Abstract
Objective
To analyze the tip–apex distance (TAD), cervicodiaphyseal angle and Garden angle in stable and unstable extracapsular fractures of the femur treated with a plate and sliding screw.
Method
Hip radiographs in anteroposterior (AP) and lateral view on 117 patients were evaluated. The fractures were classified as stable or unstable, using the AO classification, and the reduction achieved was assessed in accordance with the following criteria: TAD > 3 cm; Garden alignment index (AP) < 160°; and AP cervicodiaphyseal varus angle < 125°. When two or more criteria were present, the quality of the osteosynthesis was classified as “not ideal”.
Results
The patients with unstable fractures presented AP cervicodiaphyseal angles that were significantly greater (p = 0.05) than in those with stable fractures. The patients with unstable fractures presented lateral cervicodiaphyseal angles that were significantly smaller (p = 0.05) than in those with stable fractures. There were no significant differences in the remainder of the criteria evaluated.
Conclusion
This study did not find any significant differences in the measurements evaluated, except in relation to the cervicodiaphyseal angle. Satisfactory reduction was achieved both for the stable and for the unstable fractures, when we used a plate and sliding screw to treat proximal extracapsular fractures of the femur.
Keywords: Femoral fractures, Hip fractures, Bone screws
Resumo
Objetivo
Analisar a distância ponta-ápice (DPA), o ângulo cervicodiafisário e o ângulo de Garden em fraturas extracapsulares instáveis e estáveis do fêmur tratadas com placa e parafuso deslizante.
Método
Foram avaliadas radiografias do quadril nas incidências em anteroposterior (AP) e perfil de 117 pacientes. As fraturas foram classificadas como estáveis e instáveis, pela classificação AO, e a redução obtida foi avaliada de acordo com os critérios de distância ponta-ápice (DPA > 3 cm), índice de alinhamento de Garden (AP) < 160° e ângulo cervicodiafisário (AP) em varo < 125°. Quando dois ou mais critérios estavam presentes, a qualidade da osteossíntese foi classificada como «não ideal».
Resultados
Os pacientes com fratura instável apresentaram CD AP (p = 0,05) significativamente maior do que os estáveis. Os pacientes com fratura instável apresentaram o CD Perfil (p = 0,05) significativamente menor do que os com fratura estável. Não houve diferença significativa entre o restante dos critérios avaliados.
Conclusão
Este estudo não encontrou diferença significativa entre as medidas avaliadas, exceto o ângulo cervicodiafisário. Foi conseguida uma redução satisfatória, tanto nas fraturas estáveis como nas instáveis, quando usamos placa e parafuso deslizante nas fraturas proximais extracapsulares do fêmur.
Palavras-chave: Fraturas do fêmur, Fraturas do quadril, Parafusos ósseos
Introduction
Plates and sliding screws are currently the implants most often used for fixation of intertrochanteric fractures of the femur.1 This is because of an intrinsic characteristic of their design, which makes it possible to collapse the fracture with controlled impaction into a stable position, while maintaining a constant cervicodiaphyseal angle, without penetration of the femoral head.2, 3, 4 The plate and sliding screw join the limb together without making cuts, so as to resist penetration and the threaded screw increases the fixation in the proximal fragment. The great advantage of this is that the screw can be inserted deeply without any danger that the joint might become perforated later on, although the placement needs to be precise in order to avoid failures.5
The most common cause of failure of fixation of extracapsular fractures that are treated with plates and sliding screws relates to situations in which the screw in the femoral head cuts out. The incidence of this situation ranges from 5.3% to 16.8%.1, 2, 6, 7, 8 It occurs when the cervicodiaphyseal angle collapses in varus and the threaded screw extrudes superiorly through the femoral head.2, 3 Baumgaertner et al.2 introduced the concept of the tip–apex distance (TAD) as a strong prognostic factor for this complication.
TAD was defined by Baumgaertner et al.2 as the sum of the distance in millimeters, on radiographs in anteroposterior (AP) and lateral views, from the tip of the threaded screw to the apex of the femoral head, with appropriate correction for magnification.2, 6, 9 It has been demonstrated that TAD greater than 2.5 cm is associated with increased risk of implant failure2, 6, 9 with greater occurrence of cut-out.1, 2, 3, 6, 9, 10 Some studies have suggested that values lower than 2 cm ought to be the ideal.1
The aim of the present study was to analyze TAD, cervicodiaphyseal angle and Garden angle in stable and unstable extracapsular fractures treated with a plate and sliding screw.
Materials and methods
Between May 1998 and July 2011, 408 patients with unstable and stable extracapsular fractures of the femur underwent surgical treatment by means of reduction and fixation using a plate and sliding screw at Hospital Santa Teresa, Petrópolis, state of Rio de Janeiro. Among these, 291 patients were excluded because they presented radiographs with incorrect views or did not present one of the views needed for analysis on the TAD measurements; or because they were under 60 years of age; or because they presented pathological fractures and treatment with cephalomedullary nails. All the patients were operated on a traction table.
The technical quality of the osteosynthesis was analyzed by means of observation and using radiographs produced during the immediate postoperative period. According to Baumgaertner et al.2, 6 TAD was described as the sum of the distance in millimeters, on radiographs in anteroposterior (AP) and lateral views, from the tip of the threaded screw to the apex of the femoral head, with correction for magnification. The cervicodiaphyseal angle was measured after osteosynthesis as a line that passed through the femoral neck and femoral diaphysis. The diastasis after the reduction and osteosynthesis was also measured. The Garden alignment index,11 which analyzes the direction of the trabeculae, indicates the degree of rotation of the femoral head. In the anteroposterior projection, the cervicocephalic trabeculae form an angle of 160–175° with the medial cortical bone of the femoral diaphysis; in the lateral projection, the alignment of the trabeculae should be 180°. From the Garden alignment index, adequate reduction is taken to be a trabecular angle of between 160° and 180°, both in AP and in lateral view.
