Abstract
Literature searches of the Cochrane Library, PubMed, EMBASE, Web of Science, LILACS, China National Knowledge Infrastructure, and Wanfang Data databases were performed from 1966 to September 2014. Only randomized and quasi-randomized controlled clinical trials comparing operative and nonoperative treatments for displaced midshaft clavicle fractures were included. Data collection and extraction, quality assessment, and data analyses were performed according to the Cochrane standards. Thirteen studies were considered in the meta-analysis. Constant scores and the Disabilities of the Arm, Shoulder and Hand scores were improved in the operative fixation group at a follow up of one year or more. The nonunion and symptomatic malunion rates were significantly lower in the operative group. Additionally, the nonoperative group had a higher likelihood of neurological symptoms compared with the operative group. A significantly higher risk of complications was found in patients treated conservatively than in those who underwent operative fixation. However, when patients with nonunion and symptomatic malunion were excluded from the analysis, no significant differences in the complication rate were found. We concluded that based on the current clinical reports, operative treatment is superior to nonoperative treatment in the management of displaced midshaft clavicle fractures. However, we do not support the routine use of primary operative fixation for all displaced midshaft clavicle fractures in adults.
Keywords: Clavicle, Midshaft clavicles, Operative treatment, Nonoperative treatment, Meta-analysis
INTRODUCTION
Clavicle fractures, which account for approximately 2.6% of total body fractures and 34–45% of shoulder girdle injuries in adults, are among the most common bone injuries in the body 1,2. Appproximately 69–81% of clavicle fractures are in the middle one-third of the clavicle, which is the thinnest part and contains the smallest amount of soft tissue; 17% of clavicle fractures are in the lateral one-third, and 2% are in the medial one-third 3. Conventionally, most acute displaced midshaft clavicles fractures are treated nonoperatively with the expectationsof a high probability of fracture union, good functional outcomes and a high level of patient satisfaction 4–8.
However, the outcomes of nonoperative treatment are not as favorable as once thought, and the trend to surgically treat these fractures has grown 9,10. Whether surgical treatment is associated with improved outcomes remains unknown.
A few meta-analyses comparing operative versus nonoperative approaches for the treatment of midshaft clavicle fractures have been published in recent years 11,12, but the results were inconclusive due to the relatively small sample size in each published study. However, because several relevant studies have been published on this topic in recent years, the present meta-analysis is more precise.
The purpose of the present systematic review and meta-analysis was to determine the effectiveness of operative versus nonoperative treatment for displaced midshaft clavicle fractures by comparing the clinical results reported in all of the available related evidence.
MATERIALS AND METHODS
Literature search
This study was performed with guidance from the Cochrane Handbook for Systematic Reviews of Interventions and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement 13,14. The PubMed, Cochrane Library, EMBASE, Web of Science, LILACS, China National Knowledge Infrastructure and Wanfang Data databases were searched (from 1966 to September 2014). Keywords combined with MeSH terms, including clavicle, clavicular, and fractures, were used for searching; the search was performed without language restrictions but was limited to human subjects. Additionally, the reference lists of identified studies were manually checked to include other potentially eligible trials. This process was performed iteratively until no additional articles could be identified.
Inclusion and exclusion criteria
The search results were screened based on the following inclusion criteria: (i) the studies were randomized or quasi-randomized controlled clinical trials on patients with displaced midshaft clavicle fractures that had occurred within less than two weeks; (ii) the studies compared operative (including plate, intramedullary nail fixation) with nonoperative treatment (including sling or a figure-eight bandage), (iii) the patients were at least 16 years of age; and (iv) the studies included comparisons of the functional outcomes, measured with Disabilities of the Arm, Shoulder and Hand (DASH) and Constant scores, nonunion, symptomatic malunion, and complications. The exclusion criteria were as follows: (i) studies including patients with pathological fractures or preexisting shoulder abnormalities; (ii) studies concerning adolescent fractures; (iii) studies concerning open fractures; (iv) review literature, repeated reports, retrospective studies, or case reports; and (v) studies that did not report outcomes of interest.
Data extraction
Two reviewers independently extracted the following data from each included study: first author, year of publication, number of patients, number of patients lost to follow up, type of interventions, functional outcomes, and rates of nonunion, symptomatic malunion, neurological symptoms and total complications.
Outcomes for analysis
The primary outcome was the incidence of nonunion and symptomatic malunion; the secondary outcomes were clinical function measured by the DASH and Constant Shoulder scores, complications and subgroup analyses (neurological symptoms and complications without nonunion or symptomatic malunion).
Statistical analysis
Estimates of the treatment effect were expressed as risk ratios (RRs) for dichotomous outcomes and weighted mean differences (WMDs) for continuous outcomes, both with 95% confidence intervals (CIs). For studies that did not present standard deviations, the standard deviations were calculated from the P-value or CI following the guidance of the Cochrane Handbook for Systematic Reviews of Interventions 13. Homogeneity across the studies was assessed with a chi-square analysis, considering p<0.10 significant. A fixed effects model was used when the heterogeneity was not significant, and a random effects model was adopted if significant heterogeneity was present. A sensitivity analysis was performed by omitting one study each time to explore potential sources of heterogeneity and to test the stability of pooled results. Publication bias was observed with the funnel plot. Review Manager (RevMan) software (Version 5.3.5. The Nordic Cochrane Centre, Copenhagen, Denmark) 15, provided by The Cochrane Collaboration, was used for graphical representation of the pooled data.
Critical Appraisal
All selected articles were critically appraised by two reviewers independently, using the Jaded score 16. The score for each article could range from 0 (lowest quality) to 5 (highest quality). Scores of 3 to 5 denote good to excellent quality, and scores of 0 to 2 denote poor to low quality. All disagreements between the authors were resolved by consensus, and a third author was consulted if necessary.
