Abstract
A sizable proportion of psychiatric patients will seek clinical evaluation and treatment for anxiety symptoms reportedly refractory to treatment. This apparent lack of response is either due to “pseudo-resistance” (a failure to have received and adhered to a recognized and effective treatment or treatments for their condition) or to true “treatment resistance.” Pseudo-resistance can be due to clinician errors in selecting and delivering an appropriate treatment effectively, or to patient nonadherence to a course of treatment. True treatment resistance can be due to unrecognized exogenous anxiogenic factors (eg, caffeine overuse, sleep deprivation, use of alcohol or marijuana) or an incorrect diagnosis (eg, atypical bipolar illness, occult substance abuse, attention deficit-hyperactivity disorder). Once the above factors are eliminated, treatment should focus on combining effective medications and cognitive behavioral therapy, combining several medications (augmentation), or employing novel medications or psychotherapies not typically indicated as first-line evidence-based anxiety treatments.
Keywords: anxiety, refractory, pseudo-resistance, CBT, antidepressant, benzodiazepine
Abstract
Una proporción considerable de pacientes psiquiátricos buscará evaluación clínica y tratamiento para síntomas ansiosos que se consideran refractarios al tratamiento. Esta aparente falta de respuesta puede deberse a una “pseudo-resistencia” (un fracaso al haber recibido y adherido a un tratamiento efectivo y reconocido o a tratamientos para su condición) o a una verdadera “resistencia terapéutica”. La pseudo-resistencia puede deberse a errores clínicos en la selección y administración de un tratamiento efectivamente apropiado, o a la falta de adherencia del paciente durante un período de tratamiento. La verdadera resistencia terapéutica puede deberse a factores ansiogénicos exógenos no reconocidos (como exceso de cafeína, privación de sueño, uso de alcohol o marihuana) o a diagnósticos incorrectos (como enfermedad bipolar atípica, abuso oculto de sustancias, trastorno por déficit atencional con hiperactividad). Cuando se han descartado los factores anteriores, el tratamiento debe enfocarse en la combinación de medicamentos efectivos y terapia cognitivo conductual, combinación de varios fármacos (aumentación) o el empleo de nuevos medicamentos o psicoterapias para la ansiedad que no se indican habitualmente como tratamientos de primera línea basados en la evidencia.
Abstract
Une proportion importante de patients psychiatriques sollicite un traitement et une évaluation clinique pour des symptômes anxieux qui seraient réfractaires au traitement. Ce manque de réponse apparent est dû soit à une « pseudo-résistance » (l'absence de prescription ou d'observance d'un traitement reconnu et efficace ou à un traitement adapté à leur pathologie) soit à une véritable « résistance au traitement ». La pseudo-résistance peut être due à une erreur du médecin dans le choix et la délivrance d'un traitement approprié efficace, ou à la non-observance du patient au traitement. Une véritable résistance au traitement peut être due à des facteurs anxiogènes exogènes non reconnus (par exemple surconsommation de caféine, privation de sommeil, consommation d'alcool ou de marijuana) ou à un mauvais diagnostic (par exemple maladie bipolaire atypique, toxicomanie cachée, trouble déficit de l'attention avec hyperactivité). Une fois ces facteurs éliminés, le traitement doit se focaliser sur l'association de médicaments efficaces et de thérapie cognitive comportementale, sur l'association de plusieurs médicaments (potentialisation), ou à l'aide de nouveaux traitements ou psychothérapies non indiqués formellement en première ligne pour l'anxiété.
Introduction
Anxiety can be viewed through multiple lenses. It is a distressing subjective experience, a symptom that can be reported to a health care professional, the hallmark of a group of diagnosable disorders (the DSM-5 Anxiety Disorders), and most recently a “qualifier” that can be added to the diagnosis of Major Depressive Disorder (MDD) in DSM-5, and may have important prognostic implications. It also can be a key symptom in other major psychiatric disorders such as autism spectrum disorders, bipolar disorder (not just as part of major depression but also as an important component of “mixed” states) and substance use disorders (as seen with states of intoxication and withdrawal).
Anxiety is also one of the most vexing and difficult problems encountered by the practicing psychiatrist. Unlike many patients with depression who may be passive and willing participants in the clinical encounter, anxious patients may dramatically and urgently demand immediate relief from their distress. This places the clinician in a difficult position, narrowing the time window available for more extended expert evaluation, and requiring a high level of psychotherapeutic expertise to manage this distress in the short run. This often results in prescription of a fast-acting anxiolytic agent, usually a benzodiazepine, a practice that may be both immediately effective but fraught with longer-term difficulties. Because there are so many “faces” of anxiety, and the field has no access to objective tests to aid in the differential diagnosis, the process of successfully evaluating and treating anxiety can take some time and must ideally unfold in an iterative manner.
This article will focus on a particularly difficult issue, the problem of apparent “treatment-refractory anxiety.” It will review the extant diagnostic and treatment database informing the initial evaluation and standard treatment of anxiety, the factors that may contribute to lack of response to standard treatments, and clinical approaches that may result in more optimal outcomes in these patients.
Background
Anxiety may be the most prevalent psychiatric symptom in the general population. The group of anxiety disorders has a combined lifetime prevalence of 28%,1 far more than that of the depressive disorders, and, when considered as comorbid as well as primary diagnoses, comprise over three quarters of all psychiatric disorders surveyed in recent epidemiological studies. This does not include conditions where anxiety is an important symptom but may not rise in severity to sufficient levels to constitute a diagnosable anxiety disorder (eg, bipolar disorder, substance use disorders, attention deficithyperactivity disorder [ADHD]). As will be seen, these other disorders may sometimes constitute the major issue and account for “treatment-refractory” anxiety. Consistent with this data, a large proportion of patients presenting for psychiatric treatment have some level of “anxiety” even if they do not describe it or experience it as such (eg, it might be perceived as internal agitation or restlessness without subjective worry or acknowledgement of “nervousness” or “anxiety”). Moreover, it is now both clinical lore and growing scientific fact that anxiety seems to predict a poorer course and treatment response when it accompanies other disorders (discussed later in this article).
It is best to begin by examining the large group of anxiety disorders. Although DSM-5 has now removed both obsessive-compulsive disorder OCD) and posttraumatic stress disorder (PTSD) from the group of anxiety disorders, symptoms of anxiety significantly contribute to both these conditions, and so they are included in this discussion. The original five anxiety disorders are well known: Panic Disorder, Generalized Anxiety Disorder (GAD), Social Anxiety Disorder, OCD, and PTSD. While specific phobias are common in the general population, they rarely prompt patients to seek clinical care. Most clinical trials of these disorders document response rates of 50% to 60% and remission rates between 25% and 35%. However, refractory anxiety must also include patients who relapse after remission, and this rate is f 0% at 1 year, 20% at 5 years, and 30% at 100 years.2 Thus the prevalence of treatment-refractory anxiety can be sizable.
Neuroscience research has rapidly expanded our knowledge of the neurocircuitry of anxiety, and these neural underpinnings have been increasingly well-characterized in the past few years.3 In contrast, advances in understanding the genetic underpinnings of anxiety, like depression, have lagged behind recent findings in schizophrenia, bipolar illness, and autism, though discoveries have been made, and some have been linked to key neural circuits. Nonetheless, our growing knowledge of the neuroscientific basis of anxiety has had little if any impact in changing or even modifying clinical practice.
Effective treatments for the anxiety disorders
The basic definition of treatment-refractory anxiety requires that standard anxiety disorder treatments have been successfully delivered and found to be either totally ineffective (no response) or only modestly effective (response but no remission). Hence we need to understand these basic treatments as well as what factors might prevent them from being successfully delivered to anxious patients.
The first-line pharmacologic treatment for all five anxiety disorders is a selective serotonin uptake inhibitor (SSRI), with serotonin-norepinephrine uptake inhibitors (SNRIs) also playing a prominent role.4 Though efficacy may vary by anxiety disorder, these agents are broadly effective across multiple aspects of these disorders, ie, cognitive symptoms, phobic/avoid ant symptoms, and physiologic/autonomic symptoms. They also effectively treat the comorbid depression which commonly accompanies these disorders. Highpotency benzodiazepines (eg, clonazepam, lorazepam, alprazolam) are effective agents for panic, generalized, and social anxiety disorders, but have no proven efficacy in either OCD or PTSD.4 More importantly, they have no efficacy for comorbid depression. They are no longer first-line agents because their advantages (rapid onset of action, high tolerability with limited adverse effects, limited interaction with other medications) are offset by their narrow spectrum of action (no benefit for co-occurring depression, possibly less efficacy against cognitive/ruminative symptoms of anxiety), and the risk of abuse, cognitive side effects, and withdrawal effects with attempted discontinuation. The latter risk is most problematic and confusing for clinicians, since these withdrawal symptoms often mimic the original anxiety syndrome for which these medications were prescribed5 and make it hard to determine whether this distress represents loss of therapeutic effect or time-limited physiological withdrawal. Consistent with the concept of return of anxiety on discontinuation, withdrawal symptoms may be worse in patients with panic disorder versus those with GAD.6 Despite these caveats, these agents have definite value as adjunctive agents in anxious patients not optimally responsive to SSRI treatment and, as such, may constitute the most widely used and well-accepted initial medication approach to refractory anxiety, despite a dearth of studies in this area. An additional use of benzodiazepines has been aimed at rapidly reducing anxiety early in the course of SSRI treatment, allowing patients to “hang in there” until the SSRI begins to work. While some clinicians continue to use this strategy, the best study showed that neither outcome of nor adherence to this strategy were superior to that seen with SSRI treatment alone.7 Furthermore, clinicians often report that patients sometimes discontinue the SSRI when given a rapidly effective benzodiazepine along with it, telling their clinician “this is the medication that is really working, I don't want to take the other medication.” Finally, it is just as likely that supportive psychotherapy with regular visits or phone contacts will help patients through the delayed onset of SSRI anxiolytic effects.
The first-line psychotherapeutic treatment for all five anxiety disorders is cognitive-behavioral (CBT) or behavioral (prolonged exposure for PTSD, exposure with response prevention for OCD) treatment.8 While CBT treatments for each disorder have been separately developed and codified in patient manuals, more recent work has suggested that there are common elements that broadly define these treatments and that they may be delivered in a more “unified” fashion.9 This school of thought suggests that the “anxious process” underlying the different disorders is highly similar and that the only major difference between the patient treatments is in the cue that provokes the anxiety. Thus, all anxiety CBT treatments focus on addressing the physiological, cognitive, and behavioral (avoidant) components of these disorders by a combination of skills designed to calm and diminish hyperarousal (eg, diaphragmatic breathing, progressive muscle relaxation), training and exercises designed to correct cognitive distortions (eg, challenging over estimation of risk of anxiety and de-catastophizing expectations of what it will be like if there are some anxiety symptoms) and use of progressive exposure methods to decrease avoidance of what the anxious patient most fears (eg, internal sensations for panic, social criticism for social anxiety disorder, contamination for OCD, traumatic memories for PTSD). These components are preceded by a careful explanation of the CBT model of anxiety, and this educational step is reinforced by having people track their symptoms, thoughts, and behaviors with a daily quantitative diary.
