Abstract
The adherence by patients to diabetic foot ulcer therapy is often difficult. The goal of this study was to begin to understand how a patient’s health literacy affects their foot ulcer management decisions. Initially using a cross-sectional study design, we evaluated diabetics with foot ulcers within 4 weeks of being asked to participate in a longitudinal study. We assessed health literacy using measures of general health literacy, diabetes health literacy, diabetes self-efficacy, and diabetes numeracy. Individuals enrolled in the study had higher health literacy based on the Short Test of Functional Health Literacy in Adults (33.8 (SD 2.3) versus 27.3 (SD 9.6); p=0.009) as compared to individuals who previously declined an invitation to enroll in the study. Furthermore, patients with lower Short Test of Functional Health Literacy in Adults scores had larger (p=0.04) and older (p=0.125) wounds (markers for poorer prognosis). Other measures of literacy showed similar results. In conclusion, those with diminished health literacy were less likely to enroll in an investigational study and had wounds that were less likely to heal.
To the editor
Nearly 90% of individuals with diabetes and lower extremity amputation (LEA) have histories of foot ulcers or have lower extremity findings consistent with peripheral arterial disease (PAD) and/or neuropathy(1). It is not clear that patients understand that these medical ailments are associated with LEA risk(2). The incidence of LEA varies widely in the US even after adjustment for socioeconomic factors like income, race, and physician availability(3). At least some of the geographic variation in LEA is associated with health screening behaviors and availability of diabetes education(4). However, overall the reason for the variation in LEA is unknown.
Health literacy is broadly defined as the degree to which individuals have the capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions (5,6). The goal of this study was to begin to understand how a patient’s health literacy affects their decisions as to how their foot ulcers are managed.
Methods
We conducted a cross-sectional study on subjects eligible for a study and then conducted a prospective cohort study on a smaller subset that had enrolled. The participants were patients with diabetes and foot ulcers treated in a wound care setting in Philadelphia. Those studied had either agreed to enroll in an ongoing longitudinal cohort clinical study designed to better understand processes associated with a healing wound (cohort study) or, were from the same clinical practices, but had declined enrollment into the ongoing longitudinal cohort study (Figure 1). In all cases, wound care was determined by the podiatrist and patient and not as part of a clinical study protocol.
Figure 1.
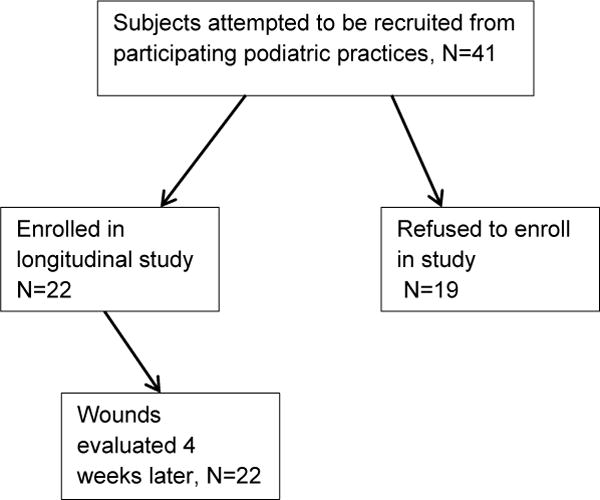
Flow diagram of the study
The health literacy of each subject was measured within four weeks of being offered enrollment into the longitudinal study. Specifically health literacy was evaluated as general health literacy, diabetes health literacy, diabetes self-efficacy, and diabetes numeracy using self-administered questionnaires. The primary measure of general health literacy was the Short Test of Functional Health Literacy in Adults (STOFHLA) (7). One wound care provider requested that this assessment not be conducted on his patients. For diabetes literacy and diabetic numeracy we used a previously validated tool by Brega et al (8,9). We also used a survey instrument to assess diabetes self-efficacy, the Perceived Diabetes Self-Management Scale (PDSMS) (10). Additional factors assessed in the cohort study included wound related findings like wound size, wound duration, and the natural log healing rate per week (for those enrolled in the cohort study) during their first four weeks of care(11,12).
All variables were described using means, medians, or percentages as appropriate. Correlations between literacy assessments were conducted using Pearson or chi-square Statistical comparisons between groups were conducted using chi-square, t-tests or linear regression as appropriate. Correlations between the literacy tests were assessed using Pearson’s correlation. All analyses were performed using Stata 13.1. This study was approved by the Institutional Review Board (IRB) of the University of Pennsylvania.
