Abstract
Alcohol-serving venues in South Africa are sites for high-risk behaviours that may lead to HIV transmission. Prevention and treatment interventions are sorely needed in these settings, but HIV-related stigma may limit their effectiveness. This study explored expressions of stigma among alcohol-serving venue patrons in Cape Town and examined the potential impact of stigma on HIV disclosure, testing, and treatment-seeking behaviours. A total of 92 in-depth interviews with male and female, Black and Coloured patrons were conducted. Transcripts were analysed via memo-writing and diagramming techniques. Many participants mentioned knowing other patrons living with HIV/AIDS (PLWH), and this visibility of HIV impacted expressions of HIV-related stigma. Participants discussed four forms of HIV-related stigma in the venues: fearing PLWH, fearing HIV acquisition, blaming others for spreading HIV, and isolating PLWH. HIV visibility and expressions of HIV-related stigma, particularly fear of isolation, influenced participants’ willingness to disclose their status. HIV-related stigma in the venues also appeared to indirectly influence testing and treatment-seeking behaviour outside the venue. Results suggest that efforts to change norms and reduce expressions of HIV-related stigma in alcohol-serving venues are necessary to successfully deliver tailored HIV prevention interventions and increase uptake of HIV testing and care in this important social setting.
Keywords: HIV-related stigma, alcohol-serving venue, South Africa, alcohol, qualitative
Introduction
South Africa has the greatest number of people living with HIV/AIDS (PLWH) of any country in the world. There are an estimated 6.1 million PLWH in South Africa (UNAIDS, 2013), representing 17% of the global burden of HIV infection (Karim, Churchyard, Karim, & Lawn, 2009). Engagement of these individuals along the continuum of HIV testing and treatment has been suboptimal. Only one in five South African adults report recent testing for HIV (Simbayi et al., 2014), one-fifth of patients who initiate antiretroviral therapy (ART) are lost within six months, and a tenth of those who remain in care have poor adherence (Clouse et al., 2013; Luque-Fernandez et al., 2013).
Studies have documented high levels of HIV-related stigma in South Africa, which could explain drop-offs in HIV care engagement (Dos Santos, Kruger, Mellors, Wolvaardt, & van der Ryst, 2014; Kalichman & Simbayi, 2003; Katz et al., 2013). Stigma negatively impacts uptake of HIV testing, with individuals who perceive HIV-related stigma or observe enacted stigma far less likely to get tested for HIV (Maughan-Brown & Nyblade, 2013). Among PLWH, HIV-related stigma is also a significant barrier to linkage to HIV care and adherence to treatment regimens. High levels of HIV-related stigma have been associated with lower ART adherence, lower CD4 cell counts, and greater numbers of HIV-related symptoms (Maman et al., 2009; Peltzer, 2013; Tomori et al., 2013).
According to Link and Phelan (2001), stigma is an inherently social process that proceeds in four steps: (1) distinguishing and labeling differences; (2) associating differences with negative attributes; (3) separating those with and without the negative attributes; and (4) discriminating those who possess the negative attribute. The process of stigma causes social marginalisation, which is especially detrimental for those who have strong bonds to their communities (Mahajan et al., 2008; Parker & Aggleton, 2003). Stigma is typically produced along existing lines of inequality (Parker & Aggleton, 2003), and it serves as a mechanism by which to further punish, exert dominance over, and judge the behaviours of marginalised groups (Campbell, Nair, & Maimane, 2006). The expressions of HIV-related stigma in South Africa appear to mirror the processes outlined by Link and Phelan. South Africans who endorse HIV/AIDS-related stigma have negative perceptions of PLWH and support social sanctions for those individuals (Kalichman & Simbayi, 2003). Moreover, HIV-related stigma in South Africa tends to be constructed along demographic lines (i.e. race, gender, economic), which serve as convenient categories for labeling and discriminating against PLWH (Mbonu, van den Borne, & De Vries, 2009; Petros, Airhihenbuwa, Simbayi, Ramlagan, & Brown, 2006). The consequences of stigma further reinforce and perpetuate societal inequalities. PLWH who report experiencing stigma have said they feel ashamed because of their status and lost contact with people in their communities, which contributed to poorer HIV-related outcomes, loss of employment or housing, and psychological distress (Simbayi et al., 2007).
Stigmatising attitudes and behaviours are shaped by social and cultural contexts, which reinforces the need to target settings where HIV-related stigma is most harmful, but also modifiable. Comparative studies conducted throughout Africa have shown that expressions of stigma (i.e. “blaming”, “othering”) differ based on socioeconomic resources, norms, and the availability of supportive services for PLWH (Maman et al., 2009; Winskell, Hill, & Obyerodhyambo, 2011). Stigma is also uniquely produced and reproduced within different social settings, such as brothels (Munoz, Adedimeji, & Alawode, 2010) and faith-based organisations (Keikelame, Murphy, Ringheim, & Woldehanna, 2010). In South Africa, alcohol-serving venues (i.e. “shebeens”) are important social settings where HIV-related stigma needs to be better understood. Qualitative research has found that men and women frequent shebeens for social interactions, and women in particular regard the venues as places for them to bond with peers and escape home stressors (Choi et al., 2013; Watt, Aunon, Skinner, Sikkema, MacFarlane, et al., 2012). The venues also serve as social arenas for individuals to meet sexual partners (Weir, Morroni, Coetzee, Spencer, & Boerma, 2002) and our previous research has demonstrated that unprotected sex (Sikkema et al., 2011), transactional sex (including the exchange of sex for alcohol) (Watt, Aunon, Skinner, Sikkema, Kalichman, et al., 2012), and gender-based violence (Watt, Aunon, Skinner, Sikkema, MacFarlane, et al., 2012) frequently occur in these venues. These findings demonstrate both the importance of venues as social settings and the vulnerability of patrons to HIV acquisition.