Both medication and CBT treatments have been shown to be comparably effective for Panic Disorder, GAD, and seasonal affective disorder (SAD).10-12 In OCD, exposure with prevention of the ritualizing response is superior to medication, which is superior to placebo.13 There are no comparative studies in PTSD. Selection of treatment modality is often determined by a combination of patient preference and CBT therapist availability. Medication is more widely employed because it is much more easily delivered, and delivery does not necessarily require a specialist and can be done in primary care. This fact is a reflection of the important therapeutic concept of “robustness,” which suggests that the more a treatment is unaffected by variability in practitioner skill and knowledge, the more easily and safely and effectively it can be delivered.14 Thus, while some initial research has suggested that CBT might provide longer-lasting benefits,15 and also has the obvious advantage that it does not have to be continued for the longer term, in contrast to medications (which may, in a significant proportion of cases, have to be taken chronically), delivering CBT with high fidelity is much more difficult than prescribing medication effectively.
Because many more anxious patients are seen and treated in primary care, it is important to note what the “usual primary care” approach to treating anxiety is. Use of benzodiazepines as first-line agents is less common than it was decades ago, though use is still considerable. However, in a recent large survey of anxious patients receiving treatment in primary care,16 SSRIs were prescribed twice as often as benzodiazepines. Unfortunately, the SSRI doses were frequently too low, because clinicians appropriately started with low doses, but then failed to titrate upward. In this same survey, relatively few anxious patients received any kind of CBT (less than 25%). Given these considerations, it would seem most appropriate to refer anxious patients who have failed an initial primary care trial of an evidencedbased medication treatment for consultation with a psychiatrist.
Approach to the evaluation of treatment-refractory anxiety
The basic approach follows a similar logic to that utilized in the approach for treatment refractory depression.17 There are two broad causes of treatment resistance: “pseudo-resistance” and true treatment resistance. Patients with “pseudo-resistance” have not actually received sufficient treatment, either because the type of treatment was wrong (ie, ineffective for the anxiety diagnosis), the “dose” (for medication) or the way the treatment was delivered (for psychotherapy) was insufficient, or the patient was nonadherent (failing to take medication or perhaps failing to engage sufficiently in the psychological treatment, eg, not doing CBT homework). Once it has been documented that adequate treatment was delivered and received, factors known to contribute to treatment resistance must be considered. These include re-evaluating what the primary diagnosis is (is the patient really an atypical bipolar 2 patient with prominent anxiety? Does the patient have an unrecognized substance use disorder? Is the disorder ADHD rather than GAD?), determining if there is a complicating medical condition that is either primary or contributing, and identifying factors that may facilitate anxiety and worsen the course of illness (eg, overuse of caffeine, sleep deprivation, interpersonal or familial conflicts). These factors are reviewed below and are followed by a discussion of therapeutic options for treatment-refractory anxiety.
Ineffective delivery of effective treatment and “pseudo-resistance ”
A number of studies have repeatedly documented a very low use of evidence-based anxiety treatments in both primary care and even specialty settings, though rates are much lower in primary care.18-20 The range of ineffective medications sometimes used in anxiety include the following: bupropion (no efficacy for any anxiety disorder); β-blockers (no efficacy except in performance anxiety); buspirone and trazodone (only effective for GAD); and tricyclic antidepressants (not effective in SAD): see ref 4 for review. However, failure to prescribe a sufficient dose and, even more often, to wait an adequate duration before giving up, is much more commonly a cause of pharmacotherapy delivery failure at the clinician end. Inspection of clinical trial response curves over time clearly show that, for some patients, response may not occur until 8 to 12 weeks (Figure 1) and, further, that response in the second 6 months may grow even more.21-23 Waiting for an adequate time to respond creates great difficulty for the treating clinician who may feel a need to prescribe anew or change a regimen at each visit to respond to a patient's distress over continued anxiety symptoms.
Figure 1. Paroxetine treatment of social anxiety disorder.
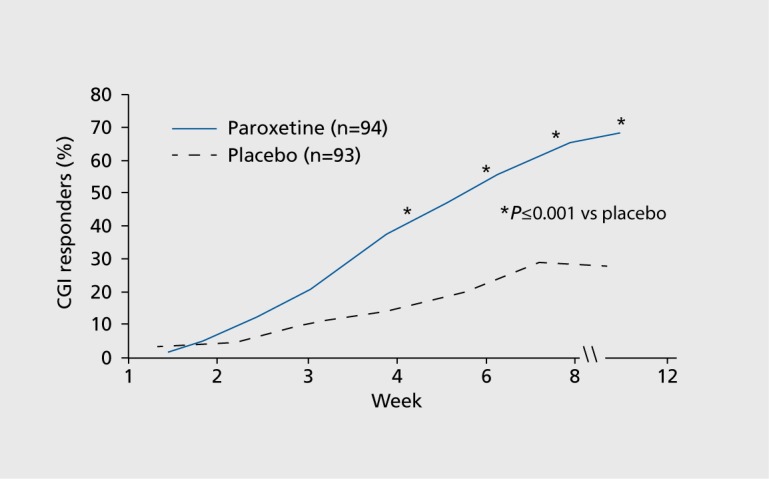
Adapted from ref 115: Stein MB, Liebowitz MR, Lydiard RB, Pitts CD, Bushnell W, Gergel I. Paroxetine treatment of generalized social phobia (social anxiety disorder): a randomized controlled trial. JAMA. 1998;280(8):708-713.
However, the biggest contributor to pseudo-resistance in pharmacotherapy is poor patient adherence. Lack of adherence is often explained as being due to medication intolerance. According to a study comparing worsening of symptoms in depressed versus anxious patients during a 1-week placebo-run in, medication intolerance in anxious patients may be a nocebo effect rather than excess sensitivity to physiologic effects of the drugs (Figure 2).24 Even if a true physiologic sensitivity exists, it may operate in part via a cognitive amplification process, whereby normal bodily sensations related to medication are thought to have catastrophic medical implications. Consistent with this concept, studies show that antidepressant medication intolerance can be lessened by CBT approaches,25 which have also been found effective for individuals undergoing tapered withdrawal from benzodiazepines.26 Sometimes, marked overstimulation and agitation as an immediate response to an antidepressant trial may not indicate increased sensitivity to medication but rather an antidepressant-induced switch to a bipolar illness “mixed state” in an undiagnosed patient27 (see more extensive discussion of this issue later). Even if a patient does not immediately terminate a medication trial, the avoidance of distress that is a common behavior in most anxiety disorders often contributes to delays in achieving adequate dose or in taking medication long enough to achieve a response. Because the required duration of treatment for pharmacological efficacy may be longer for anxiety than depressive disorders, psychotherapeutic skill is often required to gain a patient's trust and help him or her overcome their anxiety about taking medication. Sometimes, this anxiety can stem from more than just excess physiological or cognitive sensitivity eg, adverse medication experiences of family or close friends. This is consistent with studies documenting better adherence in depression with concomitant medication counseling.28
Figure 2.
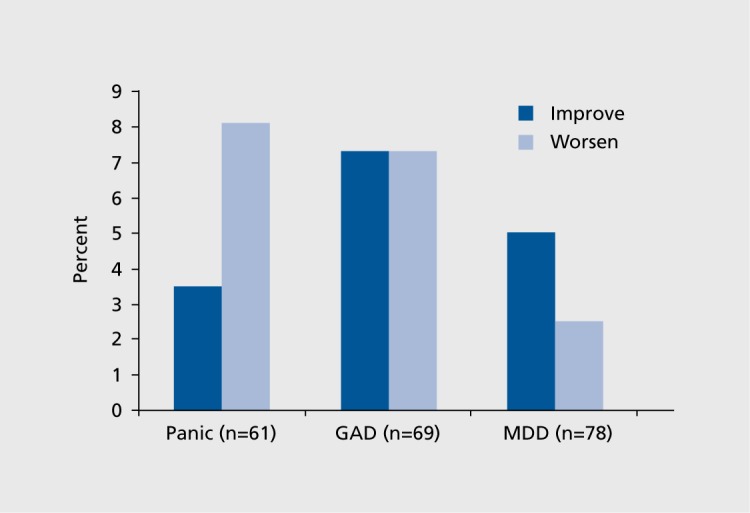
Treatment intolerance: high rate of negative placebo response in panic disorder.24 GAD, generalized anxiety disorder; MDD, major depressive disorder
Specific attitudes, experiences, conflicts, beliefs, and preferences for and about anxiety or its treatment may contribute to nonadherence. “Normalizing” attitudes, which interpret symptoms as a normal and expected consequence of stress (panic and GAD), personality (SAD), and trauma (PTSD), may account for findings that anxious patients are much less likely to perceive a need for treatment than depressed patients29 and hence likely to nonadhere. Patients may have had previous direct or vicarious experience with nonpsychotropic medication ineffectiveness (eg, family member with cancer), have psychological struggles with dependency that create a fear of becoming “addicted” to the medication, or have difficulty believing that the treatment modality offered will be effective.30 Many studies have suggested that both anxious and depressed patients prefer psychotherapy to medication,31,32 and evidence suggests that patients who receive a treatment modality they have less preference for, will be less likely to adhere to it.33 Late (after many months) nonadherence is usually due to both recovery from the anxiety syndrome and an acute illness model that treats anxiety more like a urinary tract infection than a chronic medical illness such as diabetes. This is one of the easier adherence problems to address because education often will convince a relapsing patient they need to adhere more effectively.
