Abstract
Objective
To construct profiles of self-reported health indicators to examine differences and similarities between people with lower limb loss (LLL) and a normative sample (hereafter called the norm), and to compare health indicators between subgroups based on level and etiology of limb loss.
Design
Survey
Setting
General community
Participants
Adults with unilateral lower limb loss (n=1091) participated in this study. Eligibility criteria included LLL resulting from trauma or dysvascular complications and regular use of a prosthesis.
Interventions
Not applicable
Main Outcome Measures
Patient-Reported Outcomes Measurement Information System 29-item profile (PROMIS-29) version 1.0 measures physical function, pain interference, fatigue, sleep disturbance, anxiety, depression and satisfaction with participation in social roles. The norms are based on 5,239 individuals representative of the U.S. general population in gender, age, race, ethnicity and education.
Results
People with LLL reported statistically significantly worse physical function, pain interference and satisfaction with participation in social roles and significantly less fatigue than the norm. People with transfemoral (i.e., above-knee) amputation significantly differed from people with transtibial (i.e., below-knee) amputation on physical function. Similarly, people with amputation due to trauma and dysvascular etiology significantly differed on physical function and satisfaction with social roles after adjusting for relevant clinical characteristics.
Conclusions
People with LLL generally report worse physical function, pain interference and satisfaction with social roles when compared to norm. People with dysvascular amputation reported worse physical function and satisfaction with social roles than people with traumatic amputation. Health indicator profiles are an efficient way of providing clinically meaningful information about numerous aspects of self-reported health in people with LLL.
Keywords: artificial limb, limb prosthesis, outcome assessment (health care), quality of life, rehabilitation
Loss of a limb has a profound impact on health indicators, including physical, mental, and emotional health. Associations between lower limb loss (LLL) and impaired functional mobility, an aspect of physical health, have been well documented.1–8 Limited mobility often persists in the months and years following limb amputation.2–4,9 LLL is also associated with other physical and mental health problems, such as pain (e.g., phantom limb,10,11 residuum,10,11 and back pain12,13) and depression.10 Health indicators in people with LLL also differ by factors such as level of amputation and etiology.5,10,14
Worse health outcomes are often associated with poor rehabilitation results in people with LLL.10 For example, people with LLL who experience depression also more commonly report less use of a prosthetic limb, higher perceived vulnerability, and lower self-rated overall health.10 Conversely, greater participation in social experiences is positively associated with mobility outcomes, such as walking distance.3 Assessment of health indicators in clinics is important as monitoring and addressing physical, mental and social function may improve rehabilitation outcomes in people with LLL.1 Despite the recognized importance of physical, mental, and social issues related to the rehabilitation of people with LLL,15 health providers typically focus rehabilitation efforts on patients’ physical health and may not adequately assess psychosocial functioning.16 This tendency to focus on physical recovery may be reinforced by challenges related to availability of brief and psychometrically-sound health assessment instruments that are easy for clinicians to administer, score, and interpret.17,18 New measurement tools developed with funding from the National Institutes of Health (NIH), such as Patient-Reported Outcomes Measurement Information System (PROMIS) instruments, allow for efficient assessment of multiple self-reported health indicators.19 Because PROMIS instruments are brief and the scores are on the same metric, they lend themselves to construction of profiles that include aspects of physical, mental and social health.19 Well established instruments, such as SF-36, also could be used to examine profiles of health indicators and the studies using such instruments have described worse health indicators in people with LLL compared to those without LLL.20,21 However, some domains of SF-36 and related instruments (e.g., SF-12) are different from those included in PROMIS 29. In addition, PROMIS-29 domains can be administered using computer adaptive testing, which increases the precision of the score while minimizing respondents’ burden.22 To date no studies used PROMIS measures to examine health indicators of people with LLL.
This study aimed to examine health indicator profiles in a large sample of people with LLL by comparing scores on physical function, pain interference, anxiety, depression, fatigue, sleep disturbance, and satisfaction with participation in social roles (1) between the overall sample and PROMIS normative sample (the norm) and (2) between subgroups with different levels of limb loss and etiologies of amputation. We hypothesized that (a) individuals with LLL would generally report worse health than the general United States (U.S.) population, especially on physical function, and (b) individuals with higher amputation levels and dysvascular etiology of amputation would report worse health than their peers with lower amputation levels and traumatic etiology of amputation.
Methods
Study Design
Data for this study were obtained from a cross-sectional, self-reported health survey administered to lower limb prosthesis users in the process of developing an instrument to measure mobility in people with LLL (i.e., the Prosthetic Limb Users Survey of Mobility, PLUS-M, www.plus-m.org). Surveys were administered to study participants by computer, paper, or phone, according to their preferences and included the PROMIS-29 Profile as well as self-reported demographic and clinical characteristics.
Participants
Participants were recruited across the U.S. using flyers posted in 133 private, 4 hospital, and 7 institutional clinics. Magazine advertisements, listserv postings, targeted mailings from a national clinical provider, and postings to journal, clinic, and patient organization websites were also used. All study participants were required to report that they: (1) are 18 years of age or older, (2) have a unilateral amputation below the hip and at or above the ankle resulting from trauma or dysvascular complications, (3) have no other amputations, (4) regularly use a lower limb prosthesis to walk and (5) are able to read, write, and understand English. Amputations at or above the knee were categorized as transfemoral amputations (TFA) and amputations at or above the ankle and below the knee were categorized as transtibial amputations (TTA).
For the purpose of PLUS-M development, recruitment targets were set to include a minimum of 500 people from each of the following sub-groups of people with LLL: (1) those with TTA from either traumatic or dysvascular etiologies, (2) those with TFA from either traumatic or dysvascular etiologies, (3) those with dysvascular LLL at the TTA or TFA level and (4) those with traumatic LLL at the TTA or TFA level. All participants belonged to two of these four subgroups. The subgroups were chosen as they represent the most prevalent etiologies and levels of amputation among people with LLL.23,24
All study procedures were reviewed and approved by University of Washington Institutional Review Board.
Measures
Demographic and Amputation-Specific Measures
Participants were asked to provide basic demographic information including age, gender, race and ethnicity, employment status, veteran status, education and income level. In addition, participants provided information regarding amputation level and etiology, comorbid health conditions, time since amputation (in years), daily prosthesis use (in hours) and average pain intensity.
