Abstract
Purpose
The present study was carried out to evaluate the usefulness of mini retromandibular approach on accessibility, scarring and stability in open reduction and internal fixation of sub condylar fractures.
Materials and Methods
Fifteen patients underwent open reduction and rigid fixation of middle and low subcondylar fractures, with mini-retro mandibular approach.
Results
No signs of infection were observed in any patient postoperatively. Surgical scar was imperceptible and esthetically acceptable in all the cases. Out of 15 patients, only one patient had discrepancy in occlusion and after 2 months satisfactory centric occlusion was achieved. Salivary fistula (parotid fistula) was observed in 3 cases within 1 week postoperatively, which was treated spontaneously with the use of hypertonic saline. Transient facial nerve weakness was observed in 2 patients, in one patient it resolved in 4 weeks postoperatively and in second patient 3 months postoperatively. Mouth opening increased in all the patients with time. Average mouth opening at 1 week interval was 19.6 mm, at 2 months interval 28.2 mm, and after 6 months 38.33 mm suggesting that mouth opening gradually increased with time. At the end of 2 months postoperatively none of the patients had any restriction in lateral movements. At 2 months postoperatively 4 patients had deviation but none of the patients had any deviation 6 months postoperatively.
Conclusion
It is evident from the results of our study that open reduction and internal fixation using mini-retromandibular approach is good treatment option in management of mandibular condylar fractures.
Keywords: Condylar fracture, Open reduction and rigid fixation, Mini-retromandibular approach, Anatomical reduction
Introduction
Condylar fractures are one of the most frequent site of fractures, accounting for at least one-third (26–40 %) of all mandibular fractures [1]. They can lead to anatomical and functional impairment when undiagnosed or incorrectly treated [2, 3]. Intracapsular condylar fractures can result into ankylosis if not treated with intense rehabilitation [4, 5]. Undiagnosed or incorrectly treated condylar fractures can lead to severe functional impairment, including malocclusion, reduced mouth opening associated with deviation of jaw and limited lateral mandibular movements [2, 3]. A number of reports have suggested that the treatment of condylar fractures by open reduction and rigid fixation offers much better anatomic results [6–13]. Conservative treatment is still the choice of treatment for intracapsular or comminuted fractures and fractures in pediatric patients [14, 15]. Though closed reduction is a simple and easy method of treatment of condylar fractures but long-term complications like pain, arthritis, open bite, inadequate restoration of vertical height of the ramus leading to malocclusion and ankylosis do exist with closed reduction method [16]. A number of approaches to condylar fracture are reported which can be divided into intraoral and extraoral techniques. Intraoral approach is technically demanding when treating high or medially displaced fractures and can lead to poor results in terms of anatomic reduction [13, 17, 18]. Extraoral approaches simplify the management of condylar fractures but are still associated with some unresolved issues. Many of the extraoral approaches can become technically demanding and present definite risks of facial nerve injury and unpleasant scarring [19–23]. Open reduction and rigid fixation allows good anatomic repositioning, restoration of the ramal length, avoidance of long term sequelae like clicking and late arthritic changes and an earlier return to normal function without the need for inter maxillary fixation [24, 25].
The present study was conducted on patients, with mandibular condylar fractures and were treated by open reduction and internal fixation. All patients were treated with mini-retromandibular approach. Retromandibular approach was preferred because of the following advantages: This approach exposes the entire ramus from behind the posterior border. The distance from skin incision to the area of interest is reduced in comparison to that of the submandibular approach [26]. It is found to be minimally invasive, provides good access and allows direct visual alignment of the fracture fragments [27]. Mini-retromandibular approach is useful for procedures involving the area on or near the condylar neck and the ramus itself. Subcondylar fractures, especially low level, are simple to reduce and stabilize with a bone plate via retromandibular approach. Scar produced is in less conspicuous location and good cosmetic result is achieved with this approach. The present study was carried out to evaluate the usefulness of mini-retromandibular approach associated with open reduction and internal fixation of condylar fractures.
