Abstract
Background
The present study aims to assess the knowledge and attitude about needle stick injuries and sharps disposal.
Methods
A self designed questionnaire of 15 questions was handed out to 200 participants including undergraduate students (group 1), postgraduate students (group 2), faculty members (group 3) and auxiliary staff members (group 4). The data was collected and analyzed using Chi square test.
Results
Sixty-one percent of total participants reported of experiencing needle stick injury and 25.5 % knew that there could be several causes for this. Only 22 % of total population studied got the source tested. Immunization status of group 4 was very low and they also lacked the knowledge of sharps disposal and hepatitis C being spread by needle stick injuries. 57 % participants confirmed that there was no reporting facility and 66 % were not familiar with the guidelines of reporting.
Conclusions
There is a definite scope of improvement in terms of reporting and prevention of needle stick injuries. There is a need to improve knowledge and awareness of dental health care workers about the post exposure protocol.
Keywords: Needle stick injuries (NSIs), Auxiliary staff, Post exposure protocol
Introduction
Needle stick injury (NSI) is a penetrating stab wound from a needle (or any other sharp object) which may result in blood borne infections such as AIDS, Hepatitis B and Hepatitis C [1]. The average risk for transmission after percutaneous exposure is approximately 0.3 %, 6–30 %, and 1.8 % for human immunodeficiency virus (HIV), hepatitis B and hepatitis C, respectively. Over 90 % of these infections occur in low-income countries and most are preventable [2].
Needle stick injuries can occur during usage or disposal of sharps [3]. It is important to dispose the sharps properly, otherwise they might get entangled in linen or garbage and can injure the health workers who encounter them unexpectedly [4]. In spite of published literature and training programmes to prevent these injuries, significant success has not been achieved in preventing needle stick injuries.
We conducted this study to assess the knowledge and awareness of dental health care workers towards needle stick injuries.
Materials and Methods
A cross-sectional survey was carried out among 200 dental health care workers. A structured, self administered questionnaire of 15 items was prepared by the authors that included questions on personal data, aetiology, risk factors, prevention and post exposure management. It also assessed the knowledge about sharps disposal and reporting of the injury to the concerned department and history of immunization status.
The questionnaire was distributed to the health care workers together with necessary instructions for completion. The purpose of study was explained to the participants and proper confidentiality was maintained in the collection and assessment of data.
Statistical Analysis
The data was analyzed with SPSS 17.0. The results were analyzed using Chi square test and p value (p < 0.05) was used to indicate the statistical significance.
Results
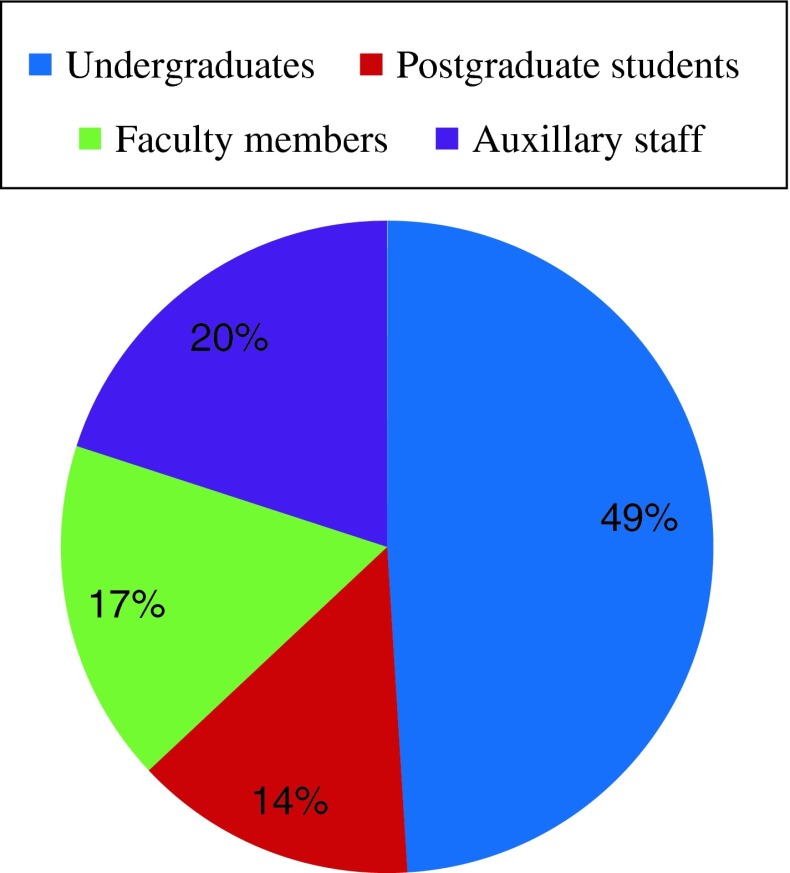
The sample size had 200 dental health care workers who were quantized into 4 groups (Fig. 1). Group 1 consisted of BDS undergraduate students (49 %), Group 2 consisted of postgraduate students (14 %), Group 3 consisted of postgraduate faculty members (17 %) and Group 4 consisted of auxiliary staff (20 %) which comprised of nurses, dental technicians, hygienists and housekeeping.