Health indicators
The PROMIS domain framework organizes the instruments into physical, metal and social health.19 PROMIS-29 Profile version 1.0 was administered to measure aspects of physical health (physical function, pain interference, fatigue, sleep disturbance), mental health (anxiety, depression) and social health (satisfaction with participation in social roles). The PROMIS item banks, on which the short forms included in PROMIS-29 are based, were developed using rigorous methodology including item response theory (IRT).19 All PROMIS instruments provide an IRT-based score on the T-metric, with a mean of 50 and a standard deviation of 10. Normative scores for each of the PROMIS-29 health domains are based on samples representative of the U.S. general population in gender, age, race, ethnicity and education.25 A higher score indicates higher levels of the trait that is being measured. For instance, a higher score on depression indicates worse health, while a higher score on physical function indicates better health. With one exception the score of 50 represents the mean of the norm that is representative of the general U.S. population. The sleep disturbance instrument is centered on a population that had a greater percentage of clinical populations than was present in the norm. Thus, the score of 50 on this domains represents a mean of somewhat less healthy population.26
Analyses
Demographic and clinical information for the overall sample and for the sub-groups based on etiology (i.e., trauma and dysvascular complications) and amputation level (i.e., TTA and TFA) were summarized using frequencies, means and standard deviations. Prior to statistical hypothesis testing, score distributions for the variables used in the health profiles were inspected for normality. When distributional assumptions were not supported, both parametric and non-parametric analyses were used and the results compared. Independent, two-tailed t-tests and Wilcoxon-Mann-Whitney tests were used for pairwise comparisons to evaluate differences in the amputation level and etiology subgroups. One-sample t-tests and one-sample median sign tests were used to compare the PROMIS scores between the normative sample and both the overall sample of people with LLL and subgroups defined by amputation level and etiology. Because of the sample size in this study the reporting of results of the parametric tests, such as t-tests, is appropriate as they are robust to violation of normality as the sample size increases.27–29 To adjust for relevant demographic and clinical variables we used multiple regression analyses. We fit seven multiple regression models. Eight independent variables were used in each model. The binary variables were used to indicate amputation level (0= transfemoral and 1=transtibial); etiology (0=dysvascular and 1=trauma); and gender (0=male and 1=female). Three binary variables were included to characterize the ethnicity: non-Hispanic black, Hispanic, and other ethnicity (reference group = non-Hispanic white). The years since amputation and age were used as continuous variables.
Results
Demographics
A total of 1,091 individuals with LLL completed the PROMIS-29 instrument. Sample demographics and clinical indicators are described in Table 1. The majority of the sample was male (n=768, 71%) and non-Hispanic white (n=871, 80%) with an average age of 55 years. On average, participants were 12 years post-amputation and used their prostheses 12 hours per day. Over a half of the sample had traumatic LLL (n=604, 55%) and almost two-thirds (n=705, 65%) reported LLL at the TTA level. The sample was similar to demographic estimates of people with LLL in the U.S. with respect to gender and age, but less diverse in ethnicity and race.24
Table 1.
Sample characteristicsǂ
| Overall n=1091 |
Amputation Etiology | Amputation Level | |||
|---|---|---|---|---|---|
|
| |||||
| Trauma n=604 |
Dysvascular n=487 |
Transtibial n=705 |
Transfemoral n=386 |
||
|
| |||||
| Mean (SD) or % (N) | Mean (SD) or % (N) | Mean (SD) or % (N) | Mean (SD) or % (N) | Mean (SD) or % (N) | |
| Demographic characteristics | |||||
| Age at survey (years) | 55.0 (13.4) | 51.1 (13.8) | 59.8 (11.2)*** | 55.4 (13.0) | 54.2 (14.2) |
| Gender (%) | |||||
| Male | 70.6 (768) | 70.1 (421) | 71.3 (347) | 70.9 (499) | 70.1 (269) |
| Female | 29.4 (320) | 30.0 (180) | 28.8 (140) | 29.1 (205) | 30.0 (115) |
| Race/Ethnicity | |||||
| Non-Hispanic White | 80.4 (871) | 81.7 (490) | 78.7 (381)** | 81.3 (570) | 78.6 (301) |
| Non-Hispanic Black | 9.1 (99) | 6.7 (40) | 12.2 (59) | 8.1 (57) | 11.0 (42) |
| Hispanic | 6.3 (68) | 6.7 (40) | 5.8 (28) | 6.3 (44) | 6.3 (24) |
| Other | 4.2 (46) | 5.0 (30) | 3.3 (16) | 4.3 (30) | 4.2 (16) |
| Military status | |||||
| Active Military/Veteran | 20.2 (218) | 18.1 (108) | 22.8 (110) | 19.8 (138) | 21.0 (80) |
| Socioeconomic characteristics | |||||
| Employment Status | |||||
| Employed | 31.7 (345) | 44.4 (267) | 16.1 (78)*** | 31.6 (222) | 32.0 (123) |
| Retired | 25.1 (273) | 18.3 (110) | 33.5 (163) | 24.9 (175) | 25.5 (98) |
| On Disability | 32.1 (349) | 23.0 (138) | 43.4 (211) | 32.7 (230) | 31.0 (119) |
| Other | 11.0 (120) | 14.3 (86) | 7.0 (34) | 10.8 (76) | 11.5 (44) |
| Individual Income | |||||
| < $25,000 | 48.5 (516) | 40.0 (235) | 58.9 (281)*** | 48.9 (337) | 47.6 (179) |
| $25,000 – $39,999 | 20.0 (213) | 18.4 (108) | 22.0 (105) | 20.6 (142) | 18.9 (71) |
| $40,000 – $54,999 | 10.3 (110) | 12.4 (73) | 7.8 (37) | 9.3 (64) | 12.2 (46) |
| $55,000 – $69,999 | 7.1 (76) | 9.5 (56) | 4.2 (20) | 7.0 (48) | 7.5 (28) |
| ≥ 70,000 | 14.1 (150) | 19.7 (116) | 7.1 (34) | 14.2 (98) | 13.8 (52) |
| Education | |||||
| HS graduate or less | 29.4 (319) | 25.8 (155) | 33.7 (164)** | 29.3 (206) | 29.5 (113) |
| Some college/tech school | 38.3 (416) | 37.0 (222) | 39.9 (194) | 40.0 (281) | 35.3 (135) |
| College graduate | 20.3 (220) | 23.0 (138) | 16.9 (82) | 19.8 (139) | 21.2 (81) |
| Advanced degree | 12.1 (131) | 14.2 (85) | 9.5 (46) | 11.0 (77) | 14.1 (54) |
| Amputation Characteristics | |||||
| Amputation Level | |||||
| Transfemoral | 31.7 (346) | 39.2 (237) | 22.4 (109)*** | -- | -- |
| Knee Disarticulation | 3.7 (40) | 4.8 (29) | 2.3 (11) | -- | -- |
| Transtibial | 63.5 (693) | 54.5 (329) | 74.7 (364) | -- | -- |
