurements. The functional exercises included unilateral squatting, which was shown to activate the hip muscles (gluteus medius and gluteus maximus)23 , 24. Thus, the improvement shown by the control group at the end of the second phase of this study may have been influenced by the addition of functional activities, which allowed the recruitment of hip muscles. This conjecture is supported by the absence of differences between groups observed by Ismail et al.13, whose study had both groups performing activities such as lateral step up, which also activates hip muscles21 , 25. In addition, other studies which included weight bearing activities (e.g. unilateral squatting) showed a reduction in pain intensity in the control group when comparing the results after intervention with baseline values13 , 14 , 17. Although the control group had a reduction in pain compared to baseline, the experimental group showed a greater reduction in pain compared to the control group in these studies14 , 17. Thus, some of the results showing pain reduction in the control group may be related to the performance of weight-bearing activities. Future studies aiming to compare hip muscle strengthening against other interventions should consider the demand on the hip muscles during the activities chosen for the control group.
The effects of hip muscle strengthening on hip muscle strength were equivocal13 , 15 , 16 , 19. One factor that may explain this result is the number of supervised sessions by the researcher. The study that offered supervision in all sessions showed increasing torque in both hip abductors and lateral rotators of participants from the experimental group15. On the other hand, the study that offered supervision in one out of three sessions per week showed the increasing torque only of hip lateral rotators of the participants from the experimental group16. In addition, this study presented a 95% confidence interval of the mean difference between groups with an inferior limit near zero (Table 4). Similarly, a study that offered one out of four supervised sessions per week did not show any muscle strength difference between groups19. Thus, one hypothesis for further research is that a greater number of supervised sessions might improve the quality of the performance of the activities thereby increasing muscle strength.
Another factor that may be considered during the analysis of the results of muscle strength is the specificity of the training26. The isometric strength test used by two studies15 , 16 did not reflect the type of muscle strengthening that was employed in the studies. Furthermore, since the majority of daily activities are dynamic, there has been discussion as to whether measures of isometric strength offer information specific to the activities of interest26. Therefore, the amount of supervised sessions and the specificity of muscle strength training may explain the differences between the studies.
These two factors to explain the equivocality of muscle strength results among the studies must be accepted with caution, however. In the research of Ismail et al.13, no differences in strength were observed between groups, even though all sessions were supervised and strength was evaluated in both concentric and eccentric tests. A confounding factor in that experiment may have been that both groups performed weight-bearing activities that might have improved muscle strength in both groups, making it difficult to identify differences between groups. The effects of hip muscle strengthening on hip muscle strength have been questioned by a previous consensus on PFPS27. This consensus stated that it was necessary to better understand whether the benefits of hip strengthening exercises are due to improvements in hip strength or to changes in neuromuscular activity27. Considering the equivocal results for muscle strengthening found by this review, future studies are still required to answer this issue.
Functional capabilities were evaluated using questionnaires and functional activities in five of the seven studies selected. Two studies14 , 18, which used the Lower Extremity Functional Scale (LEFS) and Anterior Knee Pain Scale (AKPS) questionnaires and the unilateral jump test, observed that the participants from the experimental group achieved greater improvement of function compared to the control group. Furthermore, one of these studies14 demonstrated that the functional capability in the experimental group was greater than in the control group at three, six, and 12 months after intervention, showing long-term improvement. Another study13 also used the AKPS and observed that the experimental group showed greater improvement in reported functional capability compared to the control group. Dolak et al.16 also used the LEFS, but observed that all participants, independently of group allocation, showed improvement in the reported functional capabilities after intervention. This result may be influenced by the functional exercises performed by all of the participants, as discussed previously. Ismail et al.13 evaluated function using the AKPS and did not find any differences between groups. The possible explanation for this result may be similar to that of the absence of differences in pain intensity and hip muscle strength. Khayambashi et al.15 used the Western Ontario and McMaster Universities Arthritis Index (WOMAC) to assess function and also observed improvement in the experimental group. Furthermore, the improvement in the experimental group lasted until six months after intervention15, reinforcing the long-term benefits of hip muscle strengthening on function. Thus, the majority of studies showed both short and long-term improvement in functional capabilities.