The AO classification for hip fractures was used,12 and this was subdivided into stable fractures (31 A1) or unstable fractures (31 A2) (Fig. 1, Fig. 2). The quality of the osteosynthesis was classified as “ideal” or “not ideal”, in accordance with the following criteria: (1) TAD > 3 cm; (2) Garden alignment index (AP) < 160°; and (3) cervicodiaphyseal angle (AP) in varus < 125°. When two or more criteria were present, the quality of the osteosynthesis was classified as “not ideal”.
Fig. 1.
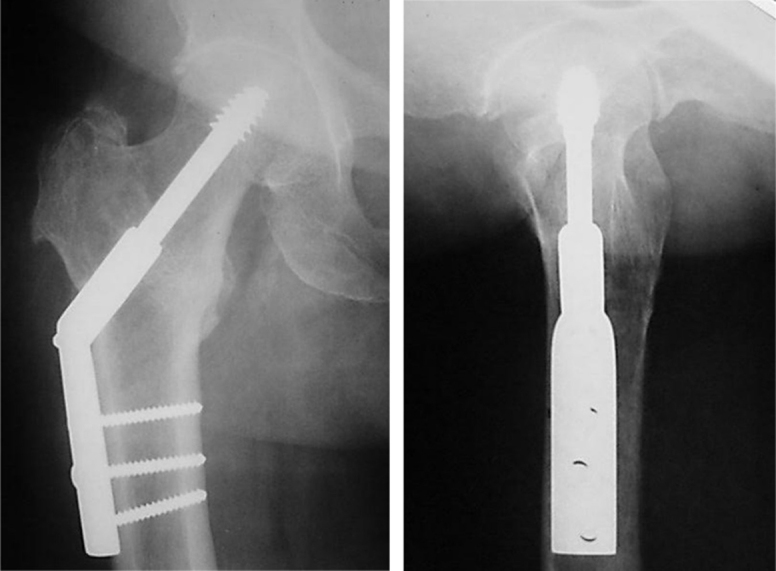
Stable intertrochanteric fracture of the femur treated with a plate and sliding screw.
Fig. 2.

Unstable intertrochanteric fracture of the femur treated with a plate and sliding screw.
Table 1 presents the characterization of the mean, standard deviation (SD), median and minimum and maximum of the numerical variables of the total sample of this study.
Table 1.
Description of the numerical variables in the total sample.
| Variable | Mean | SD | Median | Minimum | Maximum |
|---|---|---|---|---|---|
| AP | 1.21 | 0.43 | 1.20 | 0.20 | 2.50 |
| Lateral | 1.18 | 0.44 | 1.10 | 0.10 | 2.20 |
| TAD | 2.39 | 0.84 | 2.20 | 0.30 | 4.10 |
| Garden AP | 162.7 | 8.4 | 162 | 125 | 178 |
| Garden lateral | 173.1 | 4.8 | 174 | 160 | 180 |
| CD AP | 135.5 | 11.3 | 134 | 112 | 170 |
| CD lateral | 171.5 | 5.8 | 172 | 150 | 180 |
SD, standard deviation; AP, anteroposterior; TAD, tip–apex distance; CD, cervicodiaphyseal angle.
Source: Hospital Santa Teresa, Petrópolis, state of Rio de Janeiro, Brazil.
Among the 117 records examined, 74 (63.2%) related to unstable fractures, 59 (50.4%) to fractures on the right side and 66 (56.4%) to fractures in females.
Statistical methodology
The descriptive analysis presented the observed data in tables, in the form of means, standard deviations and medians.
The inferential analysis consisted of the nonparametric Mann–Whitney test for comparing the numerical variables between the subgroups of stable and unstable fractures and the χ2 (Chi-square) test for categorical variables.
A nonparametric method was used because the variables did not present normal (Gaussian) distribution, given that the hypothesis of normality was rejected through the Kolmogorov–Smirnov test.
The criterion used for determining significance was the level of 5%. The statistical analysis was processed using the SAS 6.11 software (SAS Institute, Inc., Cary, NC, USA).
Results
To show any differences among the study variables, Table 2 presents the means, standard deviations (SD) and medians of the variables according to stability (unstable or stable) and the corresponding descriptive level (p-value) from the Mann–Whitney test.
Table 2.
Analysis on variables according to stability.
| Variable | Unstable (n = 74) |
Stable (n = 43) |
p-Valuea | ||
|---|---|---|---|---|---|
| Mean ± SP | Median | Mean ± SD | Median | ||
| AP | 1.23 ± 0.43 | 1.2 | 1.17 ± 0.43 | 1.2 | 0.58 |
| Lateral | 1.22 ± 0.44 | 1.1 | 1.11 ± 0.45 | 1 | 0.19 |
| TAD | 2.45 ± 0.83 | 2.2 | 2.28 ± 0.85 | 2.2 | 0.33 |
| Garden AP | 163.0 ± 8.8 | 164 | 162.1 ± 7.9 | 162 | 0.32 |
| Garden lateral | 172.8 ± 5.0 | 174 | 173.7 ± 4.4 | 174 | 0.44 |
| CD AP | 135.6 ± 11.6 | 133 | 135.5 ± 10.8 | 134 | 0.87 |
| CD lateral | 170.7 ± 6.5 | 170 | 172.9 ± 4.1 | 172 | 0.093 |
AP, anteroposterior; TAD, tip–apex distance; CD, cervicodiaphyseal angle; SD, standard deviation.
Mann–Whitney test.