While both clinician and patient factors contribute to CBT failures, and patient failure to do “homework” and adequately buy into the CBT program is one commonly important factor, the biggest contributor to pseudo-resistance for CBT involves therapist rather than patient failures. While CBT is well known and taught in some psychology graduate programs, many more provide inadequate training, and many programs training other disciplines as therapists (eg, social worker, marriage and family counselor) emphasize other approaches and provide little CBT exposure.34 At the same time, CBT principles are not complex, so many therapists may purport to “do CBT” when all they really do is provide some basic education and provide some basic anxiety management skills such as breathing retraining and relaxation. In contrast, many studies have documented that the failure to progress to the exposure part of the CBT treatment protocol (the last and final phase after initial education, symptom management, and cognitive work) may significantly limit symptom improvement.35 Unfortunately, sometimes patients experience significant symptom resolution without progressing to exposure, reinforcing to the therapist that this truncated approach may be adequate. However, the avoidant nature of anxiety is such that patients may overendorse the extent of their improvement, ie, they are no longer anxious in a more circumscribed set of contexts but continue to avoid important events or experiences, eg, they may not drive long distances if they have panic, they may not date after being sexually assaulted. Finally, some therapists, usually those with much less exposure experience, may actively avoid the exposure phase out of concern that the initial distress required for extinction and desensitization will worsen the patients* symptoms. This directly colludes with patients' avoidance. In sum, a number of studies clearly show that exposure is the most important component of CBT and also the one most neglected by even CBT-oriented therapists. In contrast, I have seen a number of situations where experts hammer away at exposure having neglected important, more complex, cognitive elements that go beyond the simple risk overestimation and catastrophization that are the most common cognitive foci of CBT, eg, struggles with the stigmatizing effects of having an anxiety disorder.
Contributing factors to true treatment resistance
Once it has been established that an effective treatment has been adequately delivered and adhered to, there will remain a proportion of patients who have not remitted and a smaller proportion that remain quite symptomatic. Because there has been no equivalent of the STAR-D study for anxiety disorders, we do not have good data on the proportions of anxious patients who fail to remit or respond after adhering to adequately delivered treatment. However, the rates are likely to be similar to those seen in this landmark study of depression, ie, only 30% remit with initial treatment, and even after multiple treatments the remission rate is at best 60%. The clinician at this point needs to consider whether there are exogenous factors that are aggravating and/or maintaining anxiety, whether there may be a medical condition that is playing an important role, and last but not least, whether the diagnosis may be either wrong or incomplete, ie, whether there is another comorbidity present that is accounting for the poor response.
Exogenous factors
There are a number of anxiogenic factors that can contribute to anxiety. While many of these are quite obvious and may be routinely assessed by the clinician, patients may not always acknowledge them, or may minimize their severity and import. In the course of a complex intake done with limited available time, these factors are often glossed over quickly in order to cover more important diagnostic, course of illness and treatment response areas, and may come to the fore much later in the course of treatment.
Excess caffeine intake is rarely a “cause” of anxiety but is a frequent aggravator/amplifier.36 Patients will often have accompanying fatigue (perhaps as part of a comorbid depression), which is a driver of caffeine use, and if they do not experience symptom aggravation coincident with the timing of intake, they will minimize this. It is important to note that dependence on caffeine not only produces anxiety as a caffeine effect, but mayproduce this as a withdrawal effect, greatly confusing the picture.37 Moreover, patients often are not aware of the caffeine content of some beverages, eg, the patient who was drinking several cans of Mello Yello daily, believing it was a relaxant and was unaware of the amount of caffeine he was ingesting.
Over-the-counter cold preparations contain phenylpropylamine and pseudoephedrine, obvious stimulants. Yet patients with unexplained dyspnea may believe they have allergies and take these medications frequently in order to treat their anxiety symptom, further exacerbating their dyspnea and anxiety symptoms. The use of energy drinks with combinations of both caffeine and stimulants is another important example.
One night's total sleep deprivation has been shown to exacerbate panic,38 and relative sleep deprivation almost certainly plays an important role in aggravating anxiety. Relative deprivation of sleep likely plays an important role in the onset of first panic attack in college students, who may be stressed by exams, perhaps taking caffeine to stay up and study, and then losing substantial amounts of sleep.
While it is trite and tired to cite the importance of environmental stressors, it is less well appreciated that multiple studies examining anxiety outcomes have shown that life events, poor social support (Figure 3), and financial adversity are associated with inadequate or incomplete treatment response.39-41 I often will keep several figures showing these relationships on my desk and then show them to patients who are asking for an exclusively pharmacologic approach, to push for some way of either solving the specific life issues (using problem-solving therapy) or improving coping targeted toward these stressors.
Figure 3.
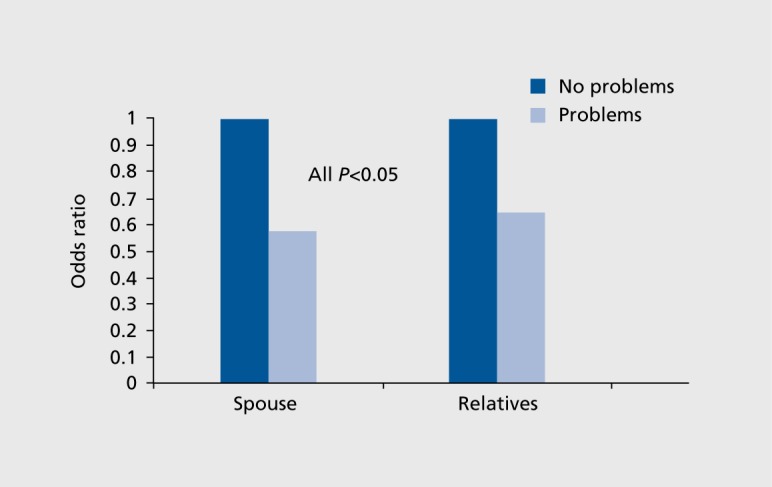
Disturbed spouse and family relationships predict lack of remission in generalized anxiety disorder.40
“Social” drinking (we will discuss alcohol abuse later) is known to aggravate panic and likely other anxiety syndromes, as the short-acting effects of alcohol wear off rapidly and there is a rapid rebound to a state of hyperexcitability that may be more problematic for anxious patients. Because this can happen to some patients after only one or two drinks, they often do not even consider that it can be an important factor. Explanation of the simple physiology of this (rebound excitation after profound neuronal inhibition) will often convince them that alcohol may be sensitizing the neural circuits subserving their anxiety and that a trial period of abstinence is indicated.
With the progressive availability of marijuana by both medicalization and now legalization in several states, clinicians need to be aware that this substance is also known to be associated with anxiety in some patients, though the exact causal relationship is unclear,42 and the extant research in this area is still quite limited because of previous restrictions. At the same time, marijuana is often utilized as an anxiety “treatment” by some people, with preclinical studies of the anxiolytic effects of cannabadiol components providing a theoretical justification for this. Nonetheless, it should be fairly obvious that someone showing up in a clinician's office with bothersome anxiety who is using marijuana frequently might want to consider reducing or eliminating this use to see if it is contributing to their anxiety. While many returning veterans may be using marijuana to “treat” PTSD and have been empowered by research showing reduced cannabinoid receptors on PET scan in patients with PTSD, it is also likely that agonist treatment will further reduce this receptor number, perhaps creating a vicious neurobiologic cycle.43
Unrecognized medical illness
It is much more frequent for anxiety disorders to be mistaken for medical illness than the converse. Thus, many anxious patients first have costly medical workups and procedures, usually focusing on cardiopulmonary, gastrointestinal, and otoneurologic systems as the explanation for these specific physical symptoms. It is rare in clinical practice that a medical condition will account for anxiety, but the probability goes up slightly if the anxiety has been refractory to treatment. A number of illnesses need to be considered.
Complex partial seizure disorder presenting with symptoms of depersonalization, paroxysmal anxiety, and rarely gastrointestinal symptoms should be considered, and a careful history looking for head trauma, including a history of playing contact sports and having concussions, is important. In a young woman with sudden paroxysmal anxiety, pulmonary embolus is often overlooked, even in emergency settings. Hyperthyroidism is commonly listed in most “medical causes of anxiety” lists, and is easy enough to screen for, but is not a common cause. The same can be said for pheochromocytoma, whose distinguishing characteristic is often referred to as “cold fear,” ie, prominent autonomic symptoms without strong subjective fear or anxiety.
In this author's experience evaluating refractory anxiety in over 1 000 patients, only one time was a definitive medical cause suspected and found: someone with odd symptoms of paroxysmal anxiety and depersonalization who was found to have a temporal lobe tumor. An additional question is whether the presence of comorbid medical illness might make treatment less effective. Our recent study of this issue showed that treatment effects are comparable in anxious patients with and without comorbid medical illness. However, anxious patients with comorbid medical illness have greater severity of anxiety than those without medical illness, and comparable change still leaves fewer of these patients meeting remission criteria.44
Wrong diagnosis, bipolar illness, and other mimics of anxiety
There are a number of other conditions that may present with prominent anxiety symptoms. The most common, of course, now re-emphasized in the DSM-5, is MDD. Some patients may actually deny depressed mood and only endorse anxious mood, yet may have multiple symptoms of MDD that they attribute to “anxiety,” ie, “of course I cannot sleep or eat, am exhausted, have no interest or enjoyment, and cannot concentrate.... you would too if you had to deal with this constant unremitting anxiety.” More importantly, recent analyses have suggested that comorbid anxiety as a symptom has more prognostic value than the presence of a comorbid anxiety disorder,45 and that “spectrum” anxiety symptoms that include separation anxiety have similar import.46 While we have made major progress in differentiating anxiety into different syndromes and disorders with successive versions of the DSM, we may have to go “back to the future” as DSM-5 did in highlighting the prognostic importance of anxiety as a more undifferentiated symptom. This particular cause of refractory anxiety is uncommonly encountered because first-line antidepressant treatment will be effective for both mood and anxiety disorders. But it can be seen in patients treated with benzodiazepines alone, or in anxious depressions refractory to first-line antidepressant treatment. Interestingly, in contrast to most of the literature showing that anxiety predicts poorer outcome in depressive illness, the acute beneficial effects of intravenous ketamine are greater with the anxious depression subtype.47 The distinction between depression and anxiety in these comorbid cases becomes more important in educating patients about refractory anxiety, because recommending a depression-specific treatment (eg, in severe cases, ECT) often causes patients to argue that “you keep talking about depression, but my problem is anxiety.”
However, perhaps the most important diagnostic mimic seen routinely in practice, which tends to collect patients with refractory anxiety, is undiagnosed bipolar illness, most often bipolar 2 or “bipolar spectrum” illness. Such patients may not endorse or report typical hypomania and may have mood states that alternate between periodic retarded depressions and anxious dysphoric mixed states. The DSM-5 has made this differential diagnosis even harder, because, while it allows an anxious distress modifier for bipolar patients, it has removed as a core feature from mixed mania, what some experts see as the most important symptom,48 that of severe internal agitation and restlessness (which in turn contributes to dysphoric mood, erratic concentration, irritability, insomnia, and anorexia).