RESULTS
Characteristics of the eligible studies
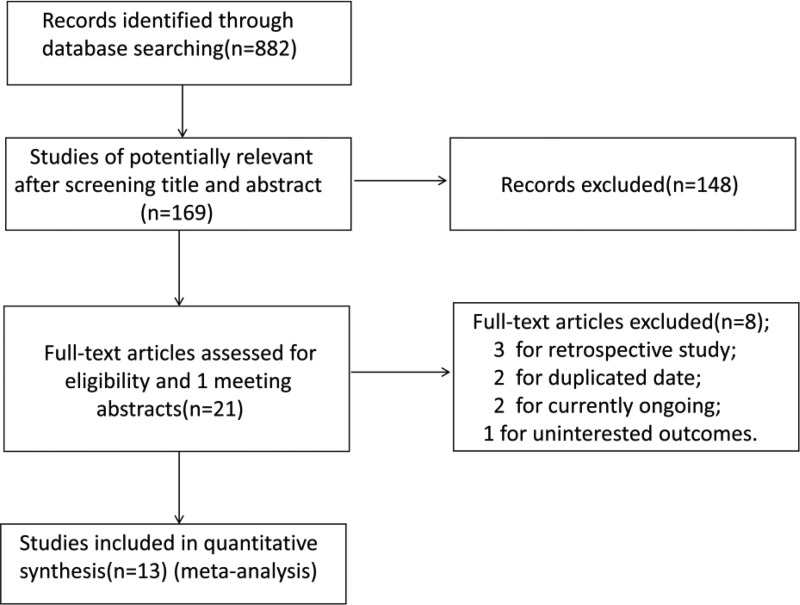
Details of the literature search are presented in a flow diagram (Figure 1). Thirteen studies with relatively low quality were included in the final analysis. Among them, the report by Smith et al. 17 was an abstract that met the inclusion criteria, and the sample sizes of the studies ranged from 40 to 178 patients. Information on the general characteristics, participants, and methodological quality of the 13 studies is summarized in Table 1. Of a total of 959 included patients, 507 were treated with operative approaches, and the others were treated with conservative approaches. Allocation concealment was reported in 8 trials 18–25 and was not stated in the other trials. Blinding was rarely used in the included studies; only one study by Robinson et al. 23 was blinded in the functional assessment.
Figure 1.
Flow chart showing article selection.
Table 1.
Characteristics and methodological quality of the included studies.
| Study | Design | No. of Patients Assessed (O/N) | Range of Ages (years) | Follow-up (months) | Internal Fixation | Nonoperative Treatment | Jadad Score |
|---|---|---|---|---|---|---|---|
| Smith (2001) | RCT | 30/35 | Adults | 12 | Plate | Sling | 3 |
| Jubel (2005) | QRCT | 26/27 | Adults | 6 | Nail | Bandage | 1 |
| COTS (2007) | RCT | 62/49 | 16–60 | 12 | Plate | Sling | 3 |
| Figueiredo (2008) | RCT | 24/16 | 18–58 | 12 | Plate | Sling | 3 |
| Judd (2009) | RCT | 29/28 | 17–40 | 12 | Nail | Sling | 3 |
| Smekal (2009) | RCT | 30/30 | 18–65 | 24 | Nail | Sling | 3 |
| Böhme (2011) | QRCT | 58/38 | 18–70 | 8 | Plate/Nail | Bandage | 1 |
| Chen (2011) | RCT | 30/30 | 18–63 | 15 | Nail | Sling | 3 |
| Mirzatolooei (2011) | RCT | 26/24 | 18–65 | 12 | Plate | Sling | 3 |
| Kulshrestha (2011) | QRCT | 45/28 | 20–50 | 18 | Plate | Sling | 1 |
| Virtanen (2012) | RCT | 26/25 | 18–70 | 12 | Plate | Sling | 3 |
| Robinson (2013) | RCT | 86/92 | 16–60 | 12 | Plate | CollarCuff | 4 |
| Mohsen (2014) | QRCT | 35/30 | 18–60 | 6 | Plate | Bandage | 1 |
O/N: operative group/nonoperative group, RCT: randomized controlled trial, QRCT: quasi-randomized controlled trial.
Nonunion and symptomatic malunion
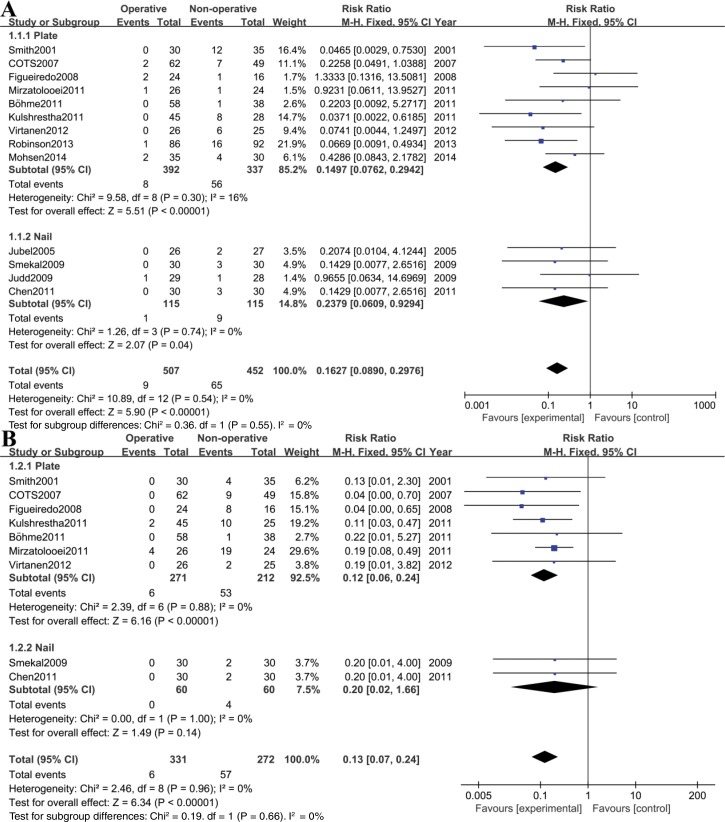
All 13 studies reported nonunion incidences. The pooled results of our primary outcome measure, nonunion incidence, presented a significant difference favoring operative over nonoperative treatment (RR, 0.16; 95%CI, 0.09-0.30; p<0.00001). Subgroup analysis concerning fixation methods showed that plate fixation (RR, 0.15; 95%CI, 0.07-0.29; p<0.00001) but not intramedullary nailing fixation (RR, 0.23; 95% CI, 0.06-0.92; p=0.04) was associated with a reduced risk compared with nonoperative treatment (Figure 2A). One study reported by Böhme et al. 27, in which fractures were reduced and fixed with both plates and nails in the operative groups, was excluded from the subgroup analysis.