Empirical evidence accumulated from several countries, including South Africa, has shown that HIV-related stigma is a barrier to prevention programmes because it limits the uptake of safer sexual behaviours and HIV testing (Mahajan et al., 2008). HIV prevention interventions that have been evaluated specifically in alcohol-serving venues have shown mixed results, possibly because of the impact of HIV-related stigma in these settings. For example, a bar-based sexual risk reduction intervention in South Africa found that stigma prevented participants from talking with HIV counselors, who were positioned in view of other patrons (Morojele et al., 2014). Other international studies have not conclusively linked HIV-related stigma to intervention effectiveness, but they do suggest that it plays a role in limiting the success of bar-based HIV prevention efforts. A popular opinion leader intervention conducted in alcohol-serving venues was effective in reducing HIV risk behaviours in the United States (Kelly et al., 1997), but was not successful when adapted to five international settings, including wine shops in India (NIMH, 2010). In Cape Town, South Africa, a behavioural risk reduction intervention demonstrated a short-term increase in condom use among patrons, but the effects waned approximately six months after the intervention potentially due to contextual factors, which could include HIV-related stigma, that prevented maintenance of risk reduction behaviours (Kalichman, Simbayi, Vermaak, et al., 2007; Kalichman, Simbayi, Vermaak, et al., 2008). In order to make HIV prevention interventions successful, more research is needed to understand HIV-related stigma’s expressions in alcohol-serving venues, where patrons are at heightened risk for acquiring HIV.
This study drew upon qualitative interviews conducted with patrons of alcohol-serving venues in Cape Town, South Africa, in order to: (1) explore the expressions of HIV-related stigma and its social function among drinkers in Cape Town, and (2) examine the potential impact that HIV-related stigma may have on disclosure, testing, and treatment-seeking behaviours. A more nuanced understanding of the perceptions and expressions of HIV stigma in alcohol-serving venues in this region may help to inform tailored HIV-related interventions for venue patrons.
Methods
This paper presents qualitative findings from a larger mixed-methods study of HIV risk among patrons in alcohol-serving venues in Cape Town, South Africa. Between June 2009 and June 2012, staff conducted in-depth interviews with 92 venue patrons. Data from these interviews were analysed to understand perceptions of HIV-related stigma and its implications for HIV prevention and treatment in this population.
Setting
This study was conducted in Delft, a peri-urban township located approximately 15 miles outside of Cape Town, South Africa. Delft was established in 1990 as a subsidised housing community and is a racially diverse township with residents of both Coloured (a South African ethnic group of mixed race ancestry) and Black African ethnicities. Delft has high unemployment rates (41% of adults are unemployed) and low levels of education (less than 30% of adults have completed secondary school).
Twelve alcohol-serving venues in Delft were identified using community intercept surveys (Weir et al., 2003). Based on 210 intercept surveys, 88 eligible venues were identified and of those, 24 met the study’s three eligibility criteria (seating areas for patrons, served at least 50 unique patrons per week, and had at least 10% female patrons). The final 12 venues were purposively selected from these, with six serving predominantly Black patrons and six serving predominantly Coloured patrons. Approximately 6% of male patrons and 5% of female patrons within the 12 selected venues reported an HIV positive diagnosis during data collection for this mixed-methods study (Sikkema et al., 2011).
Data Collection
Data were collected by South African research staff who were matched by language and ethnicity to the dominant patronage of each venue. Eligible participants consisted of regular patrons who could speak about the venue environment. Men were recruited for in-depth interviews directly from the venues. Women were first selected to enroll in a longitudinal cohort, a subset of who were then recruited to participate in interviews. Research staff approached eligible patrons and explained to them the purpose of the study. Interested individuals attended an appointment where they provided written consent and were interviewed in their preferred language (Afrikaans, Xhosa, or English). All interviews were audio-recorded and conducted in a private room in the study office. Participants received a grocery card valued at 100 Rands (approximately US$10) as compensation.
Interviewers followed a semi-structured guide that included two open-ended questions pertaining to HIV/AIDS in the community and related follow-up questions (Table 1). Since female interviewees were recruited from a longitudinal cohort, their relevant demographic data (e.g. race, HIV status) were extracted from quantitative assessments that they completed as part of that study. Limited demographic data were collected for male interviewees during interview discussions.
Table 1.
Interview-guide questions and probes.
| Interview questions |
| 1. What is your impression of how HIV is affecting this community? |
| 2. How do you think people coming to this bar understand HIV and does this impact their behaviour? |
| Probes |
| 1. What types of people do you think are at risk for HIV? |
| 2. How much do you know about HIV in this community? |
| 3. How much do people know about HIV in this community? |
| 4. How are people who are infected with HIV treated by others in this community? |
| 5. What do your friends say about HIV? |
| 6. What things make it difficult for people in this community to have safe sex? |
| 7. Do you worry about HIV yourself? |
All study procedures were approved by the institutional review boards at Duke University, University of Connecticut, and Stellenbosch University.
Analysis
Interview recordings were simultaneously translated and transcribed into English. Data analysis was conducted in four steps. First, for each transcript, the study team wrote a document memo to identify emergent themes and capture key narratives around HIV-related stigma (Birks, Chapman, & Francis, 2008). Representative quotes were included in the memos to preserve the participants’ language. Second, the memos were imported into QSR NVivo 10 software (NVivo Qualitative Data Analysis Software, 2012) and text related to perceptions of HIV risk, blame for HIV transmission, beliefs about PLWH, and disclosure, testing, and treatment-seeking behaviours were coded. Third, three authors (J.V., M.H.W., K.W.C.) reviewed the coded output and the first author wrote “advanced memos” (memos to record thoughts on categories within the data and relationships between categories) on each of those salient themes (Charmaz, 2006). The coding was reviewed in this step through a constant comparative method (Glaser & Strauss, 2009), whereby the quotations were grouped by participants’ demographics (gender, race, HIV status) to identify differences in themes across individuals. Fourth, representative quotations pertaining to each theme were identified and were used for diagramming and organising subcategories within the data (Miles, Huberman, & Saldaña, 2013). Literature on HIV-related stigma was also consulted throughout this step to help interpret the data and formulate the conceptual framework.