Results
Forty-one subjects were enrolled in the cross-sectional study, 22 (53.7%) also provided data for the prospective cohort study (Figure 1). The median age was 53.5 (interquartile range (IQR):47, 61.5) years. Sixty-three percent were male and 75% were African-American. Individuals enrolled in the cohort study had higher health literacy based on the STOFHLA as a continuous (33.8 (SD 2.3) versus 27.3 (SD 9.6); p=0.009) or categorical tool (p=0.04) as compared to individuals who did not enroll in the cohort study (Table 1). Individuals enrolled in the cohort study had greater diabetes numeracy (0.71 (SD 0.26) versus 0.55(SD 0.32) p= 0.02). However, the other measures of literacy as determined by diabetes literacy (p=0.58) or diabetes self-efficacy (p=0.29) did not statistically vary between groups (Table 1). Although for each assessment, the direction was consistent with higher literacy for subjects enrolled in the cohort study. Literacy measures did not vary by age or gender (all p-values >0.60).
Table 1.
Descriptive statistics (mean, standard deviation) of multiple measures of health literacy as described. Comparisons are shown for those enrolled and not enrolled in the longitudinal cohort study
| Metric | Cross sectional study | Enrolled in cohort | Not enrolled |
|---|---|---|---|
|
STOHLA Health literacy |
31.1 (7.0) N=32 |
33.8(2.3) N=19 |
27.3(9.6)* N=13 |
|
PDSMS Self- efficacy |
29.1 (7.0) N=41 |
28.0(6.1) N=22 |
30.4(8.0) N=19 |
| Diabetes specific literacy | 7.0 (2.6) N=41 |
6.8(2.6) N=22 |
7.3(2.6) N=19 |
| Diabetes numeracy | 0.61 (0.28) N=41 |
0.71(0.26) N=22 |
0.55(0.32)ˆ N=19 |
p=0.009
p=0.02.
For the subjects enrolled in the cohort study (N=22), the mean wound size at enrollment was 4.5 cm2 (SD 7.1) and median 2.3 cm2 (IQR; 0.48, 3.8), the mean wound duration was 13.2 (SD: 14.1) months and median 7 (IQR: 3, 24) months. By the fourth week of care 59.1% (N=13) had increased in wound size, the log healing rate was 0.09 (SD 0.29) ln(cm2)/week and, by week 12, 27.3% (N=6) healed. Patients with lower STOFHLA scores had larger (p=0.04) and older (p=0.125) wounds that trended toward statistical significance. Those with lower numeracy had similar findings (p=0.167 and p=0.227, respectively). The direction of the diabetes literacy and efficacy was consistent with lower literacy and efficacy and wounds that were less likely to heal, however these findings could not yet be classified as a trend (p>0.50). There was also a trend toward significance for the log healing rate and STOFHLA (p=0.19).
None of the literacy tests were correlated with each other (R2 < 0.12) with the exception of STOFHLA and the assessment diabetes numeracy (R2 = 0.43, p<0.0001).
Discussion
We evaluated several measures of health literacy to determine if they might be associated with diabetic foot ulcer healing. General health literacy and diabetes numeracy were associated with enrollment into an ongoing longitudinal clinical study and with poor wound prognostic factors such as wound size and wound duration (11,12). For our cohort group, a trend was noted for wound healing rate during the first four weeks of care, which is a measure associated with the failure of a wound to heal (12). The wound healing rate is measured in the first month of care and has been shown to correlate with the likelihood that a wound will heal. We evaluated literacy in the first 4 weeks because this time period likely represents an individual’s a priori knowledge of or experience with wound care thereby representing a time frame where educational activities for individuals with lower health literacy might be most impactful.
Health literacy was described in a 2004 Institute of Medicine report as a patient’s health-related knowledge, skills and behaviors that are influenced by cultural background, health systems demands, and prior learning opportunities(5). For example, multiple studies have associated glycemic control as measured by hemoglobin A1C with varying measures of patient literacy, numeracy, and self-efficacy (8,13). Specifically, measures of foot care self-efficacy have not correlated with improved wound outcomes(4,14). It is possible that a person with a new DFU may not realize the need for prompt assessment, may delay seeking help for various personal reasons (financial: both maintaining income and avoiding the costs of care), and may delay care to seek advice from friends, elders, religious leaders, and others similarly afflicted (15). It is also possible that those with a poorer understanding of health literacy are more suspicious of medical studies as well as therapies that may not resonate with their personal view of medical care thereby influencing their decision to participate in a medical study. In fact, a recent qualitative study by Feinglass et al of 26 recently amputated patients, who did not all have diabetes, undergoing inpatient care in a Chicago rehabilitation facility provided some fascinating insights that might help to explain our findings(2). Feinglass et al showed that 62% of their patients had a very limited understanding of the association between foot ulcer and amputation(2).
There are many limitations to our study. While we interviewed a large number of subjects as compared to the few other studies on this topic, many more would need to be studied to assure adequate sample size for a healed wound outcome. In addition, we studied a single large urban center. Our results may not generalize to patients seen in other sites. While our results are provocative, the results from this study should be used to help properly design a larger longitudinal study using health literacy as the primary outcome.