| Ankle Disarticulation | 1.1 (12) | 1.5 (9) | 0.6 (3) | -- | -- |
| Amputation Etiology | |||||
| Trauma | 55.4 (604) | -- | -- | 47.9 (338) | 68.9 (266)*** |
| Dysvascular | 44.6 (487) | -- | -- | 52.1 (367) | 31.1 (120) |
| Age at amputation (years) | 43.1 (17.6) | 33.8 (15.6) | 54.7 (12.4)*** | 44.5 (17.0) | 40.6 (18.5)*** |
| Years since amputation | 11.8 (14.0) | 17.2 (16.2) | 5.1 (5.5)*** | 10.8 (12.9) | 13.6 (15.6)** |
| Daily prosthesis use (hours) | 12.4 (4.1) | 13.4 (3.6) | 11.3 (4.4)*** | 12.9 (3.9) | 11.6 (4.4)*** |
| Health Characteristics | |||||
| Comorbid Health Conditions | |||||
| Asthma | 8.9 (96) | 9.7 (58) | 7.9 (38) | 9.1 (64) | 8.3 (32) |
| Arthritis | 25.6 (276) | 22.2 (132) | 29.9 (144)** | 26.4 (184) | 24.2 (92) |
| Cancer | 4.3 (47) | 3.0 (18) | 6.0 (29)* | 4.1 (29) | 4.7 (18) |
| Diabetes | 35.6 (388) | 6.3 (38) | 71.9 (350)*** | 45.7 (322) | 17.1 (66)*** |
| Digestive problems | 5.7 (62) | 4.1 (25) | 7.6 (37)* | 5.8 (41) | 5.4 (21) |
| Heart trouble | 16.4 (178) | 4.2 (25) | 31.5 (153)*** | 18.2 (128) | 13.0 (50)* |
| HIV or AIDS | 0.6 (7) | 0.5 (3) | 0.8 (4) | 0.7 (5) | 0.5 (2) |
| Kidney disease | 7.8 (85) | 0.7 (4) | 16.6 (81)*** | 10.4 (73) | 3.1 (12)*** |
| Liver Problems | 1.6 (17) | 1.0 (6) | 2.3 (11) | 1.1 (8) | 2.3 (9) |
| Stroke | 2.7 (29) | 0.8 (5) | 4.9 (24)*** | 2.8 (20) | 2.3 (9) |
| Number of Comorbid Conditions | |||||
| 0 | 37.0 (404) | 59.8 (361) | 8.8 (43)*** | 31.6 (223) | 46.9 (181)*** |
| 1 | 34.1 (372) | 30.6 (185) | 38.4 (187) | 33.9 (239) | 34.5 (133) |
| 2 | 16.8 (183) | 7.6 (46) | 28.1 (137) | 19.0 (134) | 12.7 (49) |
| ≥3 | 12.1 (132) | 2.0 (12) | 24.6 (120) | 15.5 (109) | 6.0 (23) |
| Average pain intensity | 3.4 (2.4) | 3.2 (2.4) | 3.6 (2.4)* | 3.4 (2.4) | 3.2 (2.3) |
Numbers may not add to total because of missing data and percentages may total more than 100% due to rounding.
Dysvascular mean/distribution significantly different from trauma mean/distribution or TFA mean/distribution significantly different from TTA mean/distribution at:
= p < 0.05;
= p < 0.01;
= p < 0.001.
The demographic characteristics of the sample differ significantly based on etiology and level of amputation. People with dysvascular LLL were on average 8 years older, had their amputation about 20 years later in life, and their time since amputation was 12 years less compared to people with traumatic LLL.
In addition, more than twice as many people with traumatic LLL were employed and 20% fewer had annual incomes lower than $25,000 compared to people with dysvascular LLL. Groups based on level of LLL were similar, although people with TFA were about 4 years younger when they had their amputation and were 15% more likely to report no comorbid conditions compared to people with TTA (Table 1).
Comparisons of health domains
The parametric and non-parametric statistical significance statistics were consistent except for 2 comparisons. PROMIS depression score for people with dysvascular etiology compared to the normative sample was found to be statistically significant using non-parametric statistics and the depression score of people with traumatic etiology compared to the normative sample was not significant using non-parametric tests, but was found significant using parametric statistic. For ease of interpretation parametric statistics with Bonferroni adjusted alpha levels30 are provided (Tables 2 and 3).
Table 2.
Pairwise comparisons to PROMIS norms for HRQOL indicators and symptoms
| Domain | Group | M | SD | Comparison value | 95% CI of the difference | t | df |
|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||
| Physical function | overall | 41.85 | 8.34 | 50.00 | −8.64, −7.65 | −32.23** | 1087 |
| Transfemoral | 40.54 | 7.56 | 50.00 | −10.22, −8.70 | −24.54** | 383 | |
| Transtibial | 42.57 | 8.66 | 50.00 | −8.07, −6.79 | −22.78** | 703 | |
| Dysvascular | 38.52 | 7.48 | 50.00 | −12.15, −10.81 | −33.81** | 484 | |
| Trauma | 44.53 | 8.03 | 50.00 | −6.11, −4.83 | −16.73** | 602 | |
| Anxiety | overall | 49.41 | 9.49 | 50.00 | −1.16, −0.03 | −2.07 | 1089 |
| Transfemoral | 49.76 | 9.60 | 50.00 | −1.20, 0.73 | −0.48 | 385 | |
| Transtibial | 49.21 | 9.42 | 50.00 | −1.49, −0.09 | −2.23 | 703 | |
| Dysvascular | 50.37 | 9.59 | 50.00 | −0.49, 1.22 | 0.84 | 485 | |
| Trauma | 48.63 | 9.34 | 50.00 | −2.11, −0.62 | −3.60** | 603 | |
| Depression | overall | 49.29 | 9.31 | 50.00 | −1.26, −0.15 | −2.50 | 1089 |
| Transfemoral | 49.42 | 9.33 | 50.00 | −1.52, 0.35 | −1.23 | 385 | |
| Transtibial | 49.23 | 9.31 | 50.00 | −1.46, −0.08 | −2.20 | 703 | |
| Dysvascular | 50.47 | 9.69 | 50.00 | −0.40, 1.33 | 1.07 | 485 | |
| Trauma | 48.35 | 8.90 | 50.00 | −2.36, −0.94 | −4.55** | 603 | |
| Fatigue | overall | 48.47 | 9.37 | 50.00 | −2.09, −0.98 | −5.39** | 1086 |
| Transfemoral | 47.85 | 9.00 | 50.00 | −3.05, −1.25 | −4.68** | 384 | |
| Transtibial | 48.80 | 9.56 | 50.00 | −1.90, −0.49 | −3.32** | 701 | |
| Dysvascular | 49.64 | 8.87 | 50.00 | −1.15, 0.44 | −0.88 | 483 | |
| Trauma | 47.52 | 9.66 | 50.00 | −3.25, −1.71 | −6.30** | 602 | |
| Sleep disturbance | overall | 49.39 | 9.05 | 50.00 | −1.15, −0.07 | −2.22 | 1087 |
| Transfemoral | 49.28 | 9.10 | 50.00 | −1.64, 0.19 | −1.55 | 383 | |
| Transtibial | 49.45 | 9.02 | 50.00 | −1.21, 0.12 | −1.61 | 703 | |
| Dysvascular | 49.75 | 9.49 | 50.00 | −1.10, 0.60 | −0.58 | 484 | |
| Trauma | 49.10 | 8.67 | 50.00 | −1.59, −0.20 | −2.54 | 602 | |
| Satisfaction with social roles | overall | 47.95 | 9.92 | 50.00 | −2.64, −1.46 | −6.81** | 1089 |
| Transfemoral | 48.09 | 9.33 | 50.00 | −2.84, −0.98 | −4.02** | 385 | |
| Transtibial | 47.88 | 10.23 | 50.00 | −2.88, −1.36 | −5.50** | 703 | |
| Dysvascular | 45.58 | 9.30 | 50.00 | −5.25, −3.59 | −10.48** | 485 | |
| Trauma | 49.86 | 9.99 | 50.00 | −0.93, 0.66 | −0.33 | 603 | |
| Pain interference | overall | 54.83 | 8.91 | 50.00 | 4.30, 5.36 | 17.87** | 1087 |
| Transfemoral | 54.08 | 8.79 | 50.00 | 3.20, 4.96 | 9.10** | 384 | |
| Transtibial | 55.24 | 8.96 | 50.00 | 4.58, 5.90 | 15.50** | 702 | |
| Dysvascular | 55.74 | 8.76 | 50.00 | 4.95, 6.52 | 14.41** | 483 | |
| Trauma | 54.10 | 8.98 | 50.00 | 3.38, 4.82 | 11.22** | 603 | |
Notes. We used bonferroni adjusted alpha levels of 0.01 (0.05/5) for five pariwise comparisons for each measure
= p < 0.01.