Results
Description of the sample
The sample included 37 male (41%) and 55 female (59%) participants and was fairly evenly split between Black Xhosa-speaking and Coloured Afrikaans-speaking participants. Participants ranged from 18 to 59 years old, with an average age of 35. A majority of women (76%) said they had gotten an HIV test before, which likely reflects routine HIV testing during pregnancy and not necessarily voluntary testing behaviour. There were five female participants and one male participant who disclosed to researchers that they were living with HIV. Of these, five were Black and one was Coloured.
Overview of study findings
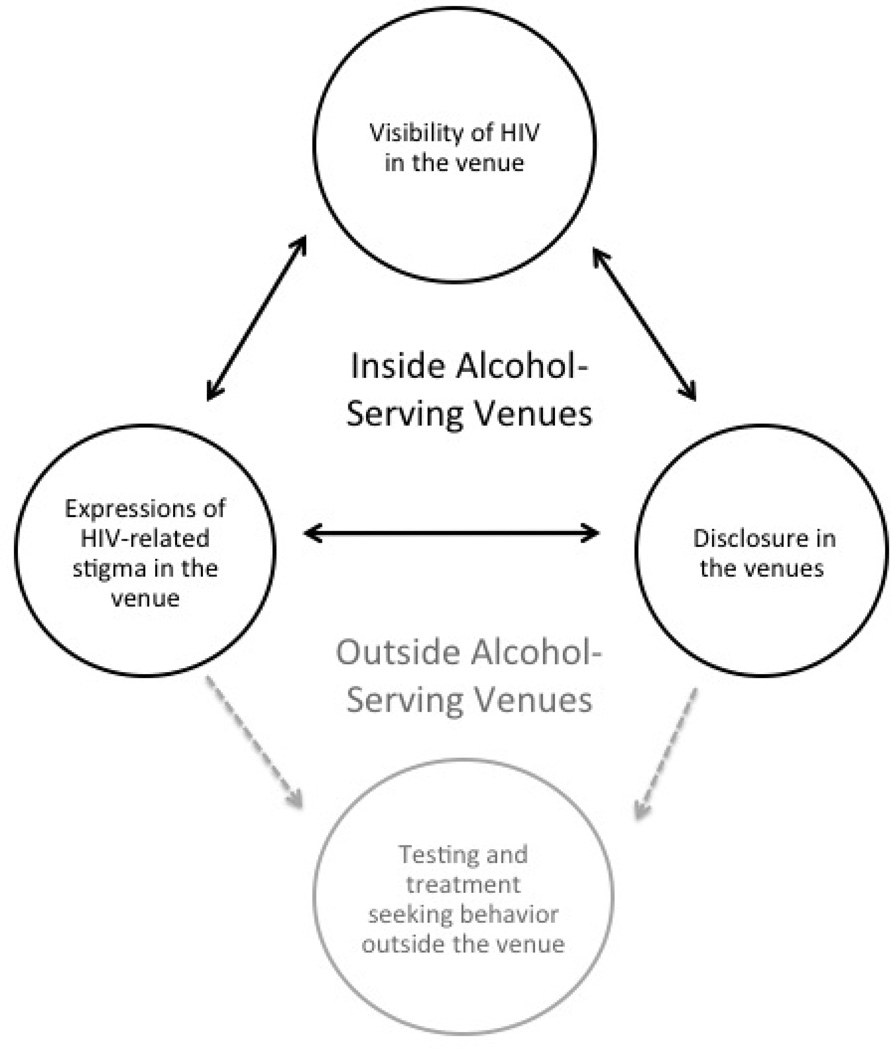
Analysis of the interviews revealed several themes around the visibility of HIV in the venue, expressions of HIV-related stigma, and the implications of stigma on disclosure, testing, and treatment-seeking behaviour (Figure 1). These themes were discussed regardless of participants’ HIV status, but issues around disclosure and treatment-seeking behaviour were mainly described by the six participants living with HIV. Participants’ perceptions about how visible HIV was in the venues influenced the expressions of HIV-related stigma they witnessed or perpetrated in the venues. Expressions of stigma in turn impacted visibility of HIV in the venue, because participants were more reluctant to discuss HIV if they feared being subject to expressions of HIV-related stigma, particularly social isolation. Together, visibility of HIV and expressions of HIV-related stigma in the venues directly influenced individuals’ willingness to disclose their HIV status to others in the venues, which served to perpetuate low visibility and high stigma in those settings. Those low rates of disclosure, combined with expressions of stigma in the venue, indirectly influenced individuals’ willingness to seek HIV testing and engage in HIV treatment outside the venues because an HIV status was seen as a reason to exclude individuals from this important social space.
Figure 1.
HIV-related stigma in the South African venue setting.
Visibility of HIV in the venues: “Ever since we heard that our friend was HIV positive, we realised that HIV is real”
Many participants talked about knowing venue patrons with HIV, suggesting high visibility of HIV in this setting. For example, one female participant said that “we live with them [PLWH], we know them, some drink with them… the people who are sick [with HIV] are the ones who mainly enjoy drinking”. These data suggest that it was commonplace for PLWH to drink at the venues. Reported visibility of HIV at the venue varied, however, by race. More participants at predominantly Black venues talked about knowing PLWH than those at Coloured venues, consistent with the higher HIV prevalence in Black communities in South Africa. Several Black participants described HIV as “everybody’s disease” or “everybody’s sickness,” which suggested that they both knew many people living with HIV and recognised their own vulnerability to the disease. On the other hand, Coloured participants described a more secretive atmosphere in talking about and knowing PLWH at the drinking venues. According to one Coloured woman, “In the [venue] no one talks about it, HIV and AIDS is a no go topic”, and while certain patrons were suspected of living with HIV, few had actually disclosed their status to others.