Figure 2.
Forest plot showing comparison of nonunion rate (A) and symptomatic malunion rate (B) between operative (experimental) and nonoperative (control) groups.
Information on the incidence of symptomatic malunion was provided in 9 studies 17,18,20–22,24–27. Using the fixed effects model, the rate of symptomatic malunion was significantly lower in the operative group compared with that in the nonoperative group (RR 0.13, 95%CI 0.07–0.24, p<0.00001) (Figure 2B). No significant heterogeneity was detected among these studies (Chi2=10.89, df=12, I2=0%, p=0.74 and Chi2=2.46, df=8, I2=0%, p=0.96, respectively).
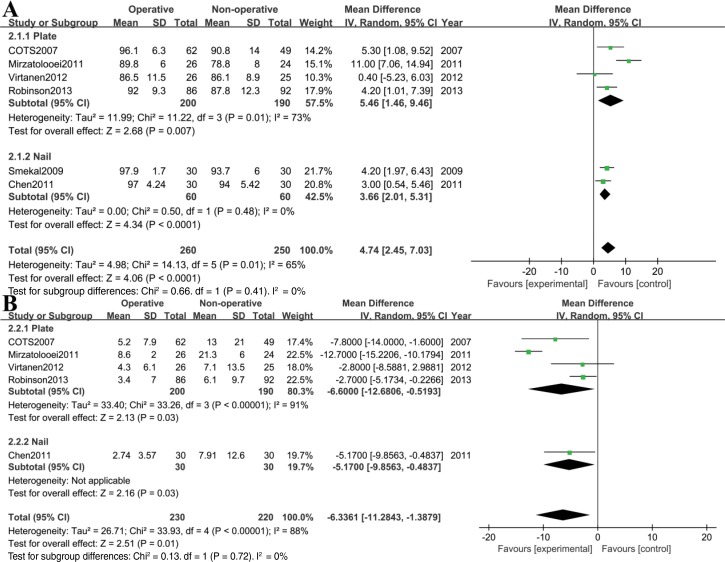
Functional outcomes
Nine studies 18,10–23,25,27–29 reported Constant scores (eight at a follow up of one year or more and one at a follow up of 6 months); the Constant scores of the operative group were higher than those of the nonoperative group. Three 27–29 of the nine studies were excluded from the analysis due to a lack of data on the standard deviation or to insufficient follow-up. The test for heterogeneity was significant (Chi2=14.13, df=5, I2=65%, p=0.01). Using the random effects model, the aggregated results suggested that the Constant score was significantly higher in the operative group compared with the nonoperative group (WMD 4.74, 95%CI, 2.45–7.03, p<0.0001) (Figure 3A). Subsequently, we performed a sensitivity analysis to explore potential sources of heterogeneity. Exclusion of the trial conducted by Mirzatolooei 21 reduced the heterogeneity (Chi2=2.47, df=4, I2=0%, p=0.65) but did not materially alter the pooled results (WMD 3.74, 95%CI, 2.39 – 5.08, p<0.00001).
Figure 3.
Forest plot showing comparison of Constant scores (A) and DASH scores (B) between operative (experimental) and nonoperative (control) groups.
DASH scores were used in eight studies 18,20–23,25,28,29; the DASH scores of the operative group were lower than those of the nonoperative group at a follow up of one year or more, but the actual standard deviations were only included in five studies 18,21–23,25. Pooled data showed that the DASH score in the operative group was significantly lower than that in the nonoperative group (WMD -6.34, 95%CI -11.28 – -1.39, p=0.01) (Figure 3B). Significant heterogeneity was detected among these studies (Chi2=33.93, df=4, I2=88%, p<0.00001). Similarly, exclusion of the trial conducted by Mirzatolooei 21 resolved the heterogeneity (Chi2=2.77, df=3, I2=0%, p=0.43) without materially altering the pooled results (WMD -3.64, 95%CI -5.58 – -1.69, p=0.0002).
