Abstract
Objective
To compare the clinical and radiographic results from osteosynthesis of fractures of the lateral third of the clavicle, using two methods: T plates or anchors together with Kirschner wires.
Methods
Fifteen patients of mean age 34.3 years (range: 19–57) and mean follow-up 22.7 months (range: 14–32) were evaluated. In nine cases, a T plate was used; and in six cases, coracoclavicular fixation was used with anchors in the coracoid process and Kirschner wires through the acromioclavicular joint. The evaluation included the Constant score, personal satisfaction and radiographic assessment.
Results
Both types of treatment achieved consolidation in all cases. Group 1 presented a higher Constant score (83.4) than that of Group 2 (76.4) (p = 0.029). Neither of the techniques presented any severe complications, and mild complications were only observed in Group 2 (80%), mostly consisting of migration of the Kirschner wire and superficial infection.
Conclusion
Surgical treatment of fractures of the distal clavicle using T plates provided the same consolidation rate as shown by coracoclavicular fixation with anchors in the coracoid process and Kirschner wires through the acromioclavicular joint, and better clinical results.
Level of evidence
Level III evidence was obtained. Comparative retrospective study and therapeutic study were performed.
Keywords: Bone fractures, Clavicle, Fracture fixation
Resumo
Objetivo
Comparar os resultados clínicos e radiográficos da osteossíntese de fraturas do terço lateral da clavícula com dois métodos: placa T ou âncoras associadas aos fios de Kirschner.
Métodos
Foram avaliados 15 pacientes com média de idade de 34,3 anos (19–57) e seguimento médio de 22,7 meses (14–32). Em nove casos foi usada a placa T e em seis casos a fixação coracoclavicular com âncoras no processo coracoide e fios de Kirschner através da articulação acromioclavicular (AC). A avaliação incluiu o escore de Constant, satisfação pessoal e avaliação radiográfica.
Resultados
Ambas as modalidades de tratamento obtiveram consolidação em todos os casos. O Grupo 1 apresentou escore de Constant mais elevado (83,4) quando comparado com o Grupo 2 (76,4) p = 0,029. Nenhuma das técnicas apresentou complicações graves, embora complicações leves tenham sido observadas apenas no Grupo 2 (80%), a maioria delas a migração do fio de Kirschner e infecção superficial.
Conclusão
O tratamento cirúrgico das fraturas da clavícula distal com placa T proporciona a mesma taxa de consolidação da fixação coracoclavicular com âncoras no coracoide e fios de Kirschner através da articulação AC e melhores resultados clínicos.
Nível de evidência
Nível III, estudo retrospectivo comparativo, estudo terapêutico.
Palavras-chave: Fraturas ósseas, Clavícula, Fixação de fratura
Introduction
Fractures of the distal extremity of the clavicle are a difficult and controversial problem in clinical practice.1, 2, 3, 4, 5 These injuries are not uncommon and account for 20% of all fractures of the clavicle.3, 4, 6, 7, 8, 9 Most authors agree with the indication of surgical treatment, because of the high rate of non-consolidation, which may reach 33%, with consequent pain and functional incapacity.2, 5, 7, 10, 11 The causes of this rate of non-consolidation are mechanical and anatomical. The trapezius and sternocleidomastoid pull the medial fragment superiorly and posteriorly and the weight of the arm displaces the lateral fragment distally. The small size of the distal fragment and the planar shape of the clavicle make bone contact difficult and impede consolidation.1, 2, 3, 12
Several techniques for fixation of these fractures have been described in the literature. They include use of Kirschner wires, use of tension bands, coracoclavicular fixation using sutures or screws, acromioclavicular fixation and, lastly, costly plates that have been specifically developed for these fractures, such as hook plates and locked plates. Despite the high consolidation rates achieved, most of these techniques are associated with complications and several of these routinely require removal of the material. The most frequent complications are infection, skin irritation, degenerative acromioclavicular alterations and periprosthetic fractures.4, 5, 12, 13, 14
The ideal fixation method should provide stability for the period of time needed for consolidation, cause few or preferably no complications and should not require subsequent removal of the material.