Expressions of HIV-related stigma in the venues: “Not that I have anything against ‘them’, but I keep my distance”
Participants reported either witnessing or perpetrating several expressions of HIV-related stigma, including being fearful of PLWH, being fearful of contracting HIV, blaming others for contracting and spreading HIV, and socially isolating PLWH. These expressions existed even while participants discussed instances of caring for PLWH in their communities.
Despite the visibility of HIV in many venues, participants spoke about an intense fear of being around PLWH in these settings, especially because the venues were seen as places for people to socialise and meet sexual partners. Several participants talked about sharing drinks and food and sitting in close proximity to one another, all of which were factors that contributed to their fear of being around PLWH. These participants either lacked knowledge about HIV transmission or knew that HIV could not be transmitted these ways and had unsubstantiated fear. Other participants said that they were afraid they might unwittingly have sex with a patron who was living with HIV. Participants described instances when they visited the venues specifically to find sex partners and did not use condoms, indicating that their fear was linked with recognition of their risky sexual behaviours. Fear of being around PLWH appeared related to visibility of HIV. In Coloured venues, participants reported that they usually could not identify who was living with HIV because no one spoke about the disease, which seemed to increase their fear. One Coloured female participant described this by saying: “You meet someone at the shebeen and you both eye each other. You don’t know what disease he has… You can’t trust anyone.”
Fear of being around PLWH at the venue was linked with discussions of participants’ own fears of contracting HIV, regardless of participants’ race and gender. One woman said she “wouldn’t be able to handle it” if she acquired HIV, both because she viewed the disease as a death sentence and because she didn’t want to experience isolation from her peers. Several men said they were “truly scared” of the disease because it is “a death penalty.” While several participants did say that their fear of contracting HIV made them more likely to use condoms, others were reluctant to use condoms because they did not want to be judged as diseased. However, information regarding safe sex behaviours was inconsistently collected across participants and limited conclusions can be drawn about the relationship between fear of contracting HIV and condom use. Reasons given to explain fear of contracting HIV were related to both high and low disease visibility. For instance, some participants said they had seen others suffer and die from HIV and did not want to experience that. Others (predominantly Coloured participants) said they were not aware of many people with HIV and therefore feared HIV because it was unknown.
Participants frequently placed blame on others for spreading HIV. This blaming was both gender- and age-based, and was discussed in Black and Coloured venues alike. Men described women in the venues as being at high risk for contracting and spreading HIV because they may have had sex with different men at the venues in exchange for alcohol: “This girl maybe sleeps with [players], they buy them alcohol…[a girl] may drop all and go with a stranger.” Conversely, women said that men are putting them at risk for acquiring HIV because they “refused to use condoms” and “stripped [women] of dignity” due to physical and sexual abuse. Female participants living with HIV said that men were to blame for passing the disease on to them and that it was “not fair [that] men bring the disease to women.” Additionally, older venue participants regularly pointed to younger patrons as responsible for transmitting HIV because they practice risky sexual behaviour: “These young people have this never mind attitude, they don’t even know if they have the disease or not.”
Both male and female participants discussed either witnessing or perpetrating the social isolation of PLWH in their venues. Female participants said that in the venues “[PLWH] are being rejected” and “those who are HIV positive are being treated as outcasts [in the venues]. Nobody wants to go near them, as if they have a dirty disease.” In addition to being avoided, PLWH were taunted and ridiculed. Participants talked about patrons who were living with HIV being called “whore” and “dog,” among other names. A woman living with HIV described being told “get away” and “you don’t smoke or drink with us” and another described her experience being gossiped about: “Positive people are treated very badly here [at the venue]. If someone finds out that you have the virus, he or she will tell everyone you know and will make a joke out of you.” When she visited the venue, men would start “whispering and laughing” at her. In turn, participants living with HIV discussed self-isolation tactics they used to avoid experiencing poor treatment from others in the venue. A woman living with HIV said that people “do not ill treat me because I do not walk around much.” This behaviour reflected PLWH internalising HIV-related stigma and losing their social standing in the venue.
Implications of HIV-related stigma for disclosure, testing, and treatment-seeking behavior
HIV-related stigma in the venues influenced patrons’ willingness to disclose their HIV status to venue patrons and others in their community, and it impacted their HIV testing and treatment-seeking behaviour outside the venues. Participants regularly said they would not want to tell other venue patrons their HIV status. In addition, few participants reported seeking out regular HIV testing services and many said they would not want to know their status or seek treatment if they were living with HIV, potentially due to fear of disclosure and an indirect impact of stigma in the venues. Participants both with and without HIV linked the absence of proactive treatment behaviours to a desire to avoid experiencing blame, social isolation, and other expressions of HIV-related stigma in the venue setting, even while they acknowledged that the venues were risky environments for HIV transmission.
Disclosure: “People who are HIV-positive are rejected…so if you are positive you won’t share because you are being stigmatised”
Many participants discussed difficulties that people in their communities have had disclosing their status, particularly to others at the venue. Unwillingness or reluctance to disclose one’s status was related to fear of being stigmatised by others and being socially isolated. PLWH were reportedly treated as “outcasts,” and gossiped about in these venues, and because of this a majority of participants said that a “person won’t even tell you that they are positive.” Participants who were HIV-negative or who did not know their status repeatedly said that if they were to acquire HIV they would not tell anyone else to avoid social rejection. In Coloured venues, where HIV was reported to be less visible, several participants said they would not want to disclose their status because “they don’t want to be labeled as carriers of death” or they did not want people to be “afraid” of them.