Patients and Methods
This institutionally approved study was done on a sample size of 15 male patients with subcondylar fractures in the age group of 18–50 years who reported to the department of oral and maxillofacial surgery. Informed consent was taken from all the patients involved in the study, who underwent open reduction and rigid fixation with mini-retromandibular approach. Among these, 13 patients presented with unilateral and 2 with bilateral condylar fractures. The 15 condylar fractures consisted of 8 middle neck fractures, 7 low neck subcondylar fractures. In all the cases patients presented with associated fractures of the facial bones (symphyseal, angle and mandibular body fractures) (Fig. 3). The average duration of surgery was 34 min (range 25–50 min) for each condylar procedure. Selection criteria—patients in the age group of 18 years or more irrespective of sex, religion and socioeconomic status and were medically fit for surgery under general anesthesia. Patients having extracapsular unilateral/bilateral condylar fractures with one or more of the following presentations—difficulty of obtaining adequate occlusion by closed reduction, displaced/dislocated condylar fractures, shortening of ramus height associated with molar premature contact, unilateral/bilateral condylar fractures associated with other fractures, unilateral/bilateral condylar fractures where maxillomandibular fixation is not recommended for medical reasons e.g. seizure disorders, undisplaced condylar fractures in which patient was not willing for closed reduction with 4 weeks of maxillomandibular fixation.
Fig. 3.

Opg showing right subcondylar fracture
Exclusion criteria were—intracapsular condylar fractures and medically compromised patients who were not fit for general anesthesia. Patients less than 18 years of age were not included.
Surgical Technique
The surgery was performed under general anesthesia with nasotracheal intubation. Maxillomandibular fixation was done and the other associated fractures of mandible (Fig. 1) were treated first with intraoral approach to achieve continuity of mandibular arch. Pre operative intra oral derangement of occlusion is shown in Fig. 2. Extraoral surgical site was prepared to approach the condylar fracture (Fig. 3). A preoperative drawing was marked as shown in Fig. 4.
Fig. 1.

Restricted pre op mouth opening
Fig. 2.

Pre op intraoral
Fig. 4.

Incision marking
For marking the angle of mandible, zygomatic arch, a 20 mm skin incision line was drawn 2 cm posterior to angle of mandible on the side of surgery (Fig. 4). The vertical vector of incision was dependent on the fracture site and elasticity of skin which varied from patient to patient. The incision line was infiltrated with local anaesthetic containing adrenaline (1:200000) or freshly prepared 1:200000 adrenaline. Incision was placed on skin and dissection was carried through subcutaneous tissues superficial to the superficial muscular aponeurotic system (SMAS) and parotid capsule, incision was placed through SMAS layer and parotid capsule, facial nerve identified and protected with retractor, dissecting in anteromedial direction towards posterior border of mandible. Pterygomassetric sling was identified and dissected. Masseter muscle was stripped from lateral surface of mandible upwards to visualize fractured condyle (Fig. 5). Fracture was reduced under direct vision and rigid fixation done with L-shape titanium mini plates (2 mm) or 4 hole with gap and 2 hole with gap (2 mm) plates and 6–8 mm screws (Fig. 6). Maxillomandibular fixation was released and occlusion checked. Wound was closed in layers. Deeper muscles and facia were closed with 3–0 vicryl and subcuticular closure of skin was done with 4–0 proline. Intraoral wound was closed with 3–0 mersilk interrupted sutures.
Fig. 5.
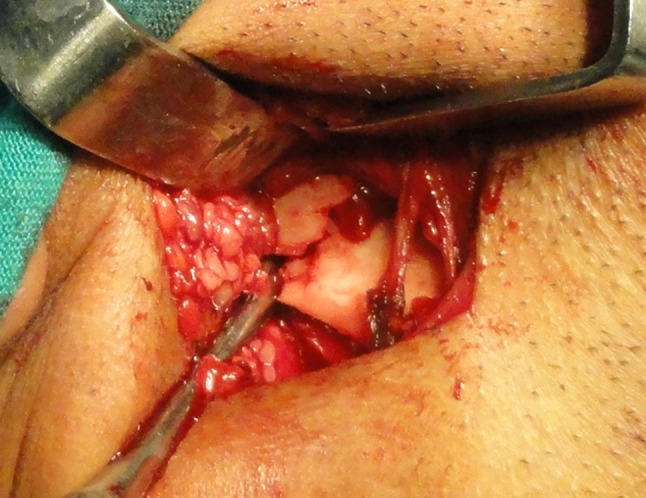
Exposure of the fracture site
Fig. 6.