This systematic review had some limitations. As discussed above, the selected studies applied different methods to evaluate pain intensity, muscle strength, and function and described different protocols of hip muscle strengthening, which prevented statistically grouping the results to perform meta-analysis. Differences in treatment protocols, including program duration, number of sets, and repetitions of the performed exercises, and the procedure to determine the exercise intensity are examples of this lack of uniformity. The program lasted four weeks in three studies14 , 17 , 18, six weeks in two studies13 , 19, and eight weeks in two other studies15 , 16. The number of sets varied between two and three and the repetitions between 10 and 15. The procedure to determine the exercise intensity was also heterogeneous among the studies. For example, one study13 set the load as 60% of 1-repetition maximum, two studies14 , 18 set it as 70% of 1-repetition maximum, and one study16 set it as percentage of body mass. Apart from this heterogeneity, the studies showed some similarities. The majority of the programs aimed to strengthen hip abductors13 - 19 and hip lateral rotators13 - 19 in different positions, such as side lying, sitting, and standing. There was also a trend in the studies to increase the exercises' intensity progressively by increasing the load13 , 14 , 18, changing the elastic resistance15 , 16, and/or changing the exercises16 , 19. Furthermore, the majority of the studies provided training three times per week13 - 16 , 18. Despite differences among the studies that prevented statistically grouping the results, the similarities among the selected studies may have contributed to the positive findings of this review. It suggests that they should be considered important variables in the analysis of the effectiveness of hip muscle strengthening.
This review aimed to look at the effectiveness of hip muscle strengthening on pain intensity, muscle strength, and function in individuals with PFPS. Other studies, however, have investigated the effects of other types of interventions in patients with PFPS (e.g. quadriceps strengthening and foot orthoses) and the combination of interventions or have made comparisons between these interventions28 - 30. The approach chosen by the current review allowed the selection of studies that specifically investigated the effectiveness of hip muscle strengthening and a more detailed discussion on the role of hip muscle strength on reducing pain and increasing function of PFPS patients. The choice of this approach was motivated by two factors: 1) the theoretical claim that modifying tissue properties around the hip will improve patellar tracking; and 2) current and common clinical practice that focuses on hip muscle force and function in alleviating knee pain. Therefore, the results of this systematic review provide an updated source of evidence for clinicians and researchers.
This review summarized the literature and evaluated the methodological quality of the RCT already published regarding the effects of hip muscle strengthening in patients with PFPS. The results showed that hip muscle strengthening has an important role in the treatment of PFPS patients, since this intervention is effective in reducing pain intensity and improving function. However, findings regarding the treatments' ability to improve muscle strength were equivocal. The synthesis of data presented here could help researchers to plan future studies. In addition, the results of this review could help in clinical decision making since they support the inclusion of hip muscle strengthening in the treatment of patients with PFPS. The results presented here can also be used by clinicians to explain the treatment's goals to the patients and thus, to increase their adherence to the treatment.
References
- 1.Powers CM, Heino JG, Rao S, Perry J. The influence of patellofemoral pain on lower limb loading during gait. Clin Biomech (Bristol, Avon) 1999;14(10):722–728. doi: 10.1016/s0268-0033(99)00019-4. http://dx.doi.org/10.1016/S0268-0033(99)00019-4 [DOI] [PubMed] [Google Scholar]