Source: Hospital Santa Teresa, Petrópolis, state of Rio de Janeiro, Brazil.
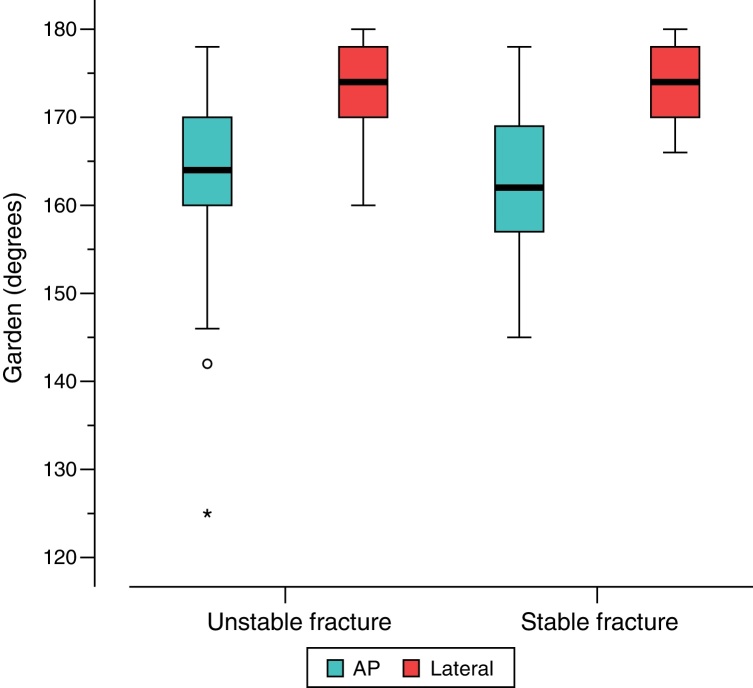
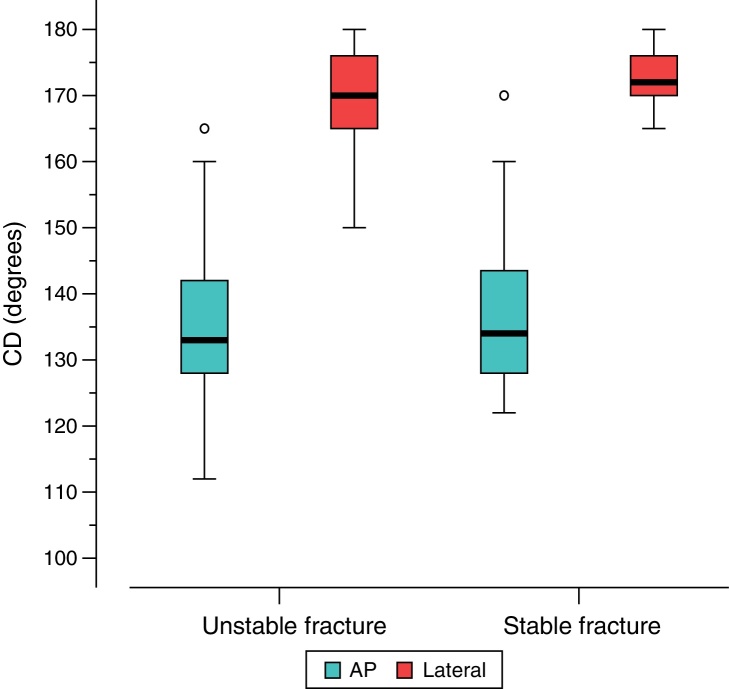
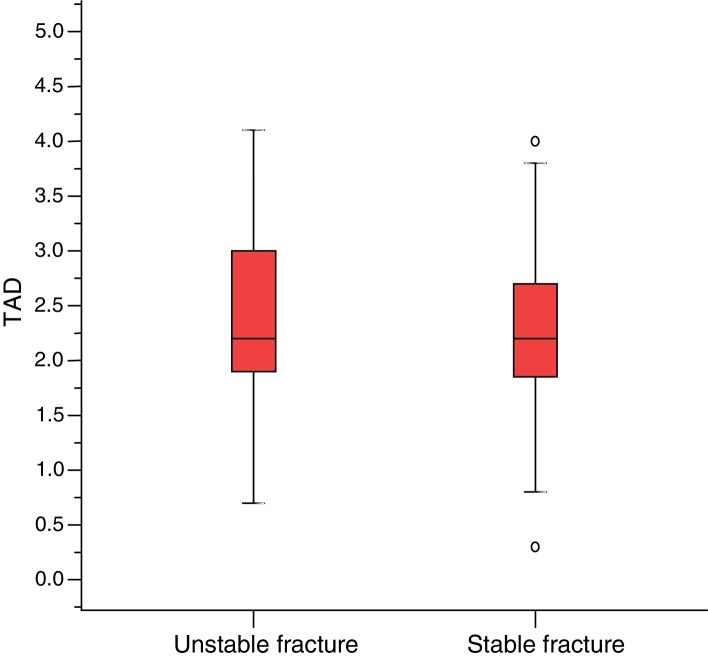
It was observed that there were no significant differences in the variables studied between the two groups of fractures, as illustrated in Fig. 3, Fig. 4, Fig. 5.