The present study retrospectively reviewed the clinical results from two surgical techniques: fixation using a T plate and coracoclavicular fixation using anchors and Kirschner wires through the acromioclavicular joint, in acute displaced fractures of the distal clavicle. The aim was to assess the clinical and radiographic differences in relation to the fixation methods and their respective complications.
Patients and methods
Approval from the research ethics committee was obtained before beginning the study (no. 0383.0.203.000-10). Each patient signed a free and informed consent statement, so as to be able to participate in the study.
Between March 2008 and March 2010, 25 patients underwent surgical fixation of displaced fractures of the distal clavicle at two different services. Ten of them were excluded from the study: three because the follow-up was insufficient, two because of insufficient data in the medical files and five because they did not return for the final assessment. Thus, 15 patients remained in the study, with ages ranging from 19 to 57 years (mean 34.3); 68.8% were male and all of the patients were right-handed. Nine fractures occurred on the right side and 11 of the cases (73.33%) resulted from high-energy trauma. According to Craig's classification, nine patients presented type II fractures, of which six were IIA and three were IIB, and six presented type V. The diagnostic criteria were clinical, comprising pain and crepitation at the fracture site, and radiographic, using the Zanca and lateral axillary views, in the cases of suspected intra-articular fracture.3
All the patients were operated by two shoulder surgeons. Each of them only applied one of the techniques: T plate or coracoclavicular fixation with anchors in association with Kirschner wires through the acromioclavicular joint. The criterion for allocating each patient was dependent on the availability of each surgeon in the appointments diary.
Nine patients were operated using the T plate technique and six using coracoclavicular fixation with anchors. All of them were operated in the deckchair position, under general anesthesia in association with interscalene brachial plexus block in order to control postoperative pain. Routine intravenous antibiotic prophylaxis was used (cefalotin, 1 g).
The fractures in group 1 were fixed using a T plate, which is generally used for volar fixation of fractures of the distal radius. The fracture was approached by means of a superior longitudinal incision starting from the acromioclavicular joint and extending 3 cm medially in relation to the fracture site, with subperiosteal dissection, anatomical reduction of the fragments and stabilization with a T plate and screws, followed by closure of the wound, compressive sterile dressings and use of a sling (Fig. 1, Fig. 2, Fig. 3).
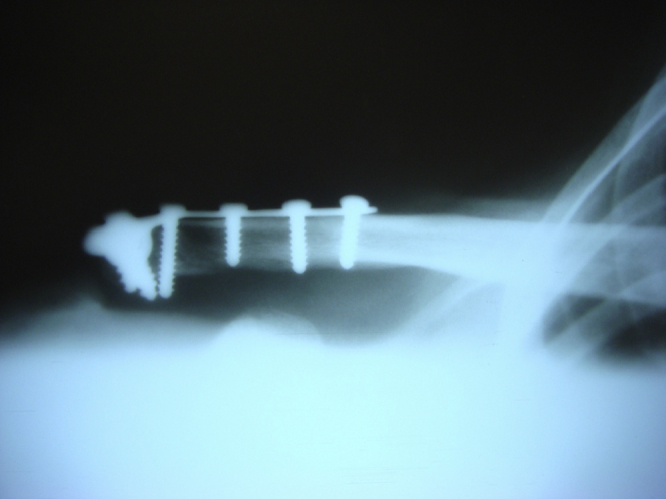
Fig. 1.

Fixation using T plate in anatomical model, in frontal view. Note the minimal protuberance of the osteosynthesis material.