- 2.César CM, Alves FC, Gonçalves LTN, Ocarino J, Lanna P. Avaliação da progressão no desempenho e capacidade funcional em indivíduos em reabilitação devido à síndrome patelofemoral. Fisioter Bras. 2007;8(1):21–24. [Google Scholar]
- 3.Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther. 2003;33(11):639–646. doi: 10.2519/jospt.2003.33.11.639. http://dx.doi.org/10.2519/jospt.2003.33.11.639 [DOI] [PubMed] [Google Scholar]
- 4.Davis IS, Powers C. Patellofemoral pain syndrome: proximal, distal, and local factors, an international retreat, April 30-May 2, 2009, Fells Point, Baltimore, MD. J Orthop Sports Phys Ther. 2010;40(3):A1–16. doi: 10.2519/jospt.2010.0302. http://dx.doi.org/10.2519/jospt.2010.0302 [DOI] [PubMed] [Google Scholar]
- 5.Harvie D, O'Leary T, Kumar S. A systematic review of randomized controlled trials on exercise parameters in the treatment of patellofemoral pain: what works? J Multidiscip Healthc. 2011;4:383–392. doi: 10.2147/JMDH.S24595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garcia FR, Azevedo FM, Alves N, Carvalho AC, Padovani CR, Negrao RF., Filho Effects of electrical stimulation of vastus medialis obliquus muscle in patients with patellofemoral pain syndrome: an electromyographic analysis. Rev Bras Fisioter. 2010;14(6):477–482. http://dx.doi.org/10.1590/S1413-35552010000600005 [PubMed] [Google Scholar]
- 7.Ireland ML, Willson JD, Ballantyne BT, Davis IM. Hip strength in females with and without patellofemoral pain. J Orthop Sports Phys Ther. 2003;33(11):671–676. doi: 10.2519/jospt.2003.33.11.671. http://dx.doi.org/10.2519/jospt.2003.33.11.671 [DOI] [PubMed] [Google Scholar]
- 8.Robinson RL, Nee RJ. Analysis of hip strength in females seeking physical therapy treatment for unilateral patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2007;37(5):232–238. doi: 10.2519/jospt.2007.2439. http://dx.doi.org/10.2519/jospt.2007.2439 [DOI] [PubMed] [Google Scholar]
- 9.Cichanowski HR, Schmitt JS, Johnson RJ, Niemuth PE. Hip strength in collegiate female athletes with patellofemoral pain. Med Sci Sports Exerc. 2007;39(8):1227–1232. doi: 10.1249/mss.0b013e3180601109. http://dx.doi.org/10.1249/mss.0b013e3180601109 [DOI] [PubMed] [Google Scholar]
- 10.Bolgla LA, Malone TR, Umberger BR, Uhl TL. Hip strength and hip and knee kinematics during stair descent in females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2008;38(1):12–18. doi: 10.2519/jospt.2008.2462. http://dx.doi.org/10.2519/jospt.2008.2462 [DOI] [PubMed] [Google Scholar]
- 11.Barton CJ, Lack S, Malliaras P, Morrissey D. Gluteal muscle activity and patellofemoral pain syndrome: a systematic review. Br J Sports Med. 2013;47(4):207–214. doi: 10.1136/bjsports-2012-090953. http://dx.doi.org/10.1136/bjsports-2012-090953 [DOI] [PubMed] [Google Scholar]
- 12.Mascal CL, Landel R, Powers C. Management of patellofemoral pain targeting hip, pelvis, and trunk muscle function: 2 case reports. J Orthop Sports Phys Ther. 2003;33(11):647–660. doi: 10.2519/jospt.2003.33.11.647. http://dx.doi.org/10.2519/jospt.2003.33.11.647 [DOI] [PubMed] [Google Scholar]
- 13.Ismail MM, Gamaleldein MH, Hassa KA. Closed kinetic chain exercises with or without additional hip strengthening exercises in management of patellofemoral pain syndrome: a randomized controlled trial. Eur J Phys Rehabil Med. 2013;49(5):687–698. [PubMed] [Google Scholar]
- 14.Fukuda TY, Melo WP, Zaffalon BM, Rossetto FM, Magalhães E, Bryk FF. Hip posterolateral musculature strengthening in sedentary women with patellofemoral pain syndrome: a randomized controlled clinical trial with 1-year follow-up. J Orthop Sports Phys Ther. 2012;42(10):823–830. doi: 10.2519/jospt.2012.4184. http://dx.doi.org/10.2519/jospt.2012.4184 [DOI] [PubMed] [Google Scholar]
- 15.Khayambashi K, Mohammadkhani Z, Ghaznavi K, Lyle MA, Powers CM. The effects of isolated hip abductor and external rotator muscle strengthening on pain, health status, and hip strength in females with patellofemoral pain: a randomized controlled trial. J Orthop Sports Phys Ther. 2012;42(1):22–29. doi: 10.2519/jospt.2012.3704. http://dx.doi.org/10.2519/jospt.2012.3704 [DOI] [PubMed] [Google Scholar]