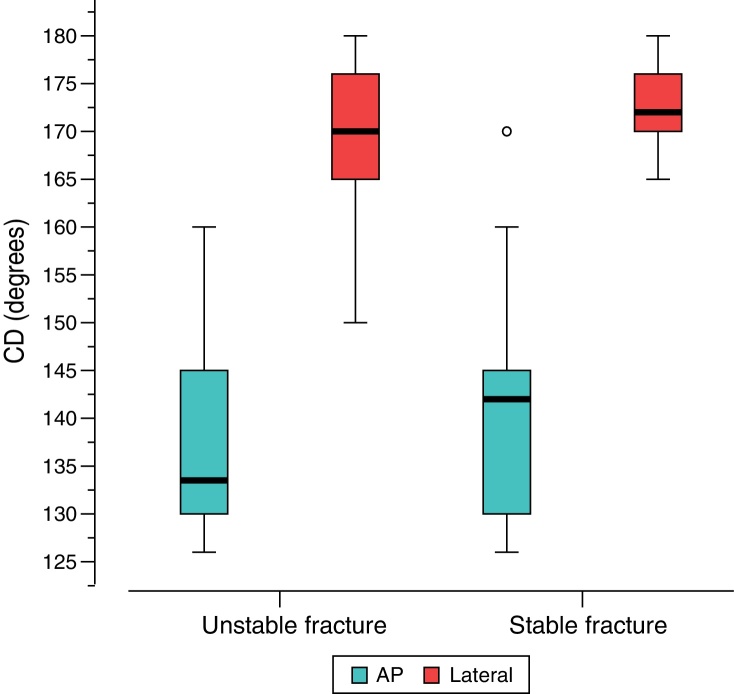
Fig. 3.
Comparison between stable and unstable fractures using the Garden angle.
Fig. 4.
Comparison between stable and unstable fractures using the cervicodiaphyseal angle (CD).
Fig. 5.
Comparison between stable and unstable fractures using the tip–apex distance (TAD).
It can be said that there was a tendency for the subgroup with unstable fractures to present a smaller cervicodiaphyseal angle in lateral view (p = 0.093) than the stable subgroup. Although clinically significant, this difference was not so great. Moreover, it was observed that the subgroup with unstable fractures presented a right-side proportion (55.4%) that was similar to that of the subgroup with stable fractures (41.7%), with p = 0.15. In addition, the subgroup with unstable fractures presented a proportion of women (54.1%) that was similar to that of the subgroup with stable fractures (60.5%), with p = 0.50.
It was also observed that there were differences in the study variables between the two groups of fractures (unstable and stable), separately according to side (right or left).
Table 3, Table 4 presented the means, standard deviations (SD) and medians of the variables according to stability (unstable or stable) and the corresponding descriptive levels (p-values) of the Mann–Whitney test, for the left and right sides, respectively.
Table 3.
Analysis on the variables according to the stability of the right side.
| Variable | Unstable (n = 41) |
Stable (n = 18) |
p-Valuea | ||
|---|---|---|---|---|---|
| Mean ± SP | Median | Mean ± SP | Median | ||
| AP | 1.20 ± 0.44 | 1.2 | 1.13 ± 0.37 | 1.15 | 0.66 |
| Lateral | 1.17 ± 0.40 | 1 | 1.04 ± 0.36 | 1.05 | 0.38 |
| TAD | 2.37 ± 0.79 | 2.2 | 2.17 ± 0.67 | 2.25 | 0.46 |
| Garden AP | 164.3 ± 7.2 | 164 | 161.9 ± 6.3 | 162 | 0.21 |
| Garden lateral | 173.1 ± 4.9 | 174 | 173.6 ± 4.3 | 174.5 | 0.81 |
| CD AP | 137.0 ± 11.4 | 135 | 131.4 ± 7.6 | 128 | 0.053 |
| CD lateral | 171.9 ± 5.4 | 172 | 172.9 ± 3.7 | 172.5 | 0.50 |
AP, anteroposterior; TAD, tip–apex distance; CD, cervicodiaphyseal angle; SD, standard deviation.
Mann–Whitney test.
Source: Hospital Santa Teresa, Petrópolis, state of Rio de Janeiro, Brazil.
Table 4.
Analysis on the variables according to the stability of the left side.
| Variable | Unstable (n = 33) |
Stable (n = 25) |
p-Valuea | ||
|---|---|---|---|---|---|
| Mean ± SP | Median | Mean ± SP | Median | ||
| AP | 1.28 ± 0.42 | 1.2 | 1.20 ± 0.48 | 1.2 | 0.61 |
| Lateral | 1.28 ± 0.47 | 1.2 | 1.15 ± 0.51 | 1 | 0.28 |
| TAD | 2.56 ± 0.87 | 2.4 | 2.35 ± 0.96 | 2.1 | 0.34 |
| Garden AP | 161.5 ± 10.3 | 164 | 162.3 ± 9.0 | 162 | 0.96 |
| Garden lateral | 172.5 ± 5.1 | 172 | 173.8 ± 4.5 | 172 | 0.33 |
| CD AP | 133.8 ± 11.7 | 130 | 138.4 ± 11.9 | 140 | 0.19 |
| CD lateral | 169.2 ± 7.5 | 170 | 172.8 ± 4.5 | 172 | 0.058 |
AP, anteroposterior; TAD, tip–apex distance; CD, cervicodiaphyseal angle; SD, standard deviation.
Mann–Whitney test.
Source: Hospital Santa Teresa, Petrópolis, state of Rio de Janeiro, Brazil.
