Abstract
Partial tears of the anterior cruciate ligament (ACL) are common and represent 10–27% of the total. The main reasons for attending to cases of non-torn bundles are biomechanical, vascular and proprioceptive. Continued presence of the bundle also serves as protection during the healing process. There is controversy regarding the definition of these injuries, which is based on anatomy, clinical examination, translation measurements, imaging examinations and arthroscopy. The way in which it is treated will depend on the existing laxity and instability. Conservative treatment is optional for cases without instability, with a focus on motor rehabilitation. Surgical treatment is a challenge, since it requires correct positioning of the bone tunnels and conservation of the remnants of the torn bundle. The pivot shift test under anesthesia, the magnetic resonance findings, the previous level and type of sports activity and the arthroscopic appearance and mechanical properties of the remnants will aid the orthopedist in the decision-making process between conservative treatment, surgical treatment with strengthening of the native ACL (selective reconstruction) and classical (anatomical) reconstruction.
Keywords: Anterior cruciate ligament/injuries, Anterior cruciate ligament/surgery, Knee
Resumo
Lesões parciais do ligamento cruzado anterior (LCA) são comuns e representam 10–27% das totais. As principais razões para atenção ao feixe não rompido são biomecânicas, vasculares e proprioceptivas. A permanência do feixe serve ainda de proteção durante o processo cicatricial. A definição dessa lesão é controversa, baseada na anatomia, no exame clínico, na medida da translação, nos exames de imagem e na artroscopia. Seu tratamento vai depender da frouxidão e da instabilidade existentes. O tratamento conservador é opcional para casos sem instabilidade, com enfoque na reabilitação motora. O tratamento cirúrgico é desafiador, pois exige correto posicionamento dos túneis ósseos e conservação dos remanescentes do feixe rompido. O teste do pivot-shift sob anestesia, os achados à ressonância magnética, o nível e o tipo de atividade esportiva prévia e o aspecto artroscópico dos remanescentes e suas propriedades mecânicas auxiliarão o ortopedista no processo decisório entre o tratamento conservador, o tratamento cirúrgico com reforço do LCA nativo (reconstrução seletiva) ou a reconstrução clássica (anatômica).
Palavras-chave: Ligamento cruzado anterior/lesões, Ligamento cruzado anterior/cirurgia, Joelho
Introduction
Over the last 15 years, knowledge of tearing and reconstruction of the anterior cruciate ligament (ACL) has evolved considerably. Anatomical studies have made it possible to precisely identify ligament insertions in bones,1, 2 while biomechanical studies have provided better understanding of the function of each of the ligament bundles.2 Better anatomical knowledge and biological interest in preserving the remnants of the torn ACL have led to modification of the classical reconstruction techniques: double-band, anatomical and selective for partial tears.3, 4, 5, 6, 7
Complete tearing of the ACL can be diagnosed through clinical examination,8 while partial tearing often cannot. In such cases, complementary examinations are needed for confirmation. The definitive diagnosis of a partial ACL tear is reached by combining clinical findings, imaging examinations and, when necessary, arthroscopic findings. In cases of partial ACL tears, it is essential to assess the competence and functionality of the remaining fibers with regard to knee stabilization. It also has to be ascertained whether the event in question was a partial tear or whether there was a complete tear that is now healing.7, 8, 9
A consensus for defining, diagnosing and treating partial ACL tears is sought. Motivated by the discussion that still exists in the literature and the need for better understanding, the present review had the aim of discussing partial ACL tears.
Definition
Norwood and Cross apud Colombet et al.9 described three bands for the ACL that have anatomical and functional importance: anteromedial (AM), posterolateral (PL) and intermediate. Others have described two bands that present known and accepted functionality.8, 9, 10, 11 Each band would contribute separately toward stabilizing the knee and could be injured separately in partial tears. According to Hong et al.,10 partial tears would be those in which less than 50% of the ligament is torn. On the other hand, according to Noyes et al.,11 the definition of partial tears would be related to the percentage of the ACL fibers that are torn, given that tearing of 50–75% of the diameter would be highly correlated with clinical failure.
The American Medical Association, which divides these injuries into three degrees of severity, defines traumatic ACL tears as grade II when these tears are partial: moderate sprains caused by direct or indirect trauma.9 The clinical presentation in these cases would be characterized by pain, partial functional limitation, hemarthrosis and the possibility of episodes of instability. DeFranco and Bach6 put forward a multifactorial definition that took into consideration the combination of clinical and arthroscopic factors, and other authors would agree with this.