Fig. 1.
Quantization of sample
When a comparison was done among groups to analyze the immunization status it was found that Group 4 was least immunized (22.5 %), (p < 0.001) against Hepatitis B in comparison to other groups.
Majority of participants were aware of AIDS and Hepatitis B being spread by needle stick injuries (NSIs) (p < 0.001) but Group 4 did not have any knowledge of hepatitis C being spread by NSIs.
Over all 61 % of the participants had NSIs and study Group 3 reported the highest frequency (Fig. 2).
Fig. 2.
Frequency of NSIs
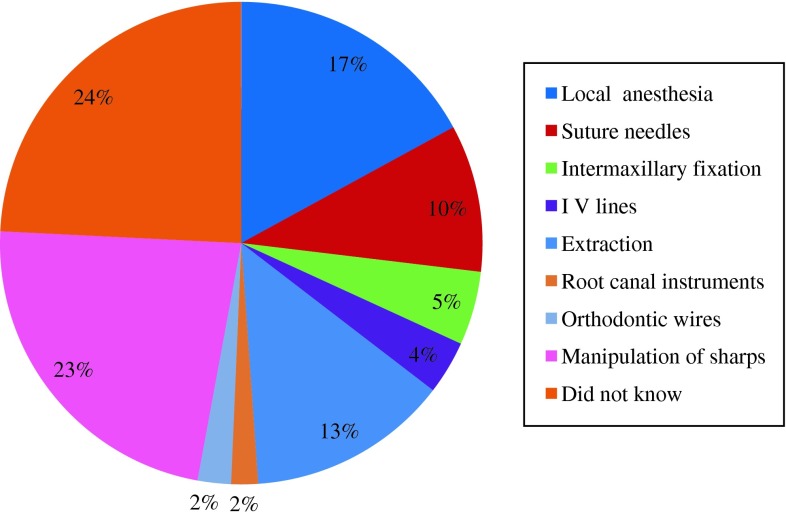
Various causes of NSIs were experienced by the dental health care workers in our study Groups which are illustrated in (Fig. 3). Only 25.5 % participants were aware of all these (p < 0.001). Among students, maximum number of NSIs were reported during extractions (p < 0.001) while in specialists suturing was the leading cause (p < 0.001).
Fig. 3.
Common causes of NSI
Although not statistically significant among groups but it was observed in our study that only 22 % of the participants got the source tested and among groups, Group 3 (35.3 %) was most proactive to get the tests done.
The incidence of NSIs was also compared amongst the participants. Maximum participants communicated to have it only once (p < 0.001) but a sizeable proportion of Group 3 respondents (41.2 %) experienced it more than twice (p < 0.01). Almost 42.5 % of all group participants reported bleeding after NSIs which indicates the severity of the injury.