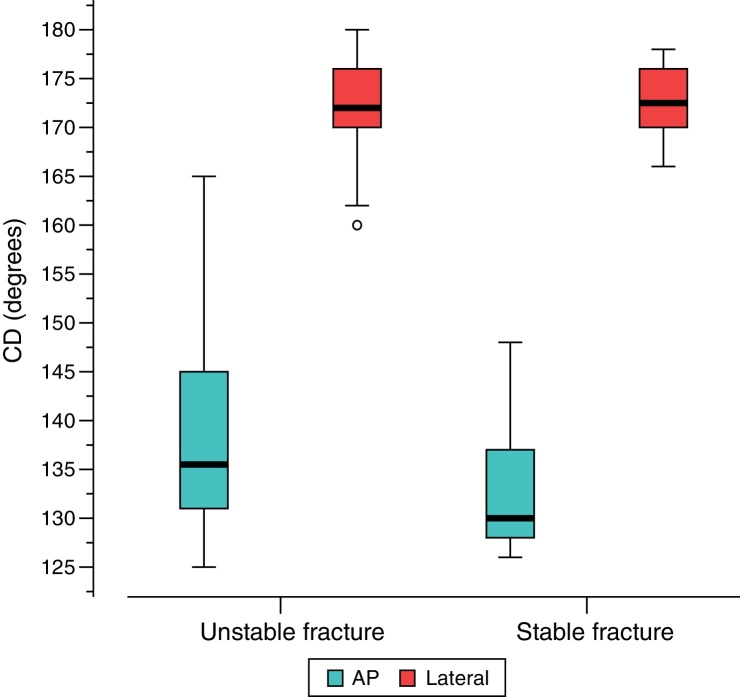
It was observed that the patients with unstable fractures presented AP cervicodiaphyseal angles that were significantly greater than those of the patients with stable fractures (p = 0.05), as shown in Fig. 6. There were no statistically significant differences in the other variables between the two subgroups.
Fig. 6.
Comparison between stable and unstable fractures using the cervicodiaphyseal angle (CD), right side.
It was also seen that the patients with unstable fractures presented lateral cervicodiaphyseal angles that were significantly smaller than those of the patients with stable fractures (p = 0.05), as shown in Fig. 6. There were no statistically significant differences in the other variables between the two subgroups of patients.
The subgroup with unstable fractures was seen to present lateral cervicodiaphyseal angles that were significantly smaller than those of the subgroup with stable fractures (p = 0.05), as shown in Fig. 7. There were no statistically significant differences in the other variables between the two subgroups at the 5% level.
Fig. 7.
Comparison between stable and unstable fractures using the cervicodiaphyseal angle (CD), left side.
Fig. 8 shows the incidence of the stable and unstable fractures relating to the 117 patients analyzed.
Fig. 8.
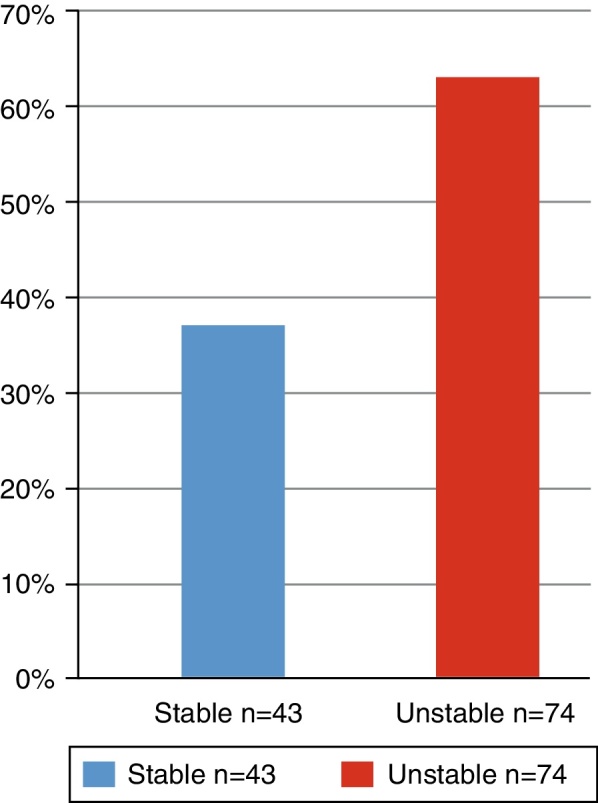
Comparison of absolute numbers between stable and unstable fractures.
Fig. 9 shows the ideal and non-ideal reductions in the stable and unstable fractures.
Fig. 9.
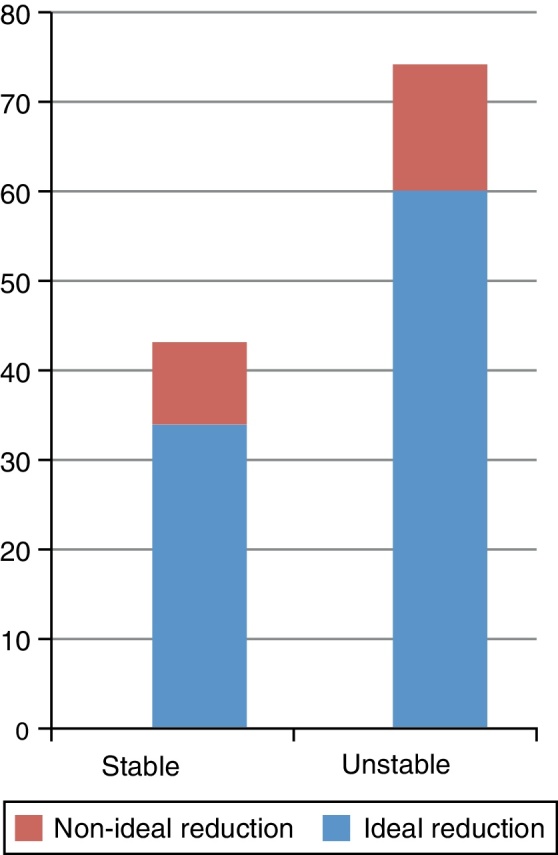
Comparison between stable and unstable fractures with ideal or non-ideal reduction.
It was seen that 79% of the stable fractures and 81% of the unstable fractures presented ideal reductions.