Rigid fixation and internal fixation
Results
Good results were achieved in all patients. Postoperatively all the patients were clinically assessed for presence of infection at operative site, signs of Frey’s syndrome, salivary fistula formation, facial nerve palsy, postoperative scar, discrepancy in occlusion, TMJ examination in the form of maximum mouth opening (Table 1), restriction in lateral movements, pain in preauricular region, and deviation of jaw at the intervals of 24 h, 1 week, 2 and 6 months postoperatively (Fig. 7). Radiographically, the approximation of fracture fragments, plate fracture and screw loosening on orthopantamogram were evaluated at intervals of 24 h, 2 and 6 months postoperatively (Fig. 8). During clinical assessment, none of the patients developed postoperative infection, Frey’s syndrome or hypertrophic scar. Surgical scar was imperceptible and esthetically acceptable in all the cases after 6 months (Fig. 9). Out of 15 patients, only one patient had discrepancy in occlusion after 24 h and 1 week postoperatively, which gradually reduced and after 2 months satisfactory centric occlusion was achieved. Salivary fistula (parotid fistula) was observed in three cases within 1 week postoperatively, which was treated spontaneously with the use of hypertonic saline. Transient facial nerve weakness was observed in 2 patients, which resolved after 3 months postoperatively. Mouth opening increased in all the patients with time. Average mouth opening at 1 week interval was 19.6 mm, at 2 months interval 28.2 mm, and after 6 months 38.33 mm suggesting that mouth opening gradually increased with time (Table 1) (Figs. 1, 7). All fifteen patients had restricted laterotursive movements after 1 week interval but after 2 and 6 months interval none had any restriction in lateral movements. Six patients had preauricular tenderness postoperatively but none of the patients had preauricular tenderness 6 months postoperatively (Table 2). Eight patients had deviation on mouth opening towards the operated joint side but none of the patients had any deviation 6 months postoperatively. On radiographic assessment, the approximation of fracture fragments, plate fracture and screw loosening were evaluated in all cases, the radiographs revealed proper approximation of fracture fragments with good bone healing. No evidence of plate exposure, and screw loosening at fracture site was observed. Evaluation of surgical scar was done at 3 and 6 months post-operatively (Fig. 9).
Table 1.
Maximum mouth opening
| Sl. no. | 1 week (in mm) | 2 months (in mm) | 6 months (in mm) |
|---|---|---|---|
| 1 | 18 | 24 | 35 |
| 2 | 17 | 28 | 37 |
| 3 | 14 | 20 | 30 |
| 4 | 28 | 38 | 44 |
| 5 | 18 | 25 | 37 |
| 6 | 19 | 26 | 37 |
| 7 | 20 | 28 | 38 |
| 8 | 22 | 29 | 40 |
| 9 | 17 | 30 | 37 |
| 10 | 20 | 30 | 40 |
| 11 | 21 | 32 | 42 |
| 12 | 18 | 27 | 39 |
| 13 | 22 | 30 | 38 |
| 14 | 19 | 27 | 40 |
| 15 | 21 | 29 | 41 |
| Mean | 19.6 | 28.2 | 38.33 |
Fig. 7.

Six months post op mouth opening
Fig. 8.

6 months post op OPG
Fig. 9.

Six months post op scar
Table 2.
