Abstract
Although tumors or pseudotumoral lesions are rare in the infrapatellar fat, they may affect it. Osteochondroma is the commonest benign bone tumor. However, extraskeletal presentations are rare. There are three extraskeletal variants of osteochondroma: synovial chondromatosis, para-articular chondroma and soft-tissue chondroma. We present a case of a single intra-articular lesion in the area of Hoffa's fat, in a 78-year-old female patient with a complaint of progressive knee pain associated with severe arthrosis. From the clinical and radiological findings, the diagnosis was para-articular osteochondroma. However, the histopathological findings, after excision of the lesion, showed that this was synovial chondromatosis secondary to osteoarthrosis.
Keywords: Adipose tissue, Osteochondroma, Synovial chondromatosis
Resumo
Tumores ou lesões pseudotumorais, apesar de raros, podem acometer a gordura infrapatelar. O osteocondroma é o tumor ósseo benigno mais comum. Entretanto, sua apresentação extraesquelética é rara. Três são as variantes do osteocondroma extraesquelético: a condromatose sinovial, o condroma para-articular e o condroma de partes moles. Apresentamos um caso de lesão intra-articular única na topografia da gordura de Hoffa em uma paciente feminina de 78 anos com queixa de dor progressiva em joelho associada a artrose grave. Pelos achados clínicos e radiológicos o diagnóstico foi de osteocondroma para-articular. Entretanto, os achados histopatológicos – após exérese da lesão – evidenciaram condromatose sinovial secundária a osteoartrose.
Palavras-chave: Tecido adiposo, Osteocondroma, Condromatose sinovial
Introduction
The infrapatellar fat pad, also known as Hoffa's fat, is an intra-articular and extrasynovial structure that forms part of the anterior compartment of the knee.
The main ailments that affect Hoffa's fat are degenerative joint disease, inflammatory pathological conditions and sequelae of trauma. Tumors or pseudotumoral lesions may also affect this fat pad, although these are rare.
Because of abundant innervation, these alterations frequently present significant symptoms, although the presence of calcifications has only been reported in a small number of cases.
Here, we report on a case of a single intra-articular lesion in the anterior compartment that was associated with severe arthrosis.
Case report
The patient was a 78-year-old black woman with hypertension and diabetes who complained of progressive pain in her left knee that had been evolving over a period of more than 6 years, in association with functional limitation. On physical examination, her axis was seen to present valgus of 15° and she had muscle atrophy of ++/3+. She had a painful range of motion from 10° to 130°, which was associated with crepitation in three compartments. Palpation showed that the volume in the infrapatellar region was greater than normal, with hardened consistency and limited mobility.
Radiographic examinations showed a calcified oval-shaped infrapatellar image with well-delimited outlines, and also hypodense areas associated with degenerative alterations and joint pinching in the lateral femorotibial space. Examinations on the patient from 3 years earlier documented the same lesion and showed that there had not been any radiographic alterations over the past 36 months (Fig. 1).
Fig. 1.
(A) Anteroposterior radiograph. (B) Lateral-view radiograph of tumor formation in the anterior compartment of the knee.
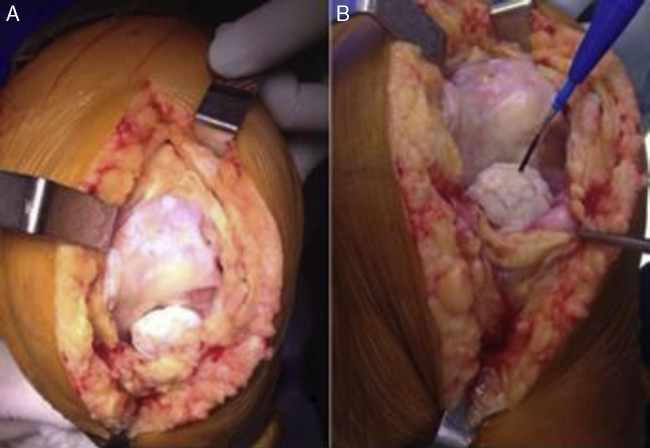
Because the lesion presented benign characteristics, we chose to resect it en-bloc and perform total knee arthroplasty within the same operation. A medial parapatellar access to the left knee was opened and this showed a mass with hardened characteristics, visible laminas in the cartilage, well-defined outlines and lack of adherence to deep planes. We did not identify any communication with the femur or tibia (Fig. 2).
Fig. 2.
Intraoperative appearance of the lesion.