Discussion
In our setting, the majority of intertrochanteric fractures are still treated using plates and sliding screws. The success of treatments using this type of implant depends on the impaction of the head and neck segments in the proximal region of the femur, into a stable position. After this has been achieved, the load on the fracture will be shared between the bone and implant and the bone will absorb approximately 75% of the load transmitted.13 Kaufer14 described five variables that could affect the resistance of the combination of implant and fracture fragment: (1) bone quality; (2) fragment geometry; (3) fracture reduction; (4) implant model; and (5) implant choice. Among these, the last three are under the control of the surgeon. According to the literature, complications relating to the plate and sliding screw occur in around 16–23% of the cases. Therefore, adequate placement of the screw is fundamentally important.15, 16, 17 These complications may include loss of the reduction, pseudarthrosis, skewed consolidation with varus deformity of the femoral neck, shortening or screw cut-out.7, 16, 18, 19, 20, 21, 22, 23 Our main objective here was to analyze the positions of the plate and sliding screw through comparing stable and unstable intertrochanteric fractures.
Despite the mechanical advantages of plates and sliding screws, sliding screw cut-out remains a significant problem, especially in cases of unstable fractures. However, internal fixation of stable intertrochanteric fractures has shown low incidence of complications.5, 7, 24
Many authors have tried to quantify the positioning of the sliding screw.25, 26, 27 Clawson5 recommended that the screw should be placed 6 mm from the subchondral bone. Some authors have described the location of the screw in relation to the distance from the central axis of the femoral head and neck, on AP and lateral radiographs.25, 26, 27 The screw penetration depth has been calculated according to the number of turns that would be needed to advance the screw inside the bone. The nine-zone system used by Kyle et al.24 did not represent the screw penetration depth. Larsson et al.28 took into consideration the direction and depth of the screw and divided the femoral head into perpendicular axes and the remaining quadrants into 11 zones in both radiographs. Bridle et al.29 used similar axes, but divided each radiograph into nine areas. Parker30 used a proportional technique for defining the direction of the screw, but not its depth, in both radiographic views.
The two main methods for quantifying the positioning of the screw that have been described are the proportional method described by Parker30 and the tip–apex distance (TAD) method described by Baumgaertner et al., apud Evans31 and Garden.32 The latter method has been shown to be a useful intraoperative indicator for screw positioning at depth and for central placement in the femoral head. This is perhaps the most important indicator for precise placement of the screw and has been shown in several studies to have prognostic value after treatments for intertrochanteric fractures.2, 17, 33 TAD < 2.5 cm has been reported to represent a good prognosis for the results. However, some studies have taken the view that the ideal would be TAD < 2 cm.2, 17, 33
Several authors have reported that failures are practically nonexistent in relation to fixation of stable two-part intertrochanteric fractures.7, 34 The most common mechanical complication after using a plate and sliding screw is progressive collapse in varus through the femoral head, with proximal migration and possibly screw cut-out in the head.6, 7 Adequate positioning of the screw inside the head protects against these complications.6, 7 Nonetheless, divergences of opinion exist in relation to instability.26, 34, 35, 36 Lindskog and Baumgaertner37 demonstrated that age and unstable fractures were also independent factors for a prognosis of cut-out. Baumgaertner et al.6 reported cut-out rates ranging from 4% to 20%, with higher rates in unstable fractures. Haidukewych38 reviewed unstable fractures (AO/OTA types A3.1 and A3.3) and found complication rates of up to 56% (consisting of cut-out and pseudarthrosis) when a plate and sliding screw were used. Our results showed that there was no significant difference in TAD between stable fractures (2.28 ± 0.85 cm) and unstable fractures (2.45 ± 0.83 cm). Our TAD results of 2.39 ± 0.84 cm remained within the limit determined by Baumgaertner, i.e. below 2.5 cm. Our data do not support the hypothesis that TAD might be higher (thereby favoring complications) in cases of unstable fractures because of possible difficulty in reducing such fractures.
Studies on cadavers and radiographic studies have demonstrated that the mean cervicodiaphyseal angle in the general population is 127 ± 7°.39, 40 No significant differences in relation to side and gender have been demonstrated, despite cultural differences.41 The AP radiographic evaluation of the cervicodiaphyseal angle was shown to be more precise when the femur was internally rotated at 10°, given that external rotation might lead to an apparent increase in the cervicodiaphyseal angle.42 The present study demonstrated that good reduction is an important factor for avoiding complications. However, since no intra- or interobserver comparisons were made, we cannot conclude that there was no significant difference in cervicodiaphyseal angle on AP radiographs, between stable and unstable patients (135.5 ± 10.8° and 135.6 ± 11.6°, respectively), or on lateral-view radiographs (172.9 ± 4.1° and 170.7 ± 6.5°, respectively).
Some studies have indicated that correct reduction of fractures seen on radiographs, especially in AP view, and good correction of the trabecular angle to around 165–170° are associated with reduction of the risk of cut-out.41, 43 Pervez et al.1 confirmed the value of fracture reduction on radiographs in AP view, with an increase in cut-out rates in cases of fractures that had been reduced in varus. Fracture reduction and implant positioning are directly related. Therefore, correct reduction of the fracture is a prerequisite for implant placement.44
We observed that the cervicodiaphyseal angle in AP view was significantly greater in unstable fractures and that there was a tendency toward reduction in valgus. We also observed in lateral view that the cervicodiaphyseal angle was significantly smaller in unstable fractures, which suggested that there was a tendency toward posterior collapse.
Conclusion
The results from this study confirmed that there are no significant differences between the measurements evaluated, except the cervicodiaphyseal angle. Moreover, both for stable and for unstable fractures, good reduction is an important factor for avoiding complications when plates and siding screws are used for extracapsular fractures of the femur.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Work developed at the Prof. Dr. Donato D’Ângelo Orthopedics and Traumatology Service, Hospital Santa Teresa, and at the Petrópolis School of Medicine, Petrópolis, RJ, Brazil.