Preauricular tenderness
| Sl. no. | 1 week | 2 months | 6 months |
|---|---|---|---|
| 1 | 1 | 0 | 0 |
| 2 | 1 | 0 | 0 |
| 3 | 2 | 0 | 0 |
| 4 | 0 | 0 | 0 |
| 5 | 7 | 3 | 0 |
| 6 | 0 | 0 | 0 |
| 7 | 7 | 5 | 0 |
| 8 | 1 | 0 | 0 |
| 9 | 0 | 0 | 0 |
| 10 | 8 | 5 | 0 |
| 11 | 1 | 0 | 0 |
| 12 | 7 | 3 | 0 |
| 13 | 0 | 0 | 0 |
| 14 | 1 | 0 | 0 |
| 15 | 0 | 0 | 0 |
0–3 minimal pain, 4–6 moderate pain, 7–10 severe pain
Discussion
Many studies have reported that surgical treatment with open reduction and rigid fixation leads to significantly better results than conservative management of condylar fractures [6–13]. With the exception of undisplaced, intracapsular fractures and fractures in pediatric patients younger than 12 years of age [14–15], most mandibular condylar fractures should be treated with open reduction and rigid fixation. Points to be clarified regarding surgical treatment, is how many fixation devices should be used [6], and the choice of approach for treating condylar fractures. The ideal surgical approach should be the least invasive method available, allow comfortable and easy solution to the surgical problem, be versatile, allow satisfactory vision, have the lowest rate of surgical complications, and be easily performed. In the past, condylar fractures have been treated solely by closed reduction for various reasons like; surgical procedures in the TMJ area were associated with complications involving the facial nerve, technical problems in manipulating the fracture fragments into good anatomical reduction and visible scar at the site of surgery. So reasonably good results have been achieved with conservative treatment [15]. Though closed reduction is a simple and easy method of treatment for condylar fractures but results were not satisfactory in all cases. Long-term complications like pain, arthritis, open bite, deviation of the mandible on opening and closing movement, inadequate restoration of vertical height of the ramus leading to the malocclusion and ankylosis do exist with closed reduction method [13]. Use of closed treatment methods have not been able to provide satisfactory and uncomplicated results for all types of condylar fractures; simultaneously, on the other hand, with advancement of radiographic techniques, anesthesia and use of antibiotics to control infection, surgical techniques have also been continuously refined thereby overcoming most of the potential complications of surgery and providing solutions where closed treatment failed. Open reduction and rigid fixation allows good anatomic repositioning, restoration of the ramal length, avoidance of long term sequalae like clicking and late arthritic changes and an earlier return to normal function without the need for inter maxillary fixation [24]. The approach we have used differs significantly from classic submandibular and retromandibular approaches. The skin incision is limited to 20 mm and hidden behind the angle of mandible. The dissection plane towards the fracture is superficial to the superficial muscular aponeurotic system, instead of deep to this structure. When the dissection is superficial the skin access can be placed under traction, so the fractures at any level from condylar head to subcondylar area can be accessed, which may not be done with other approaches. Advantage of mini-retromandibular technique is that the correct reduction of the fracture and positioning of the fixation devices are easily checked intraoperatively, for these reasons, the maxillomandibular fixation can be removed at the end of the procedure [28]. The ease of the access was demonstrated by the average operative time of 34 min. The mini-retromandibular technique should be considered a relatively simple procedure. The present study was carried out to evaluate the morbidity associated with open reduction and internal fixation of condylar fractures. Presence or absence of infection, sinus or fistula or dehiscence at the operation site was recorded at intervals of 1 week, 2 and 6 months postoperatively and was found absent in all the cases. Salivary fistula formation was another anticipated complication associated with open reduction and internal fixation especially with retromandibular approach. Salivary fistula formation recorded at intervals of 1 week, 2 and 6 months postoperatively and in the first week post-operatively occurred in three patients (20 %). The presence of salivary fistula in our cases is attributed to failure to achieve watertight closure of the parotid capsule. After placing horizontal mattress sutures watertight closure was achieved and no such complication was encountered. Salivary fistula was managed conservatively by means of hot hypertonic (3 %) saline [29, 30] which was injected in the fistulous tract. Complete closure of the fistula was achieved in 3–5 days without any morbidity of facial nerve. Frey’s syndrome was assessed at intervals of 2 and 6 months postoperatively and was found absent in all the cases, which correlates with the findings of Ellis et al. [21]. Facial nerve and its branches are at risk while using retromandibular approach for open reduction and internal fixation, damage to which may cause weakness of facial muscles. Transient facial nerve weakness was seen in two patients, which resolved within 3 months postoperatively. Manisali et al. [22], Ellis et al. [21] and Delvin et al. [31] also recorded transient facial nerve weakness postoperatively. Hyde et al. [32] observed no weakness of facial nerve in any of the patients in their study. The facial nerve weakness in our study can be attributed to relatively more stretching of the soft tissues, as the length of the incision was small and there were relatively more chances for excessive stretching of the nerve fibers and hence increased chances of transient facial nerve weakness. Surgical scar was imperceptible in all the cases which is similar with the findings of Ellis et al. [21] and Delvin et al. [31] who opined that retromandibular approach seems to give the benefit of good cosmesis and adequate exposure. As the approach used was the mini-retromandibular so the scar was minimal and esthetically acceptable. Out of 15 patients, only one patient had transient malocclusion in the form of posterior open bite of 1.5 mm on operated side after 24 h and, 1 week postoperatively. After 2 and 6 months interval, all patients showed satisfactory centric occlusion. Malocclusion may be attributable to concomitant fractures and transient spasm of masticatory muscles. Mouth opening increased in all the patients with time (maximum of 44 mm, 6 months post-operatively). This is compatible with the findings of Hyde et al. [32]. After 1 week post-operatively, mouth opening was relatively less, which can be attributed to trauma to the soft tissues during surgery. However trismus reduced with the passage of time. All 15 patients had restricted laterotursive movements after 1 week interval but after 2 and 6 months interval, none of the patients had any restriction in lateral movements, similar to the findings of Iannetti et al. [33]. Initial restriction in lateral movements is attributable to the swelling and edema after surgery owing to stripping of the tissues during surgery. Four patients had preauricular tenderness at 1-week interval and two patients at 2 months interval but none of the patients had preauricular tenderness 6 months postoperatively which correlates with the findings of Widmark et al. [34]. Initial tenderness is attributed to retraction of soft tissues during surgery. Deviation on mouth opening towards the operated joint side after 1 week was seen in six cases, after 2 months postoperatively 4 patients had deviation but none had any deviation at 6 months postoperatively. This is consistent with the findings of Sugiura et al. [35] and Villarreal et al. [36].