Table 3.
Pairwise comparisons between subgroups based on amputation level and etiology for HRQOL indicators and symptoms
| Domain | Amputation Level | 95% CI | t | df | Amputation Etiology | 95% CI | t | df | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Transfemoral
|
Transtibial
|
Dysvascular
|
Trauma
|
||||||||||||||||
| M | SD | n | M | SD | n | M | SD | n | M | SD | n | ||||||||
|
|
|
||||||||||||||||||
| Physical function | 40.54 | 7.56 | 384 | 42.57 | 8.66 | 704 | −3.06, −1.00 | −3.86** | 1086 | 38.52 | 7.48 | 485 | 44.53 | 8.03 | 603 | −6.95, −5.08 | −12.66** | 1086 | |
| Anxiety | 49.76 | 9.60 | 386 | 49.21 | 9.42 | 704 | −0.62, 1.73 | 0.92 | 1088 | 50.37 | 9.59 | 486 | 48.63 | 9.34 | 604 | 0.60, 2.87 | 3.01** | 1088 | |
| Depression | 49.42 | 9.33 | 386 | 49.23 | 9.31 | 704 | −0.97, 1.35 | 0.32 | 1088 | 50.47 | 9.69 | 486 | 48.35 | 8.90 | 604 | 1.01, 3.23 | 3.75** | 1088 | |
| Fatigue | 47.85 | 9.00 | 385 | 48.80 | 9.56 | 702 | −2.12, 0.21 | −1.60 | 1085 | 49.64 | 8.87 | 484 | 47.52 | 9.66 | 603 | 1.01, 3.24 | 3.73** | 1085 | |
| Sleep disturbance | 49.28 | 9.10 | 384 | 49.45 | 9.02 | 704 | −1.30, 0.95 | −0.31 | 1086 | 49.75 | 9.49 | 485 | 49.10 | 8.67 | 603 | −0.44, 1.73 | 1.17 | 1086 | |
| Satisfaction with social roles | 48.09 | 9.33 | 386 | 47.88 | 10.23 | 704 | −1.02, 1.44 | 0.34 | 1088 | 45.58 | 9.30 | 486 | 49.86 | 9.99 | 604 | −5.44, −3.13 | −7.26** | 1088 | |
| Pain interference | 54.08 | 8.79 | 385 | 55.24 | 8.96 | 703 | −2.27, −0.05 | −2.06 | 1086 | 55.74 | 8.76 | 484 | 54.10 | 8.98 | 604 | 0.57, 2.70 | 3.02** | 1086 | |
|
|
|
|
|
||||||||||||||||
Notes. we used bonferroni adjusted alpha levels of 0.025 (0.05/2) for two pariwise comparisons for each measure
= p < 0.025;
= p < 0.01.
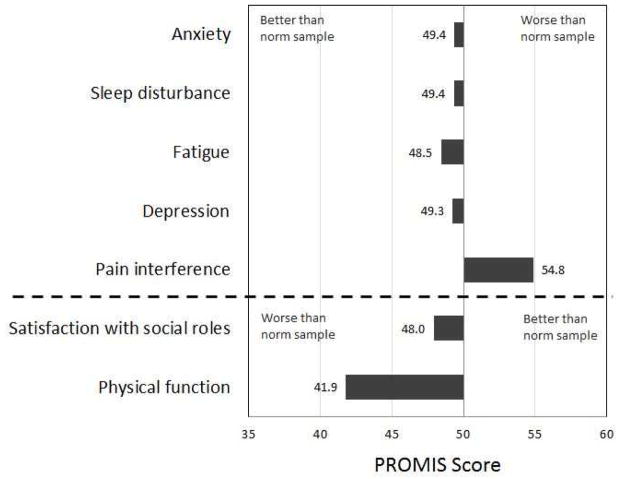
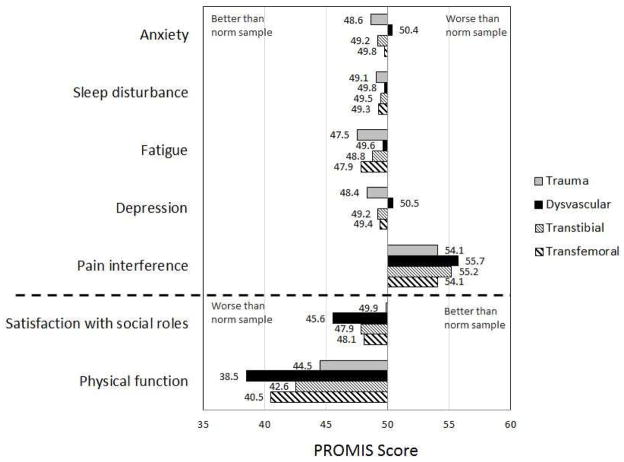
Comparisons between People with LLL and the Norm
The health profile for the overall sample is shown in Figure 1, and the health profiles by amputation level and etiology are shown in Figure 2. People with LLL reported significantly different scores than the norm in four of the seven health domains assessed. Specifically, mean scores for people with LLL were about 8 points lower for physical function, 2 points lower for fatigue and satisfaction with participation in social roles, and 5 points higher for pain interference than the norm. Our sample did not significantly differ (i.e., differences less than 1 point) from the norm in reported anxiety, depression, or sleep disturbance.