Participants with HIV described their particular hardships disclosing their status to others in the venues. One woman said, “it’s difficult to tell people about your status” and another said that she only talked about her status with her family members and kept it hidden from other venue patrons. One man said that he has kept his status a secret because if people knew, they “will see you as a leper.” Several participants who were living with HIV described situations when they only told one or a few people about their status, but then that person told other venue patrons. One woman said that “when [people] fight they will disclose each other’s status,” indicating that status disclosure has been used as a way to socially marginalise venue patrons.
HIV testing: “He’d rather get sick and die instead of being told that he is HIV positive”
HIV-related stigma in the venues seemed to indirectly influence HIV testing outside the venues by promoting fear around knowing one’s HIV status and creating a hostile environment for patrons who sought testing. While some participants did say that they sought regular testing for HIV, many others said that they would rather not know their HIV status. For example, one female participant said that she’s “always been afraid” and “[doesn’t] want to know if I have the disease”. A male participant explained that he and his friends “don’t want to know if we have HIV and that’s why none of us have ever tested.” Both men and women felt that men were more fearful of getting tested. For example, several men said that women had “courage,” while men “don’t want to be stressed when they found out the result so it’s better not to know.” Participants gave a variety of reasons for not wanting to get tested for HIV, including that they didn’t want others to see them being tested, they didn’t intend to disclose their status regardless of the test result, and they feared being socially isolated in the venues and gossiped about by fellow patrons.
Treatment-seeking behaviour: “When HIV-positive people are standing at the clinic they are afraid you will see them”
Although treatment-seeking behaviours were not discussed at length by participants, potentially due to the small number of participants with HIV in the sample, it is possible that the social setting of the venue reduced the willingness of patrons living with HIV to seek treatment. Issues around treatment-seeking behaviour were primarily related to fear of unintended HIV-status disclosure within the venues. Instances of clinic patients being seen by venue patrons and then gossiped about in the venue setting were discussed both by participants living with HIV and by participants who were HIV-negative but knew patrons living with HIV. Participants expressed a desire to keep the social milieu of the HIV clinics separate from that of the alcohol-serving venues. Individuals who reported being HIV-positive faced barriers related to seeking treatment because they did not want other venue patrons to know their status. For example, one woman said that she had a friend who would not go to collect her ARVs because “she was scared that people would find out she has AIDS.” People who went to the local clinic feared being seen entering or leaving by others who happened to walk by the clinic, and also feared being recognised by other PLWH at the clinic. When talking about a venue patron who was living with HIV, one female participant said, “We heard she was HIV positive from others who are also HIV positive…they take HIV treatment together.” Another woman living with HIV was concerned about other patients disclosing her status and said that she has chosen to receive care at a clinic in another community because “people don’t have to know when I go to do my CD4 count.”
Discussion
In-depth interviews with patrons of alcohol-serving venues in South Africa revealed the expressions of HIV-related stigma in this setting and its potential implications. A majority of participants expressed fear of acquiring HIV and/or being around PLWH, which could have led these participants to isolate and distance themselves from other patrons who they suspected were a “threat” to their health (Campbell & Deacon, 2006). Participants living with HIV described instances of discrimination when other patrons associated them with disease and referred to them by derogatory names. These individuals may have been seen as unable to maintain their social and economic contributions to their communities, including the community of alcohol-serving venues. This could explain their loss of social status, particularly in these low-income environments (Tsai, Bangsberg, & Weiser, 2013). Additionally, the social expressions of HIV-related stigma (i.e. blame, isolation) found in this study are perhaps more salient in the venues than other settings because alcohol-serving venues are inherently social settings and important locations for community interactions.
These results support other findings regarding the implications of HIV-related stigma for disclosure, testing, and treatment-seeking behaviours. Stigma is produced differently in various cultural contexts, and social environments have been shown to impact both expressions of individual and community-level HIV-related stigma as well as HIV intervention effectiveness (Airhihenbuwa, Ford, & Iwelunmor, 2014; Reid, Dovidio, Ballester, & Johnson, 2014). Several studies conducted in Sub-Saharan Africa have illustrated the powerful influence of HIV-related stigma on reducing uptake of HIV prevention and testing services (Kalichman & Simbayi, 2003; Mahajan et al., 2008; Musheke et al., 2013) and treatment adherence (Merten et al., 2010). This study adds to this body of research by understanding the expressions and implications of HIV-related stigma specifically within the context of alcohol-serving venues. Participants mentioned fear of disclosing their HIV status to other patrons, in conjunction with fear of losing their social standing within the venue. Venue-based stigma produces a hostile context for patrons living with HIV, and participants reported regularly witnessing and promoting the social marginalisation of these individuals. They also expressed their own desires to avoid experiencing isolation themselves, which may have increased their fear of acquiring HIV and reduced HIV testing and treatment-seeking behaviour outside of the venue.
This qualitative analysis revealed some salient differences in perceptions of HIV-related stigma by different demographic groups. Participants recruited from primarily Coloured venues regularly said that HIV was “hidden” in their communities. Because HIV was seldom discussed in this population, many Coloured participants talked about not feeling comfortable around those who they knew or suspected were living with HIV and expressed an intense fear of contracting the disease. In contrast, participants in predominantly Black venues discussed the commonplace nature of HIV in their communities and how it was seen as a “disease of the people.” This perception of higher burden of HIV in Black communities coincides with HIV prevalence statistics in Cape Town (Shisana et al., 2009) and seems to have resulted in less stigma and fear among Black participants, as compared to Coloured participants. This racial difference in HIV visibility and expressions of stigma could also be attributed to differing reach of HIV interventions and HIV-awareness social media campaigns in the communities. Quantitative research conducted in South Africa has shown that HIV-related stigma is inversely related to HIV visibility (Mall, Middelkoop, Mark, Wood, & Bekker, 2013). Therefore, interventions that increase the visibility of HIV in Coloured communities (e.g., popular opinion leaders, social media campaigns) might be effective in reducing HIV-related stigma in these settings.