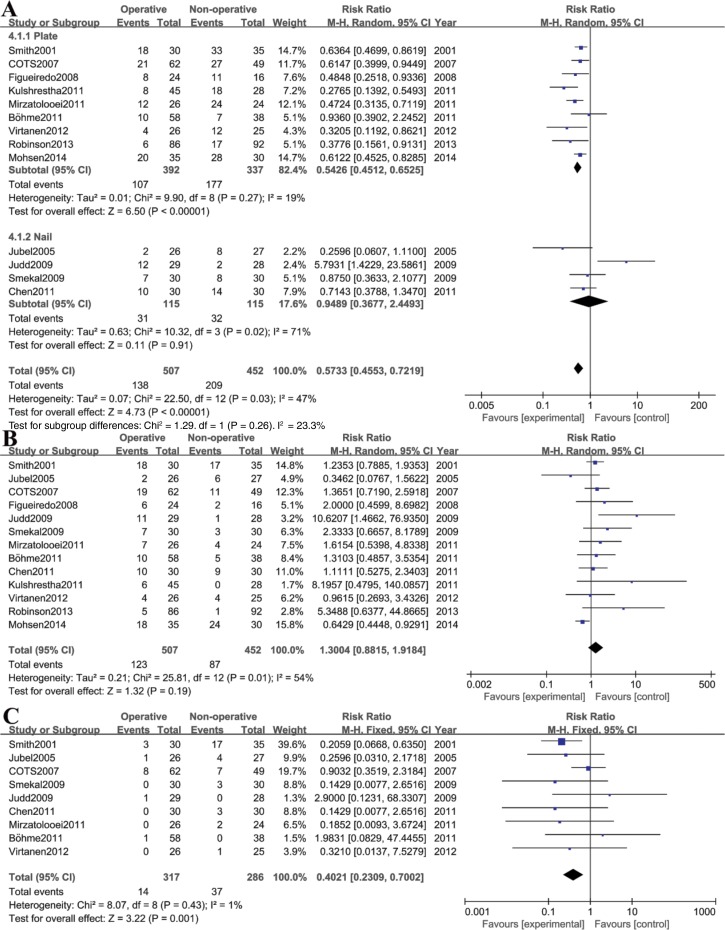
Complications
Because the definition of complications varied in all of the studies, we defined complications as all adverse events that were reported in those trials: nonunion (usually defined as no evidence of healing at fifty-two weeks after injury), delayed union (no evidence of healing at twenty-four weeks after injury), symptomatic malunion, infection, hardware removal, neurological symptoms, and refracture, among others.
In an overall analysis of the 13 selected studies, significant heterogeneity (Chi2=22.50, df=12, I2=47%, p=0.03) was detected among these studies. Sensitivity analysis found that the study reported by Judd et al. 19 was the source of heterogeneity, probably owing to a high rate of hardware-related complications associated with the use of Hagie pins in this study. Thus, the random effects model was applied. A significantly higher risk of complications was found in patients treated conservatively than in those who underwent operative fixation (RR 0.57, 95%CI 0.46-0.72, p<0.00001) (Figure 4A). Furthermore, we also performed a subgroup analysis of the complications without nonunion and symptomatic malunion. The aggregated results suggested that there were no significant differences between groups in the rates of complications (RR 1.30, 95%CI 0.88–1.92, p=0.19) (Figure 4B). Significant heterogeneity was detected among these studies (Chi2=25.81, df=12, I2=54%, p=0.01). We then performed sensitivity analysis and found that the study reported by Mohsen et al. 29 was source of heterogeneity (Chi2=12.95, df=11, I2=15%, p=0.30). Although heterogeneity was found, statistically similar results to those of the overall analysis were obtained in the sensitivity analysis. The predominant complications in the nonoperative group were nonunion, neurological symptoms (including brachial plexus irritation and compression) and symptomatic malunion. The operative complications tended to be hardware related (including plate irritation, pin protrusion and removal).
Figure 4.
Forest plot showing comparison of complications rates (A and B) and neurologic symptoms rates (C) between operative (experimental) and nonoperative (control) groups.
Neurologic symptoms
Nine studies reported neurological symptoms 17–22,25,27,28. Pooled data showed that the operative group had a significantly lower likelihood of developing neurological symptoms compared with the nonoperative group (RR 0.40, 95%CI 0.23–0.70, p=0.001). No significant heterogeneity was detected among these studies (Chi2=8.07, df=8, I2=1%, p=0.43) (Figure 4C).
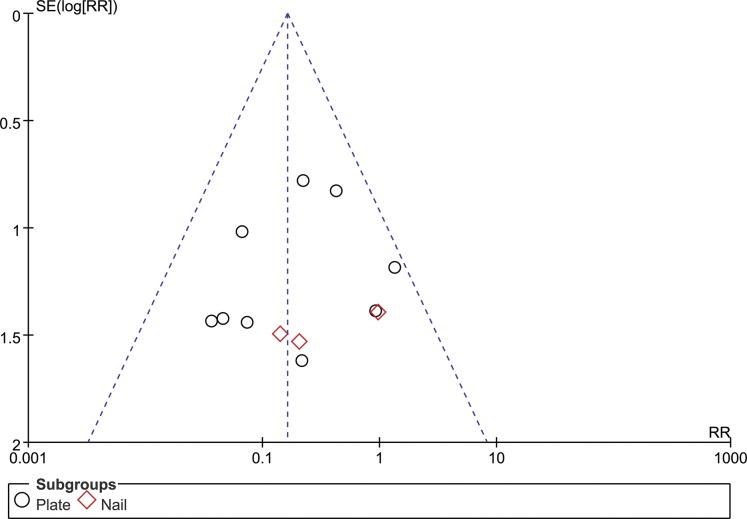
Publication bias
Publication bias was assessed by comparing the WMDs of nonunion; no evidence of publication bias was detected (Figure 5).
Figure 5.
Funnel plot of detection of publication bias.
DISCUSSION
Our meta-analysis revealed that primary operative fixation could effectively reduce the rates of nonunion, symptomatic malunion, neurological symptoms and overall complications. In addition, DASH and Constant scores were significantly improved after operative fixation compared with nonoperative treatment after a follow up of one year or more. Based on current clinical reports, we conclude that operative treatment is superior to nonoperative treatment in the management of displaced midshaft clavicle fractures.