Fig. 1.
PROMIS Profile-29 scores for the overall sample of people with LLL (N=1091). The bars represent the mean score in each domain. Scores above 50 indicate that the sample of people with LLL had more of the measured construct (e.g., anxiety, sleep disturbance) and scores below 50 indicate that the sample of people with LLL had less of the measured construct. 50 represents the mean of the large samples representative of the US general population, except for sleep disturbance where 50 represents a mean of a large sample that includes a slightly higher proportion of less healthy people than the general population.
Fig. 2.
PROMIS Profile-29 scores for subgroups based on etiology and level of amputation. Bars represent the mean score in each domain. Scores above 50 indicate that the sample of people with LLL had more of the measured construct (e.g., anxiety, sleep disturbance) and scores below 50 indicate that the sample of people with LLL had less of the measured construct.
All subgroups (TFA and TTA levels; traumatic and dysvascular amputation etiologies) had physical function scores between 6–12 points lower and pain interference scores 4–6 points higher than the norm. The subgroup with amputation from trauma reported significantly less anxiety, depression, and fatigue than did the norm. However, differences were relatively small (~1, 2, and 3 points, respectively). Similarly, both subgroups defined by level of amputation reported less fatigue and satisfaction with social roles (between 1 and 2 points) compared to the norm. People with amputation from dysvascular etiology reported lower satisfaction with participation in social roles (difference of about 4 points) than the normative sample. No significant differences were found for sleep disturbance between subgroups with LLL and the normative sample (Table 2).
Comparisons between Subgroups Defined by Amputation Level and Etiology
All amputation subgroups differed significantly in physical function scores. Participants with TTA and traumatic etiologies had higher physical function than participants with TFA and dysvascular etiologies, respectively (etiology: 6 points, level: 2 points). The differences in physical function scores remained statistically significant after controlling for demographic and clinical characteristics. However, the adjusted mean difference increased from 2 to 3 points for level and decreased from 6 to 3 points for etiology (Appendix 1). The direction of the differences were maintained (i.e., people with TTA and traumatic etiologies had higher physical function than their counterparts).
Appendix 1.
Summary of the multiple regression analyses with the PROMIS-29 T-scores as dependent variables and demographic and clinical characteristics as independent variables
| Dependent variable | Independent variable | Unstandardized coefficient (B) | SE B | Standardized coefficient (β) | p | R2 | Adjusted R2 |
|---|---|---|---|---|---|---|---|
| Physical function | (Intercept) | 45.72 | 1.25 | - | <.0001 | 0.26 | 0.26 |
| Amputation transtibiala | 3.29 | 0.47 | 0.19 | <.0001 | |||
| Traumatic etiologyb | 3.34 | 0.56 | 0.20 | <.0001 | |||
| Female gender | −2.11 | 0.48 | −0.12 | <.0001 | |||
| Non-Hispanic blackc | −1.52 | 0.78 | −0.05 | 0.05 | |||
| Hispanicc | −2.79 | 0.92 | −0.08 | 0.00 | |||
| Other ethnicityc | −3.10 | 1.11 | −0.07 | 0.01 | |||
| Years since amputation | 0.16 | 0.02 | 0.27 | <.0001 | |||
| Age | −0.16 | 0.02 | −0.25 | <.0001 | |||
|
| |||||||
| Anxiety | (Intercept) | 53.16 | 1.60 | - | <.0001 | 0.06 | 0.06 |
| Amputation transtibiala | −0.90 | 0.60 | −0.05 | 0.13 | |||
| Traumatic etiologyb | −0.87 | 0.72 | −0.05 | 0.22 | |||
| Female gender | 2.33 | 0.62 | 0.11 | 0.00 | |||
| Non-Hispanic blackc | 1.52 | 0.99 | 0.05 | 0.13 | |||
| Hispanicc | 1.19 | 1.18 | 0.03 | 0.31 | |||
| Other ethnicityc | 2.57 | 1.40 | 0.05 | 0.07 | |||
| Years since amputation | −0.11 | 0.02 | −0.16 | <.0001 | |||
| Age | −0.04 | 0.02 | −0.06 | 0.07 | |||
|
| |||||||
| Depression | (Intercept) | 53.90 | 1.57 | - | <.0001 | 0.06 | 0.06 |
| Amputation transtibiala | −0.67 | 0.59 | −0.03 | 0.26 | |||
| Traumatic etiologyb | −1.46 | 0.70 | −0.08 | 0.04 | |||
| Female gender | 1.65 | 0.61 | 0.08 | 0.01 | |||
| Non-Hispanic blackc | 0.31 | 0.97 | 0.01 | 0.75 | |||
| Hispanicc | 1.07 | 1.16 | 0.03 | 0.35 | |||
| Other ethnicityc | 3.90 | 1.38 | 0.08 | 0.00 | |||
| Years since amputation | −0.10 | 0.02 | −0.16 | <.0001 | |||
| Age | −0.05 | 0.02 | −0.08 | 0.03 | |||
|
| |||||||
| Fatigue | (Intercept) | 50.89 | 1.58 | - | <.0001 | 0.06 | 0.06 |
| Amputation transtibiala | 0.35 | 0.59 | 0.02 | 0.55 | |||
| Traumatic etiologyb | −1.01 | 0.71 | −0.05 | 0.15 | |||
| Female gender | 2.23 | 0.61 | 0.11 | 0.00 | |||
| NonHispanic blackc | −1.34 | 0.98 | −0.04 | 0.17 | |||
| Hispanicc | −1.01 | 1.17 | −0.03 | 0.39 | |||
| Other ethnicityc | 2.48 | 1.39 | 0.05 | 0.07 | |||
| Years since amputation | −0.12 | 0.02 | −0.17 | <.0001 | |||
| Age | −0.02 | 0.02 | −0.03 | 0.34 | |||
|
| |||||||
| Sleep disturbance | (Intercept) | 55.16 | 1.55 | - | <.0001 | 0.04 | 0.03 |
| Amputation transtibiala | 0.01 | 0.58 | 0.00 | 0.99 | |||
| Traumatic etiologyb | −0.83 | 0.69 | −0.05 | 0.23 | |||
| Female gender | 1.17 | 0.60 | 0.06 | 0.05 | |||
| Non-Hispanic blackc | −0.43 | 0.96 | −0.01 | 0.65 | |||
| Hispanicc | −0.68 | 1.14 | −0.02 | 0.55 | |||
| Other ethnicityc | 2.84 | 1.35 | 0.06 | 0.04 | |||
| Years since amputation | −0.05 | 0.02 | −0.08 | 0.02 | |||
| Age | −0.09 | 0.02 | −0.14 | <.0001 | |||
|
| |||||||
| Satisfaction with social role | (Intercept) | 48.99 | 1.65 | - | <.0001 | 0.09 | 0.08 |
| Amputation transtibiala | 0.75 | 0.62 | 0.04 | 0.23 | |||
| Traumatic etiologyb | 2.33 | 0.74 | 0.12 | 0.00 | |||
| Female gender | −0.47 | 0.64 | −0.02 | 0.46 | |||
| Non-Hispanic blackc | 0.89 | 1.03 | 0.03 | 0.39 | |||
| Hispanicc | −2.79 | 1.22 | −0.07 | 0.02 | |||
| Other ethnicityc | −3.20 | 1.45 | −0.07 | 0.03 | |||
| Years since amputation | 0.14 | 0.02 | 0.19 | <.0001 | |||
| Age | −0.07 | 0.03 | −0.10 | 0.00 | |||
|
| |||||||
| Pain interference | (Intercept) | 56.52 | 1.51 | - | <.0001 | 0.06 | 0.05 |
| Amputation transtibiala | 0.89 | 0.57 | 0.05 | 0.12 | |||
| Traumatic etiologyb | −0.66 | 0.68 | −0.04 | 0.33 | |||
| Female gender | 1.74 | 0.58 | 0.09 | 0.00 | |||
| Non-Hispanic blackc | 1.27 | 0.94 | 0.04 | 0.18 | |||
| Hispanicc | 2.33 | 1.11 | 0.06 | 0.04 | |||
| Other ethnicityc | 3.13 | 1.32 | 0.07 | 0.02 | |||
| Years since amputation | −0.09 | 0.02 | −0.15 | <.0001 | |||
| Age | −0.03 | 0.02 | −0.05 | 0.18 | |||
Note:
Reference group: Amputation transfemoral;
Reference group: Dysvascular etiology;
Reference group: non-Hispanic white.