In cases of partial ACL tears, the most important objective is to determine whether any remnant fibers are present and whether they would enable clinical stability if they were kept. Although arthroscopic evaluation makes it possible to observe these remnants, use of the traditional portals may give rise to confusion in assessing them. Sonnery-Cottet and Chambat12 suggested using a “figure of 4” (Cabot) position for better assessment of the remnants of the PL band. Crain et al.,7 Colombet et al.9 and Sonnery-Cottet et al.13 described patterns of partial tears. Among the cases evaluated, 17% were considered to present good clinical quality and 83%, poor quality. Better-quality tissue with preserved mechanical properties was seen more frequently when the PL band was present (70%), to the detriment of intercondylar healing (27%) or healing of remnants adhering to the posterior cruciate ligament (13%). Although some studies have demonstrated clinical stability associated with partial tears, Maeda et al.14 did not find great stability in these cases.
Diagnosis
Diagnosing partial ACL tears remains a challenge. It needs to be based on a combination of clinical examination and imaging examinations (radiography and magnetic resonance), with the definitive diagnosis reached through arthroscopic assessment, when this is indicated.
Clinical examination
In a study conducted by the French Society of Arthroscopy,15 a clinically significant degree of laxity (p < 0.05) was detected in a comparison between a population with complete ACL tears (98% of the patients presented a positive Lachman test and 80% had a positive pivot shift test, i.e. +2 or +3) and a group with partial tears (30–64% presented a hard or delayed stop in the Lachman test and had a negative pivot shift test, i.e. 0 or +1). In that study, having a “soft stop” in the Lachman test was considered to be a strong predictor of complete ACL tears, while a pivot shift test with less rebound (0 or +1) would correspond in 94% of the cases to partial tears or even to incomplete healing.
Studies on cadavers have proven the difficulty in correlating the magnitude of the injury and its types with the alterations seen in clinical tests.16 Several authors have reported that it is possible to observe a hard stop in the Lachman test in cases of partial tears.9, 16, 17 The Lachman test is more sensitive for diagnosing complete ACL tears, while the pivot shift test and jerk test are more specific.16, 17, 18 Another point to be considered is that the sensitivity of the pivot shift test increases from 24% to 92% when the patient is assessed under anesthesia, which is the best situation for evaluating the functional state of the remaining fibers.9, 19, 20, 21 When this test is positive, it indicates rotational instability, which is not evaluated through differential anterior translation tests. In negative cases, the arthroscopic evaluation makes it possible to assess associated injuries that might cause difficulty in the test: meniscal lesions, displaced chondral lesions and interposing of the remnants of the ACL.
Measurement of the differential anterior translation
A variety of devices are available for measuring differential anterior translation. The ones that are best known and used in clinical practice are the KT 1000®, KT 2000®, Rolimeter® and Telos® devices. Their use for making diagnoses is more accurate in cases of subacute and chronic lesions with better pain control and absence of muscle contractions. The differential anterior translation is less than 3 mm in 95% of normal knees. In comparative evaluations, when this translation is greater than 3 mm in relation to the asymptomatic side, 90% of such cases present ACL tears. Measurements of between 3 and 5 mm may represent partial tears.17, 20, 21 Dejour et al.17 described differences in translation measurements between patients with complete and partial tears. The patients with complete tears presented a mean of 9.1 ± 3.4 mm, in comparison with 5.2 ± 2.9 mm among those with partial tears (p < 0.05). They also observed that 67% of the patients with preservation of the PL band presented adequate remaining clinical function, versus 17% of those in whom the AM band was present. It was considered that functionality remained when the pivot shift test result was 0 or +1 and when the differential anterior translation was less than 4 mm. It needs to be borne in mind that these devices only evaluate the differential anterior translation, without any rotational evaluation. Their use in association with the other tests and imaging examinations is fundamental for making the diagnosis and defining the therapy.