What is the supporting evidence for this concept? In addition to the high prevalence of anxiety disorders in bipolar illness (50% to 75% lifetime),49 studies have documented that in those with comorbid anxiety and bipolar disorders, the anxiety disorder occurs an average of 3 years earlier,49 and that the presence of an anxiety disorder predicts the transition from a diagnosis of major depression to bipolar illness in adults.50,51 Additionally, mania or mixed states, especially when occurring in the course of a rapid-cycling bipolar 2 disorder, may be misdiagnosed as anxiety states.52 Interestingly, children of bipolar parents treated for anxiety with antidepressants have a high rate of adverse responses including increased agitation and irritability.53 This may indicate what is often called a “treatment emergent affective switch.”54 Refractory patients in this category may also report rapid improvement on antidepressants that is not sustained beyond a few weeks or months at the most, and a stair-step pattern of responding, and then losing response, to multiple changes in antidepressants. Only recently are experts considering the possibility that antidepressants are overused and may be harmful to some bipolar patients.55 Some of these patients may report inability to tolerate antidepressants and need for benzodiazepines which can prompt clinician concern about abuse and or psychological dependence, when it only means these agents are far more tolerable for someone in the midst of a mixed state. The study of mixed states has been difficult, and the state of the art in a recent review leaves much that is wanting.56
Unfortunately, this differential diagnosis can be vexing for the clinician wedded to a strict interpretation of the diagnostic criteria for bipolar illness, due to the absence of clearly defined mania or hypomania. But attention to other features thought to indicate a soft bipolar condition will greatly improve the probability of diagnosis. These include the following: a history of post-partum depression, a family history of bipolar illness, agitation with antidepressants, rapid (within days) response to antidepressants, frequent loss of antidepressant effects, brief psychotic/paranoid episodes, and early-onset depression.57 Treatment with mood stabilizers and atypical antipsychotics often has major benefit in these patients. Recent cases have included a patient with early-onset panic attacks and subsequent development of agoraphobia, an intensive course of CBT, anxiety remission but then unexplained bouts of panic despite “working” a CBT program. Further inquiry revealed an accompanying loss of anti-panic effect to an SSRI requiring a second antidepressant, and then when this was lost, a switch to an SNRI that caused rapid improvement in days, but a loss of effect in several months. The panic breakthrough occurred briefly during these apparent remissions. Following this, there were more depressive episodes. Treatment with the anticonvulsant oxcarbazepine resulted in sustained remission.
Substance use disorder is an important comorbidity in patients with primary anxiety disorders and often makes it difficult to distinguish between naturallyoccurring alterations in anxiety and those induced by substance use or withdrawal. Anxiety can occur as part of withdrawal from multiple substances, especially alcohol, marijuana and opiates, and as a symptom of intoxication with marijuana, psychedelics, cocaine, and other stimulants. Substance use is often unrecognized in ambulatory settings, where clinicians assume that most patients with this problem are already being treated in specialty or inpatient settings. Ambulatory clinicians rarely obtain a urine drug screen as part of a routine intake evaluation, much less order some of the newer tests capable of assessing recent alcohol use. Screening measures like the AUDIT-C are often useful to assess problem alcohol use or abuse because it contains only three questions on use frequency and quantity, has standardized cutoffs, and is not viewed with suspicion bymost heavy alcohol users who think their use amount may be “normal.” 58
A wealth of data supports poorer outcome in multiple anxiety disorders when there is a comorbid substance use problem.2,59 In anxious patients with bipolar illness, substance use is even more important a consideration in view of the high rate of substance use disorder comorbidity in bipolar patients and a similar association with poor outcome. A trial of abstinence will usually answer this question, although the duration has to be several months to evaluate the link between anxiety and use, there has to be ongoing treatment, preferably in a 12-step program (such programs have been shown to have anxiolytic effects themselves due to the support and empowerment they offer) and residual anxiety then has to be treated with either medication or CBT.
A number of studies have shown high rates of GAD comorbidity in adult patients with ADHD.60 It is not clear whether this is simply due to definitional overlap, with ADHD symptoms of restlessness and impatience being misattributed to GAD. This is a very tricky differential, since more refractory ADHD cases often suffer from comorbid anxiety.61 In these cases, use of guanfacine is sometimes preferable to stimulant treatment and may even mitigate adverse effects of the latter when used in combination. ADHD can also confuse evaluation of phobic avoidance, eg, a patient whose flying phobia seemed to be reactivated during several years of not being treated with stimulants, and who on close questioning revealed it is the aggravation and impatience related to the long waiting periods to get on a flight and the confinement during the long flight that was most problematic, rather than actual “anxiety.”
Treatments
After all the above considerations have been addressed, the clinician needs to provide additional treatment. There are extremely few RCTs that have examined approaches to treatment refractory anxiety. Thus, we will not only review this data, but also review the efficacy of more novel treatments not in the mainstream of the SSRI/SNRI, benzodiazepine, CBT family of first-line treatments. However, the most common first step employed by most anxiety treatment experts when a patient has failed to respond optimally to one of the two standard modalities is to add the other modality ie, to provide “combined treatment.”
Combination medication and CBT
Randomized trials comparing combined antidepressant and CBT treatment, with either modality alone and also with an active placebo, have most often been done in nonrefractory patients seeking initial treatment. These studies have suggested slight superiority for combined treatment with panic disorder,62 more definitive advantage for social anxiety disorder,63 but absolutely no advantage of combined treatment compared with CBT alone for OCD.13 One study in elderly GAD patients showed an augmentation effect of combined CBT compared with SSRI alone on worry symptoms,64 although no advantage of the combined treatment over SSRI alone in preventing relapse. There are no adequately powered studies of combined versus single treatment in PTSD.
There is more controversy over the combination of benzodiazepines with CBT. One early study showed that alprazolam combined with CBT produced worse panic disorder outcome in the long term, compared with CBT alone,65 and an observational analysis indicated poorer outcome in panic patients receiving benzodiazepines during group CBT.66 There has been longstanding speculation that these agents could interfere with desensitization in phobic disorders, perhaps by blocking the anxiety response needed to initiate an extinction process, perhaps by preventing a more internal locus of control needed for successful CBT, or perhaps by interacting in complex ways with context. However, randomized trials with the exception of the Marks study do not support adverse effects of benzodiazepines on anxiety disorder outcomes with CBT.67,68
These data on the advantage of combined treatment in treatment naive anxious patients does not answer the question of whether anxious patients symptomatic with one treatment modality would benefit from the addition of the other. What is the available evidence here? Added SSRI medication may help CBT-refractory panic according to one small study showing efficacy for paroxetine in a population of panic disorder patients failing to respond to CBT69 Another unpublished studyin CBT-nonresponsive panic disorder patients showed equivalent benefit to the addition of either paroxetine or more CBT, with paroxetine superior to CBT at 6 weeks but not at 12 weeks vs placebo (David Barlow, personal communication, under review). Adding CBT in patients refractory to medications may also be of benefit. In one study of refractory panic given higher dose and longer duration SSRI treatment without benefit, there was equivalent benefit to added CBT vs added clonazepam.70 An unpublished secondary analysis from our multicenter Coordinated Anxiety Learning and Management (CALM) study71 examined a large mixed group of anxiety disorder patients with panic, GAD, SAD, and PTSD who entered the study having already received an adequate dose and duration of either an SSRI or a benzodiazepine. Patients randomized to the CALM intervention and receiving additional CBT (they continued their medication) had significantly higher response and remission rates than those continuing with naturalistic treatment in usual care (Figure 4). A study of Cambodian refugees with PTSD from the Pol Pot era, who continued to have symptoms despite SSRI treatment, showed benefit of adding a culturally tailored CBT72 Finally, in OCD patients refractory to SSRIs, the addition of ERP resulted in a much greater response rate than addition of an atypical neuroleptic medication.73
Figure 4.
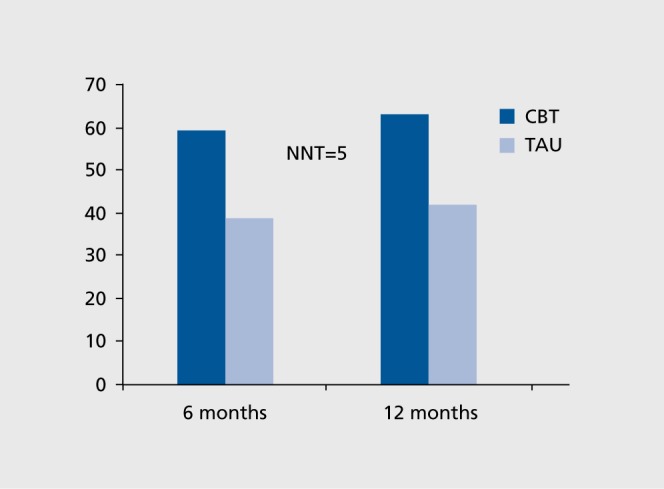
Response rates for cognitive behavioral therapy (CBT) vs treatment as usual (TAU) in medication-resistant anxiety: the CALM study.71
A novel combination treatment has been the addition of d-cycloserine, a partial agonist at the N-methyl-D-aspartate (NMDA) receptor, to CBT. This is based not on synergistically combining two anxiolytic modalities but rather on providing a medication that can somehow enhance the extinction process either by increasing NMDA mediated neuroplasticity or by interfering with reconsolidation or reinstatement of fear via a reduction of NMDA activity.74 An augmenting effect has been shown for panic, SAD, OCD, specific phobia, and PTSD, though the majority of studies have utilized a truncated course of CBT, ie, fewer than the optimal number of sessions to get maximal effect, which likelyenhanced the ability to see an advantage for d-cycloserine augmentation. Use of a more complete CBT course resulted in no effect for SAD75 but still an effect for PTSD.76 Most recently, a reanalysis of prior studies suggested that effects are beneficial ONLY when d-cycloserine is given after a successful exposure session ie, anxiety decreases after the initial rise with exposure. In fact, in unsuccessful sessions ie, no anxiety reduction, d-cycloserine may enhance the anxiety response rather than the extinction response.77 Unfortunately, there are still no studies of this agent in CBT-refractory patients, where it would be potentially most useful. Thus, studies so far suggest that this agent might accelerate the course of CBT treatment, but at the expense of making it more cumbersome.