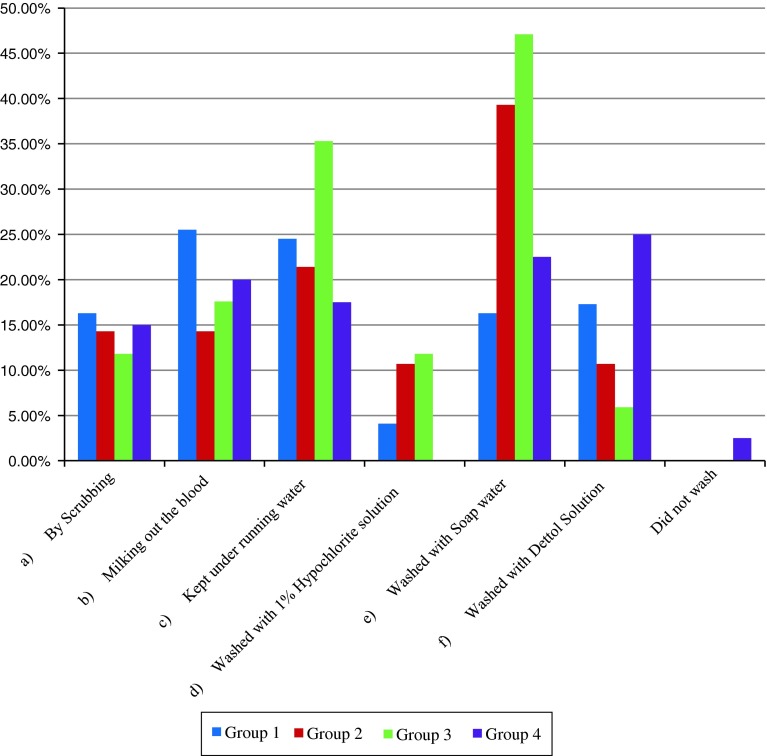
Majority of the participants did not know the ideal protocol to be followed after exposure. The steps followed by different participants are described in Fig. 4.
Fig. 4.
First aid steps followed
Significantly, Group 3 participants differed from Group 1 and Group 4 participants in practice of washing the wound with soap water (p < 0.001) post exposure while few participants in Group 4 did not even wash the wound.
There was a lack of knowledge regarding whom to contact post needle stick injury. There was a significant relationship between knowledge about contacting the concerned person and qualification of the participant. Group 4 participants (36 %) wanted to consult their friends (p < 0.001) while Group 1 (50 %) were in favour of consulting a pathologist (p < 0.001). The immunologist was suggested by Group 3 (32.4 %) (p < 0.001).
57 % of the participants communicated that there were no existing policies and procedures for reporting NSIs in the institute. Surprisingly 70 % of Group 3 respondents i.e. faculty members were also found to be ignorant of it. 66 % of the dental health workers were not familiar with the guidelines to report these injuries (Fig. 5).
Fig. 5.
Whom to contact
Knowledge about the disposal of sharps was also inadequate. Percentages obtained in the study revealed that Group 4 (57.5 %) participants confirmed throwing sharps in regular dust bins (p < 0.001). 55.9 % of Group 3 participants practiced burning the tip of needle and disposing sharps in sharps bin, which is highly significant (p < 0.001).
Discussion
Dental health care workers are exposed to blood borne virus infections in their professional work as they are in close contact with patient’s saliva and blood [5].These viruses are transmitted by NSIs. There have been several studies conducted in India and internationally which show that a large proportion of health care workers are prone to these viral infections [6].
In our study 61 % of participants experienced NSIs which is in accordance with a study conducted by Sharma et al. [7] who reported a rate of 79.5 %. The rate of exposure is high among faculty members and students (61.2 %) which are in contrast with a study conducted by Salzer et al. [8] who reported a rate of 34 %. This could be due to under reporting by the other groups or because of a small sample size of the study.
A variety of dental procedures carry the risk of NSIs such as administration of local anaesthesia, intermaxillary fixation, suturing, root canal treatment, manipulation of sharps and extractions. Specialists reported suturing as the main cause of NSIs as established by Hauman [9]. Bali et al. [10] observed a 23 % rate of NSIs during intermaxillary fixation in oral and maxillofacial surgeons and the observed rate in our study is 32.4 % among specialists. Extraction as the main cause was reported by students. This is explained by the fact that students are inexperienced and there is a lack of awareness in following universal precautions protocol by students in our institute.
Among auxiliary staff, manipulation of sharp objects has been found to be the leading cause of NSIs (32.5 %). The exposure prevention information network (EPInet) [11] study also reported an incidence of 42 % NSIs after use of needle and before its disposal. Many housekeeping staff members and technicians have reported manipulating sharps without wearing gloves. This group was found to be deficient in the knowledge of sharps disposing practices and this group was least immunized as well.
In this study, maximum participants experienced the event of one NSI (71.3 %) while a significant proportion of Group 3 i.e. faculty members (41.2 %) reported 2–5 incidents. Students had lesser years of experience but Group 3 participants had more experience which might be contributing for this.
Almost all participants were aware of AIDS and Hepatitis B being spread by NSIs but Group 4 was relatively unaware of Hepatitis C being spread by NSIs . This can be attributed to lack of knowledge and awareness of auxiliary staff towards Hepatitis C. This study is in accordance with the study conducted by Muralidhar et al. [12] except that in their study health care workers were aware of Hepatitis C as well.