Gender and age of venue patrons were also discussed in relation to HIV visibility and expressions of HIV-related stigma in the venues. Stigma has been shown to reinforce unequal power dynamics between men and women (Parker & Aggleton, 2003). Gender inequality increases women’s vulnerability to contracting HIV, and women are more likely to experience social marginalisation due to their HIV status than men (Mbonu et al., 2009). For instance, women living with HIV may be called sexually promiscuous, or could experience physical violence or economic abandonment from their spouse (Mbonu et al., 2009). Males and females in this study were likely to blame each other for spreading HIV in their communities. These findings align with other qualitative research conducted in South Africa, which has shown that women are blamed for transmitting HIV because they tend to be economically dependent on men and are perceived as manipulating relationships for their own good (Watt, Aunon, Skinner, Sikkema, Kalichman, et al., 2012). Conversely, men may be blamed for transmitting HIV because of their perceived promiscuity and power in sexual relationships (Petros et al., 2006). These results suggest that future interventions to effectively reduce HIV transmission and HIV-related stigma will also need to address issues of gender inequality and promote women’s empowerment. In addition to gender-based blame for HIV transmission, many participants (both in older and younger age groups) said that young venue patrons are most responsible for spreading HIV because they are not “afraid” of the disease. This suggests that HIV might be more normalised among younger people, which could impact their perceptions of stigma and sexual risk behaviours. The findings from this study provide some evidence of an interaction between age and stigma, which should be expanded upon in future stigma research.
This study has several important strengths and limitations. First, it drew data from a large, diverse sample, which allowed investigators to reach saturation of themes and explore participants’ responses as they related to their race, gender, and HIV status. Additionally, by completing memo writing and selecting key quotations early in the analysis process, authors were able to ground the findings in the participants’ words. Despite these strengths, the findings must be interpreted in light of several limitations related to data collection. Demographic data were not available for all participants, particularly the men who did not participate in the cohort study. Demographic data for male participants had to be extracted from the interviews, and this information was inconsistent across respondents. Individuals who reported living with HIV were underrepresented in the sample, which limited our understanding of their unique experiences at the venues. Also, six different interviewers conducted the interviews, using a semi-structured guide, which could have influenced the topics discussed and depth per topic across the interviews.
Overall, the results of this qualitative analysis imply that HIV prevention, testing, and treatment programmes conducted in alcohol-serving venues may have limited effectiveness without concurrently addressing the social issues of HIV-related stigma. Social forces in the venue (i.e. fear of status loss, isolation) may hinder disclosure, HIV testing, and adherence to HIV treatment. These findings suggest that culturally-targeted interventions in the venues may be necessary to change norms and reduce HIV-related stigma in these settings. For example, interventions in predominantly Coloured venues might reduce HIV-related stigma by targeting HIV visibility, while interventions in predominantly Black venues might provide peer support programmes to reduce social isolation among patrons living with HIV. Future qualitative research on the impact of social expressions of HIV-related stigma, in conjunction with quantitative studies, could be used to inform HIV-related interventions in the venues that raise awareness and tolerance of HIV. Such research could build upon the successes of existing HIV-related stigma interventions (Stangl, Lloyd, Brady, Holland, & Baral, 2013), address critical gaps in the field of stigma research, and target alcohol-serving venues. By changing norms and reducing HIV-related stigma in these important social contexts, we can lay a foundation for the successful implementation of effective HIV prevention, testing, and treatment interventions in these high-risk settings.
Acknowledgments
Funding
This project was supported by the National Institute of Alcohol Abuse and Alcoholism, [grant R01 AA018074]. We also acknowledge the support of the Duke Center for AIDS Research [grant P30 AI064518].