Imaging examinations
Radiology
Radiological evaluation performed together with measurements of the differential anterior translation has been shown to be important for diagnosing ACL injuries. In lateral radiographs with anteriorization of the tibia that are produced on individuals with complete tears, significant translation of the medial and lateral compartments can be seen, while in those with partial tears, little translation is seen in relation to the normal side.9, 22
Magnetic resonance
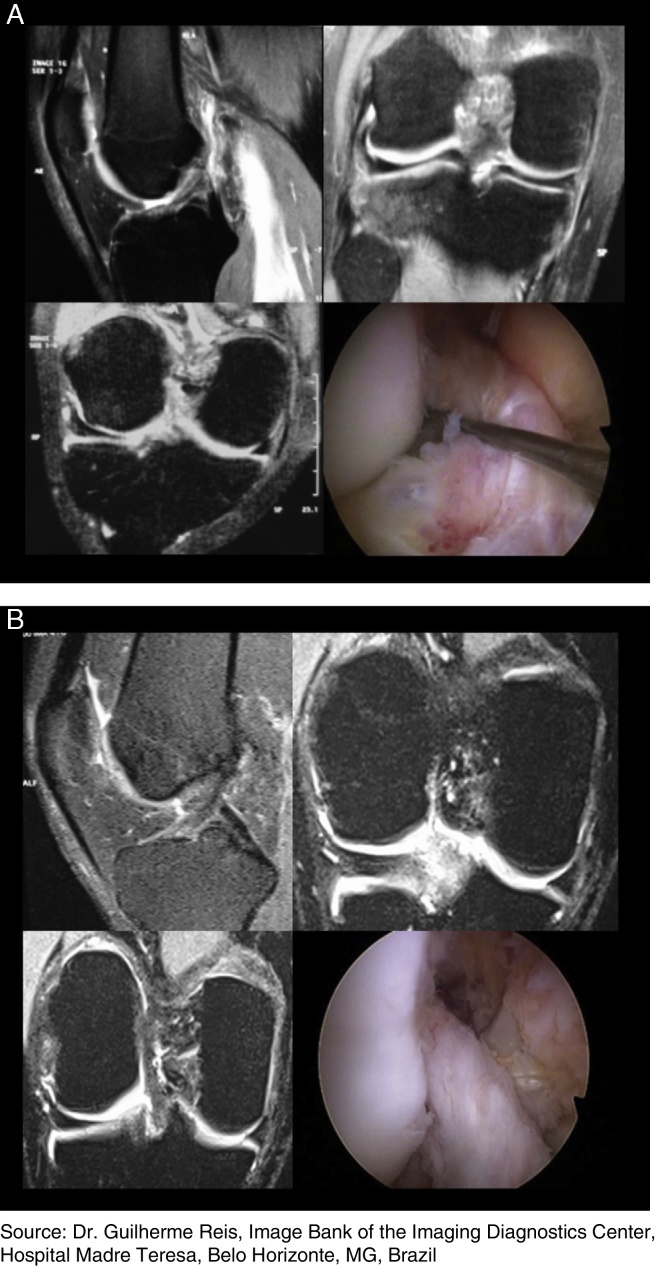
Despite all the technological development that has taken place, it is still difficult to diagnose partial ACL tears. Magnetic resonance may suggest that such injuries are present but without the capacity to confirm this or make a functional assessment on the remaining portions.21, 22, 23 Specific slices are necessary in order to make a distinction between complete and partial tears. Van Dyck et al.22 suggested that certain axial and perpendicular views would be more accurate in making diagnoses based on magnetic resonance. Along with clinical examination and measurement of the differential anterior translation, magnetic resonance imaging is important for defining and guiding the best treatment (Fig. 1).
Fig. 1.
Magnetic resonance imaging of partial tears of the anterior cruciate ligament of the knee. (A) Injury to the posterolateral band and preservation of the anteromedial band; (B) injury to the anteromedial band and preservation of the posterolateral band.
Source: Dr. Guilherme Reis, Image Bank of the Imaging Diagnostics Center, Hospital Madre Teresa, Belo Horizonte, MG, Brazil.
Arthroscopic evaluation
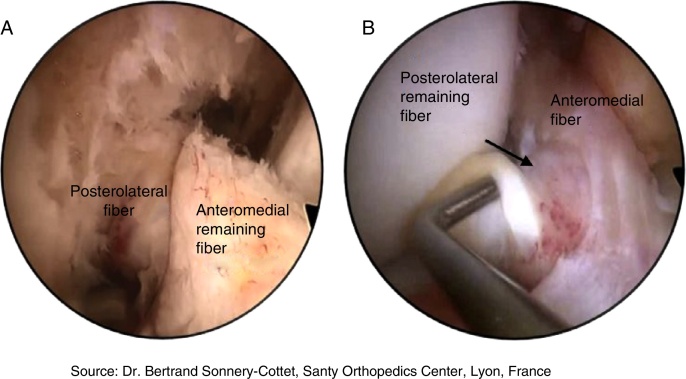
Arthroscopic evaluation has been proposed by some authors for diagnosing partial tears.9, 12, 13, 16, 17 However, in the light of the current knowledge, there is no indication for systematic arthroscopic evaluations for diagnosing such injuries. Arthroscopy makes it possible to diagnose the type of partial tear and, together with the clinical and imaging examinations, it determines the best type of reconstruction in cases in which surgical treatment is indicated (Fig. 2).
Fig. 2.
Arthroscopic view of partial tears of the anterior cruciate ligament of the knee. (A) Injury to the anteromedial band and preservation of the posterolateral band; (B) injury to the posterolateral band and preservation of the anteromedial band.