Significant differences were also observed between etiology subgroups in five of the six remaining domains: anxiety, depression, fatigue, pain interference (about 2 points each), and satisfaction with social roles (4 points). For these domains, people with traumatic etiology had better health indicators than people with dysvascular etiology. However, only satisfaction with social roles remained significant after adjusting for demographic and clinical variables, with an adjusted mean difference of 2 points (Appendix 1). No further significant differences were observed between subgroups based on amputation level. In addition, no significant differences were observed between any of the subgroups for sleep disturbance (Table 3).
Discussion
The purpose of this study was to examine health indicators in a large sample of people with LLL by comparing overall and subgroup scores to the norm scores and quantifying differences between subgroups based on etiology and level of amputation. Similar to reports in previous literature,24,31 participants with dysvascular LLL were significantly older, had more recent limb loss, and reported a greater number of comorbidities than participants with traumatic LLL. Additionally, people with TFA had significantly longer time since limb loss and were generally healthier than people with TTA, likely because a greater proportion of people in our TTA sample had dysvascular LLL.
Consistent with our hypotheses, participants with LLL reported worse health indicators compared to the norm that represents the U.S. general population on several health domains with the biggest differences observed on physical function. Our finding that etiology was associated with more health indicators than amputation level contrasts with findings from a review that concluded that higher levels of amputation were associated with increased anxiety, social discomfort, and depression while etiology had weak or no associations with these outcomes.10
Physical Function
Pronounced differences in physical function were observed between people with LLL and the norm, and indicate that people with LLL have considerably lower self-reported physical function than the general U.S. population. Participants with LLL, in general, had physical function scores that were more than a half standard deviation (i.e., 8 points) lower than the average score for the norm. This difference in scores exceeds established minimally important differences (MIDs) estimated for physical function in people with cancer (MID: 4–6 points)32 and rheumatoid arthritis (MID: 2),33 suggesting that this difference is clinically meaningful. Such differences in self-reported physical function between people with and without LLL are consistent with previous findings.1–3 Additionally, participants with TTA and traumatic etiologies had higher physical function scores than participants with TFA and dysvascular etiologies.
Pain Interference and Fatigue
Overall and subgroup scores for participants with LLL were significantly worse than the norm for pain interference, indicating that people with LLL have greater pain that interferes with participation in life activities than the general population. Differences between group scores were approximately 5 points, which are within the established MID of 4–6 points.32 Previous studies have found greater experiences of pain in people with LLL compared to people without LLL,1,2,34,35 and one study found that more than 90% of 255 participants with LLL reported chronic experiences with pain.11 Additionally, participants with dysvascular etiology had significantly greater pain interference than people with traumatic etiology. However, neither the level of amputation or etiology were statistically significantly associated with pain interference after controlling for demographic and clinical characteristics.
Participants with LLL in our study reported less fatigue than the norm. In addition, subgroups based on level and etiology of amputation had lower fatigue scores than the norm, with the exception of the subgroup with dysvascular amputation etiology. The overall finding that fatigue is lower in people with LLL than people without LLL is contrary to results of previous research.1,36 It is possible that lower fatigue in people with LLL may be due to lower physical activity, however, differences reported in our study were generally small (i.e., between 1–3 points) and are unlikely to be clinically meaningful.
Social Health, Anxiety, Depression, and Sleep Disturbance
People with dysvascular LLL reported satisfaction with social roles over 4 points lower than both the norm and people with traumatic LLL. Although MID has not been estimated for this measure, an alternative and commonly used option is to use 0.5 of a standard deviation as a clinically meaningful difference,37 which is 5 points for PROMIS instruments. Thus, these scores approximate a clinically meaningful difference in social role satisfaction between people with dysvascular LLL and the general population and support findings from previous research.14 Traumatic etiology was significantly associated with satisfaction with social roles after controlling for demographic and clinical characteristics, however the difference may no longer be clinically significant. The overall sample did not significantly differ from the U.S. general population in anxiety, depression, or sleep disturbance.
Overall, our results suggest that limb loss is associated with generally worse health when compared to a normative sample: physical function, satisfaction with social roles and pain interference were most negatively affected. Level of amputation is associated with worse physical function and etiology of amputation is associated with both physical function and satisfaction with social roles. However in the regression models, time since amputation was the best predictor for most health indicators in people with LLL with greater time since amputation associated with better health outcomes.
Study Limitations
The sampling strategy for this study was selected for the primary purpose of PLUS-M instrument development. As a result, the sample is not representative of the population of persons with LLL in the U.S. For example, the majority of the sample had amputation secondary to trauma whereas, in the U.S., the majority of people with LLL have amputation secondary to dysvascular etiology.24,38 Because people with LLL from dysvascular etiology reported worse health than people with LLL from traumatic causes in this study, it is likely that the profiles based on these data present better health and higher function than a profile based on a more representative sample. Therefore, it is possible that differences between the norms and scores of people with LLL are underestimated in this study. In addition, only English speakers were included in the study due to the limited funds. Thus the results cannot be generalized to the people with LLL with limited English proficiency.