References
- Airhihenbuwa CO, Ford CL, Iwelunmor JI. Why culture matters in health interventions: Lessons from HIV/AIDS stigma and NCDs. Health Education & Behavior. 2014;41(1):78–84. doi: 10.1177/1090198113487199. [DOI] [PubMed] [Google Scholar]
- Birks M, Chapman Y, Francis K. Memoing in qualitative research: Probing data and processes. Journal of Research in Nursing. 2008;13(1):68–75. [Google Scholar]
- Campbell C, Deacon H. Unravelling the contexts of stigma: From internalisation to resistance to change. Journal of Community & Applied Social Psychology. 2006;16:411–417. [Google Scholar]
- Campbell C, Nair Y, Maimane S. AIDS stigma, sexual moralities, and the policing of women and youth in South Africa. Feminist Review. 2006;83:132–138. [Google Scholar]
- Charmaz K. Constructing grounded theory: A practical guide through qualitative analysis. London: Sage Publications; 2006. [Google Scholar]
- Choi KW, Watt MH, MacFarlane JC, Sikkema KJ, Skinner D, Pieterse D, Kalichman SC. Drinking in the context of life stressors: A multidimensional coping strategy among South African women. Substance Use& Misuse. 2013;49(1-2):66–76. doi: 10.3109/10826084.2013.819365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clouse K, Pettifor AE, Maskew M, Bassett J, Van Rie A, Behets F, Fox MP. Patient retention from HIV diagnosis through one year on antiretroviral therapy at a primary health care clinic in Johannesburg, South Africa. Journal of Acquired Immune Deficiency Syndromes. 2013;62(2):e39–e46. doi: 10.1097/QAI.0b013e318273ac48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dos Santos MM, Kruger P, Mellors SE, Wolvaardt G, van der Ryst E. An exploratory survey measuring stigma and discrimination experienced by people living with HIV/AIDS in South Africa: The People Living with HIV Stigma Index. BMC Public Health. 2014;14:80. doi: 10.1186/1471-2458-14-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glaser BG, Strauss AL. The discovery of grounded theory: Strategies for qualitative research. Piscataway, New Jersey: Transaction Publishers; 2009. [Google Scholar]
- Kalichman SC, Simbayi LC. HIV testing attitudes, AIDS stigma, and voluntary HIV counselling and testing in a black township in Cape Town, South Africa. Sexually Transmitted Infections. 2003;79(6):442–447. doi: 10.1136/sti.79.6.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Vermaak R, Cain D, Jooste S, Peltzer K. HIV/AIDS risk reduction counseling for alcohol using sexually transmitted infections clinic patients in Cape Town, South Africa. Journal of Acquired Immune Deficiency Syndromes. 2007;44(5):594–600. doi: 10.1097/QAI.0b013e3180415e07. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Vermaak R, Cain D, Smith G, Mthebu J, Jooste S. Randomized trial of a community-based alcohol-related HIV risk-reduction intervention for men and women in Cape Town South Africa. Annals of Behavioral Medicine. 2008;36(3):270–279. doi: 10.1007/s12160-008-9067-2. [DOI] [PubMed] [Google Scholar]
- Karim SSA, Churchyard GJ, Karim QA, Lawn SD. HIV infection and tuberculosis in South Africa: An urgent need to escalate the public health response. The Lancet. 2009;374:921–933. doi: 10.1016/S0140-6736(09)60916-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, Tsai AC. Impact of HIV-related stigma on treatment adherence: Systematic review and meta-synthesis. Journal of the International AIDS Society. 2013;16(3 Suppl 2):18640. doi: 10.7448/IAS.16.3.18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keikelame MJ, Murphy CK, Ringheim KE, Woldehanna S. Perceptions of HIV/AIDS leaders about faith-based organisation’s inflluence on HIV/AIDS stigma in South Africa. African Journal of AIDS Research. 2010;9(1):63–70. doi: 10.2989/16085906.2010.484571. [DOI] [PubMed] [Google Scholar]
- Kelly JA, Murphy DA, Sikkema KJ, McAuliffe TL, Roffman RA, Solomon LJ, Kalichman SC. Randomised, controlled, community-level HIV-prevention intervention for sexual-risk behaviour among homosexual men in US cities. The Lancet. 1997;350:1500–1505. doi: 10.1016/s0140-6736(97)07439-4. [DOI] [PubMed] [Google Scholar]
- Link BG, Phelan JC. Conceptualizing stigma. Annual Review of Sociology. 2001:363–385. [Google Scholar]
- Link BG, Phelan JC. Stigma and its public health implications. The Lancet. 2006;367:528–529. doi: 10.1016/S0140-6736(06)68184-1. [DOI] [PubMed] [Google Scholar]
- Luque-Fernandez MA, Van Cutsem G, Goemaere E, Hilderbrand K, Schomaker M, Mantangana N, Hernán MA. Effectiveness of patient adherence groups as a model of care for stable patients on antiretroviral therapy in Khayelitsha, Cape Town, South Africa. PLoS ONE. 2013;8(2):e56088. doi: 10.1371/journal.pone.0056088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahajan AP, Sayles JN, Patel VA, Remien RH, Sawires SR, Ortiz D, Coates TJ. Stigma in the HIV/AIDS epidemic: A review of the literature and recommendations for the way forward. AIDS. 2008;22(Suppl 2):S67–S79. doi: 10.1097/01.aids.0000327438.13291.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mall S, Middelkoop K, Mark D, Wood R, Bekker LG. Changing patterns in HIV/AIDS stigma and uptake of voluntary counselling and testing services: The results of two consecutive community surveys conducted in the Western Cape, South Africa. AIDS Care. 2013;25(2):194–201. doi: 10.1080/09540121.2012.689810. [DOI] [PubMed] [Google Scholar]
- Maman S, Abler L, Parker L, Lane T, Chirowodza A, Ntogwisangu J, Fritz K. A comparison of HIV stigma and discrimination in five international sites: The influence of care and treatment resources in high prevalence settings. Social Science & Medicine. 2009;68(12):2271–2278. doi: 10.1016/j.socscimed.2009.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maughan-Brown B, Nyblade L. Different dimensions of HIV-related stigma may have opposite effects on HIV testing: Evidence among young men and women in South Africa. AIDS and Behavior. 2013;18(5):958–965. doi: 10.1007/s10461-013-0636-4. [DOI] [PubMed] [Google Scholar]
- Mbonu NC, van den Borne B, De Vries N. Stigma of people with HIV/AIDS in sub-Saharan Africa: A literature review. Journal of Tropical Medicine. 2009;2009:1–14. doi: 10.1155/2009/145891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merten S, Kenter E, McKenzie O, Musheke M, Ntalasha H, Martin-Hilber A. Patient-reported barriers and drivers of adherence to antiretrovirals in sub-Saharan Africa: A meta-ethnography. Tropical Medicine & International Health. 2010;15(s1):16–33. doi: 10.1111/j.1365-3156.2010.02510.x. [DOI] [PubMed] [Google Scholar]