Pooled data showed that 14% of 452 patients in the nonoperative group developed a nonunion, which is significantly higher (p=0.00001) than the 1.7% rate of nonunion in the 507 patients of the operative group. Symptomatic malunion was also significantly more common in the nonoperative group (20% in the nonoperative group versus 1.8% in the operative group, p<0.00001). However, with the data available, we were not able to draw any specific conclusions as to which patients were most likely to suffer from one of these significant complications; we also do not support the routine use of primary operative fixation for all displaced clavicle fractures in adults because an unacceptably high number of patients would be exposed to the risks of surgery 23.
Although significant differences were found between the two treatment groups in terms of functional outcomes, the reasons for functional outcome differences are probably multifactorial because most individuals who developed nonunion or symptomatic malunion had significantly lower outcome scores (i.e., a mean of sixteen points worse on the DASH score in nonunion patients in the study by Virtanen et al. 22). Additionally, Robinson et al. 23 showed that the development of nonunion was the only independent predictor of functional outcomes. When patients with nonunions were excluded, there was only a trend toward better functional outcomes in the operative group, with no significantly different scores at any time. Therefore, we thought that the improved outcomes may have resulted from the prevention of nonunion and symptomatic malunion by operative fixation. Unfortunately, without sufficient original data, we cannot perform a subgroup analysis of patients with overall healed fractures.
Overall complication and neurological symptom rates were higher in the nonoperative group than in the operative group. The subgroup analysis of the complications without nonunion and symptomatic malunion suggested that no significant between-group differences existed in the complication rates (p=0.23). The most common complications in the operative group were hardware related (including plate irritation, pin protrusion and removal). Theoretically, these complications could be reduced by using less prominent implants or improved surgical techniques. The predominant complications in the nonoperative group were nonunion, neurological symptoms (including brachial plexus irritation and compression) and symptomatic malunion; however, most of those complications require operative intervention.
Although modern plate fixation techniques provide reliable healing rates, the optimal plate position and type remain controversial. The clavicle contour and anatomy are curved in multiple planes. The reconstruction plate is easier to contour in all planes than the stiffer dynamic compression plates (DCP), which allow bending only along the length of the plate. For superior plating, a reconstruction plate or precontoured plate can more precisely fit the ‘S'-shaped anatomy. For anteroinferior plating, DCPs can be bent to conform to the anatomy very well 39. Regarding stability, two biomechanical studies have found greater stability with compression plates compared with reconstruction plates 31,32. In addition, a finite element study showed that anteroinferior plating best resists the effects of most daily living forces that act on the clavicle and can be considered more mechanically physiological 33.
Will et al. 34 suggested that locked compression plates (LCPs) provided more stiffness and less deflection than low-contact dynamic compression plates (LC-DCPs). Using a simulated segmental clavicle fracture model, another biomechanical study by Iannotti et al. 35 reported that LC-DCPs offer significantly greater biomechanical stability than reconstruction plates and DCPs and that clavicles plated at the superior aspect exhibited significantly greater biomechanical stability than those plated at the anterior aspect. However, most of the biomechanical studies must be interpreted with caution because such testing can offer clean comparisons of instrumentation and technique without the confounding factors of patient and surgeon variations. Nine of the 13 studies included in this review used plate fixation; among them, three studies used reconstruction plates 21,22,26, two studies used DCPs 24,29, and two studies used LCPs 17,23. Another two studies that used a mixture of plate implants 18,27 was not analyzed here. The rate of nonunion was 6% in the DCP group, which was higher than that in the reconstruction plate group (1%) and LCP group (1%). Symptomatic malunion only occurred in the reconstruction plate group, with a rate of 6%. In addition, overall complication rates were higher than 20% in all of the groups, which is consistent with previous literature 30. Recent clinical studies have shown efficient healing, few complications, and excellent return to function for anteroinferior plating 36–38. The advantages of this technique include the avoidance of potentially dangerous infraclavicular structures and the reduction of patient complaints due to implant prominence 36. A retrospective cohort study 39 with 156 midshaft clavicle fractures concluded that anteroinferior clavicle fracture fixation with DCPs results in excellent healing rates and lower removal rates. Moreover, implant failure occurred more often with reconstruction plates compared with dynamic compression plates (p=0.029).
Considering these mechanical and clinical findings, the plate type, precontouring, and position likely affect outcomes and implant-related complication rates. However, these effects have yet to be fully examined and more prospective trials are required to analyze the influence of various plate types and positions on implant-related complications in the future.
Further subgroup analysis by type of surgery indicated that plate fixation but not intramedullary nail fixation was associated with a reduced risk of nonunion, symptomatic malunion and total complications compared with nonoperative treatment. No significant difference in the functional outcomes between these two techniques was observed. However, the pooled data showed that the incidences of nonunion, symptomatic malunion and total complications were comparable in the two operative groups (2% versus 1%, 2% versus 0, 27% versus 27%, respectively).
Both the plating and intramedullary nail methods have advantages and disadvantages. Biomechanically, plate fixation is superior to intramedullary fixation 40. Patients treated with plate fixation can achieve full range of motion. The disadvantages of plate fixation include the necessity for increased exposure and soft tissue stripping, the increased risk of damage to the supraclavicular nerve, slightly higher infection rates, and the risk of refracture after plate removal 18. A recent randomized clinical trial comparing locked intramedullary nailing versus plating for displaced midshaft clavicle fractures performed by Ferran et al. 41 showed no significant differences between the two operative techniques. Another two prospective comparative studies concluded that both plating and intramedullary flexible nailing are equally effective alternatives for the surgical fixation of displaced midshaft clavicle fractures but that intramedullary techniques have potential advantages such as less soft tissue injury, shorter operative times and hospital stays, less blood loss and higher cosmetic satisfaction 42,43. The subgroup analysis results of our review are partially consistent with the results of the three trials; however, due to the limitations of those studies such as their small sample sizes and single center designs, we cannot provide any strong conclusions. Studies with sound rationale and design are required to accurately and definitively assess the differences in outcomes between plate fixation and intramedullary fixation 44.