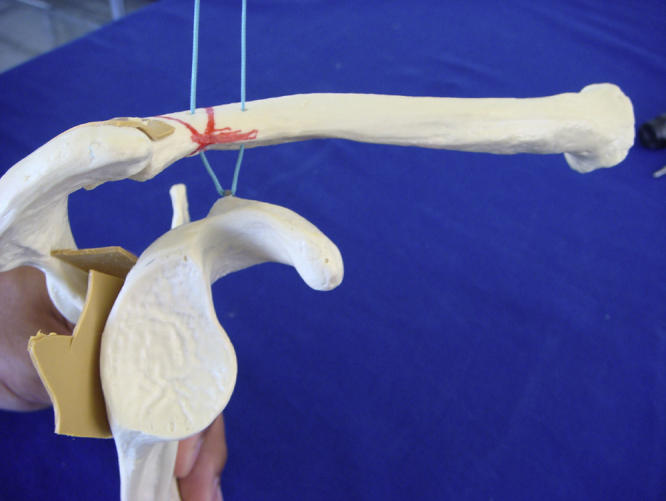
Fig. 2.

Fixation using T plate in anatomical model, in view from above.
Fig. 3.
Final radiograph by the technique using T plate. Note the greater number of screws in the distal fragment and anatomical consolidation.
The fractures in group 2 were fixed using clavicular cerclage, two anchors in the coracoid process and two Kirschner wires through the acromioclavicular joint. The access was by means of an anterior vertical incision starting from the fracture site and extending as far as the tip of the coracoid process. Two 5 mm metal anchors (Hexagon Ind. Com. Aparelhos Ortopédicos, Campinas, SP, Brazil) were fixed to the coracoid process. The suturing threads (which were non-absorbable, braided, sterile and made of polyethylene) were passed through two holes that had been made earlier in the medial fragment of the clavicle and were tied off in the anatomical position. In addition, two Kirschner wires were passed through the acromioclavicular joint in order to increase the stability; a compressive sterile dressing was applied and the limb was immobilized by means of a sling (Fig. 4, Fig. 5, Fig. 6).
Fig. 4.
Fixation using anchor in anatomical model, in frontal view.
Fig. 5.
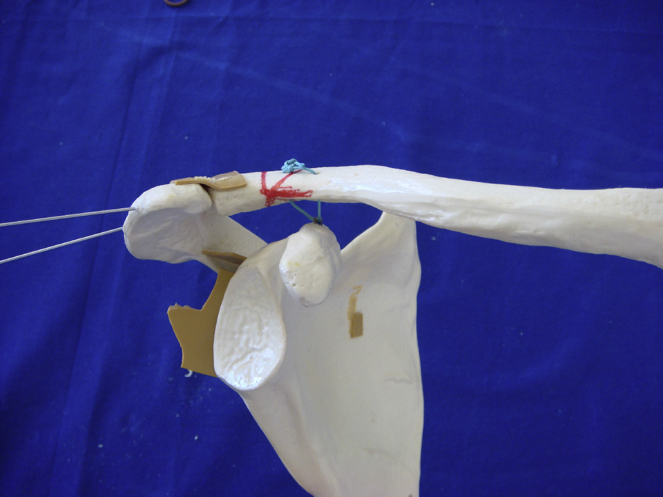
Fixation using anchor in anatomical model, in lateral view.
Fig. 6.
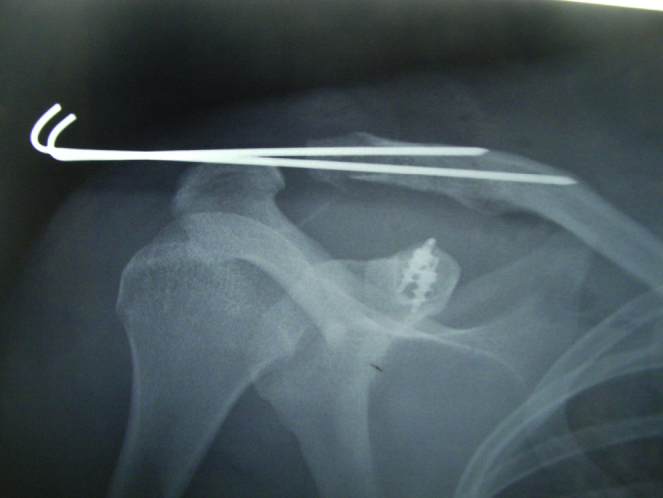
Final radiograph by the technique using anchors and Kirschner wires.