Novel medication treatments
Studies document superiority, compared with placebo, for both gabapentin (for social anxiety78 and high-severity panic79) and pregabalin (for generalized80 and social anxiety81). These medications, considered to be in the broad class of anticonvulsants, have the unique mechanism of blocking the alpha delta calcium channel. A number of studies have showed comparability in onset and amount of effect with comparison benzodiazepines, such as alprazolam and lorazepam,80 and with earlier onset and comparable effect as standard SNRIs such as venlafaxine.82 Pregabalin has become a major treatment for anxiety in Europe but has not been approved by the FDA. Whether this agent has any efficacy advantage over standard benzodiazepines is unclear, though it appears to have fewer adverse effects in terms of risk of abuse and dependence. Hydroxyzine is an effective agent for GAD but is unlikely to provide any benefit in a refractory patient.80 Prazosin may provide significant benefit for PTSD patients struggling with nightmares and other symptoms of hyperarousal.83 In contrast to the above study which focused on general entry level samples, some of the earlier trials were performed in de facto treatment-refractory PTSD patients with decades of nightmares and the effect was dramatic.84 There have been a number of positive open trials of more typical anticonvulsant agents such as valproate, topirimate, and tiagabine, but no consistent RCT evidence showing efficacy of these agents. It is interesting to speculate that some of the inconsistent and spotty evidence with these agents might reflect anxious patients with a bipolar diathesis who are responding to their mood -stabilizing effects (see above).
Epidemiologic surveys have shown individuals with emotional distress as more likely than those without distress to seek out and utilize herbal medicine approaches,85 though a recent primary care survey of mixed group of anxious and depressed and nondistressed patients showed that use was more specific for depression rather than anxiety.86 Recent reviews have highlighted a large number of plant-based substances with possible efficacy for anxiety, but the studies are small and methodologically poor.87,88 One of the most well supported agents used in the past for anxiety has been kava kava, but recently this has been found to have unacceptable hepatotoxicity and is no longer widely utilized. These reviews also note that other approaches found effective for depression such as omega 3 fatty acids and St John's wort have not been shown to be effective for anxiety. Finally, another herbal medicine commonly used in past years for anxiety, valerian root, has limited evidence of efficacy according to these reviews.
Novel nonmedication treatments
In addition to CBT, there is emerging evidence from randomized controlled trials documenting efficacy of psychodynamic psychotherapy for panic,89 generalized,90 and social anxiety,91 and for interpersonal therapy (IPT) for both social anxiety92 and more recently PTSD.93 In the PTSD study, many of the patients had chronic PTSD and could be viewed as treatment-refractory. In these studies, CBT (or prolonged exposure for the PTSD study) seems to have a slight edge when used as a comparator, and in treatment delivery, psychodynamic therapy requires more sessions and more therapist training, making it is a less “robust” treatment. Mindfulness-based stress reduction, already known to have potent effects in recurrent major depression,94 appears to be effective in pilot work for mixed groups with multiple anxiety disorders, with a particular benefit versus CBT against rumination, but less efficacy against arousal symptoms.95 Finally, after a promising early study suggesting potential benefits of exercise in panic disorder,96 meta-analyses of the available studies in multiple anxiety disorder groups, suggest effects are less consistent, and inferior to standard treatments.97,98 These latter two treatments seem to have the best empirical evidence of any complementary medicine approaches to anxiety, and seem quite superior to the herbal medicine approaches for anxiety cited earlier.
Evidence from randomized controlled trials
Although benzodiazepine addition to an SSRI/SNRI is the most commonly used augmentation strategy for refractory anxiety, there have been no studies until this past year when Pollack et al conclusively showed in SAD that addition of clonazepam to sertraline was superior to switching to venlafaxine or just giving more time for the sertraline to work.99 The beneficial effect was in response but not remission, which may be consistent with clinical experience that in refractory patients, these agents are most often beneficial, but not curative. This study is at variance with concerns about noxious effects of benzodiazepines, initially supported by some observational analyses showing that benzodiazepines predicted poor outcome in panic disorder,100 and were associated with increased anxiety sensitivity,101 by two small randomized studies suggesting PTSD outcomes might be worse with benzodiazepines,102,103 and by a secondary analysis from one benzodiazepine study of GAD showing that outcome was worse compared with imipramine in the subgroup of patients with higher severity depressive symptoms (Figure 5), even though they did not meet diagnostic criteria for major depression.104 However, the addition of a selective benzodiazapine-receptor binding hypnotic agonist, eszopiclone, to an SSRI produced significantly greater improvement in non-sleep-related anxiety symptoms in two separate studies of GAD and PTSD.105,106
Figure 5.
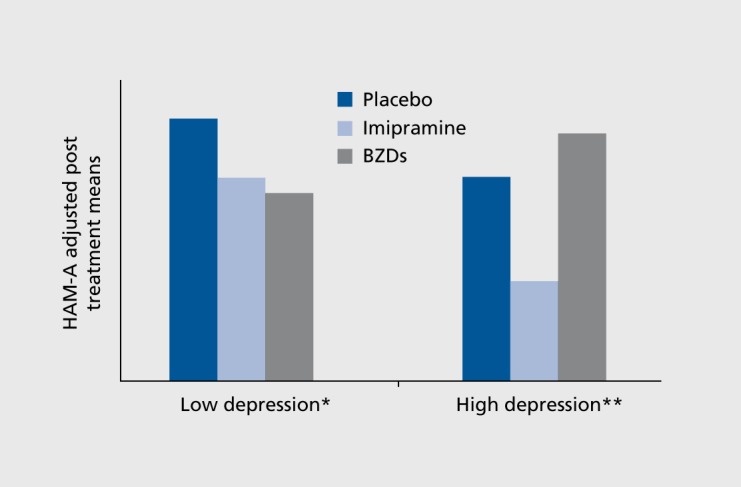
Generalized anxiety disorder with depressive symptoms: could benzodiazepines make anxiety worse? BZD, benzo-diazepine.104
*Imipramine/diazepam>placebo P<0.05.
**Imipramine>diazepam P<0.05.
Unlike depression, there is less consistent evidence that atypical neuroleptics may be beneficial for some anxiety disorders.107 The best meta-analytic evidence supports augmentation of SSRIs in refractory OCD patients with risperidone.108 While quetiapine has shown evidence of efficacy as monotherapy in nonrefractory patients with generalized anxiety (with an effect size at least as large for SSRIs if not larger), there is no effect in refractory generalized anxiety.109 While a recent meta-analysis suggested that atypical neuroleptics show promise in PTSD, with specific effects for olanzapine, quetiapine, and risperidone in small studies,110 the largest PTSD study failed to show a positive effect for risperidone as an augmenting agent to SSRIs,111 considerably dampening enthusiasm for this strategy in PTSD. However, this study was done in veterans with very chronic and refractory PTSD, and a recent study in civilian populations suggested efficacy for olanzapine as an augmenting agent.112 There is no evidence that atypical neuroleptics are effective as either monotherapy or augmentation agents for panic disorder and social anxiety disorder.
Two studies have explored efficacy of the β-blocker pindolol, which also has serotonin 1A partial aonist effects, added to antidepressants in refractory anxiety. While it was shown to be effective in a small study of panic disorder,113 it was not shown to be effective in SAD.114 This is not a strategy commonly used in refractory anxiety.
Conclusion
These findings suggest that the initial focus of the clinician facing a patient seeking care for treatment-refractory anxiety should be on the factors related to pseudoresistance. This author's clinical experience over several decades with this population suggests that the most common factors relate to an unrecognized mood disorder, often a bipolar spectrum variant, occult substance abuse, often with alcohol, and beliefs and attitudes that have prevented adequate treatment uptake. It is a legitimate objection that many successfully treated newly diagnosed bipolar patients do not have bipolar illness, but rather an anxiety disorder that is responsive to mood stabilizer treatment. Nonetheless, this group of patients shares many characteristics of bipolar patients but often does not have evidence of frank and obtrusive hypomania. After the above factors have been addressed, the clinician should proceed by exploring combination treatment with multiple modalities (this has usually been tried already) and then either multiple novel medications, more aggressive, longer-duration CBT, or a switch to another psychotherapeutic modality such as IPT or psychodynamic psychotherapy.