In addition, MIDs, which assist in determining the clinical meaningfulness of statistically significant mean differences, have not been established for PROMIS instruments in people with LLL. The MIDs used to interpret data presented in this manuscript were based on those established in people with cancer32 and arthritis.33 Thus, these MID estimates should be used with caution as they may not accurately describe MIDs for people with LLL. Further, to our knowledge, there are no established MIDs in any population for PROMIS measures of satisfaction with social roles and sleep disturbance.
Finally, pain in people with LLL often presents in ways unique to this population. People with LLL commonly experience phantom and residual limb pain,10 which cannot be assessed with a general measure of health such as PROMIS-29. The lack of specific pain measurement limits discussion on differences in pain type between subgroups of people with LLL, however, it allows for comparisons to normative sample.
Conclusions
Health indicator profiles provide clinically meaningful information and can be used to efficiently examine numerous aspects of self-reported health in people with LLL. Results suggest that people with LLL generally report worse physical function, satisfaction with social roles, and pain interference when compared to the general population. Additionally, people with dysvascular amputation report worse physical function and satisfaction with social roles than people with traumatic amputation. The large number of participants with LLL in this study is rare in the limb loss literature and strengthens these conclusions.
Acknowledgments
Funding: This research is supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NIH grant number HD-065340).
Abbreviations
- IRT
item response theory
- LLL
lower limb loss
- MID
minimal important difference
- PLUS-M
Prosthetic Limb Users Survey of Mobility
- PROMIS
Patient-Reported Outcomes Measurement Information System
- TFA
transfemoral amputation
- TTA
transtibial amputation
- U.S.
United States
Footnotes
Previous Presentation of Material:
Hafner BJ, Amtmann D, Abrahamson DC, Morgan SJ, Kajlich AJ, Salem R. Patient reported outcome measurement information system profiles of persons with lower limb loss. Proceedings of the American Academy of Orthotists & Prosthetists (AAOP) 39th Annual Meeting and Scientific Symposium, Orlando, FL, February 20–23, 2013.
Hafner BJ, Amtmann D, Abrahamson DC, Morgan SJ, Kajlich AJ, Salem R. Health profiles of persons with lower limb loss. Proceedings of the 14th World Congress of the International Society of Prosthetics and Orthotics, Hyderabad, India, February 4–7, 2013
Amtmann D, Abrahamson DA, Morgan SJ, Salem R, Askew RL, Hafner BJ. Symptoms and quality of life indicators of persons with lower limb loss. Proceedings of the ISOQOL 19th Annual Conference, Budapest, Hungary, October 24–27, 2012
Conflicts of interest: The authors report no conflicts of interest. They do acknowledge funding for this research through the National Institute of Child Health and Human Development (as stated above).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Pell JP, Donnan PT, Fowkes FG, Ruckley CV. Quality of life following lower limb amputation for peripheral arterial disease. Eur J Vasc Surg. 1993 Jul;7(4):448–451. doi: 10.1016/s0950-821x(05)80265-8. [DOI] [PubMed] [Google Scholar]
- 2.Pezzin LE, Dillingham TR, MacKenzie EJ. Rehabilitation and the long-term outcomes of persons with trauma-related amputations. Arch Phys Med Rehabil. 2000 Mar;81(3):292–300. doi: 10.1016/s0003-9993(00)90074-1. [DOI] [PubMed] [Google Scholar]
- 3.Fortington LV, Dijkstra PU, Bosmans JC, Post WJ, Geertzen JH. Change in health-related quality of life in the first 18 months after lower limb amputation: a prospective, longitudinal study. J Rehabil Med. 2013 Jun;45(6):587–594. doi: 10.2340/16501977-1146. [DOI] [PubMed] [Google Scholar]
- 4.Zidarov D, Swaine B, Gauthier-Gagnon C. Quality of life of persons with lower-limb amputation during rehabilitation and at 3-month follow-up. Arch Phys Med Rehabil. 2009 Apr;90(4):634–645. doi: 10.1016/j.apmr.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 5.Penn-Barwell JG. Outcomes in lower limb amputation following trauma: A systematic review and meta-analysis. Injury. 2011;42(12):1474–1479. doi: 10.1016/j.injury.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 6.Davies B, Datta D. Mobility outcome following unilateral lower limb amputation. Prosthet Orthot Int. 2003 Dec;27(3):186–190. doi: 10.1080/03093640308726681. [DOI] [PubMed] [Google Scholar]
- 7.Sansam K, Neumann V, O’Connor R, Bhakta B. Predicting walking ability following lower limb amputation: a systematic review of the literature. J Rehabil Med. 2009 Jul;41(8):593–603. doi: 10.2340/16501977-0393. [DOI] [PubMed] [Google Scholar]
- 8.Burger H, Marincek C, Isakov E. Mobility of persons after traumatic lower limb amputation. Disabil Rehabil. 1997 Jul;19(7):272–277. doi: 10.3109/09638289709166538. [DOI] [PubMed] [Google Scholar]
- 9.Czerniecki JM, Turner AP, Williams RM, Hakimi KN, Norvell DC. Mobility changes in individuals with dysvascular amputation from the presurgical period to 12 months postamputation. Arch Phys Med Rehabil. 2012 Oct;93(10):1766–1773. doi: 10.1016/j.apmr.2012.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Horgan O, MacLachlan M. Psychosocial adjustment to lower-limb amputation: a review. Disability and Rehabilitation. 2004;26(14–15):837–850. doi: 10.1080/09638280410001708869. Jul 22–Aug 5. [DOI] [PubMed] [Google Scholar]
- 11.Ehde DM, Czerniecki JM, Smith DG, et al. Chronic phantom sensations and pain following lower extremity amputation. Arch Phys Med Rehabil. 2000 Aug;81:1039–1044. doi: 10.1053/apmr.2000.7583. [DOI] [PubMed] [Google Scholar]
- 12.Ehde DM, Smith DG, Czerniecki JM, Campbell KM, Malchow DM, Robinson RLR. Back pain as a secondary disability in persons with lower limb amputations. Arch Phys Med Rehabil. 2001 Jun;82(6):731–734. doi: 10.1053/apmr.2001.21962. [DOI] [PubMed] [Google Scholar]
- 13.Gailey R, Allen K, Castles J, Kucharik J, Roeder M. Review of secondary physical conditions associated with lower-limb amputation and long-term prosthesis use. J Rehabil Res Dev. 2008;45(1):15–29. doi: 10.1682/jrrd.2006.11.0147. [DOI] [PubMed] [Google Scholar]