The two groups followed the same postoperative protocol. Clinical and radiographic evaluations were made by the same shoulder surgeon in the first, second and fourth weeks and monthly thereafter until the sixth month. Exercises to increase the passive range of motion (ROM) were started on the first day after the operation. The sling was used until the fourth week. In group 2, the Kirschner wires were removed in the sixth week. After full passive ROM had been attained, muscle strengthening was started.
All the patients were assessed clinically and radiographically at each outpatient visit. A visual analog scale was used to evaluate the intensity of pain (on a scale from 1 to 10). The radiographic evaluation included the Zanca and lateral axillary views. The Constant-Murley score was applied at the time of the final assessment, in the sixth month.
The SPSS 13.0 software (IBM for Mac) was used for the statistical analysis. The Fisher test was used for dichotomous variables and Student's t test was used for continuous variables. The statistical significance level was taken to be p < 0.05.
Results
The mean length of follow-up was 26.7 months (range: 18–36). All of the fractures became consolidated after four to eight weeks. There were no differences between the two groups (p > 0.05) in relation to age, gender, ROM, Craig's classification or presence of consolidation (Table 1).
Table 1.
Physical evaluation parameters of 15 patients who were operated using the T plate technique (n = 9) or coracoclavicular fixation (n = 6), between 2008 and 2010.
| Parameter | T plate | Coracoclavicular fixation |
|---|---|---|
| Elevation | 168.3 | 158 |
| External rotation | 61.7 | 58 |
| Activities of daily living | 9.6 | 8 |
| Strength | 5.9 kg | 5.7 kg |
Complications occurred only in the groups with coracoclavicular fixation, with a rate of 80%. The most frequent complications were superficial skin infection and migration of the Kirschner wires. All the cases of infection were controlled by means of removal of the wires. All the wires migrated to the exterior of the shoulder. The mean Constant score was 83.4 in group 1 and 76.4 in group 2 (p = 0.029) (Table 2).
Table 2.
Radiographic, functional and complication assessments on 15 patients who were operated due to fractures of the distal clavicle, between 2008 and 2010.
| Group 1 | Group 2 | p | |
|---|---|---|---|
| Consolidation | 100% | 100% | N.S. |
| Constant score | 83.4 | 76.4 | 0.029 |
| Complications | 0% | 80% | 0.04 |
In relation to personal satisfaction, all the patients except for one in each group were satisfied and said that they would undergo the procedure again, if necessary.
Discussion
The clavicle performs a key role in coordinating the biomechanics of the shoulder. It is the only bone connection between the axial and appendicular skeletons and supports the weight of the upper limbs. These functions emphasize the importance of achieving anatomical consolidation of fractures of the clavicle, in order to preserve the function of the upper limbs.1, 7, 10 There is a consensus in the literature that displaced fractures of the distal clavicle in young patients are an indication for surgical fixation, given that conservative treatment may lead to non-consolidation, pain, functional incapacity and personal dissatisfaction.11, 14
Fractures of the distal clavicle present some challenging issues. Their low incidence makes it difficult to prospectively compare two different types of treatment with reasonable sample sizes and lengths of follow-up. The anatomical properties of the distal fragment of the clavicle (narrow, less dense and often comminutive) make fixation with screws difficult. The subcutaneous position gives rise to skin irritation caused by the implants and frequently requires implant removal. All of this has led to development of costly exclusive anatomical plates for fixation of this pattern of fractures.4, 7, 14