REFERENCES
- 1.Kessler RC., Berglund P., Dernier O., Jin R., Merikangas KR., Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 2.Bruce SE., Yonkers KA., Otto MW., et al Influence of psychiatric comorbidity on recovery and recurrence in generalized anxiety disorder, social phobia, and panic disorder: a 12-year prospective study. Am J Psychiatry. 2005;162(6):1179–1187. doi: 10.1176/appi.ajp.162.6.1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Etkin A. Neurobiology of anxiety: from neural circuits to novel solutions? Depress Anxiety. 2012;29(5):355–358. doi: 10.1002/da.21957. [DOI] [PubMed] [Google Scholar]
- 4.Ravindran LN., Stein MB. The pharmacologic treatment of anxiety disorders: a review of progress. J Clin Psychiatry. 2010;71(7):839–854. doi: 10.4088/JCP.10r06218blu. [DOI] [PubMed] [Google Scholar]
- 5.Pecknold JC., Swinson RP., Kuch K., Lewis CP. Alprazolam in panic disorder and agoraphobia: Results from a multicenter trial: III. Discontinuation effects. Arch Gen Psychiatry. 1988;45:429–436. doi: 10.1001/archpsyc.1988.01800290043006. [DOI] [PubMed] [Google Scholar]
- 6.Klein E., Colin V., Stolk J., Lenox RH. Alprazolam withdrawal in patients with panic disorder and generalized anxiety disorder: vulnerability and effect of carbamazepine. Am J Psychiatry. 1994;151:1760–1766. doi: 10.1176/ajp.151.12.1760. [DOI] [PubMed] [Google Scholar]
- 7.Goddard AW., Brouette T., Almai A., Jetty P., Woods SW., Charney D. Early coadministration of clonazepam with sertraline for panic disorder. Arch Gen Psychiatry. 2001;58(7):681–686. doi: 10.1001/archpsyc.58.7.681. [DOI] [PubMed] [Google Scholar]
- 8.Olatunji BO., Cisler JM., Deacon BJ. Efficacy of cognitive behavioral therapy for anxiety disorders: a review of meta-analytic findings. Psychiatr Clin North Am. 2010;33(3):557–577. doi: 10.1016/j.psc.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 9.Wilamowska ZA., Thompson-Hollands J., Fairholme CP., Ellard KK., Farchione TJ., Barlow DH. Conceptual background, development, and preliminary data from the unified protocol for transdiagnostic treatment of emotional disorders. Depress Anxiety. 2010;27(10):882–890. doi: 10.1002/da.20735. [DOI] [PubMed] [Google Scholar]
- 10.Mitte K. Meta-analysis of cognitive-behavioral treatments for generalized anxiety disorder: a comparison with pharmacotherapy. Psychol Bull. 2005;131(5):785–795. doi: 10.1037/0033-2909.131.5.785. [DOI] [PubMed] [Google Scholar]
- 11.Davidson JR., Foa EB., Huppert JD., et al Fluoxetine, comprehensive cognitive behavioral therapy, and placebo in generalized social phobia. Arch Gen Psychiatry. 2004;61(10):1005–1013. doi: 10.1001/archpsyc.61.10.1005. [DOI] [PubMed] [Google Scholar]
- 12.Mitte K. A meta-analysis of the efficacy of psycho- and pharmaco-therapy in panic disorder with and without agoraphobia. J Affect Disord. 2005;88(1):27–45. doi: 10.1016/j.jad.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 13.Foa EB., Liebowitz MR., Kozak MJ., et al Randomized, placebo-controlled trial of exposure and ritual prevention, clomipramine, and their combination in the treatment of obsessive-compulsive disorder. Am J Psychiatry. 2005;162(1):151–161. doi: 10.1176/appi.ajp.162.1.151. [DOI] [PubMed] [Google Scholar]
- 14.Duan N., Braslow JT., Weisz JR., Wells KB. Fidelity, adherence, and robustness of interventions. Psychiatr Serv. 2001;52(4):413. doi: 10.1176/appi.ps.52.4.413. [DOI] [PubMed] [Google Scholar]
- 15.Otto MW., Smits JA., Reese HE. Cognitive-behavioral therapy for the treatment of anxiety disorders. J Clin Psychiatry. 2004;65(suppl 5):34–41. [PubMed] [Google Scholar]
- 16.Stein MB., Roy-Byrne PP., Craske MG., et al Quality of and patient satisfaction with primary health care for anxiety disorders. J Clin Psychiatry. 2011;72(7):970–976. doi: 10.4088/JCP.09m05626blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Keitner Gl., Mansfield AK. Management of treatment-resistant depression. Psychiatr Clin North Am. 2012;35(1):249–265. doi: 10.1016/j.psc.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 18.Goisman RM., Warshaw MG., Keller MB. Psychosocial treatment prescriptions for generalized anxiety disorder, panic disorder, and social phobia, 1991-1996. Am J Psychiatry. 1999;156(11):1819–1821. doi: 10.1176/ajp.156.11.1819. [DOI] [PubMed] [Google Scholar]
- 19.Yonkers KA., Ellison JM., Shera DM., et al Description of antipanic therapy in a prospective longitudinal study. J Clin Psychopharmacol. 1996;16(3):223–232. doi: 10.1097/00004714-199606000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Young AS., Klap R., Sherbourne CD., Wells KB. The quality of care for depressive and anxiety disorders in the United States. Arch Gen Psychiatry. 2001;58(1):55–61. doi: 10.1001/archpsyc.58.1.55. [DOI] [PubMed] [Google Scholar]
- 21.Londborg PD., Hegel MT., Goldstein S., et al Sertraline treatment of posttraumatic stress disorder: results of 24 weeks of open-label continuation treatment. J Clin Psychiatry. 2001;62(5):325–331. doi: 10.4088/jcp.v62n0503. [DOI] [PubMed] [Google Scholar]
- 22.Montgomery SA., Sheehan DV., Meoni P., Haudiquet V., Hackett D. Characterization of the longitudinal course of improvement in generalized anxiety disorder during long-term treatment with venlafaxine XR. J Psychiatr Res. 2002;36(4):209–217. doi: 10.1016/s0022-3956(02)00005-5. [DOI] [PubMed] [Google Scholar]
- 23.Zitrin CM., Klein DF., Woerner MG., Ross DC. Treatment of phobias. I. Comparison of imipramine hydrochloride and placebo. Arch Gen Psychiatry. 1983;40(2):125–138. doi: 10.1001/archpsyc.1983.01790020019002. [DOI] [PubMed] [Google Scholar]
- 24.Loebel AD., Hyde TS., Dunner DL. Early placebo response in anxious and depressed patients. J Clin Psychiatry. 1986;47(5):230–233. [PubMed] [Google Scholar]
- 25.Marcus SM., Gorman J., Shear MK., et al A comparison of medication side effect reports by panic disorder patients with and without concomitant cognitive behavior therapy. Am J Psychiatry. 2007;164(2):273–275. doi: 10.1176/ajp.2007.164.2.273. [DOI] [PubMed] [Google Scholar]
- 26.Otto MW., Pollack MH., Sachs GS., Reiter SR., Meltzer-Brody S., Rosenbaurn JF. Discontinuation of benzodiazepine treatment: efficacy of cognitive-behavioral therapy for patients with panic disorder. Am J Psychiatry. 1993;150(10):1485–1490. doi: 10.1176/ajp.150.10.1485. [DOI] [PubMed] [Google Scholar]
- 27.Iwanami T., Maeshima H., Baba H., et al Psychomotor agitation in major depressive disorder is a predictive factor of mood-switching. J Affect Disord. 2015;170:185–189. doi: 10.1016/j.jad.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 28.Peveler R., George C., Kinmonth AL., Campbell M., Thompson C. Effect of antidepressant drug counselling and information leaflets on adherence to drug treatment in primary care: randomised controlled trial. BMJ. 1999;319(7210):612–615. doi: 10.1136/bmj.319.7210.612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mojtabai R., Olfson M., Mechanic D. Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Arch Gen Psychiatry. 2002;59(1):77–84. doi: 10.1001/archpsyc.59.1.77. [DOI] [PubMed] [Google Scholar]
- 30.Grilo CM., Money R., Barlow DH., et al Pretreatment patient factors predicting attrition from a multicenter randomized controlled treatment study for panic disorder. Compr Psychiatry. 1998;39(6):323–332. doi: 10.1016/s0010-440x(98)90043-8. [DOI] [PubMed] [Google Scholar]
- 31.Hofmann SG., Barlow DH., Papp LA., et al Pretreatment attrition in a comparative treatment outcome study on panic disorder. Am J Psychiatry. 2998;155(1):43–47. doi: 10.1176/ajp.155.1.43. [DOI] [PubMed] [Google Scholar]
- 32.Zoellner LA., Feeny NC., Cochran B., Pruitt L. Treatment choice for PTSD. Behav Res Then. 2003;41(8):879–886. doi: 10.1016/s0005-7967(02)00100-6. [DOI] [PubMed] [Google Scholar]
- 33.Kwan BM., Dimidjian S., Rizvi SL. Treatment preference, engagement, and clinical improvement in pharmacotherapy versus psychotherapy for depression. Behav Res Ther. 2010;48(8):799–804. doi: 10.1016/j.brat.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Weissman MM., Verdeli H., Gameroff MJ., et al National survey of psychotherapy training in psychiatry, psychology, and social work. Arch Gen Psychiatry. 2006;63(8):925–934. doi: 10.1001/archpsyc.63.8.925. [DOI] [PubMed] [Google Scholar]
- 35.Glenn D., Golinelli D., Rose RD., et al Who gets the most out of cognitive behavioral therapy for anxiety disorders? The role of treatment dose and patient engagement. J Consult Clin Psychol. 2013;81(4):639–649. doi: 10.1037/a0033403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vilarim MM., Rocha Araujo DM., Nardi AE. Caffeine challenge test and panic disorder: a systematic literature review. Exp Rev Neurotherapeutics. 2011;11(8):1185–1195. doi: 10.1586/ern.11.83. [DOI] [PubMed] [Google Scholar]
- 37.Dews PB., O'Brien CP., Bergman J. Caffeine: behavioral effects of withdrawal and related issues. Food Chem Toxicol. 2002;40(9):1257–1261. doi: 10.1016/s0278-6915(02)00095-9. [DOI] [PubMed] [Google Scholar]
- 38.Roy-Byrne PP., Uhde TW., Post RM. Effects of one night's sleep deprivation on mood and behavior in panic disorder. Patients with panic disorder compared with depressed patients and normal controls. Arch Gen Psychiatry. 1986;43(9):895–899. doi: 10.1001/archpsyc.1986.01800090085011. [DOI] [PubMed] [Google Scholar]
- 39.Roy-Byrne PP., Russo J., Cowley DS., Katon WJ. Panic disorder in public sector primary care: clinical characteristics and illness severity compared with “mainstream” primary care panic disorder. Depress Anxiety. 2003;17(2):51–57. doi: 10.1002/da.10082. [DOI] [PubMed] [Google Scholar]
- 40.Yonkers KA., Dyck IR., Warshaw M., Keller MB. Factors predicting the clinical course of generalised anxiety disorder. Br J Psychiatry. 2000;176:544–549. doi: 10.1192/bjp.176.6.544. [DOI] [PubMed] [Google Scholar]
- 41.Wade SL., Monroe SM., Michelson LK. Chronic life stress and treatment outcome in agoraphobia with panic attacks. Am J Psychiatry. 1993;150(10):1491–1495. doi: 10.1176/ajp.150.10.1491. [DOI] [PubMed] [Google Scholar]