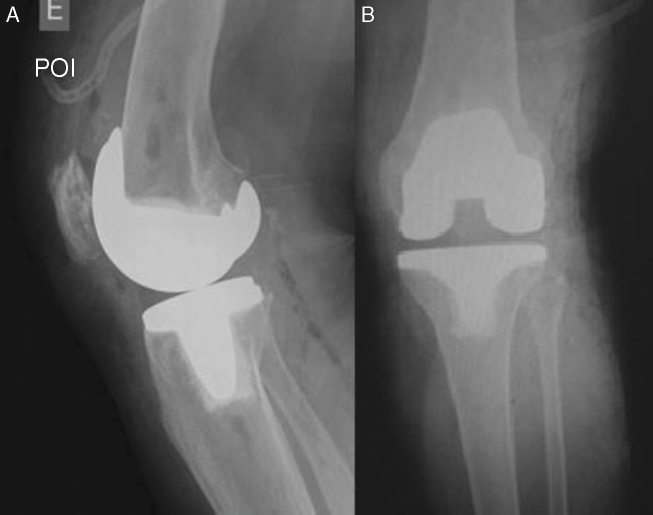
After tumor resection and implantation of the prosthetic component, the patient evolved without complications (Fig. 3).
Fig. 3.
(A) postoperative lateral-view radiograph. (B) Postoperative anteroposterior radiograph.
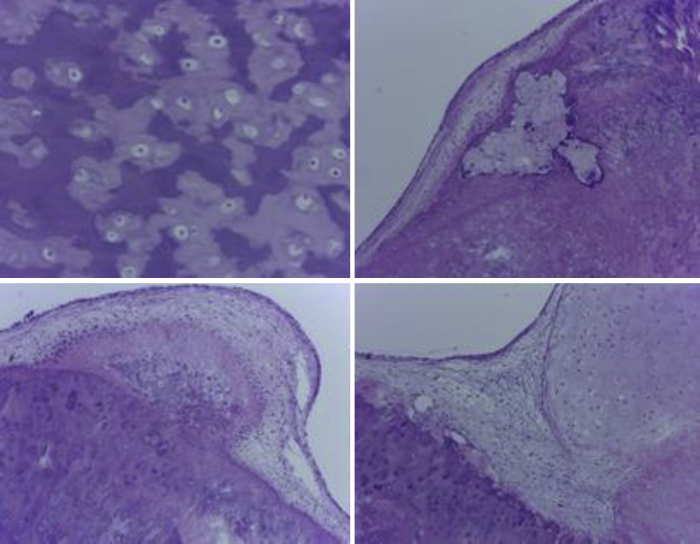
Anatomopathological examination revealed a nodule with a knobbly surface of whitish gray color, measuring 3.3 cm × 2.5 cm. After sectioning, it was seen to have a stratified appearance of hardened consistency and there was also a central cavity measuring 1.6 cm × 0.5 cm (Fig. 4). Under a microscope, the nodule was seen to be formed by typical chondrocytes that were immersed in a chondroid matrix and distributed in a stratified manner, with areas of calcification, ossification and degeneration, and with formation of pseudocysts. The lesion was covered by a synovial membrane and it displayed flattened coating cells. The diagnosis was concluded to be synovial chondromatosis (Fig. 5).
Fig. 4.
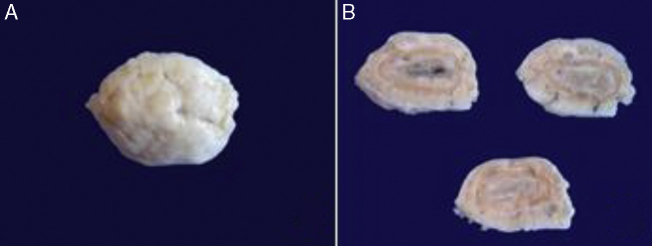
(A) Anatomical specimen. (B) Sections through the specimen showing central cavity.
Fig. 5.
Analysis under microscope, showing typical chondrocytes that were immersed in a chondroid matrix and distributed in a stratified manner, with areas of calcification.
Discussion
Osteochondromas are the commonest benign bone tumors and are often located in the metaphyseal region of the long bones. However, extraskeletal presentations of these tumors are rare.1 There are three variants of extraskeletal osteochondroma: synovial chondromatosis, para-articular chondroma and soft-tissue chondroma.2
Synovial chondromatosis of the knee is an uncommon entity. Knowledge on this subject is based on reports on single cases or small series of cases. It is defined as benign proliferation of multiple cartilaginous bodies in the synovial tissue that is present in joints, bursas or tendinous sheaths.3 It is believed that free cartilaginous fragments in joints undergo calcification and/or ossification through the process of metaplasia formation.3
The process of metaplasia formation can be divided into three phases: confined to the synovial membrane; activation of the synovial membrane; progression to free bodies; and a late stage with an inactive synovial membrane and residual free bodies.4
Milgram divided synovial chondromatosis into three categories: (a) free bodies originating from osteochondral fractures; (b) degenerative arthritis or avascular necrosis that leads to fragmentation of the cartilage; (c) primary synovial chondromatosis.4 In cases of chondromatosis secondary to osteoarthrosis, as presented here, metaplasia is formed in fragments coming from subchondral fractures or in fragmented cartilage.4
The clinical condition generally affects a single joint. The knees are the most frequent location, followed by the hips, shoulders and elbows.5 This condition affects individuals between their third and fifth decades of life, and especially males.5, 6 The symptoms are pain, edema and limitations on the range of movement.5, 6 The results from the physical examination range from normal to a finding of a palpable mass.5
The radiographic findings comprise multiple lesions that are rounded or oval-shaped, of regular outline and with a calcified appearance. The main differential diagnosis for synovial chondromatosis is synovial sarcoma, in which the calcification is irregular, coarse and generally extra-articular.3
The treatment is surgical, with excision of the lesions, preferably combined with total synovectomy.6 Partial synovectomy has been correlated with greater recurrence of the lesions.7
Para-articular osteochondromas are often located in the knees, but cases in the elbows, hips and ankles have also been reported.8 Around 50 cases of para-articular osteochondromas have already been described.8 Hoffa's fat is the most prevalent location in the knees.8 The presence of residual synovial tissue possibly demonstrates that the primary neoplastic conditions originated in and were confined to this structure.9
Reith et al.2 defined three criteria for diagnosing para-articular osteochondroma: a single lesion, as seen radiologically and clinically; histologically composed of bone and cartilaginous tissue; and presentation as an extrasynovial lesion.