Source: Dr. Bertrand Sonnery-Cottet, Santy Orthopedics Center, Lyon, France; Posterolateral fiber; Anteromedial remaining fiber; Posterolateral remaining fiber; Anteromedial fiber.
Multifactorial theory
Partial tears are common and account for 10% to 27% of ACL injuries.9 Preservation of the AM and PL bands is seen in 11% and 16% of the cases, respectively. The frequency of meniscal lesions is similar and the mean differential anterior translation is 4.49 and 4.97 mm, respectively. The time that elapses between injury and surgical treatment is shorter (five months).3 DeFranco and Bach6 proposed a better approach in which multiple factors would be defined, such that asymmetrical Lachman tests, negative pivot shift tests, differential anterior translation from 3 to 4.9 mm and complementary positive evaluations using magnetic resonance imaging and arthroscopy would be taken into consideration.6, 21, 23
Treatment
The treatment needs to be individualized and appropriate for each patient's needs. Identifying patients with low and high risk of progression of the clinical deficiency of the ACL is fundamental for providing therapeutic guidance. Low-risk patients are the ones with low physical demands, without associated injuries or complaints of instability, whose clinical tests are negative. These patients’ signs and symptoms generally tend not to progress and can be treated conservatively.9, 21, 23 High-risk patients are the ones with proven clinical instability and lifestyles that present a high risk of new torsion. In these cases, the best option would be to perform selection surgical reconstruction of the ACL.21, 23 The treatment strategy always needs to take into consideration the symptoms, clinical examination, percentage of fibers remaining, associated injuries, length of time since the injury and daily physical work demands.
Conservative treatment
The conservative treatments used include immobilization while the patient remains symptomatic and then, after the acute phase, stimulation of complete movement and progressive weight-bearing.9, 21, 23 The principles of rehabilitation for patients with partial tears are the same as those used for patients with complete tears. This rehabilitation consists of exercises for muscle stretching and strengthening and cardiovascular, proprioceptive and adaptive training.24, 25, 26 Pujol et al.27 demonstrated that partial ACL tears may have the capacity to heal, contrary to what had been thought.
Conservative treatment produces good results when correctly indicated, with minimal reduction of activity level and without impairing stability.21, 23, 24 Other authors have suggested that partial tears are functionally equivalent to complete tears and that conservative treatment would imply worse clinical and functional results.26, 27 Pujol et al.27 described a series in which 25% of the patients with partial ACL tears evolved with functional instability over the medium to long term. Serial assessments would be necessary in order to monitor the rehabilitation and residual laxity, which thus would enable evaluation of whether conservative treatment should be maintained or whether it should be changed to a surgical approach.17, 21, 26, 27, 28
Surgical treatment
Indication
Treatment with selective ACL reconstruction in cases of partial tears may be justified by different factors. The first of these is clinical: many partial tears progress to complete tears with increasing differential anterior translation and the consequent possibility of meniscal and chondral lesions.9, 16, 17, 28 The second is biological: the central fibers of the ACL provide adequate vascular and nervous supplies to the new ligaments. Mechanoreceptors present in the remaining ligament are responsible for preserving and restoring the stability and joint balance.3, 4, 7, 27 Histological evaluations on ACL remnants have demonstrated that they have the capacity to accelerate cell proliferation, revascularization and, consequently, integration of the graft in cases of selective reconstruction.27, 28, 29, 30, 31 The third is epidemiological: the risk of degenerative lesions subsequent to partial tears has not yet been established, although Kannus and Jarvinen25 reported that 15% of their patients with partial tears presented degenerative lesions after eight years of follow-up.
Treatment
Selective reconstruction has some points in common with anatomical ACL reconstruction: graft options, rehabilitation program and time taken to return to physical practices. The most important difference lies in the biological concept. Other differences relate to tunnel positioning and milling, along with the graft diameter and passage. The options for surgical treatment of partial ACL tears include thermal measures, classical reconstruction and selective reconstruction. Thermal measures and classical reconstruction are not addressed in this review.