There are more than 30 surgical techniques available for stabilizing these fractures. The majority present high consolidation rates. The factors that differentiate them are their costs and complication rates (infections, skin irritation, nerve injuries, need for implant removal, periprosthetic fractures, etc.).3, 4, 12
In the present study, consolidation was achieved in all the patients and most of them were personally satisfied, independent of the technique used. In group 2 (coracoclavicular fixation and Kirschner wires through the acromioclavicular joint), higher rates of complications, infection and migration of Kirschner wires were observed. All the infections were superficial and were properly treated through removal of the Kirschner wires. Although there have been reports of migration of these wires to the heart, eyes and other organs, the wires that migrated in the present study were expelled out of the shoulder.15 Another complication associated with tying off the thread (which was not observed in the present study) comprises fracturing due to erosion of the clavicle or coracoid.15, 16
Probably because of the short follow-up period, no degenerative osteoarthrosis in the acromioclavicular joint was observed, despite using Kirschner wires that passed through this joint.8, 15, 16 The methods that use fixation with a plate to stabilize fractures of the clavicle frequently require removal of the implant, probably because of the subcutaneous position of the plate, especially in cases in which the acromioclavicular joint is penetrated (hook plates). These cases may also present periprosthetic fractures.4
In the present study, there were no periprosthetic fractures. It was also not necessary to remove any plate because the one used here had a thickness of only 2 mm, whereas the thickness of DCP and hook plates is 3.5 mm.17 Special care was taken to make the incision anteriorly to the clavicle, so as to furnish a good flap of soft tissue over the plate such that the wound would not be above the plate.4, 7, 12
Other complications of hook plates include osteolysis of the acromion and erosion of the rotator cuff.17 One of the advantages of both of the methods used in this study was that there was no rigid fixation above the coracoid process or the acromion, for example using Bosworth screws, which might have delayed the rehabilitation or promoted periprosthetic fractures, because of the small but finite movement between the clavicle and the scapula.4, 5, 11, 18
In the present study, which had homogenous samples in both groups, better clinical-functional results and Constant scores were observed in the plate group. Although there were no differences in the consolidation rate, we believe that the group treated with plates began to expand the physiological range of motion earlier and also achieved the full range earlier.
The limitations of the present study were that it was retrospective and non-randomized, with a small sample of patients. On the other hand, the results presented are conclusive and provide sufficient evidence for comparing the two techniques and their results.
Conclusion
The fracture fixation technique using T plates was superior to the technique using anchors with Kirschner wires because it showed better functional results and fewer complications, while presenting the same consolidation rate. This study positions the use of T plates as an option for surgical treatment of displaced fractures of the distal clavicle.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Work developed at the Orthopedics and Shoulder and Elbow Surgery Service, Unimed Hospital of Belo Horizonte, and at Hospital Risoleta Tolentino Neves, Belo Horizonte, MG, Brazil.
References
- 1.Checchia S.L., Doneux P., Miyazaki A.N., Carvalho L.A., Caneca O.A., Jr. Fraturas da clavícula distal: tratamento e resultados. Rev Bras Ortop. 1996;31(10):838–842. [Google Scholar]