However, with a myriad of options available for both plate fixation and intramedullary fixation, the question of which form of fixation is superior remains. According to currently available data, the superior surgical technique and implant choice are those that the surgeon was originally trained to perform and use.
Previous literature has addressed the issue of nails, yet the difference between locked and unlocked nails has not been considered. This study may provide additional interesting clues for future research on this topic.
We identified six systematic reviews that approached the comparison between surgical versus conservative interventions to treat middle-third clavicle fracture in adults 11,12,45–48. The results of our review are consistent with those of the eight systematic reviews; however, the conclusions of those published reviews varied, which was partly in accordance with our conclusions. The only Cochrane systematic review, reported by Lenza et al, used more comprehensive statistical methods, which were lacking in our present study. The most distinguishing characteristic of those published reviews was that analysis was conducted with incomplete information. With the exception of one study by Lenza et al, the reviews did not include the two RCTs 24,25. Additionally, new RCTs have been published since then. Our review adds consistent information for current clinical practice. We applied more specific subgroup analysis by surgery and implant type and then discussed the results in detail. Furthermore, we performed a broader literature search that included non-English publications. Bias is inherent in many analyses focusing on specific populations or geographic areas. By including all of the available studies, including those from multiple countries and reported in multiple languages, we believe that our conclusions are applicable to most populations.
There are some limitations of this study. First, the recruited studies were not all randomized controlled trials. The lack of inadequate allocation concealment and blinding, which can lead to over-reporting of the treatment effect and selection or allocation biases, likely affected the study results. Second, the preoperative fracture pattern was found to be significantly related to implant failure 49, but our meta-analysis could not show fracture type–specific effects between operative and nonoperative treatments because of the limited data of the studies. Finally, despite our best efforts to use multiple search methods, we may not have detected all eligible existing trials with results that are applicable to our meta-analysis. Therefore, the results should be interpreted with caution. Further research entailing high-quality randomized controlled, multicenter trials with long-term functional outcomes and fracture type–specific designs is required to address key clinical questions regarding the effects of operative treatment versus nonoperative treatment in the management of displaced midshaft clavicle fractures in adults.
In summary, we conclude that operative treatment is superior to nonoperative treatment in the management of displaced midshaft clavicle fractures, although we do not support the routine use of primary operative fixation for all displaced clavicle fractures in adults. Patients with a completely displaced midshaft clavicle fracture should be informed that they will be at a higher risk of sustaining nonunion, symptomatic malunion and potential neurological symptoms if the fracture is treated conservatively.
REFERENCES
- 1.Neer C. Fractures of the clavicle. In: Rockwood CA Jr, Green DP, editors. Fractures in adults. 2nd ed. Philadelphia: Lippincottp. 1984;707-13. [Google Scholar]
- 2.Neer CSII. Fractures of the distal third of the clavicle. Clin Orthop Relat Res. 1968;58:43–50. [PubMed] [Google Scholar]
- 3.Van der Meijden OA, Gaskill TR, Millett PJ. Treatment of clavicle fractures: current concepts review. J Shoulder Elbow Surg. 2012;21((3)):423–9. doi: 10.1016/j.jse.2011.08.053. [DOI] [PubMed] [Google Scholar]
- 4.Sankarankutty M, Turner BW. Fractures of the clavicle. Injury. 1975;7((2)):101–6. doi: 10.1016/0020-1383(75)90006-6. [DOI] [PubMed] [Google Scholar]
- 5.Rowe CR. (58) An atlas of anatomy and treatment of midclavicular fractures. Clin Orthop Relate Res; pp. 29–42. 1968. [PubMed] [Google Scholar]
- 6.Andersen K, Jensen PO, Lauritzen J. Treatment of clavicular fractures. Figure-of eight bandage versus a simple sling. Acta Orthop Scand. 1987;58((1)):71–4. doi: 10.3109/17453678709146346. [DOI] [PubMed] [Google Scholar]
- 7.Eskola A, Vainionpää S, Myllynen P, Pätiälä H, Rokkanen P. Outcome of clavicular fracture in 89 patients. Arch Orthop Trauma Surg. 1986;105((6)):337–8. doi: 10.1007/BF00449938. [DOI] [PubMed] [Google Scholar]
- 8.Nordqvist A, Petersson CJ, Redlund-Johnell I. Mid-clavicle fractures in adults: end result study after conservative treatment. J Orthop Trauma. 1998;2((8)):572–6. doi: 10.1097/00005131-199811000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br. 1997;79((4)):537–9. doi: 10.1302/0301-620X.79B4.7529. [DOI] [PubMed] [Google Scholar]