The approximation of fracture fragments, plate fracture and screw loosening on radiographs (OPG) were evaluated at intervals of 24 h, 2 and 6 months postoperatively. In all cases, the radiographs revealed proper approximation of fracture fragments with good bone healing as shown by Choi et al. [37]. No evidence of plate exposure, and screw loosening at fracture site was observed but this is not compatible with the findings of Choi et al. [37]. The absence of plate fracture and screw loosening in our study may be due to the fact that most screws were placed vertically against the plate. The results of our study suggest that some transient complications are associated with open reduction and internal fixation of condylar fractures but in the long run there are better results in terms of functional rehabilitation and esthetics. We can conclude that among the extraoral routes, we suggest that the mini-retromandibular approach is ideal owing to its simple, speed, versatility, and freedom from the complications that are common with other extraoral approaches. Although the study was done on less number of patients an elaborate study should be done to achieve more conclusive results and statistics.
Contributor Information
J. K. Dayashankara Rao, Email: dsraojk@yahoo.com.
Neelima Gehlot, Email: gehlotneelima@yahoo.com.
Vijay Siwach, Email: vijay.siwach@gmail.com.
References
- 1.Ellis E, III, Dean J. Rigid fixation of mandibular condyle fractures. Oral Surg Oral Med Oral Pathol. 1993;76:6–15. doi: 10.1016/0030-4220(93)90285-C. [DOI] [PubMed] [Google Scholar]
- 2.Silvennoinen U, Iizuka T, Lindqvist C, Oikarinen K. Different patterns of condylar fractures: an analysis of 382 patients in a 3-year period. J Oral Maxillofac Surg. 1992;50:1032–1037. doi: 10.1016/0278-2391(92)90484-H. [DOI] [PubMed] [Google Scholar]
- 3.Zachariades N, Mezitis M, Mourouzis C, Papadakis D, Spanou A. Fractures of the mandibular condyle: a review of 466 cases. Literature review, reflections and proposals. J Cranio Maxillofac Surg. 2006;34:421–432. doi: 10.1016/j.jcms.2006.07.854. [DOI] [PubMed] [Google Scholar]
- 4.Wassmund M. Uber luxationsfrakturen des kiefergelenkes. Dtsch Kieferchir. 1934;1:27. [Google Scholar]
- 5.Kohler A. Die Behandlung der luxationsfrakturen in wachsendenund ausgewachsenen Kiefer—Sowie ihre Ergebnisse. Dtsch Stomatol. 1956;6:561. [Google Scholar]
- 6.Haug RH, Brandt MT. Closed reduction, open reduction, and endoscopic assistance: current thoughts on the management of mandibular condyle fractures. Plast Reconstr Surg. 2007;120(Suppl. 2):90S. doi: 10.1097/01.prs.0000260730.43870.1b. [DOI] [PubMed] [Google Scholar]
- 7.Palmieri C, Ellis E, III, Throckmorton GS. Mandibular motion after closed and open treatment of unilateral mandibular condylar process fractures. J Oral Maxillofac Surg. 1999;57:764. doi: 10.1016/S0278-2391(99)90810-8. [DOI] [PubMed] [Google Scholar]
- 8.Ellis E, III, Simon P, Throckmorton GS. Occlusal results after open or closed treatment of fractures of the mandibular condylar process. J Oral Maxillofac Surg. 2000;58:260. doi: 10.1016/S0278-2391(00)90047-8. [DOI] [PubMed] [Google Scholar]
- 9.Ellis E, III, Throckmorton GS. Bite forces after open or closed treatment of mandibular condylar process fractures. J Oral Maxillofac Surg. 2001;59:389. doi: 10.1053/joms.2001.21873. [DOI] [PubMed] [Google Scholar]