It is surprising to note that in our study overall only 22 % of the participants got the source tested and among the individual groups this percentage was minimum in Group 4 (7.5 %) and maximum in Group 3 (35.3 %).This shows negligence and an indifferent attitude towards NSIs of the dental health care workers in our institute.
It is recommended that after accidental exposure the wound should be washed with soap and water and free bleeding encouraged [13]. The rationale behind such first aid measures is to reduce the bio burden below the threshold of infectious dose.
The risk of HIV transmission from patients to health care workers due to occupational NSIs has been reported to be about 0 .3 % by Tokars et al. [13]. Immediate induction of bleeding (squeezing wound carefully and rinsing with a large volume of water) followed by timely administration of post exposure prophylaxis further decreases this percentage [14].
In case of exposure to mucous membrane (mouth, nose, eyes) flush exposed surface with plenty of running water. Scrubbing is not recommended [1] since this may inoculate the virus into the tissues [15].
In our study most of the participants practiced these first aid steps except auxiliary staff, wherein only 17.5 % reported washing the wound with soap water. Although statistically not significant it was found that scrubbing after exposure was done by 16.3 % students and 15 % auxiliary staff which is a matter of concern.
Reporting of any NSIs is of paramount importance however the non reporting rate (66 %) was high in our study and even higher in experienced faculty members who were not aware of the policies and procedures of reporting NSIs.
Reasons for non reporting among students could be lack of knowledge of being at risk, shame, fear of consequences resulting from reporting or poor awareness of institutional reporting facilities [16]. Teachers and well experienced staff members play an important role in educating students however this study indicates that they also lacked the knowledge of reporting facilities and guidelines. This also has been reported by Makary et al. [17] who found an occupational non reporting rate of 51 %. Among specialists the other reason for not reporting may be fear of disciplinary action due to negligence. It is essential to ensure that the process of reporting should be simple including follow up.
There is always a dilemma as to whom we should report after NSIs. According to AOTEA pathology guidelines, general physician should be notified immediately who may choose microbiologist, clinical immunologist for further consultations. A key finding in our study shows that Group 4 participants did not know whom to contact and many of them reported that they contact their friends. This is reflective of a lack of knowledge and awareness among our auxillary staff.
Many NSIs occur due to improper disposal of sharps e.g. unsuitable bins or on the floor and incorrect disposal of instruments by the dentists on instrumental trays. Health care workers suffered injuries in the process of sorting and cleaning the instruments after use. Our study highlights the fact that auxiliary staff members were not aware that there were separate sharps bins for sharps disposal.
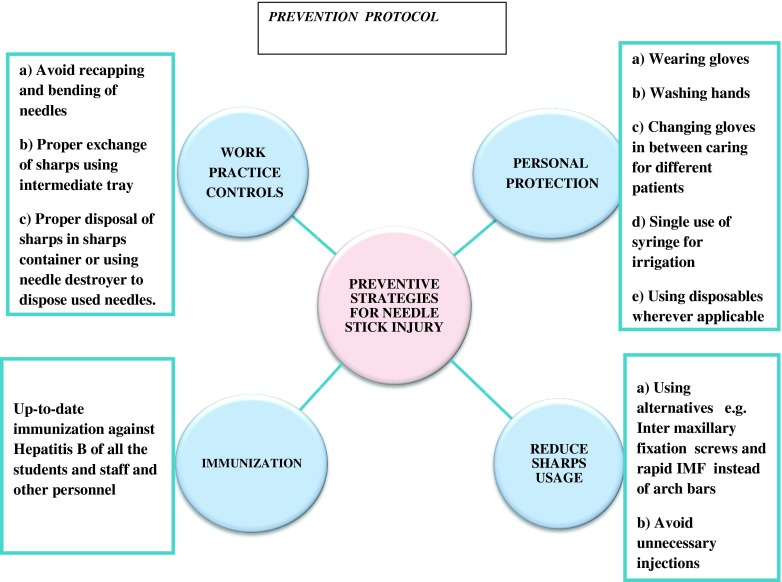
Prevention is better than cure. NSIs can be prevented by continued education, effective training, better safety devices, positive work environment and following standard precautions (Fig. 6). Induction programmes should be held for all new recruits. The concept of universal precautions should be explained to all health workers and steps should be taken to enforce them. Appropriate disposal of sharps and avoidance of recapping and bending should form an essential component of the training.
Fig. 6.