- 2.Checchia S.L., Doneux P.S., Miyazaki A.N., Fregoneze M., Silva L.A. Treatment of distal clavicle fractures using an arthroscopic technique. J Shoulder Elbow Surg. 2008;17(3):395–398. doi: 10.1016/j.jse.2007.08.011. [DOI] [PubMed] [Google Scholar]
- 3.Khan L.A.K., Bradnock T.J., Scott C., Robinson C.M. Fractures of the clavicle. J Bone Joint Surg Am. 2009;91(2):447–460. doi: 10.2106/JBJS.H.00034. [DOI] [PubMed] [Google Scholar]
- 4.Klein S.M., Badman B.L., Keating C.J., Devinney D.S., Frankle M.A., Mighell M.A. Results of surgical treatment for unstable distal clavicular fractures. J Shoulder Elbow Surg. 2010;19(7):1049–1055. doi: 10.1016/j.jse.2009.11.056. [DOI] [PubMed] [Google Scholar]
- 5.Shin S.-J., Roh K.J., Kim J.O., Sohn H.-S. Treatment of unstable distal clavicle fractures using two suture anchors and suture tension bands. Injury. 2009;40(12):1308–1312. doi: 10.1016/j.injury.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 6.Allman F.L., Jr. Fractures and ligamentous injuries of the clavicle and its articulation. J Bone Joint Surg Am. 1967;49(4):774–784. [PubMed] [Google Scholar]
- 7.Flinkkilä T., Ristiniemi J., Hyvönen P., Hämäläinen M. Surgical treatment of unstable fractures of the distal clavicle: a comparative study of Kirschner wire and clavicular hook plate fixation. Acta Orthop Scand. 2002;73(1):50–53. doi: 10.1080/000164702317281404. [DOI] [PubMed] [Google Scholar]
- 8.Nordqvist A., Petersson C., Redlund-Johnell I. The natural course of lateral clavicle fracture. 15 (11–21) year follow-up of 110 cases. Acta Orthop Scand. 1993;64(1):87–91. doi: 10.3109/17453679308994539. [DOI] [PubMed] [Google Scholar]
- 9.Robinson C.M. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br. 1998;80(3):476–484. doi: 10.1302/0301-620x.80b3.8079. [DOI] [PubMed] [Google Scholar]
- 10.Postacchini F., Gumina S., De Santis P., Albo F. Epidemiology of clavicle fractures. J Shoulder Elbow Surg. 2002;11(5):452–456. doi: 10.1067/mse.2002.126613. [DOI] [PubMed] [Google Scholar]
- 11.Robinson C.M., Akhtar M.A., Jenkins P.J., Sharpe T., Ray A., Olabi B. Open reduction and endobutton fixation of displaced fractures of the lateral end of the clavicle in younger patients. J Bone Joint Surg Br. 2010;92(6):811–816. doi: 10.1302/0301-620X.92B6.23558. [DOI] [PubMed] [Google Scholar]
- 12.Kalamaras M., Cutbush K., Robinson M. A method for internal fixation of unstable distal clavicle fractures: early observations using a new technique. J Shoulder Elbow Surg. 2008;17(1):60–62. doi: 10.1016/j.jse.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 13.Robinson C.M., Cairns D.A. Primary nonoperative treatment of displaced lateral fractures of the clavicle. J Bone Joint Surg Am. 2004;86(4):778–782. doi: 10.2106/00004623-200404000-00016. [DOI] [PubMed] [Google Scholar]
- 14.Yoo J.H., Chang J.D., Seo Y.J., Shin J.H. Stable fixation of distal clavicle fracture with comminuted superior cortex using oblique T-plate and cerclage wiring. Injury. 2009;40(4):455–457. doi: 10.1016/j.injury.2008.05.028. [DOI] [PubMed] [Google Scholar]
- 15.Leppilahti J., Jalovaara P. Migration of Kirschner wires following fixation of the clavicle – a report of 2 cases. Acta Orthop Scand. 1999;70(5):517–519. doi: 10.3109/17453679909000992. [DOI] [PubMed] [Google Scholar]
- 16.Petersson C.J. Resection of the lateral end of the clavicle. A 3 to 30-year follow-up. Acta Orthop Scand. 1983;54(6):904–907. doi: 10.3109/17453678308992931. [DOI] [PubMed] [Google Scholar]
- 17.Lin H.Y., Wong P.K., Ho W.P., Chuang T.Y., Liao Y.S., Wong C.C. Clavicular hook plate may induce subacromial shoulder impingement and rotator cuff lesion – dynamic sonographic evaluation. J Orthop Surg Res. 2014;9:6. doi: 10.1186/1749-799X-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Breslow M.J., Jazrawi L.M., Bernstein A.D., Kummer F.J., Rokito A.S. Treatment of acromioclavicular joint separation: suture or suture anchors? J Shoulder Elbow Surg. 2002;11(3):225–229. doi: 10.1067/mse.2002.123904. [DOI] [PubMed] [Google Scholar]