- 10.Throckmorton GS, Ellis E., III Recovery of mandibular motion after closed and open treatment of unilateral mandibular condylar process fractures. Int J Oral Maxillofac Surg. 2000;29:421. doi: 10.1016/S0901-5027(00)80072-7. [DOI] [PubMed] [Google Scholar]
- 11.Throckmorton GS, Ellis E, III, Hayasaki H. Masticatory motion after surgical or nonsurgical treatment for unilateral fractures of the mandibular condylar process. J Oral Maxillofac Surg. 2004;62:127. doi: 10.1016/j.joms.2003.01.003. [DOI] [PubMed] [Google Scholar]
- 12.Eckelt U, Schneider M, Erasmus F, et al. Open versus closed treatment of fractures of the mandibular condylar process—A prospective randomized multi-centre study. J Cranio Maxillofacial Surg. 2006;34:306. doi: 10.1016/j.jcms.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 13.Schneider M, Lauer G, Eckelt U. Surgical treatment of fractures of the mandibular condyle: a comparison of long term results following different approaches—functional, axiographical, and radiological findings. J Cranio Maxillofacial Surg. 2007;35:151. doi: 10.1016/j.jcms.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 14.Myall R. Condylar injuries in children: what is different about them? In: Whortington P, editor. Controversies in oral and maxillofacial surgery. Philadelphia: WB Saunders; 1994. pp. 191–200. [Google Scholar]
- 15.Hovinga J, Boering G, Stegenga B. Long term results of nonsurgical management of condylar fractures in children. Int J Oral Maxillofac Surg. 1999;28:429. doi: 10.1016/S0901-5027(99)80056-3. [DOI] [PubMed] [Google Scholar]
- 16.Undt G, Kermer C, Rasse M, Sinko K, Ewers R. Transoral miniplate osteosynthesis of condylar neck fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:534–543. doi: 10.1016/S1079-2104(99)70082-X. [DOI] [PubMed] [Google Scholar]
- 17.Loukota RA. Endoscopically assisted reduction and fixation of condylar neck/base fractures–the learning curve. Br J Oral Maxillofac Surg. 2006;44:480. doi: 10.1016/j.bjoms.2005.11.019. [DOI] [PubMed] [Google Scholar]
- 18.Jensen T, Jensen J, Norholt SE et al (2006) Open reduction and rigid internal fixation of mandibular condylar fractures by an intraoral approach: a long term follow-up study of 15 patients. J Oral Maxillofac Surg 64:1771 [DOI] [PubMed]
- 19.Tasanen A, Lamberg MA. Transosseous wiring in the treatment of condylar fractures of the mandible. J Maxillofac Surg. 1976;4:200. doi: 10.1016/S0301-0503(76)80036-7. [DOI] [PubMed] [Google Scholar]
- 20.Kallela I, Soderholm AL, Paukku P, et al. Lag screw osteosynthesis of mandibular condyle fractures: a clinical and radiological study. J Oral Maxillofac Surg. 1995;53:1397. doi: 10.1016/0278-2391(95)90663-0. [DOI] [PubMed] [Google Scholar]
- 21.Ellis E, III, McFadden D, Simon P, et al. Surgical complications with open treatment of mandibular condylar process fractures. J Oral Maxillofac Surg. 2000;58:950. doi: 10.1053/joms.2000.8734. [DOI] [PubMed] [Google Scholar]
- 22.Manisali M, Amin M, Aghabeigi B, et al. Retromandibular approach to the mandibular condyle: a clinical and cadaveric study. Int J Oral Maxillofac Surg. 2003;32:253. doi: 10.1054/ijom.2002.0270. [DOI] [PubMed] [Google Scholar]
- 23.Vesnaver A, Gorjanc M, Eberlinc A et al (2005) The periauricular transparotid approach for open reduction and internal fixation of condylar fractures. J Cranio Maxillofacial Surg 33:169 [DOI] [PubMed]