- 42.Crippa JA., Zuardi AW., Martin-Santos R., et al Cannabis and anxiety: a critical review of the evidence. Hum Psychopharmacol. 2009;24(7):515–523. doi: 10.1002/hup.1048. [DOI] [PubMed] [Google Scholar]
- 43.Neumeister A. The endocannabinoid system provides an avenue for evidence-based treatment development for PTSD. Depress Anxiety. 2013;30(2):93–96. doi: 10.1002/da.22031. [DOI] [PubMed] [Google Scholar]
- 44.Campbell-Sills L., Stein MB., Sherbourne CD., et al Effects of medical comorbidity on anxiety treatment outcomes in primary care. Psychosomat Med. 2013;75(8):713–720. doi: 10.1097/PSY.0b013e31829def54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Coryell W., Fiedorowicz JG., Solomon D., Leon AC., Rice JP., Keller MB. Effects of anxiety on the long-term course of depressive disorders. Br J Psychiatry. 2012;200(3):210–215. doi: 10.1192/bjp.bp.110.081992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Frank E., Cassano GB., Rucci P., et al Predictors and moderators of time to remission of major depression with interpersonal psychotherapy and SSRI pharmacotherapy. Psychol Med. 2011;41(1):151–162. doi: 10.1017/S0033291710000553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.lonescu DF., Luckenbaugh DA., Niciu MJ., et al Effect of baseline anxious depression on initial and sustained antidepressant response to ketamine. J Clin Psychiatry. 2014;75(9):e932–938. doi: 10.4088/JCP.14m09049. [DOI] [PubMed] [Google Scholar]
- 48.Koukopoulos A., Sani G., Ghaemi SN. Mixed features of depression: why DSM-5 is wrong (and so was DSM-IV). Br J Psychiatry. 2013;203(1):3–5. doi: 10.1192/bjp.bp.112.124404. [DOI] [PubMed] [Google Scholar]
- 49.Sala R., Goldstein Bl., Morcillo C., Liu SM., Castellanos M., Blanco C. Course of comorbid anxiety disorders among adults with bipolar disorder in the U.S. population. J Psychiatr Res. 2012;46(7):865–872. doi: 10.1016/j.jpsychires.2012.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Goldstein Bl., Levitt AJ. The specific burden of comorbid anxiety disorders and of substance use disorders in bipolar I disorder. Bipolar Disord. 2008;10(1):67–78. doi: 10.1111/j.1399-5618.2008.00461.x. [DOI] [PubMed] [Google Scholar]
- 51.Gilman SE., Dupuy JM., Perils RH. Risks for the transition from major depressive disorder to bipolar disorder in the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2012;73(6):829–836. doi: 10.4088/JCP.11m06912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gao K., Kemp DE., Conroy C., Ganocy SJ., Findling RL., Calabrese JR. Comorbid anxiety and substance use disorders associated with a lower use of mood stabilisers in patients with rapid cycling bipolar disorder: a descriptive analysis of the cross-sectional data of 566 patients. Int J Clin Pract. 2010;64(3):336–344. doi: 10.1111/j.1742-1241.2009.02284.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Strawn JR., Adler CM., McNamara RK., et al Antidepressant tolerability in anxious and depressed youth at high risk for bipolar disorder: a prospective naturalistic treatment study. Bipolar Disord. 2014;16(5):523–530. doi: 10.1111/bdi.12113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Post RM., Altshuler LL., Leverich GS., et al Mood switch in bipolar depression: comparison of adjunctive venlafaxine, bupropion and sertraline. Br J Psychiatry. 2006;189:124–131. doi: 10.1192/bjp.bp.105.013045. [DOI] [PubMed] [Google Scholar]
- 55.Pacchiarotti I., Bond DJ., Baldessarini RJ., et al The International Society for Bipolar Disorders (ISBD) task force report on antidepressant use in bipolar disorders. Ami J Psychiatry. 2013;170(11):1249–1262. doi: 10.1176/appi.ajp.2013.13020185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Swann AC., Lafer B., Perugi G., et al Bipolar mixed states: an international society for bipolar disorders task force report of symptom structure, course of illness, and diagnosis. Ami J Psychiatry. 2013;170(1):31–42. doi: 10.1176/appi.ajp.2012.12030301. [DOI] [PubMed] [Google Scholar]
- 57.Phelps J., Ghaemi SN. The mistaken claim of bipolar'overdiagnosis': solving the false positives problem for DSM-5/ICD-11. Acta Psychiatr Scand. 2012;126(6):395–401. doi: 10.1111/j.1600-0447.2012.01912.x. [DOI] [PubMed] [Google Scholar]
- 58.Dawson DA., Grant BF., Stinson FS., Zhou Y. Effectiveness of the derived Alcohol Use Disorders Identification Test (AUDIT-C) in screening for alcohol use disorders and risk drinking in the US general population. Alcohol Clin Exp Res. 2005;29(5):844–854. doi: 10.1097/01.alc.0000164374.32229.a2. [DOI] [PubMed] [Google Scholar]
- 59.Forbes D., Creamer M., Hawthorne G., Allen N., McHugh T. Comorbidity as a predictor of symptom change after treatment in combat-related posttraumatic stress disorder. J Nerv Ment Dis. 2003;191(2):93–99. doi: 10.1097/01.NMD.0000051903.60517.98. [DOI] [PubMed] [Google Scholar]
- 60.Roy-Byrne P., Scheele L., Brinkley J., et al Adult attention-deficit hyperactivity disorder: assessment guidelines based on clinical presentation to a specialty clinic. Compr Psychiatry. 1997;38(3):133–140. doi: 10.1016/s0010-440x(97)90065-1. [DOI] [PubMed] [Google Scholar]
- 61.Moderators and mediators of treatment response for children with attention-deficit/hyperactivity disorder: the Multimodal Treatment Study of children with Attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 1999;56(12):1088–1096. doi: 10.1001/archpsyc.56.12.1088. [DOI] [PubMed] [Google Scholar]
- 62.Furukawa TA., Watanabe N., Churchill R. Psychotherapy plus antidepressant for panic disorder with or without agoraphobia: systematic review. Br J Psychiatry. 2006;188:305–312. doi: 10.1192/bjp.188.4.305. [DOI] [PubMed] [Google Scholar]
- 63.Blanco C., Heimberg RG., Schneier FR., et al A placebo-controlled trial of phenelzine, cognitive behavioral group therapy, and their combination for social anxiety disorder. Arch Gen Psychiatry. 2010;67(3):286–295. doi: 10.1001/archgenpsychiatry.2010.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wetherell JL., Petkus AJ., White KS., et al Antidepressant medication augmented with cognitive-behavioral therapy for generalized anxiety disorder in older adults. Am J Psychiatry. 2013;170(7):782–789. doi: 10.1176/appi.ajp.2013.12081104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Marks IM., Swinson RP., Basoglu M., et al Alprazolam and exposure alone and combined in panic disorder with agoraphobia. A controlled study in London and Toronto. Br J Psychiatry. 1993;162:776–787. doi: 10.1192/bjp.162.6.776. [DOI] [PubMed] [Google Scholar]
- 66.Westra HA., Stewart SH., Conrad BE. Naturalistic manner of benzodiazepine use and cognitive behavioral therapy outcome in panic disorder with agoraphobia. J Anxiety Disord. 2002;16(3):233–246. doi: 10.1016/s0887-6185(02)00091-9. [DOI] [PubMed] [Google Scholar]
- 67.Power KG., Simpson RJ., Swanson V., Wallace LA. Controlled comparison of pharmacological and psychological treatment of generalized anxiety disorder in primary care. Br J Gen Pract. 1990;40(336):289–294. [PMC free article] [PubMed] [Google Scholar]
- 68.Watanabe N., Churchill R., Furukawa TA. Combined psychotherapy plus benzodiazepines for panic disorder. Cochrane Database Syst Rev. 2009;(1):CD005335. doi: 10.1002/14651858.CD005335.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kampman M., Keijsers GP., Hoogduin CA., Hendriks GJ. A randomized, double-blind, placebo-controlled study of the effects of adjunctive paroxetine in panic disorder patients unsuccessfully treated with cognitivebehavioral therapy alone. J Clin Psychiatry. 2002;63(9):772–777. doi: 10.4088/jcp.v63n0904. [DOI] [PubMed] [Google Scholar]
- 70.Simon NM., Otto MW., Worthington JJ., et al Next-step strategies for panic disorder refractory to initial pharmacotherapy: a 3-phase randomized clinical trial. J Clin Psychiatry. 2009;70(11):1563–1570. doi: 10.4088/JCP.08m04485blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Roy-Byrne P., Craske MG., Sullivan G., et al Delivery of evidence-based treatment for multiple anxiety disorders in primary care: a randomized controlled trial. JAMA. 19 2010;303(19):1921–1928. doi: 10.1001/jama.2010.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hinton DE., Chhean D., Pich V., Safren SA., Hofmann SG., Pollack MH. A randomized controlled trial of cognitive-behavior therapy for Cambodian refugees with treatment-resistant PTSD and panic attacks: a cross-over design. J Trauma Stress. 2005;18(6):617–629. doi: 10.1002/jts.20070. [DOI] [PubMed] [Google Scholar]
- 73.Simpson HB., Foa EB., Liebowitz MR., et al Cognitive-behavioral therapy vs risperidone for augmenting serotonin reuptake inhibitors in obsessive-compulsive disorder: a randomized clinical trial. JAMA Psychiatry. 2013;70(11):1190–1199. doi: 10.1001/jamapsychiatry.2013.1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sulkowski ML., Geller DA., Lewin AB., et al The future of D-cycloserine and other cognitive modifiers in obsessive-compulsive and related disorders. Curr Psychiatry Rev. 2014;10(4):317–324. doi: 10.2174/1573400510666140619224942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hofmann SG., Smits JA., Rosenfield D., et al D-Cycloserine as an augmentation strategy with cognitive-behavioral therapy for social anxiety disorder. Am J Psychiatry. 2013;170(7):751–758. doi: 10.1176/appi.ajp.2013.12070974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.de Kleine RA., Hendriks GJ., Kusters WJ., Broekman TG., van Minnen A. A randomized placebo-controlled trial of D-cycloserine to enhance exposure therapy for posttraumatic stress disorder. Biol Psychiatry. 2012;71(11):962–968. doi: 10.1016/j.biopsych.2012.02.033. [DOI] [PubMed] [Google Scholar]
- 77.Smits JA., Rosenfield D., Otto MW., et al D-cycloserine enhancement of fear extinction is specific to successful exposure sessions: evidence from the treatment of height phobia. Biol Psychiatry. 2013;73(11):1054–1058. doi: 10.1016/j.biopsych.2012.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Pande AC., Davidson JR., Jefferson JW., et al Treatment of social phobia with gabapentin: a placebo-controlled study. J Clin Psychopharmacol. 1999;19(4):341–348. doi: 10.1097/00004714-199908000-00010. [DOI] [PubMed] [Google Scholar]