The arthroscopic evaluation is started through the classical portals: anteromedial and anterolateral. Some authors have proposed that an accessory anteromedial portal should be created: this would facilitate viewing the graft and the footprints. Sonnery-Cottet et al.29 proposed that the anterolateral portal should be constructed slightly proximally in order to have better viewing and less need for debridement of Hoffa's fat. After an inventory of all compartments has been made, the associated lesions are treated and then the remaining fibers of the ACL are assessed. This evaluation is visual (with confirmation of the presence of continuous fibers connecting footprints) and mechanical, and is done both in a semi-flexed position and in a “figure of 4” position. Tension is assessed by means of palpation and via clinical tests under arthroscopic viewing.32, 33
Graft selection
The choice of graft should follow the surgeon's routine. Several authors have reported making increasing use of flexor tendons, which may be triple or quadruple and either free or maintained in their tibial insertions.3, 4, 9, 13 The presence of bone blocks may make passage through the tunnels thus created more difficult. From the intercondylar space that is associated with preservation of greatest numbers of remnant fibers, a graft diameter of 8 mm has been found to be most appropriate.5, 9, 12, 13 The concept that the greater the graft diameter is the better this would be conflicts with the anatomical concept of preservation of the remnants and with the biology of healing between these remnants and the graft.32, 33
Technical details
Reconstruction of the AM band
The arthroscopic procedure begins with moderate debridement of the remnants of the AM band with preservation of the PL band. Siebold and Fu34 recommended that a tibial guide at an angle of 60° should be used, with an entry point around 1.5 cm medially to the anterior tuberosity of the tibia. The position of the femoral tunnel should follow the presence of the remnants in the femur in the anatomical position. To construct this tunnel, inside-out or outside-in guides can be used. Milling should be done manually or by means of low-velocity drilling, so as to avoid further injuring the remains of the ACL.
Reconstruction of the PL band
The position of the tibial tunnel is more medial and begins around 3.5 cm medially to the anterior tuberosity of the tibia. The intra-articular portion is located in the posterior part of the tibial insertion and 5 mm medially to the lateral intercondylar eminence. Use of the femoral remains is the most reliable way of finding the site for the femoral tunnel. It is constructed by means of the anteromedial portal or using an outside-in technique. For tunnels constructed by means of the medial portal, attention needs to be given to the risk of iatrogenic lesions in the medial femoral condyle at the time of milling.
Graft fixation
The fixation will depend on the technique used. If the inside-out technique is used, interference screws or Endobutton® are recommended for the femoral portion and interference screws for the tibial portion. If the outside-in technique is used, interference screws can be used in both tunnels. There is room for debate regarding whether the fixation should be done without pre-tensioning, or whether it should be done after pre-tensioning, which theoretically would ensure better adaptation of the graft.28, 29, 34 For selective reconstruction of the PL band, fixation is done with flexion of between 0° and 10°, while for reconstruction of the AM band, the fixation angle is more variable. Some authors have described fixation at between 50° and 60°, while others have recommended flexion of 20°.9, 21, 23, 34 After fixation, the entire range of motion should be tested, with special attention to extension. If this is not achieved, it may be a source of pain and/or loss of movement.
Clinical evaluation
Mott was the first author to report satisfactory clinical results from selective reconstruction after acute ACL tearing.9, 21, 23 Adachi et al.3, 35 and Ochi et al.4, 36 published data on patient series in which they compared selective and classical ACL reconstruction. Smaller differential anterior translation was found in the selective group. This observation was perhaps due to the better vascularization and reinnervation at the time of selective reconstruction. In 2009, Ochi et al.36 published data on a new series of 45 patients who underwent selective reconstruction with a follow-up of two years. They showed using magnetic resonance imaging that the differential anterior translation was less than 0.5 mm, proprioception was better and healing was effective after the operation. These findings corroborated those of a study conducted in 2002 that demonstrated that there was an association between the presence of mechanoreceptors in the remaining fibers and better proprioception.4, 36
Buda et al.5 evaluated 47 patients who underwent selective reconstruction. Good or excellent clinical results were seen in 95.7% of the cases. Good clinical results were correlated with integration of the graft with the remaining fibers and with presence of a signal on magnetic resonance imaging. Attention was drawn to the fact that in selective reconstruction procedures, the graft needs to be between 7 and 8 mm, which would avoid an excess of fibers between the remainder of the ACL and the graft.5, 32 Sonnery-Cottet et al.37 evaluated 36 patients who underwent reconstruction of the AM band and observed that the differential anterior translation was less than 0.8 mm. In following up patients who had been treated with selective reconstruction of partial tears, Chouteau et al.38 demonstrated that the stability and proprioception of the treated knee were similar to those of the normal knee.