The nomenclature used to describe this condition is confusing. Similar lesions have previously been reported as capsular osteochondroma, extraskeletal osteochondroma, ossifying chondroma, para-articular chondroma, giant extrasynovial intra-articular osteochondroma and Hoffa's disease.1
Complete resolution of the symptoms occurs in the majority of the cases, after complete excision of the lesion. Lesion recurrence is a rare event.1, 10
It is believed that because of the clinical, radiological and histopathological similarity between Hoffa's disease and intra-articular chondromas, these conditions are closely related. Mechanical alterations such as valgus or recurvatum, and rotational instability, contribute toward increasing the impact between these structures.10
The radiological diagnosis is based on viewing the osteochondroma in its corresponding setting, but it only becomes visible after the process of ossification.10 Histologically, trabeculated bone that is characteristic of endochondral ossification is presented, with a covering of hyaline cartilage.1, 8
We therefore conclude that, in the case presented here, the radiographic findings of a single lesion and its location inside Hoffa's fat favor a diagnosis of para-articular osteochondroma secondary to Hoffa's disease. However, histologically, the lesion was compatible with synovial chondromatosis. This diagnosis was probably related to the associated condition of severe osteoarthrosis of the knee.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Work developed at the Knee Surgery Center of the National Institute of Traumatology and Orthopedics, Rio de Janeiro, RJ, Brazil.
References
- 1.Sanga S., Goswami G., Negi R.S. Intra-articular osteochondroma: a case report. NHL J Med Sci. 2013;2(1):77–78. [Google Scholar]
- 2.Reith J.D., Bauer T.W., Joyce M.J. Paraarticular osteochondroma of the knee: report of two cases and review of literature. Clin Orthop Relat Res. 1997;(334):225–232. [PubMed] [Google Scholar]
- 3.Perry B.E., McQueen D.A., Lin J.J. Synovial chondromatosis with malignant degeneration to chondrosarcoma. J Bone Joint Surg Am. 1988;70(8):1259–1261. [PubMed] [Google Scholar]
- 4.Milgram J.W. The classification of loose bodies in human joints. Clin Orthop Relat Res. 1977;(124):282–291. [PubMed] [Google Scholar]
- 5.Lewis M., Marshall J., Mirra J.M. Synovial chondromatosis of the thumb. J Bone Joint Surg Am. 1974;56(1):180–183. [PubMed] [Google Scholar]
- 6.Filho J.S., Carvalho R.T., Sayum J., Matsuda M.M., Cohen M. Condromatose sinovial de joelho: relato de caso. Rev Bras Ortop. 2011;46(5):605–606. doi: 10.1016/S2255-4971(15)30420-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oglive-Harris D.J., Saleh K. Generalized synovial chondromatosis of the knee: a comparison of removal of the loose bodies alone with arthroscopic synovectomy. Arthroscopy. 1994;10(2):166–170. doi: 10.1016/s0749-8063(05)80088-x. [DOI] [PubMed] [Google Scholar]
- 8.Sen M.D., Satija B.L., Kumar K.S., Rastogi V., Sunita B.S. Giant intra-articular extrasynovial osteochondroma of the Hoffa's fat pad: a case report. MJAFI. 2012:1–4. doi: 10.1016/j.mjafi.2012.11.005. Available at: http://www.mjafi.net/article/S0377-1237%2812%2900254-7/fulltext. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saddik D., McNally E.G., Richardson M. MRI of Hoffa's fat pad. Skelet Radiol. 2004;33(8):433–444. doi: 10.1007/s00256-003-0724-z. [DOI] [PubMed] [Google Scholar]
- 10.Lourenço R.B., Rodrigues M.B. Which is your diagnosis? Radiol Bras. 2007;40(3):9–10. [Google Scholar]