The treatment of a DFU is highly dependent on accessing health care, understanding the gravity of the relationship between having a foot ulcer and the loss of a lower limb, understanding and following treatment recommendations, and ultimately the execution of treatment recommendations which are often difficult for a patient to manage. Therefore, it is very likely that health literacy can greatly affect whether a patient has a successful wound outcome. In our study we have shown that those with diminished health literacy are less likely to volunteer for clinical investigations and at the time they initiate care they have wounds that are less likely to heal. It appears that education in the first month of care may offer an opportunity to improve clinical outcomes.
Acknowledgments
Funding for the longitudinal cohort study described above was from the National Institutes of Health (R01-DK094260 (Thom,S/Margolis,D).
Footnotes
The authors have no conflicts of interest related to this study.
Reference List
- 1.Reiber GE, Ledous WE. Epidemiology of Diabetic Foot Ulcers and Amputations: Evidence for Prevention. In: Williams R, Herman W, Kinmonth A-L, Wareham NJ, editors. The Evidence Base for Diabetes Care. London: John Wiley & Sons, Ltd; 2002. pp. 641–65. [Google Scholar]
- 2.Feinglass J, Shively VP, Martin GJ, Huang ME, Soriano RH, Rodriguez HE, Pearce WH, Gordon EJ. How ‘preventable’ are lower extremity amputations? A qualitative study of patient perceptions of precipitating factors. Disability & Rehabilitation. 2012;34(25):2158–65. doi: 10.3109/09638288.2012.677936. [DOI] [PubMed] [Google Scholar]
- 3.Margolis DJ, Hoffstad O, Nafash J, Leonard CE, Freeman CP, Hennessy S, Wiebe DJ. Location, location, location: geographic clustering of lower-extremity amputation among medicare beneficiaries with diabetes. Diabetes Care. 2011;34(11):2363–7. doi: 10.2337/dc11-0807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Margolis DJ, Hoffstad O, Weibe DJ. Lower extremity amputation risk is associated with variation in Behavorial Risk Factor Surveillance System responses. Diabetes Care. 2014;37(8):2296–31. doi: 10.2337/dc14-0788. [DOI] [PubMed] [Google Scholar]
- 5.Nielson-Bohlman L, Panzer AM, Kindig DA. Health literacy: a prescription to end confusion. Washington DC: Instittue of Medicine: National Academic Press; 2004. [PubMed] [Google Scholar]
- 6.Paasche-Orlow MK, Wolf MS. Promoting health literacy research to reduce health disparities. Journal of Health Communications. 2010;15:34–41. doi: 10.1080/10810730.2010.499994. [DOI] [PubMed] [Google Scholar]
- 7.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: A new instrument for measuring patients’ literacy skills. J Gen Intern Med. 1995;10:537–41. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 8.Brega AG, Ang A, Vega W, Jiang L, Beals J, Mitchell CM, Moore K, Manson SM, Action KJ, Roubideaux Y. Mechanisms underlying the relationship between health literacy and glycemic control in American Indians and Alaska Natives. Patient Education and Counseling. 2012;88:61–8. doi: 10.1016/j.pec.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 9.Brega AG, Jiang L, Beals J, Manson SM, Acron KJ, Roubideaux Y. Speical diabetes program for Indians: Reliability and validity of brief measures of print literacy and numeracy. Patient Education and Cuonseling. 2012;88:61–8. [PubMed] [Google Scholar]
- 10.Wallston KA, Rothman R, Cherrington A. Psychometirc properties of the perceived diabetes self-management scale (PDSMS) Journal of Behavioral Medicine. 2007;30:395–401. doi: 10.1007/s10865-007-9110-y. [DOI] [PubMed] [Google Scholar]
- 11.Margolis DJ, Taylor LA, Hofstad O, Berlin JA. Diabetic neuropathic foot ulcer: The association of wound size, wound duration, and wound grade. Diabetes Care. 2002;25:1835–9. doi: 10.2337/diacare.25.10.1835. [DOI] [PubMed] [Google Scholar]
- 12.Margolis DJ, Gelfand JM, Hofstad O, Berlin JA. Surrogate endpoints for the treatment of diabetic neuropathic foot ulcers. Diabetes Care. 2003;26:1696–700. doi: 10.2337/diacare.26.6.1696. [DOI] [PubMed] [Google Scholar]
- 13.Osborn CY, Cavanaugh K, Wallson KA, Rothman RL. Self-efficacy links health literacy and numeracy to glycemic control. Journal of Health Communications. 2010;15:146–158. doi: 10.1080/10810730.2010.499980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abdulhameed Al-Khawaldeh O, Ali Al-Hassan M, Froelicher ES. Self-efficacy, self-management, and glucemic control in adults with type 2 diabetes mellitus. Journal of Diabetes and its Complications. 2012;26:10–6. doi: 10.1016/j.jdiacomp.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 15.Margolis DJ, Jeffcoate WJ. Epidemiology of foot ulceration and amputation-can global variation be explained? Medical Clinics of North America. 2013;97:791–805. doi: 10.1016/j.mcna.2013.03.008. [DOI] [PubMed] [Google Scholar]