Few published papers have compared classical ACL reconstructions and selective reconstruction procedures, with functional and non-functional remnant ligaments. A greater number of studies would be useful in order to evaluate the environment created by the remnants and their effect on graft healing. The results from selective reconstruction are encouraging, although there is still a lack of evidence that would prove its real benefit.39
Final remarks
Partial ACL tears are being diagnosed more and more frequently. They account for 10–27% of all such injuries. There is no single definition for them in the literature. They can be diagnosed through a combination of clinical examination and imaging examination, with confirmation through arthroscopic examination. The pivot shift test under anesthesia, the hard-stop Lachman test, magnetic resonance findings, the level and type of sports activity, the arthroscopic appearance of the remnant ligament and the mechanical properties are elements used by orthopedists for deciding between conservative treatment, surgical treatment with reinforcement of the native ACL (selective reconstruction) and classical (anatomical) ACL reconstruction. When there is an indication for surgery, preservation of the remaining fibers is fundamental, in order to preserve the mechanical, vascular and proprioceptive capacity of the knee.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgments
To the Knee Group of the Orthopedics and Traumatology Service, Hospital Madre Teresa, Belo Horizonte, Brazil, and to the Santy Orthopedics Center, Lyon, France.
References
- 1.Purnell M.L., Larson A.I., Clancy W. Anterior cruciate ligament insertions on the tibia and femur and their relationships to critical bony landmarks using high-resolution volume-rendering computed tomography. Am J Sports Med. 2008;36(11):2083–2090. doi: 10.1177/0363546508319896. [DOI] [PubMed] [Google Scholar]
- 2.Zantop T., Herbort M., Raschke M.J., Fu F.H., Petersen W. The role of the anteromedial and posterolateral bundles of the anterior cruciate ligament in anterior tibial translation and internal rotation. Am J Sports Med. 2007;35(2):223–227. doi: 10.1177/0363546506294571. [DOI] [PubMed] [Google Scholar]
- 3.Adachi N., Ochi M., Uchio Y., Sumen Y. Anterior cruciate ligament augmentation under arthroscopy. A minimum 2-year follow-up in 40 patients. Arch Orthop Trauma Surg. 2000;120(3–4):128–133. doi: 10.1007/s004020050028. [DOI] [PubMed] [Google Scholar]
- 4.Ochi M., Adachi N., Deie M., Kanaya A. Anterior cruciate ligament augmentation procedure with a 1-incision technique: anteromedial bundle or posterolateral bundle reconstruction. Arthroscopy. 2006;22(4) doi: 10.1016/j.arthro.2005.06.034. 463.e1-5. [DOI] [PubMed] [Google Scholar]
- 5.Buda R., Ferruzzi A., Vannini F., Zambelli L., Di Caprio F. Augmentation technique with semitendinosus and gracilis tendons in chronic partial lesions of the ACL: clinical and arthrometric analysis. Knee Surg Sports Traumatol Arthrosc. 2006;14(11):1101–1107. doi: 10.1007/s00167-006-0117-7. [DOI] [PubMed] [Google Scholar]
- 6.DeFranco M.J., Bach B.R., Jr. A comprehensive review of partial anterior cruciate ligament tears. J Bone Jt Surg Am. 2009;91(1):198–208. doi: 10.2106/JBJS.H.00819. [DOI] [PubMed] [Google Scholar]
- 7.Crain E.H., Fithian D.C., Paxton E.W., Luetzow W.F. Variation in anterior cruciate ligament scar pattern: does the scar pattern affect anterior laxity in anterior cruciate ligament-deficient knees? Arthroscopy. 2005;21(1):19–24. doi: 10.1016/j.arthro.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 8.Amis A.A., Dawkins G.P. Functional anatomy of the anterior cruciate ligament. Fibre bundle actions related to ligament replacements and injuries. J Bone Jt Surg Br. 1991;73(2):260–267. doi: 10.1302/0301-620X.73B2.2005151. [DOI] [PubMed] [Google Scholar]
- 9.Colombet P., Dejour D., Panisset J.C., Siebold R. Current concept of partial anterior cruciate ligament ruptures. Orthop Traumatol Surg Res. 2010;96(8 Suppl):S109–S118. doi: 10.1016/j.otsr.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 10.Hong S.H., Choi J.Y., Lee G.K., Choi J.A., Chung H.W., Kang H.S. Grading of anterior cruciate ligament injury. Diagnostic efficacy of oblique coronal magnetic resonance imaging of the knee. Comput Assist Tomogr. 2003;27(5):814–819. doi: 10.1097/00004728-200309000-00022. [DOI] [PubMed] [Google Scholar]