- Miles MB, Huberman AM, Saldaña J. Qualitative data analysis: A methods sourcebook. London: SAGE Publications; 2013. [Google Scholar]
- Morojele NK, Kitleli N, Ngako K, Kekwaletswe CT, Nkosi S, Fritz K, Parry CD. Feasibility and acceptability of a bar-based sexual risk reduction intervention for bar patrons in Tshwane, South Africa. SAHARA-J. 2014:1–9. doi: 10.1080/17290376.2014.890123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munoz J, Adedimeji A, Alawode O. ‘They bring AIDS to us and say we give it to them’: Socio-structural context of female sex workers’ vulnerability to HIV infection in Ibadan Nigeria. SAHARA-J. 2010;7(2):52–61. doi: 10.1080/17290376.2010.9724957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musheke M, Ntalasha H, Gari S, Mckenzie O, Bond V, Martin-Hilber A, Merten S. A systematic review of qualitative findings on factors enabling and deterring uptake of HIV testing in Sub-Saharan Africa. BMC Public Health. 2013;13(1):220. doi: 10.1186/1471-2458-13-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIMH Collaborative HIV/STD Prevention Trial Group. Results of the NIMH collaborative HIV/sexually transmitted disease prevention trial of a community popular opinion leader intervention. Journal of Acquired Immune Deficiency Syndromes. 2010;54(2):204–214. doi: 10.1097/QAI.0b013e3181d61def. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NVivo Qualitative Data Analysis Software (Version 10) QSR International. 2012. [Google Scholar]
- Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: A conceptual framework and implications for action. Social Science & Medicine. 2003;57(1):13–24. doi: 10.1016/s0277-9536(02)00304-0. [DOI] [PubMed] [Google Scholar]
- Peltzer K. HIV-related symptoms and management in HIV and antiretroviral therapy patients in KwaZulu-Natal, South Africa: A longitudinal study. SAHARA-J. 2013;10(2):96–104. doi: 10.1080/17290376.2013.870119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petros G, Airhihenbuwa CO, Simbayi L, Ramlagan S, Brown B. HIV/AIDS and ‘othering’ in South Africa: The blame goes on. Culture, Health & Sexuality. 2006;8(1):67–77. doi: 10.1080/13691050500391489. [DOI] [PubMed] [Google Scholar]
- Reid AE, Dovidio JF, Ballester E, Johnson BT. HIV prevention interventions to reduce sexual risk for African Americans: The influence of community-level stigma and psychological processes. Social Science & Medicine. 2014;103:118–125. doi: 10.1016/j.socscimed.2013.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shisana O, Rehle T, Simbayi LC, Zuma K, Jooste S, Pillay-van Wyk V the SABSSM III Implementation Team. South African national HIV prevalence, incidence, behaviour, and communication survey 2008: A turning tide among teenagers? Cape Town: HSRC Press; 2009. [Google Scholar]
- Sikkema KJ, Watt MH, Meade CS, Ranby KW, Kalichman SC, Skinner D, Pieterse D. Mental health and HIV sexual risk behavior among patrons of alcohol serving venues in Cape Town, South Africa. Journal of Acquired Immune Deficiency Syndromes. 2011;57(3):230–237. doi: 10.1097/QAI.0b013e3182167e7a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simbayi LC, Kalichman S, Strebel A, Cloete A, Henda N, Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Social Science & Medicine. 2007;64(9):1823–1831. doi: 10.1016/j.socscimed.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simbayi LC, Shisana O, Rehle T, Onoya D, Jooste S, Zungu N, Zuma K. South African national HIV prevalence, incidence and behavior survey, 2012. Cape Town: Human Sciences Research Council; 2014. [DOI] [PubMed] [Google Scholar]
- Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: How far have we come? Journal of the International AIDS Society. 2013;16(3 Suppl 2):18734. doi: 10.7448/IAS.16.3.18734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomori C, Kennedy CE, Brahmbhatt H, Wagman JA, Mbwambo JK, Likindikoki S, Kerrigan DL. Barriers and facilitators of retention in HIV care and treatment services in Iringa, Tanzania: The importance of socioeconomic and sociocultural factors. AIDS Care. 2013;26(7):907–913. doi: 10.1080/09540121.2013.861574. [DOI] [PubMed] [Google Scholar]
- Tsai AC, Bangsberg DR, Weiser SD. Harnessing poverty alleviation to reduce the stigma of HIV in sub-Saharan Africa. PloS Medicine. 2013;10(11):e1001557. doi: 10.1371/journal.pmed.1001557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. Global report: UNAIDS report on the global AIDS epidemic, 2013. Geneva, Switzerland: Joint United Nations Programme on HIV/AIDS (UNAIDS); 2013. [Google Scholar]
- Watt MH, Aunon FM, Skinner D, Sikkema KJ, Kalichman SC, Pieterse D. “Because he has bought for her he wants to sleep with her”: Alcohol as a currency for sexual exchange in South African drinking venues. Social Science & Medicine. 2012;74(7):1005–1012. doi: 10.1016/j.socscimed.2011.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt MH, Aunon FM, Skinner D, Sikkema KJ, MacFarlane JC, Pieterse D, Kalichman SC. Alcohol-serving venues in South Africa as sites of risk and potential protection for violence against women. Substance Use &Misuse. 2012;47(12):1271–1280. doi: 10.3109/10826084.2012.695419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weir SS, Morroni C, Coetzee N, Spencer J, Boerma JT. A pilot study of a rapid assessment method to identify places for AIDS prevention in Cape Town, South Africa. Sexually Transmitted Infections. 2002;78(suppl 1):i106–i113. doi: 10.1136/sti.78.suppl_1.i106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weir SS, Pailman C, Mahlalela X, Coetzee N, Meidany F, Boerma JT. From people to places: Focusing AIDS prevention efforts where it matters most. AIDS. 2003;17(6):895–903. doi: 10.1097/01.aids.0000050809.06065.e0. [DOI] [PubMed] [Google Scholar]
- Winskell K, Hill E, Obyerodhyambo O. Comparing HIV-related symbolic stigma in six African countries: Social representations in young people’s narratives. Social Science & Medicine. 2011;73(2011):1257–1265. doi: 10.1016/j.socscimed.2011.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]