- 24.Zide MF, Kent JN. Indications for open reduction of mandibular condyle fractures. J Oral Maxillofac Surg. 1983;41:89–98. doi: 10.1016/0278-2391(83)90214-8. [DOI] [PubMed] [Google Scholar]
- 25.Fernandez JA, Mathog RH. Open treatment of condylar fractures with biphase technique. Arch Otolaryngol Head Neck Surg. 1987;113:262–266. doi: 10.1001/archotol.1987.01860030038004. [DOI] [PubMed] [Google Scholar]
- 26.Stiesch-Scholz M, Schmidt S, Eckardt A. Condylar motion after open and closed treatment of mandibular condylar fractures. J Oral Maxillofac Surg. 2005;63:1304–1309. doi: 10.1016/j.joms.2005.05.293. [DOI] [PubMed] [Google Scholar]
- 27.Chossegros C, Cheynet F, Blanc JL, Bourezak Z. Short retromandibular approach of subcondylar fractures: clinical and radiologic long-term evaluation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:248–252. doi: 10.1016/S1079-2104(96)80347-7. [DOI] [PubMed] [Google Scholar]
- 28.Biglioli F, Colletti G. Transmasseter approach to condylar fractures by mini- retromandibular access. J Oral Maxillofac Surg. 2009;67:2418–2424. doi: 10.1016/j.joms.2009.04.066. [DOI] [PubMed] [Google Scholar]
- 29.Parsons ME. Sclerotherapy basics. Dermatol Clin. 2004;22:501–508. doi: 10.1016/j.det.2004.03.017. [DOI] [PubMed] [Google Scholar]
- 30.Rao JKD, Gehlot N, Laxmy V, Siwach V. Management of parotid fistula using hypertonic saline. Natl J Maxillofac Surg. 2011;2:177–180. doi: 10.4103/0975-5950.94477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Devlin MF, Hislop WS, Carton AT. Open reduction and internal fixation of fractured mandibular condyles by a retromandibular approach: surgical morbidity and informed consent. Br J Oral Maxillofac Surg. 2002;40:23–25. doi: 10.1054/bjom.2001.0748. [DOI] [PubMed] [Google Scholar]
- 32.Hyde N, Manisali M, Aghabeigi B, Sneddon K, Newman L. The role of open reduction and internal fixation in unilateral fractures of the mandibular condyle: a prospective study. Br J Oral Maxillofac Surg. 2002;40:19–22. doi: 10.1054/bjom.2001.0734. [DOI] [PubMed] [Google Scholar]
- 33.Iannetti G, Cascone P. Use of rigid external fixation in fractures of the mandibular condyle. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:394–397. doi: 10.1016/S1079-2104(05)80330-0. [DOI] [PubMed] [Google Scholar]
- 34.Widmark G, Bågenholm T, Kahnberg KE, Lindahl L. Open reduction of subcondylar fractures. A study of functional rehabilitation. Int J Oral Maxillofac Surg. 1996;25:107–111. doi: 10.1016/S0901-5027(96)80052-X. [DOI] [PubMed] [Google Scholar]
- 35.Sugiura T, Yamamoto K, Murakami K, Sugimura M. A comparative evaluation of osteosynthesis with lag screws, miniplates, or Kirschner wires for mandibular condylar process fractures. J Oral Maxillofac Surg. 2001;59:1161–1168. doi: 10.1053/joms.2001.26718. [DOI] [PubMed] [Google Scholar]
- 36.Villarreal PM, Monje F, Junquera LM, Mateo J, Morillo AJ, González C. Mandibular condyle fractures: determinants of treatment and outcome. J Oral Maxillofac Surg. 2004;62:155–163. doi: 10.1016/j.joms.2003.08.010. [DOI] [PubMed] [Google Scholar]
- 37.Choi BH, Yi CK, Yoo JH. Clinical evaluation of 3 types of plate osteosynthesis for fixation of condylar neck fractures. J Oral Maxillofac Surg. 2001;59:734–737. doi: 10.1053/joms.2001.24283. [DOI] [PubMed] [Google Scholar]