- 11.Noyes F.R., Mooar L.A., Moorman C.T., 3rd, McGinniss G.H. Partial tears of the anterior cruciate ligament. Progression to complete ligament deficiency. J Bone Jt Surg Br. 1989;71(5):825–833. doi: 10.1302/0301-620X.71B5.2584255. [DOI] [PubMed] [Google Scholar]
- 12.Sonnery-Cottet B., Chambat P. Arthroscopic identification of the anterior cruciate ligament posterolateral bundle: the figure-of-four position. Arthroscopy. 2007;23(10) doi: 10.1016/j.arthro.2006.11.028. 1128. e1-3. [DOI] [PubMed] [Google Scholar]
- 13.Sonnery-Cottet B., Barth J., Graveleau N., Fournier Y., Hager J.P., Chambat P. Arthroscopic identification of isolated tear of the posterolateral bundle of the anterior cruciate ligament. Arthroscopy. 2009;25(7):728–732. doi: 10.1016/j.arthro.2008.12.018. [DOI] [PubMed] [Google Scholar]
- 14.Maeda S., Ishibashi Y., Tsuda E., Yamamoto Y., Toh S. Intraoperative navigation evaluation of tibial translation after resection of anterior cruciate ligament remnants. Arthroscopy. 2011;27(9):1203–1210. doi: 10.1016/j.arthro.2011.03.080. [DOI] [PubMed] [Google Scholar]
- 15.Panisset J.C., Duraffour H., Vasconcelos W., Colombet P., Javois C., Potel J.F. Clinical, radiological and arthroscopic analysis of the ACL tear. A prospective study of 418 cases. Rev Chir Orthop Reparatrice Appar Mot. 2008;94(8 Suppl):362–368. doi: 10.1016/j.rco.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 16.Abat F., Gelber P.E., Erquicia J.I., Pelfort X., Tey M., Monllau J.C. Promising short-term results following selective bundle reconstruction in partial anterior cruciate ligament tears. Knee. 2013;20(5):332–338. doi: 10.1016/j.knee.2013.05.006. [DOI] [PubMed] [Google Scholar]
- 17.Dejour D., Ntagiopoulos P.G., Saggin P.R., Panisset J.C. The diagnostic value of clinical tests, magnetic resonance imaging, and instrumented laxity in the differentiation of complete versus partial anterior cruciate ligament tears. Arthroscopy. 2013;29(3):491–499. doi: 10.1016/j.arthro.2012.10.013. [DOI] [PubMed] [Google Scholar]
- 18.Robert H., Nouveau S., Gageot S., Gagnière B. A new knee arthrometer, the GNRB: experience in ACL complete and partial tears. Orthop Traumatol Surg Res. 2009;95(3):171–176. doi: 10.1016/j.otsr.2009.03.009. [DOI] [PubMed] [Google Scholar]
- 19.Araki D., Kuroda R., Matsushita T., Matsumoto T., Kubo S., Nagamune K. Biomechanical analysis of the knee with partial anterior cruciate ligament disruption: quantitative evaluation using an electromagnetic measurement system. Arthroscopy. 2013;29(6):1053–1062. doi: 10.1016/j.arthro.2013.02.012. [DOI] [PubMed] [Google Scholar]
- 20.Panisset J.C., Ntagiopoulos P.G., Saggin P.R., Dejour D. A comparison of Telos™ stress radiography versus Rolimeter™ in the diagnosis of different patterns of anterior cruciate ligament tears. Orthop Traumatol Surg Res. 2012;98(7):751–758. doi: 10.1016/j.otsr.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 21.Lorenz S., Imhoff A.B. Reconstruction of partial anterior cruciate ligament tears. Oper Orthop Traumatol. 2014;26(1):56–62. doi: 10.1007/s00064-013-0265-0. [DOI] [PubMed] [Google Scholar]
- 22.Van Dyck P., Vanhoenacker F.M., Gielen J.L., Dossche L., Van Gestel J., Wouters K. Three tesla magnetic resonance imaging of the anterior cruciate ligament of the knee: can we differentiate complete from partial tears? Skelet Radiol. 2011;40(6):701–707. doi: 10.1007/s00256-010-1044-8. [DOI] [PubMed] [Google Scholar]
- 23.Tjoumakaris F.P., Donegan D.J., Sekiya J.K. Partial tears of the anterior cruciate ligament: diagnosis and treatment. Am J Orthop (Belle Mead NJ) 2011;40(2):92–97. [PubMed] [Google Scholar]
- 24.Sonnery-Cottet B., Panisset J.C., Colombet P., Cucurulo T., Graveleau N., Hulet C. Partial A.C.L. reconstruction with preservation of the posterolateral bundle. Orthop Traumatol Surg Res. 2012;98(8 Suppl):S165–S170. doi: 10.1016/j.otsr.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 25.Kannus P., Järvinen M. Conservatively treated tears of the anterior cruciate ligament. Long-term results. J Bone Jt Surg Am. 1987;69(7):1007–1012. [PubMed] [Google Scholar]