- 14.Demet K, Martinet N, Guillemin F, Paysant J, Andre JM. Health related quality of life and related factors in 539 persons with amputation of upper and lower limb. Disabil Rehabil. 2003 May 6;25(9):480–486. doi: 10.1080/0963828031000090434. [DOI] [PubMed] [Google Scholar]
- 15.Deans SA, McFadyen AK, Rowe PJ. Physical activity and quality of life: A study of a lower-limb amputee population. Prosthet Orthot Int. 2008 Jun;32(2):186–200. doi: 10.1080/03093640802016514. [DOI] [PubMed] [Google Scholar]
- 16.Schaffalitzky E, Gallagher P, Maclachlan M, Ryall N. Understanding the benefits of prosthetic prescription: exploring the experiences of practitioners and lower limb prosthetic users. Disability and Rehabilitation. 2011;33(15–16):1314–1323. doi: 10.3109/09638288.2010.529234. [DOI] [PubMed] [Google Scholar]
- 17.Duncan EA, Murray J. The barriers and facilitators to routine outcome measurement by allied health professionals in practice: a systematic review. BMC Health Serv Res. 2012;12:96. doi: 10.1186/1472-6963-12-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jette DU, Halbert J, Iverson C, Miceli E, Shah P. Use of standardized outcome measures in physical therapist practice: perceptions and applications. Phys Ther. 2009 Feb;89(2):125–135. doi: 10.2522/ptj.20080234. [DOI] [PubMed] [Google Scholar]
- 19.Cella D, Riley W, Stone A, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. Journal of Clinical Epidemiology. 2010;63(11):1179–1194. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sinha R, van den Heuvel WJ, Arokiasamy P. Factors affecting quality of life in lower limb amputees. Prosthetics and Orthotics International. 2011 Mar;35(1):90–96. doi: 10.1177/0309364610397087. [DOI] [PubMed] [Google Scholar]
- 21.Hawkins AT, Henry AJ, Crandell DM, Nguyen LL. A systematic review of functional and quality of life assessment after major lower extremity amputation. Ann Vasc Surg. 2014 Apr;28(3):763–780. doi: 10.1016/j.avsg.2013.07.011. [DOI] [PubMed] [Google Scholar]
- 22.Cook KF, Choi SW, Crane PK, Deyo RA, Johnson KL, Amtmann D. Letting the CAT out of the bag: comparing computer adaptive tests and an 11-item short form of the Roland-Morris Disability Questionnaire. Spine. 2008 May 20;33(12):1378–1383. doi: 10.1097/BRS.0b013e3181732acb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dillingham TR, Pezzin LE, Mackenzie EJ. Racial differences in the incidence of limb loss secondary to peripheral vascular disease: a population-based study. Arch Phys Med Rehabil. 2002 Sep;83(9):1252–1257. doi: 10.1053/apmr.2002.34805. [DOI] [PubMed] [Google Scholar]
- 24.Ziegler-Graham K, MacKenzie EJ, Ephraim PL, Travison TG, Brookmeyer R. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008 Mar;89(3):422–429. doi: 10.1016/j.apmr.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 25.Liu H, Cella D, Gershon R, et al. Representativeness of the Patient-Reported Outcomes Measurement Information System Internet panel. J Clin Epidemiol. 2010 Nov;63(11):1169–1178. doi: 10.1016/j.jclinepi.2009.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patient Reported Outcomes Measurement Information System. [Accessed Accessed December 12, 2014];PROMIS Adult Profile Instruments. 2014 http://www.assessmentcenter.net.
- 27.Posten HO. The robustness of the two—sample t—test over the Pearson system. Journal of Statistical Computation and Simulation 1978. 1978 Jan 01;6(3–4):295–311. [Google Scholar]
- 28.Posten HO, Cheng Yeh H, Owen DB. Robustness of the two-sample t-test under violations of the homogeneity of variance assumption. Communications in Statistics - Theory and Methods 1982. 1982 Jan 01;11(2):109–126. [Google Scholar]
- 29.Rasch D, Guiard V. The robustness of parametric statistical methods. Psychology Science. 2004;46:175–208. [Google Scholar]
- 30.Bland JM, Altman DG. Multiple significance tests: the Bonferroni method. BMJ. 1995;310:170. doi: 10.1136/bmj.310.6973.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dillingham TR, Pezzin LE, Shore AD. Reamputation, mortality, and health care costs among persons with dysvascular lower-limb amputations. Arch Phys Med Rehabil. 2005 Mar;86(3):480–486. doi: 10.1016/j.apmr.2004.06.072. [DOI] [PubMed] [Google Scholar]
- 32.Yost KJ, Eton DT, Garcia SF, Cella D. Minimally important differences were estimated for six Patient-Reported Outcomes Measurement Information System-Cancer scales in advanced-stage cancer patients. J Clin Epidemiol. 2011 May;64(5):507–516. doi: 10.1016/j.jclinepi.2010.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hays RD, Spritzer KL, Fries JF, Krishnan E. Responsiveness and minimally important difference for the Patient-Reported Outcomes Measurement Information System (PROMIS) 20-item physical functioning short form in a prospective observational study of rheumatoid arthritis. Ann Rheum Dis. 2015;74(1):104–7. doi: 10.1136/annrheumdis-2013-204053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hagberg K, Branemark R. Consequences of non-vascular trans-femoral amputation: a survey of quality of life, prosthetic use and problems. Prosthet Orthot Int. 2001 Dec;25(3):186–194. doi: 10.1080/03093640108726601. [DOI] [PubMed] [Google Scholar]
- 35.Davidson JH, Khor KE, Jones LE. A cross-sectional study of post-amputation pain in upper and lower limb amputees, experience of a tertiary referral amputee clinic. Disabil Rehabil. 2010;32(22):1855–1862. doi: 10.3109/09638281003734441. [DOI] [PubMed] [Google Scholar]
- 36.Hoogendoorn JM, van der Werken C. Grade III open tibial fractures: functional outcome and quality of life in amputees versus patients with successful reconstruction. Injury. 2001 May;32(4):329–334. doi: 10.1016/s0020-1383(00)00250-3. [DOI] [PubMed] [Google Scholar]
- 37.Farivar SS, Liu H, Hays RD. Half standard deviation estimate of the minimally important difference in HRQOL scores? Expert review of pharmacoeconomics & outcomes research. 2004 Oct;4(5):515–523. doi: 10.1586/14737167.4.5.515. [DOI] [PubMed] [Google Scholar]
- 38.Dillingham T, Pezzin L, MacKenzie EJ. Limb amputation and limb deficiency: epidemiology and recent trends in the United States. South Med J. 2002;95:875–883. doi: 10.1097/00007611-200208000-00018. [DOI] [PubMed] [Google Scholar]