- 16.Dolak KL, Silkman C, McKeon JM, Hosey RG, Lattermann C, Uhl TL. Hip strengthening prior to functional exercises reduces pain sooner than quadriceps strengthening in females with patellofemoral pain syndrome: a randomized clinical trial. J Orthop Sports Phys Ther. 2011;41(8):560–570. doi: 10.2519/jospt.2011.3499. http://dx.doi.org/10.2519/jospt.2011.3499 [DOI] [PubMed] [Google Scholar]
- 17.Razeghi M, Etemadi Y, Sh T, Ghaem H. Could hip and knee muscle strengthening alter the pain intensity in patellofemoral pain syndrome? Iranian Red Crescent Medical Journal. 2010;12(2):104–110. [Google Scholar]
- 18.Fukuda TY, Rossetto FM, Magalhães E, Bryk FF, Lucareli PRG, Carvalho NAA. Short-term effects of hip abductors and lateral rotators strengthening in females with patellofemoral pain syndrome: a randomized controlled clinical trial. J Orthop Sports Phys Ther. 2010;40(11):736–742. doi: 10.2519/jospt.2010.3246. http://dx.doi.org/10.2519/jospt.2010.3246 [DOI] [PubMed] [Google Scholar]
- 19.Nakagawa TH, Muniz TB, Baldon RM, Dias Maciel C, Menezes Reiff RB, Serrão FV. The effect of additional strengthening of hip abductor and lateral rotator muscles in patellofemoral pain syndrome: a randomized controlled pilot study. Clin Rehabil. 2008;22(12):1051–1060. doi: 10.1177/0269215508095357. http://dx.doi.org/10.1177/0269215508095357 [DOI] [PubMed] [Google Scholar]
- 20.Kunz R, Oxman AD. The unpredictability paradox: review of empirical comparisons of randomised and non-randomised clinical trials. BMJ. 1998;317(7167):1185–1190. doi: 10.1136/bmj.317.7167.1185. http://dx.doi.org/10.1136/bmj.317.7167.1185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mulrow CD. Rationale for systematic reviews. BMJ. 1994;309(6954):597–599. doi: 10.1136/bmj.309.6954.597. http://dx.doi.org/10.1136/bmj.309.6954.597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shiwa SR, Costa LOP, Moser ADL, Aguiar IC, Oliveira LVF. PEDro: a base de dados de evidências em fisioterapia. Fisioter Mov. 2011;24(3):523–533. http://dx.doi.org/10.1590/S0103-51502011000300017 [Google Scholar]
- 23.Boren K, Conrey C, Le Coguic J, Paprocki L, Voight M, Robinson TK. Electromyographic analysis of gluteus medius and gluteus maximus during rehabilitation exercises. Int J Sports Phys Ther. 2011;6(3):206–223. [PMC free article] [PubMed] [Google Scholar]
- 24.Felicio LR, Dias LA, Silva AP, Oliveira AS, Bevilaqua-Grossi D. Muscular activity of patella and hip stabilizers of healthy subjects during squat exercises. Rev Bras Fisioter. 2011;15(3):206–211. [PubMed] [Google Scholar]
- 25.Souza RB, Draper CE, Fredericson M, Powers CM. Femur rotation and patellofemoral joint kinematics: a weight-bearing magnetic resonance imaging analysis. J Orthop Sports Phys Ther. 2010;40(5):277–285. doi: 10.2519/jospt.2010.3215. http://dx.doi.org/10.2519/jospt.2010.3215 [DOI] [PubMed] [Google Scholar]
- 26.Enoka RM. Neural adaptations with chronic physical activity. J Biomech. 1997;30(5):447–455. doi: 10.1016/s0021-9290(96)00170-4. http://dx.doi.org/10.1016/S0021-9290(96)00170-4 [DOI] [PubMed] [Google Scholar]
- 27.Powers CM, Bolgla LA, Callaghan MJ, Collins N, Sheehan FT. Patellofemoral pain: proximal, distal, and local factors, 2nd International Research Retreat. J Orthop Sports Phys Ther. 2012;42(6):A1–54. doi: 10.2519/jospt.2012.0301. http://dx.doi.org/10.2519/jospt.2012.0301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barton CJ, Munteanu SE, Menz HB, Crossley KM. The efficacy of foot orthoses in the treatment of individuals with patellofemoral pain syndrome: a systematic review. Sports Med. 2010;40(5):377–395. doi: 10.2165/11530780-000000000-00000. http://dx.doi.org/10.2165/11530780-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 29.Bolgla LA, Boling MC. An update for the conservative management of patellofemoral pain syndrome: a systematic review of the literature from 2000 to 2010. Int J Sports Phys Ther. 2011;6(2):112–125. [PMC free article] [PubMed] [Google Scholar]
- 30.Peters JS, Tyson NL. Proximal exercises are effective in treating patellofemoral pain syndrome: a systematic review. Int J Sports Phys Ther. 2013;8(5):689–700. [PMC free article] [PubMed] [Google Scholar]