- 10.McKee MD, Pedersen EM, Jones C, Stephen DJ, Kreder HJ, Schemitsch EH, et al. Deficits following nonoperative treatment of displaced midshaft clavicular fractures. J Bone Joint Surg Am. 2006;88((1)):35–40. doi: 10.2106/JBJS.D.02795. [DOI] [PubMed] [Google Scholar]
- 11.McKee RC, Whelan DB, Schemitsch EH, McKee MD. Operative versus nonoperative care of displaced midshaft clavicular fractures: a meta-analysis of randomized clinical trials. J Bone Joint Surg Am. 2012;94((8)):675–84. doi: 10.2106/JBJS.J.01364. [DOI] [PubMed] [Google Scholar]
- 12.Lenza M, Buchbinder R, Johnston RV, Belloti JC, Faloppa F. Surgical versus conservative interventions for treating fractures of the middle third of the clavicle. Cochrane Database Syst Rev. 2013;6:CD009363. doi: 10.1002/14651858.CD009363.pub2. [DOI] [PubMed] [Google Scholar]
- 13.Higgins J, Green S. Cochrane handbook for systematic reviews of interventions Version 5.1.0. (Accessed July 15, 2014 at: http://handbook.cochrane.org.) [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62((10)):1006–12. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 15.Review Manager (RevMan) [Computer Program] Version 5.3.5. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; 2014. [Google Scholar]
- 16.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary. Control Clin Trials. 1996;17((1)):1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 17.Smith CA RJ, Crosby LA, editors. The 68th Annual Meeting of the American Academy of Orthopaedic Surgeons. ed. 2001. Results of operative versus nonoperative treatment for 100% displaced mid-shaft clavicle fractures: a prospective randomized trial. editor. [Google Scholar]
- 18.Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007;89((1)):1–10. doi: 10.2106/JBJS.F.00020. [DOI] [PubMed] [Google Scholar]
- 19.Judd DB, Pallis MP, Smith E, Bottoni CR. Acute operative stabilization versus nonoperative management of clavicle fractures. Am J Orthop (Belle Mead NJ) 2009;38((7)):341–5. [PubMed] [Google Scholar]
- 20.Smekal V, Irenberger A, Struve P, Wambacher M, Krappinger D, Kralinger FS. Elastic stable intramedullary nailing versus nonoperative treatment of displaced midshaft clavicular fractures-a randomized, controlled, clinical trial. J Orthop Trauma. 2009;23((2)):106–12. doi: 10.1097/BOT.0b013e318190cf88. [DOI] [PubMed] [Google Scholar]
- 21.Mirzatolooei F. Comparison between operative and nonoperative treatment methods in the management of comminuted fractures of the clavicle. Acta Orthop Traumatol Turc. 2011;45((1)):34–40. doi: 10.3944/AOTT.2011.2431. [DOI] [PubMed] [Google Scholar]
- 22.Virtanen KJ, Remes V, Pajarinen J, Savolainen V, Björkenheim JM, Paavola M, et al. Sling compared with plate osteosynthesis for treatment of displaced midshaft clavicular fractures: a randomized clinical trial. J Bone Joint Surg Am. 2012;94((17)):1546–53. doi: 10.2106/JBJS.J.01999. [DOI] [PubMed] [Google Scholar]
- 23.Robinson CM, Goudie EB, Murray IR, Jenkins PJ, Ahktar MA, Read EO, et al. Open reduction and plate fixation versus nonoperative treatment for displaced midshaft clavicular fractures: a multicenter, randomized, controlled trial. J Bone Joint Surg Am. 2013;95((17)):1576–84. doi: 10.2106/JBJS.L.00307. [DOI] [PubMed] [Google Scholar]
- 24.Figueiredo EA, Neves EJ, Yoshizawa Júnior H, Dall'Ara Neto A, Nascimento LFC, Faria GHM, et al. Prospective randomized study comparing surgical treatment using anterior plate to non-surgical treatment of midshaft clavicle fractures. Revista Brasileira de Ortopedia. 2008;43((10)):419–25. doi: 10.1590/S0102-36162008001000001. [DOI] [Google Scholar]
- 25.Chen QY, Kou DQ, Cheng XJ, Zhang W, Wang W, Lin ZQ, et al. Intramedullary nailing of clavicular midshaft fractures in adults using titanium elastic nail. Chin J Traumatol. 2011;14((5)):269–76. [PubMed] [Google Scholar]
- 26.Kulshrestha V, Roy T, Audige L. Operative versus nonoperative management of displaced midshaft clavicle fractures: a prospective cohort study. J Orthop Trauma. 2011;25((1)):31–8. doi: 10.1097/BOT.0b013e3181d8290e. [DOI] [PubMed] [Google Scholar]
- 27.Böhme J, Bonk A, Bacher G, Wilharm A, Hoffmann R, Josten C. Current treatment concepts for mid-shaft fractures of the clavicle-results of a prospective multicentre study. Z Orthop Unfall. 2011;149((1)):68–76. doi: 10.1055/s-0030-1250334. [DOI] [PubMed] [Google Scholar]
- 28.Jubel A, Andermahr J, Prokop A, Lee J, Schiffer G, Rehm K. Treatment of mid-clavicular fractures in adults. Early results after rucksack bandage or elastic stable intramedullary nailing. Unfallchirurg. 2005;108((9)):707–14. doi: 10.1007/s00113-005-0970-8. [DOI] [PubMed] [Google Scholar]
- 29.Mohsen K, Mohammad F, Hossein M, Hamid RA, Abdolhossein MN, Farid S, et al. The comparison of results of treatment of midshaft clavicle fracture between operative treatment with plate and non-operative treatment. Arch Bone Jt Surg. 2014;2((3)):210–4. [PMC free article] [PubMed] [Google Scholar]
