Abstract
Introduction
Demonstrations and training on live-subjects are not always the optimal means of introducing the students to minor oral surgery. Hence, the use of teaching models permit the students to handle the surgical instruments in a limited field under a semi-realistic circumstance and also helps in developing psychomotor skills in an non stressed situation. One among the competent exercise in oral surgery is suturing. Though there exist a variety of commercially available suturing training models, cost factor restrain their acquirement in few units.
Methods & Materials
This paper describes the construction of a simple and cost-effective suturing model for preclinical training. The construction of this model requires an orange peel, putty impression material and plaster of paris. This suturing model can be created in ten minutes.
Conclusion
This model can be constructed by the students with minimal effort and low cost in order to practice suturing.
Keywords: Suturing technique, Training model, Surgical skill, Affordable
Introduction
Sutures are an essential requirement for optimal healing following various surgical procedures [1]. Improperly placed sutures, besides causing delayed healing, also results in more damage to the tissue. Hence, a proper suturing technique is an important skill for any surgeon [2]. The high degree of psychomotor skills required to expertise in intraoral suturing, and the lack of patients willing to have oral surgery procedures performed by students have made it necessary to find alternatives to prepare dental students for their future clinical work [3]. One possible solution to overcome this problem is the use of training models. Various self-made and commercial suturing models are available. Self-made suturing models mostly lack the imitation of human tissue while, commercially available suturing models though provide excellent tactile sensation, their acquirement to train on may be hindered by cost [4]. Herewith we demonstrate a suturing training model with affordability as the priority and which is easy to construct.
Technique
A fresh orange is cut into two segments from top to bottom. The pulp of the fruit is carefully removed thereby separating it from the rind (the thick orange colored outer skin) and mesocarp (the inner porous white tissue) of the fruit (Fig. 1). A thin layer of putty vinyl polysiloxane impression material is smeared on to the inner surface of the orange skin peel and the pulp space is filled with either plaster of paris or dental stone (Fig. 2). Subsequently, when the dental stone sets, the suture model is ready for use which can be incised similar to tissue and sutured (Fig. 3).
Fig. 1.
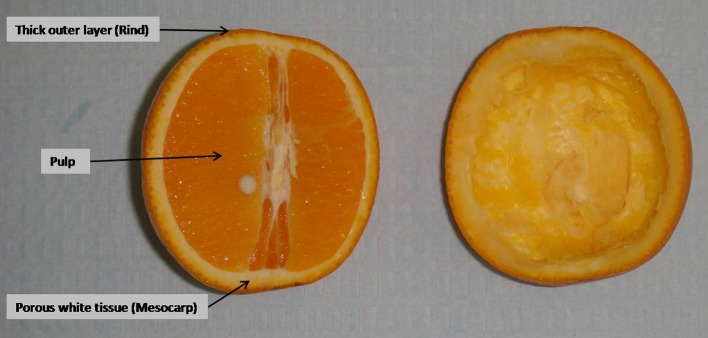
A fresh orange is cut and the pulp portion separated
Fig. 2.
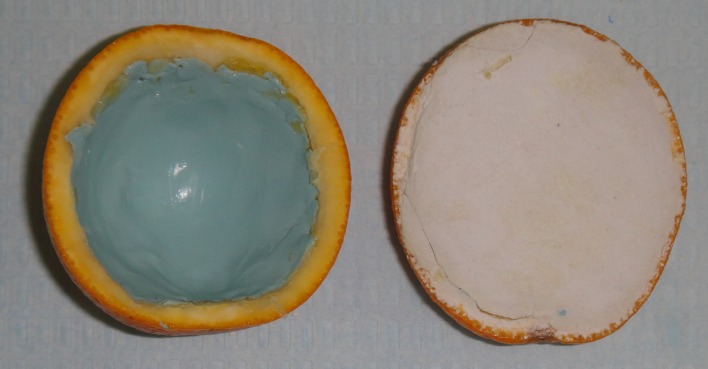
A thin layer of putty impression material smeared and plaster of paris filled
Fig. 3.
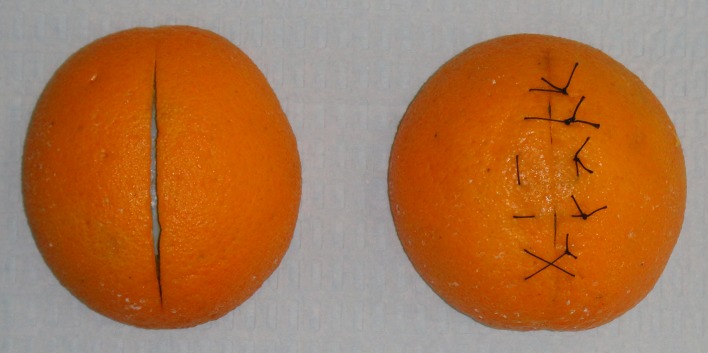
The gaping of the incised wound noted and sutures practiced
The orange peel replicates the human skin with an outer keratinized texture and a sub-cuticular layer (mesocarp). The keratinized nature of the outer skin layer offers suitable resistance to the passage of the surgical needle and its mild rubbery nature gives good tear strength thereby preventing the suture material from cutting through the incision margins while placing the knot. The basic principles of incision indicate that while giving an incision, skin should be stretched in a way that marked line of incision rests on a solid bone thereby providing a firm base for a clean incision. For this reason, a layer of putty impression material is smeared on the inner surface of the orange peel which mimics the bone. This reinforces the bony feel when an incision in placed. The plaster of paris or dental stone forms a firm base for the model.
The mesocarp layer of the orange peel is appropriate to practice subcuticular sutures. As the cut orange possess a curved outer surface, minimal dissection following an incision will make the incised wound to gape (Fig. 3). This gapping aid in understanding of wound tension and the need for adequate tissue bites to avoid a potential dead space. This model even though being of low fidelity, will expedite the training of sutures in cases requiring a multiple layer approach as it mimics the human skin and underlying tissues; with the colored surface of the peel acting as the epidermis, the white portion below being similar to the subcutaneous cellular tissue and if an adequate layer of fruit pulp is retained comparing it to muscle layer and the smear of putty impression material resembling the bone.
The detrimental aspect of this model is that it cannot be stored for several days. In 2 or 3 days the skin gets dried and loses its resilient nature. However, the deficiencies of the described model are compensated for by the simple production, low cost and the possibility of mass production offering identical surgical procedures to the students. This model can be constructed by the students with minimal effort in order to practice suturing at their residence.
References
- 1.Hupp JR, Ellis E, Tucker MR (2008) Contemporary Oral and Maxillofacial Surgery, fifth edn. Mosby Elsevier
- 2.Weaver JM, Lu M, McCloskey KL, Herndon ES, Tanaka W. Digital multimedia instruction enhances teaching oral and maxillofacial suturing. J Calif Dent Assoc. 2009;37(12):859–862. [PubMed] [Google Scholar]
- 3.Stelzle F, Farhoumand D, Neukam FW, Nkenke E. Implementation and validation of an extraction course using mannequin models for undergraduate dental students. Acta Odontol Scand. 2011;69:80–87. doi: 10.3109/00016357.2010.517560. [DOI] [PubMed] [Google Scholar]
- 4.Uppal N, Saldanha S. Low-cost suturing training model for use in developing nations. Br J Oral Maxillofac Surg. 2012;50:e13–e14. doi: 10.1016/j.bjoms.2011.07.004. [DOI] [PubMed] [Google Scholar]