- 79.Pande AC., Pollack MH., Crockatt J., et al Placebo-controlled study of gabapentin treatment of panic disorder. J Clin Psychopharmacol. 2000;20(4):467–471. doi: 10.1097/00004714-200008000-00011. [DOI] [PubMed] [Google Scholar]
- 80.Lydiard RB., Rickels K., Herman B., Feltner DE. Comparative efficacy of pregabalin and benzodiazepines in treating the psychic and somatic symptoms of generalized anxiety disorder. Int J Neuropsychopharmacol. 2010;13(2):229–241. doi: 10.1017/S1461145709990460. [DOI] [PubMed] [Google Scholar]
- 81.Feltner DE., Crockatt JG., Dubovsky SJ., et al A randomized, doubleblind, placebo-controlled, fixed-dose, multicenter study of pregabalin in patients with generalized anxiety disorder. J Clin Psychopharmacol. 2003;23(3):240–249. doi: 10.1097/01.jcp.0000084032.22282.ff. [DOI] [PubMed] [Google Scholar]
- 82.Kasper S., Herman B., Nivoli G., et al Efficacy of pregabalin and venlafaxine-XR in generalized anxiety disorder: results of a double-blind, placebo-controlled 8-week trial. Int Clin Psychopharmacol. 2009;24(2):87–96. doi: 10.1097/yic.0b013e32831d7980. [DOI] [PubMed] [Google Scholar]
- 83.Raskind MA., Peterson K., Williams T., et al A trial of prazosin for combat trauma PTSD with nightmares in active-duty soldiers returned from Iraq and Afghanistan. Am J Psychiatry. 2013;170(9):1003–1010. doi: 10.1176/appi.ajp.2013.12081133. [DOI] [PubMed] [Google Scholar]
- 84.Raskind MA., Peskind ER., Kanter ED., et al Reduction of nightmares and other PTSD symptoms in combat veterans by prazosin: a placebo-controlled study. Am J Psychiatry. 2003;160(2):371–373. doi: 10.1176/appi.ajp.160.2.371. [DOI] [PubMed] [Google Scholar]
- 85.Eisenberg DM., Davis RB., Ettner SL., et al Trends in alternative medicine use in the United States, 1990-1997: results of a follow-up national survey. JAMA. 1998;280(18):1569–1575. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 86.Roy-Byrne PP., Bystritsky A., Russo J., Craske MG., Sherbourne CD., Stein MB. Use of herbal medicine in primary care patients with mood and anxiety disorders. Psychosomatics. 2005;46(2):117–122. doi: 10.1176/appi.psy.46.2.117. [DOI] [PubMed] [Google Scholar]
- 87.Sarris J., Mclntyre E., Camfield DA. Plant-based medicines for anxiety disorders, part 2: a review of clinical studies with supporting preclinical evidence. CNS Drugs. 2013;27(4):301–319. doi: 10.1007/s40263-013-0059-9. [DOI] [PubMed] [Google Scholar]
- 88.Sarris J., Panossian A., Schweitzer I., Stough C., Scholey A. Herbal medicine for depression, anxiety and insomnia: a review of psychopharmacology and clinical evidence. Eur Neuropsychopharmacol. 2011;21(12):841–860. doi: 10.1016/j.euroneuro.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 89.Milrod B., Leon AC., Busch F., et al A randomized controlled clinical trial of psychoanalytic psychotherapy for panic disorder. Am J Psychiatry. 2007;164(2):265–272. doi: 10.1176/ajp.2007.164.2.265. [DOI] [PubMed] [Google Scholar]
- 90.Leichsenring F., Salzer S., Jaeger U., et al Short-term psychodynamic psychotherapy and cognitive-behavioral therapy in generalized anxiety disorder: a randomized, controlled trial. Am J Psychiatry. 2009;166(8):875–881. doi: 10.1176/appi.ajp.2009.09030441. [DOI] [PubMed] [Google Scholar]
- 91.Leichsenring F., Salzer S., Beutel ME., et al Psychodynamic therapy and cognitive-behavioral therapy in social anxiety disorder: a multicenter randomized controlled trial. Am J Psychiatry. 2013;170(7):759–767. doi: 10.1176/appi.ajp.2013.12081125. [DOI] [PubMed] [Google Scholar]
- 92.Markowitz JC., Lipsitz J., Milrod BL. Critical review of outcome research on interpersonal psychotherapy for anxiety disorders. Depress Anxiety. 2014;31(4):316–325. doi: 10.1002/da.22238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Markowitz JC., Petkova E., Neria Y., et al Is exposure necessary? A randomized clinical trial of interpersonal psychotherapy for PTSD. Am J Psychiatry. 2015;172(5):430–440. doi: 10.1176/appi.ajp.2014.14070908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Segal ZV., Bieling P., Young T., et al Antidepressant monotherapy vs sequential pharmacotherapy and mindfulness-based cognitive therapy, or placebo, for relapse prophylaxis in recurrent depression. Arch Gen Psychiatry. 2010;67(12):1256–1264. doi: 10.1001/archgenpsychiatry.2010.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Arch JJ., Ayers CR., Baker A., Almklov E., Dean DJ., Craske MG. Randomized clinical trial of adapted mindfulness-based stress reduction versus group cognitive behavioral therapy for heterogeneous anxiety disorders. Behav Res Ther. 2013;51(4-5):185–196. doi: 10.1016/j.brat.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 96.Broocks A., Bandelow B., Pekrun G., et al Comparison of aerobic exercise, clomipramine, and placebo in the treatment of panic disorder. Am J Psychiatry. 1998;155(5):603–609. doi: 10.1176/ajp.155.5.603. [DOI] [PubMed] [Google Scholar]
- 97.Bartley CA., Hay M., Bloch MH. Meta-analysis: aerobic exercise for the treatment of anxiety disorders. Prog Neuropsychopharmacol Biol Psychiatry. 2013;45:34–39. doi: 10.1016/j.pnpbp.2013.04.016. [DOI] [PubMed] [Google Scholar]
- 98.Jayakody K., Gunadasa S., Hosker C. Exercise for anxiety disorders: systematic review. Br J Sports Med. 2014;48(3):187–196. doi: 10.1136/bjsports-2012-091287. [DOI] [PubMed] [Google Scholar]
- 99.Pollack MH., Van Ameringen M., Simon NM., et al A double-blind randomized controlled trial of augmentation and switch strategies for refractory social anxiety disorder. Am J Psychiatry. 2014;171(1):44–53. doi: 10.1176/appi.ajp.2013.12101353. [DOI] [PubMed] [Google Scholar]
- 100.van Balkorn AJ., de Beurs E., Koele P., Lange A., van Dyck R. Long-term benzodiazepine use is associated with smaller treatment gain in panic disorder with agoraphobia. J Nerv Ment Dis. 1996;184(2):133–135. doi: 10.1097/00005053-199602000-00015. [DOI] [PubMed] [Google Scholar]
- 101.Fava GA., Grandi S., Belluardo P., et al Benzodiazepines and anxiety sensitivity in panic disorder. Prog Neuropsychopharmacol Biol Psychiatry. 1994;18(7):1163–1168. doi: 10.1016/0278-5846(94)90118-x. [DOI] [PubMed] [Google Scholar]
- 102.Mellman TA., Byers PM., Augenstein JS. Pilot evaluation of hypnotic medication during acute traumatic stress response. J Trauma Stress. 1998;11(3):563–569. doi: 10.1023/A:1024460814230. [DOI] [PubMed] [Google Scholar]
- 103.Risse SC., Whitters A., Burke J., Chen S., Scurfield RM., Raskind MA. Severe withdrawal symptoms after discontinuation of alprazolam in eight patients with combat-induced posttraumatic stress disorder. J Clin Psychiatry. 1990;51(5):206–209. [PubMed] [Google Scholar]
- 104.Rickels K., Downing R., Schweizer E., Hassman H. Antidepressants for the treatment of generalized anxiety disorder. A placebo-controlled comparison of imipramine, trazodone, and diazepam. Arch Gen Psychiatry. 1993;50(11):884–895. doi: 10.1001/archpsyc.1993.01820230054005. [DOI] [PubMed] [Google Scholar]
- 105.Pollack M., Kinrys G., Krystal A., et al Eszopiclone coadministered with escitalopram in patients with insomnia and comorbid generalized anxiety disorder. Arch Gen Psychiatry. 2008;65(5):551–562. doi: 10.1001/archpsyc.65.5.551. [DOI] [PubMed] [Google Scholar]
- 106.Pollack MH., Hoge EA., Worthington JJ., et al Eszopiclone for the treatment of posttraumatic stress disorder and associated insomnia: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2011;72(7):892–897. doi: 10.4088/JCP.09m05607gry. [DOI] [PubMed] [Google Scholar]
- 107.Depping AM., Komossa K., Kissling W., Leucht S. Second-generation antipsychotics for anxiety disorders. Cochrane Database Syst Rev. 2010;(12):CD008120. doi: 10.1002/14651858.CD008120.pub2. [DOI] [PubMed] [Google Scholar]
- 108.Dold M., Aigner M., Lanzenberger R., Kasper S. Antipsychotic augmentation of serotonin reuptake inhibitors in treatment-resistant obsessivecompulsive disorder: a meta-analysis of double-blind, randomized, placebo-controlled trials. Int J Neuropsychopharmacol. 2013;16(3):557–574. doi: 10.1017/S1461145712000740. [DOI] [PubMed] [Google Scholar]
- 109.LaLonde CD., Van Lieshout RJ. Treating generalized anxiety disorder with second generation antipsychotics: a systematic review and metaanalysis. J Clin Psychopharmacol. 2011;31(3):326–333. doi: 10.1097/JCP.0b013e31821b2b3f. [DOI] [PubMed] [Google Scholar]
- 110.Wang HR., Woo YS., Bahk WM. Atypical antipsychotics in the treatment of posttraumatic stress disorder. Clin Neuropharmacol. 2013;36(6):216–222. doi: 10.1097/WNF.0b013e3182aa365f. [DOI] [PubMed] [Google Scholar]
- 111.Krystal JH., Rosenheck RA., Cramer JA., et al Adjunctive risperidone treatment for antidepressant-resistant symptoms of chronic military service-related PTSD: a randomized trial. JAMA. 2011;306(5):493–502. doi: 10.1001/jama.2011.1080. [DOI] [PubMed] [Google Scholar]
- 112.Carey P., Suliman S., Ganesan K., Seedat S., Stein DJ. Olanzapine monotherapy in posttraumatic stress disorder: efficacy in a randomized, double-blind, placebo-controlled study. Hum Psychopharmacol. 2012;27(4):386–391. doi: 10.1002/hup.2238. [DOI] [PubMed] [Google Scholar]
- 113.Hirschmann S., Dannon PN., lancu I., Dolberg OT., Zohar J., Grunhaus L. Pindolol augmentation in patients with treatment-resistant panic disorder: A double-blind, placebo-controlled trial. J Clin Psychopharmacol. 2000;20(5):556–559. doi: 10.1097/00004714-200010000-00011. [DOI] [PubMed] [Google Scholar]
- 114.Stein MB., Sareen J., Hami S., Chao J. Pindolol potentiation of paroxetine for generalized social phobia: a double-blind, placebo-controlled, crossover study. Am J Psychiatry. 2001;158(10):1725–1727. doi: 10.1176/appi.ajp.158.10.1725. [DOI] [PubMed] [Google Scholar]
- 115.Stein MB., Liebowitz MR., Lydiard RB., Pitts CD., Bushnell W., Gergel I. Paroxetine treatment of generalized social phobia (social anxiety disorder): a randomized controlled trial. JAMA. 1998;280(8):708–713. doi: 10.1001/jama.280.8.708. [DOI] [PubMed] [Google Scholar]