References
- 1.Pervez H., Parker M.J., Vowler S. Prediction of fixation failure after sliding hip screw fixation. Injury. 2004;35(10):994–998. doi: 10.1016/j.injury.2003.10.028. [DOI] [PubMed] [Google Scholar]
- 2.Baumgaertner M.R., Curtin S.L., Lindskog D.M., Keggi J.M. The value of the tip–apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995;77(7):1058–1064. doi: 10.2106/00004623-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Lorich D.G., Geller D.S., Nielson J.H. Osteoporotic pertrochanteric hip fractures: management and current controversies. Instr Course Lect. 2004;53:441–454. [PubMed] [Google Scholar]
- 4.Jacobs R.R., Armstrong H.J., Whitaker J.H., Pazell J. Treatment of intertrochanteric hip fractures with a compression hip screw and a nail plate. J Trauma. 1976;16(8):599–603. doi: 10.1097/00005373-197608000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Clawson Dk. Trochanteric fractures treated by the sliding screw plate fixation method. J Trauma. 1964;4:737–752. doi: 10.1097/00005373-196411000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Baumgaertner M.R., Solberg B.D. Awareness of tip–apex distance reduces failure of fixation of trochanteric fractures of the hip. J Bone Joint Surg Br. 1997;79(6):969–971. doi: 10.1302/0301-620x.79b6.7949. [DOI] [PubMed] [Google Scholar]
- 7.Davis T.R., Sher J.L., Horsman A., Simpson M., Porter B.B., Checketts R.G. Intertrochanteric femoral fractures. Mechanical failure after internal fixation. J Bone Joint Surg Br. 1990;72(1):26–31. doi: 10.1302/0301-620X.72B1.2298790. [DOI] [PubMed] [Google Scholar]
- 8.Jensen J.S., Tøndevold E., Mossing N. Unstable trochanteric fractures treated with the sliding screw-plate system. A biomechanical study of unstable trochanteric fractures III. Acta Orthop Scand. 1978;49(4):392–397. doi: 10.3109/17453677809050094. [DOI] [PubMed] [Google Scholar]
- 9.Stapley S.A., Kumar B.A., Parker M.J. The prediction of fixation failure of intertrochanteric fractures of the femur using the sliding hip screw: which is the best method? J Bone Joint Surg Br. 2000;82(Suppl. 1):56. [Google Scholar]
- 10.Walton N.P., Wynn-Jones H., Ward M.S., Wimhurst J.A. Femoral neck-shaft angle in extra-capsular proximal femoral fracture fixation: does it make a TAD of difference? Injury. 2005;36(11):1361–1364. doi: 10.1016/j.injury.2005.06.039. [DOI] [PubMed] [Google Scholar]
- 11.Ly T.V., Swiontkowski M.F. Treatment of femoral neck fractures in young adults. J Bone Joint Surg Am. 2008;90(10):2254–2266. [PubMed] [Google Scholar]
- 12.Marsh J.L., Slongo T.F., Agel J., Broderick J.S., Creevey W., DeCoster T.A. Fracture and dislocation classification compendium – 2007: Orthopaedic Trauma Association classification, database, and outcomes committee. J Orthop Trauma. 2007;21(Suppl. 10):S1–S133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 13.Frankel V.H., Burstein A.H. Lea and Febiger; Philadelphia: 1970. Orthopedics biomecanics. The application of engineering to the musculoskeletal system. [Google Scholar]
- 14.Kaufer H. Mechanics of the treatment of hip injuries. Clin Orthop Relat Res. 1980;(146):53–61. [PubMed] [Google Scholar]
- 15.Bannister G.C., Gibson A.G., Ackroyd C.E., Newman J.H. The fixation and prognosis of trochanteric fractures. A randomized prospective controlled trial. Clin Orthop Relat Res. 1990;(254):242–246. [PubMed] [Google Scholar]
- 16.Simpson A.H., Varty K., Dodd C.A. Sliding hip screws: modes of failure. Injury. 1989;20(4):227–231. doi: 10.1016/0020-1383(89)90120-4. [DOI] [PubMed] [Google Scholar]
- 17.Wolfgang G.L., Bryant M.H., O’Neill J.P. Treatment of intertrochanteric fracture of the femur using sliding screw plate fixation. Clin Orthop Relat Res. 1982;(163):148–158. [PubMed] [Google Scholar]
- 18.Kaufer H., Matthews L.S., Sonstegard D. Stable fixation of intertrochanteric fractures. J Bone Joint Surg Am. 1974;56(5):899–907. [PubMed] [Google Scholar]
- 19.Kyle R.F. Fractures of the proximal part of the femur. J Bone Joint Surg Am. 1994;76:924–950. [Google Scholar]
- 20.Madsen J.E., Naess L., Aune A.K., Alho A., Ekeland A., Strømsøe K. Dynamic hip screw with trochanteric stabilizing plate in the treatment of unstable proximal femoral fractures: a comparative study with the Gamma nail and compression hip screw. J Orthop Trauma. 1998;12(4):241–248. doi: 10.1097/00005131-199805000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Liu M., Yang Z., Pei F., Huang F., Chen S., Xiang Z. A meta-analysis of the Gamma nail and dynamic hip screw in treating peritrochanteric fractures. Int Orthop. 2010;34(3):323–328. doi: 10.1007/s00264-009-0783-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nordin S., Zulkifli O., Faisham W.I. Mechanical failure of dynamic hip screw (DHS) fixation in intertrochanteric fracture of the femur. Med J Malaysia. 2001;56(Suppl. D):12–17. [PubMed] [Google Scholar]