- 26.Kocher M.S., Micheli L.J., Zurakowski D., Luke A. Partial tears of the anterior cruciate ligament in children and adolescents. Am J Sports Med. 2002;30(5):697–703. doi: 10.1177/03635465020300051201. [DOI] [PubMed] [Google Scholar]
- 27.Pujol N., Colombet P., Cucurulo T., Graveleau N., Hulet C., Panisset J.C. Natural history of partial anterior cruciate ligament tears: a systematic literature review. Orthop Traumatol Surg Res. 2012;98(8 Suppl):S160–S164. doi: 10.1016/j.otsr.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 28.Dejour D., Potel J.F., Gaudot F., Panisset J.C., Condouret J. The ACL tear from the pre-operative analysis to a 2-year follow-up, influence of the graft choice on the subjective and objective evaluation. Rev Chir Orthop Reparatrice Appar Mot. 2008;94(8 Suppl):356–361. doi: 10.1016/j.rco.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 29.Sonnery-Cottet B., Lavoie F., Ogassawara R., Scussiato R.G., Kidder J.F., Chambat P. Selective anteromedial bundle reconstruction in partial ACL tears: a series of 36 patients with mean 24 months follow-up. Knee Surg Sports Traumatol Arthrosc. 2010;18(1):47–51. doi: 10.1007/s00167-009-0855-4. [DOI] [PubMed] [Google Scholar]
- 30.Adachi N., Ochi M., Uchio Y., Iwasa J., Ryoke K., Kuriwaka M. Mechanoreceptors in the anterior cruciate ligament contribute to the joint position sense. Acta Orthop Scand. 2002;73(3):330–334. doi: 10.1080/000164702320155356. [DOI] [PubMed] [Google Scholar]
- 31.Nakamae A., Ochi M., Deie M., Adachi N., Kanaya A., Nishimori M. Biomechanical function of anterior cruciate ligament remnants: how long do they contribute to knee stability after injury in patients with complete tears? Arthroscopy. 2010;26(12):1577–1585. doi: 10.1016/j.arthro.2010.04.076. [DOI] [PubMed] [Google Scholar]
- 32.Buda R., Ruffilli A., Parma A., Pagliazzi G., Luciani D., Ramponi L. Partial ACL tears: anatomic reconstruction versus nonanatomic augmentation surgery. Orthopedics. 2013;36(9):e1108–e1113. doi: 10.3928/01477447-20130821-10. [DOI] [PubMed] [Google Scholar]
- 33.Condouret J., Cohn J., Ferret J.M., Lemonsu A., Vasconcelos W., Dejour D. Isokinetic assessment with two years follow-up of anterior cruciate ligament reconstruction with patellar tendon or hamstring tendons. Rev Chir Orthop Reparatrice Appar Mot. 2008;94(8 Suppl):375–382. doi: 10.1016/j.rco.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 34.Siebold R., Fu F.H. Assessment and augmentation of symptomatic anteromedial or posterolateral bundle tears of the anterior cruciate ligament. Arthroscopy. 2008;24(11):1289–1298. doi: 10.1016/j.arthro.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 35.Adachi N., Ochi M., Uchio Y., Iwasa J., Ryoke K., Kuriwaka M. Mechanoreceptors in the anterior cruciate ligament contribute to the joint position sense. Acta Orthop Scand. 2002;73(3):330–334. doi: 10.1080/000164702320155356. [DOI] [PubMed] [Google Scholar]
- 36.Ochi M., Adachi N., Uchio Y., Deie M., Kumahashi N., Ishikawa M. A minimum 2-year follow-up after selective anteromedial or osterolateral bundle anterior cruciate ligament reconstruction. Arthroscopy. 2009;25(2):117–122. doi: 10.1016/j.arthro.2008.10.011. [DOI] [PubMed] [Google Scholar]
- 37.Sonnery-Cottet B., Lavoie F., Ogassawara R., Scussiato R.G., Kidder J.F., Chambat P. Selective anteromedial bundle reconstruction in partial ACL tears: a series of 36 patients with mean 24 months follow-up. Knee Surg Sports Traumatol Arthrosc. 2010;18(1):47–51. doi: 10.1007/s00167-009-0855-4. [DOI] [PubMed] [Google Scholar]
- 38.Chouteau J., Testa R., Viste A., Moyen B. Knee rotational laxity and proprioceptive function 2 years after partial ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20(4):762–766. doi: 10.1007/s00167-012-1879-8. [DOI] [PubMed] [Google Scholar]
- 39.Papalia R., Franceschi F., Zampogna B., Tecame A., Maffulli N., Denaro V. Surgical management of partial tears of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2014;22(1):154–165. doi: 10.1007/s00167-012-2339-1. [DOI] [PubMed] [Google Scholar]