Prevention protocol
Conclusion
NSIs were observed in all groups among participants. There is much room for improvement in safety measures and preventive protocols. Reporting of NSIs should be mandatory. It is of utmost importance that our institution has a clear cut and uniform policy to report NSIs. There is a need for training all dental health care workers of our institute, especially auxillary staff in handling and disposal of sharps, and inculcating a responsible attitude among them.
References
- 1.Kapila K, Gupta RM, Chopra GS. Post-exposure prophylaxis: what every health care worker should know. Med J Armed Forces India. 2008;64:250–253. doi: 10.1016/S0377-1237(08)80106-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sangwan BR, Kotwal A, Verma BK. Occupational exposure to blood and body fluids amongst health care workers in a teaching hospital of the armed forces. Med J Armed Forces India. 2011;67:21–24. doi: 10.1016/S0377-1237(11)80006-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rodrigues C. Needle stick injuries and the health care worker—the time to act is now. Indian J Med Res. 2010;131:384–386. [PubMed] [Google Scholar]
- 4.Guruprasad Y, Chauhan DS. Knowledge, attitude and practice regarding risk of HIV infection through accidental needlestick injuries among dental students of Raichur, India. Nat J Maxillofac Surg. 2011;2:152–155. doi: 10.4103/0975-5950.94470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chopra SS, Pandey SS. Occupational hazards among dental surgeons. Med J Armed Forces India. 2007;63:23–25. doi: 10.1016/S0377-1237(07)80100-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singru SA, Banerjee A. Occupational exposure to blood and body fluids among health care workers in a teaching hospital in Mumbai, India. Indian J Community Med. 2008;33:26–30. doi: 10.4103/0970-0218.39239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sharma R, Rasania SK, Verma A, Singh S. Study of prevalence and response to needle stick injuries among health care workers in a tertiary care hospital in Delhi, India. Indian J Community Med. 2010;35:74–77. doi: 10.4103/0970-0218.62565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salzer HJF, Hoenigla M, Kessler HH et al (2011) Lack of risk-awareness and reporting behavior towards HIV infection through needle stick injury among European medical students. Int J Hyg Environ Health (in press) [DOI] [PubMed]
- 9.Hauman CHJ (1995) Infection control in the dental surgery. Dental Update 12–6
- 10.Bali R, Sharma P, Garg A. Incidence and patterns of needle stick injuries during I ntermaxillary fixation. Br J Oral Maxillofac Surg. 2011;49:221–224. doi: 10.1016/j.bjoms.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 11.International Health Care Workers Safety Center . Exposure prevention information network (EPI net) Data reports. Charlottesville: University of Virginia; 1999. [Google Scholar]
- 12.Muralidhar S, Singh PK, Jain RK, Malhotra M, Bala M. Needle stick injuries among health care workers in a tertiary care hospital of India. Indian J Med Res. 2010;131:405–410. [PubMed] [Google Scholar]
- 13.TokarsJI Marcus R, Culver DH, Schable CA, McKibben PS, Bandea CI, Bell DM. Surveillance of HIV infection and zidovudine use among health care workers after occupational exposure to HIV-infected blood. The CDC Cooperative Needle stick Surveillance Group. Ann Intern Med. 1993;118:913–919. doi: 10.7326/0003-4819-118-12-199306150-00001. [DOI] [PubMed] [Google Scholar]
- 14.Young TN, Arens FJ, Kennedy GE, Laurie JW, Rutherford G. Antiretro-viral post-exposure prophylaxis (PEP) for occupational HIV exposure. Cochrane Database Syst Rev. 2007;1:CD002835. doi: 10.1002/14651858.CD002835.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smith AJ, Cameron SO, Bagg J, Kennedy D. Management of needle stick injuries in general dental practice. Br Dent J. 2001;190:645–650. doi: 10.1038/sj.bdj.4801064. [DOI] [PubMed] [Google Scholar]
- 16.Raggam RB, Rossmann AM, Salzer HJF, Stauber RE, Kessler HH. Health care worker-to-patient transmission of hepatitis C virus in the health care setting: many questions and few answers. J Clin Virol. 2009;45:272–275. doi: 10.1016/j.jcv.2009.04.015. [DOI] [PubMed] [Google Scholar]
- 17.Makary MA, Al-Attar A, Holzmueller CG, Sexton JB, Syin D, Gilson MM, Sulkowski MS, Pronovost PJ. Needle stick injuries among surgeons in training. N Engl J Med. 2007;356:2693–2699. doi: 10.1056/NEJMoa070378. [DOI] [PubMed] [Google Scholar]