- 23.Saarenpää I., Heikkinen T., Ristiniemi J., Hyvönen P., Leppilahti J., Jalovaara P. Functional comparison of the dynamic hip screw and the Gamma locking nail in trochanteric hip fractures: a matched-pair study of 268 patients. Int Orthop. 2009;33(1):255–260. doi: 10.1007/s00264-007-0458-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kyle R.F., Gustilo R.B., Premer R.F. Analysis of six hundred and twenty-two intertrochanteric hip fractures. J Bone Joint Surg Am. 1979;61(2):216–221. [PubMed] [Google Scholar]
- 25.Doherty J.H., Jr., Lyden J.P. Intertrochanteric fractures of the hip treated with the hip compression screw: analysis of problems. Clin Orthop Relat Res. 1979;(141):184–187. [PubMed] [Google Scholar]
- 26.Greider J.L., Jr., Horowitz M. Clinical evaluation of the sliding compression screw in 121 hip fractures. South Med J. 1980;73(10):1343–1348. doi: 10.1097/00007611-198010000-00016. [DOI] [PubMed] [Google Scholar]
- 27.Mulholland R.C., Gunn D.R. Sliding screw plate fixation of intertrochanteric femoral fractures. J Trauma. 1972;12(7):581–591. doi: 10.1097/00005373-197207000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Larsson S., Friberg S., Hansson L.I. Trochanteric fractures. Mobility, complications, and mortality in 607 cases treated with the sliding-screw technique. Clin Orthop Relat Res. 1990;(260):232–241. [PubMed] [Google Scholar]
- 29.Bridle S.H., Patel A.D., Bircher M., Calvert P.T. Fixation of intertrochanteric fractures of the femur. A randomised prospective comparison of the Gamma nail and the dynamic hip screw. J Bone Joint Surg Br. 1991;73(2):330–334. doi: 10.1302/0301-620X.73B2.2005167. [DOI] [PubMed] [Google Scholar]
- 30.Parker M.J. Cutting-out of the dynamic hip screw related to its position. J Bone Joint Surg Br. 1992;74(4):625. doi: 10.1302/0301-620X.74B4.1624529. [DOI] [PubMed] [Google Scholar]
- 31.Evans E.M. Trochanteric fractures; a review of 110 cases treated by nail-plate fixation. J Bone Joint Surg Br. 1951;33(2):192–204. [PubMed] [Google Scholar]
- 32.Garden R.S. Low-angle fixation in fractures of the femoral neck. J Bone Joint Surg Br. 1961;43:647–663. [Google Scholar]
- 33.Levy R.N., Capozzi J.D., Mont M.A. Intertrochanteric hip fractures. In: Browner D., Jupiter J., Levine A., Tafton P., editors. Skeletal trauma: fractures, dislocations, ligamentous injuries. Saunders; Philadelphia: 1992. pp. 1442–1484. [Google Scholar]
- 34.Watson J.T., Moed B.R., Cramer K.E., Karges D.E. Comparison of the compression hip screw with the Medoff sliding plate for intertrochanteric fractures. Clin Orthop Relat Res. 1998;(348):79–86. [PubMed] [Google Scholar]
- 35.Chirodian N., Arch B., Parker M.J. Sliding hip screw fixation of trochanteric hip fractures: outcome of 1024 procedures. Injury. 2005;36(6):793–800. doi: 10.1016/j.injury.2005.01.017. [DOI] [PubMed] [Google Scholar]
- 36.Larsson S., Friberg S., Hansson L.I. Trochanteric fractures. Influence of reduction and implant position on impaction and complications. Clin Orthop Relat Res. 1990;(259):130–139. [PubMed] [Google Scholar]
- 37.Lindskog D.M., Baumgaertner M.R. Unstable intertrochanteric hip fractures in the elderly. J Am Acad Orthop Surg. 2004;12(3):179–190. doi: 10.5435/00124635-200405000-00006. [DOI] [PubMed] [Google Scholar]
- 38.Haidukewych G.J. Intertrochanteric fractures: ten tips to improve results. J Bone Joint Surg Am. 2009;91(3):712–719. [PubMed] [Google Scholar]
- 39.Isaac B., Vettivel S., Prasad R., Jeyaseelan L., Chandi G. Prediction of femoral neck-shaft angle from the length of the femoral neck. Clin Anat. 1997;10(5):318–323. doi: 10.1002/(SICI)1098-2353(1997)10:5<318::AID-CA5>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 40.Reikeras O., Hoiseth A., Reigstad A., Fonstelien E. Femoral neck angles: a specimen study with special regard to bilateral differences. Acta Orthop Scand. 1982;53(5):775–779. doi: 10.3109/17453678208992291. [DOI] [PubMed] [Google Scholar]
- 41.Parker M.J. Valgus reduction of trochanteric fractures. Injury. 1993;24(5):313–316. doi: 10.1016/0020-1383(93)90053-9. [DOI] [PubMed] [Google Scholar]
- 42.Kay R.M., Jaki K.A., Skaggs D.L. The effect of femoral rotation on the projected femoral neck-shaft angle. J Paediatr Orthop. 2000;20(6):736–739. doi: 10.1097/00004694-200011000-00007. [DOI] [PubMed] [Google Scholar]
- 43.Bonamo J.J., Accettola A.B. Treatment of intertrochanteric fractures with a sliding nail-plate. J Trauma. 1982;22(3):205–215. doi: 10.1097/00005373-198203000-00006. [DOI] [PubMed] [Google Scholar]
- 44.Lima A.L.P., Azevedo Filho A.J., Amaral N.P., Franklin C.E., Giordano V. Tratamento das fraturas intertrocanterianas com placa e parafuso deslizante. Rev Bras Ortop. 2003;38(5):271–280. [Google Scholar]