- 30.Wijdicks FJG, Van der Meijden OAJ, Millett PJ, Verleisdonk E, Houwert RM. Systematic review of the complications of plate fixation of clavicle fractures. Arch Orthop Trauma Surg. 2012;132((5)):617–25. doi: 10.1007/s00402-011-1456-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Eden L, Doht S, Frey SP, Ziegler D, Stoyhe J, Fehske K, et al. Meffert RH: Biomechanical comparison of the locking compression superior anterior clavicle plate with seven and ten hole reconstruction plates in midshaft clavicle fracture stabilisation Int Orthop. 2012;36((12)):2537–43. doi: 10.1007/s00264-012-1671-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Drosdowech DS, Manwell SEE, Ferreira LM, Goel DP, Faber KJ, Johnson JA. Biomechanical analysis of fixation of middle third fractures of the clavicle. J Orthop Trauma. 2011;25((1)):39–43. doi: 10.1097/BOT.0b013e3181d8893a. [DOI] [PubMed] [Google Scholar]
- 33.Favre P, Kloen P, Helfet DL, Werner CML. Superior versus anteroinferior plating of the clavicle: a finite element study. J Orthop Trauma. 2011;25((11)):661–5. doi: 10.1097/BOT.0b013e3182143e06. [DOI] [PubMed] [Google Scholar]
- 34.Will R, Englund R, Lubahn J, Cooney TE. Locking plates have increased torsional stiffness compared to standard plates in a segmental defect model of clavicle fracture. Arch Orthop Trauma Surg. 2011;131((6)):841–7. doi: 10.1007/s00402-010-1240-y. [DOI] [PubMed] [Google Scholar]
- 35.Iannotti MR, Crosby LA, Stafford P, Grayson G, Goulet R. Effects of plate location and selection on the stability of midshaft clavicle osteotomies: A biomechanical study. J Shoulder Elbow Surg. 2002;11((5)):457–62. doi: 10.1067/mse.2002.125805. [DOI] [PubMed] [Google Scholar]
- 36.Collinge C, Devinney S, Herscovici D, DiPasquale T, Sanders R. Anterior-inferior plate fixation of middle-third fractures and nonunions of the clavicle. J OrthopTrauma. 2006;20((10)):680–6. doi: 10.1097/01.bot.0000249434.57571.29. [DOI] [PubMed] [Google Scholar]
- 37.Kloen P, Werner CML, Stufkens SAS, Helfet DL. Anteroinferior plating of midshaft clavicle nonunions and fractures. Oper Orthop Traumatol. 2009;21((2)):170–9. doi: 10.1007/s00064-009-1705-8. [DOI] [PubMed] [Google Scholar]
- 38.Galdi B, Yoon RS, Choung EW, Reilly MC, Sirkin M, Smith WR, et al. Anteroinferior 2.7-mm versus 3.5-mm plating for AO/OTA type B clavicle fractures: a comparative cohort clinical outcomes study. J Orthop Trauma. 2013;27((3)):121–5. doi: 10.1097/BOT.0b013e3182693f32. [DOI] [PubMed] [Google Scholar]
- 39.Gilde AK, Jones CB, Sietsema DL, Hoffmann MF. Does plate type influence the clinical outcomes and implant removal in midclavicular fractures fixed with 2.7-mm anteroinferior plates? A retrospective cohort study. J Orthop Surg Res. 2014;9:55. doi: 10.1186/s13018-014-0055-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Golish SR, Oliviero JA, Francke EI, Miller MD. A biomechanical study of plate versus intramedullary devices for midshaft clavicle fixation. J Orthop Surg Res. 2008;16((3)):28. doi: 10.1186/1749-799X-3-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ferran NA, Hodgson P, Vannet N, Williams R, Evans RO. Locked intramedullary fixation vs. plating for displaced and shortened mid-shaft clavicle fractures: a randomized clinical trial. J Shoulder Elbow Surg. 2010;19((6)):783–9. doi: 10.1016/j.jse.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 42.Narsaria N, Singh AK, Arun GR, Seth RRS. Surgical fixation of displaced midshaft clavicle fractures: elastic intramedullary nailing versus precontoured plating. J Orthopaed Traumatol. 2014;15((3)):165–71. doi: 10.1007/s10195-014-0298-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Assobhi JEH. Reconstruction plate versus minimal invasive retrograde titanium elastic nail fixation for displaced midclavicular fractures. J Orthopaed Traumatol. 2011;12((4)):185–92. doi: 10.1007/s10195-011-0158-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Alves K, Jupiter J. Clavicle Fractures: Plate Versus Intramedullary Fixation. Tech Should Surg. 2014;15:55–9. doi: 10.1097/BTE.0000000000000007. [DOI] [Google Scholar]
- 45.Duan X, Zhong G, Cen SQ, Huang FG, Xiang Z. Plating versus intramedullary pin or conservative treatment for midshaft fracture of clavicle: a meta-analysis of randomized controlled trials. J Shoulder Elbow Surg. 2011;20((6)):1008–15. doi: 10.1016/j.jse.2011.01.018. [DOI] [PubMed] [Google Scholar]
- 46.Virtanen K, Malmivaara AOV, Remes VM, Paavola MP. Operative and nonoperative treatment of clavicle fractures in adults: A systematic review of 1,190 patients from the literature. Acta Orthopaedica. 2012;83((1)):65–73. doi: 10.3109/17453674.2011.652884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Xu J, Xu L, Xu WD, Gu YD, Xu JG. Operative versus nonoperative treatment in the management of midshaft clavicular fractures: a meta-analysis of randomized controlled trials. J Shoulder Elbow Surg. 2014;23((2)):173–81. doi: 10.1016/j.jse.2013.06.025. [DOI] [PubMed] [Google Scholar]
- 48.Liu GD, Tong SL, Ou S, Zhou LS, Fei J, Nan GX, et al. Operative versus non-operative treatment for clavicle fracture: a meta-analysis. Int Orthop. 2013;37((8)):1495–500. doi: 10.1007/s00264-013-1871-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shin SJ, Do NH, Jang KY. Risk factors for postoperative complications of displaced clavicular midshaft fractures. J Trauma Acute Care Surg. 2012;72((4)):1046–50. doi: 10.1097/TA.0b013e31823efe8a. [DOI] [PubMed] [Google Scholar]