Abstract
Objective
To evaluate the presence of the anterolateral ligament (ALL) of the knee in magnetic resonance imaging (MRI) examinations.
Methods
Thirty-three MRI examinations on patients’ knees that were done because of indications unrelated to ligament instability or trauma were evaluated. T1-weighted images in the sagittal plane and T2-weighted images with fat saturation in the axial, sagittal and coronal planes were obtained. The images were evaluated by two radiologists with experience of musculoskeletal pathological conditions. In assessing ligament visibility, we divided the analysis into three portions of the ligament: from its origin in the femur to its point of bifurcation; from the bifurcation to the meniscal insertion; and from the bifurcation to the tibial insertion. The capacity to view the ligament in each of its portions and overall was taken to be a dichotomous categorical variable (yes or no).
Results
The ALL was viewed with signal characteristics similar to those of the other ligament structures of the knee, with T2 hyposignal with fat saturation. The main plane in which the ligament was viewed was the coronal plane. Some portion of the ligament was viewed clearly in 27 knees (81.8%). The meniscal portion was evident in 25 knees (75.7%), the femoral portion in 23 (69.6%) and the tibial portion in 13 (39.3%). The three portions were viewed together in 11 knees (33.3%).
Conclusion
The anterolateral ligament of the knee is best viewed in sequences in the coronal plane. The ligament was completely characterized in 33.3% of the cases. The meniscal portion was the part most easily identified and the tibial portion was the part least encountered.
Keywords: Knee, Joint instability, Magnetic resonance imaging, Anatomy
Resumo
Objetivo
Avaliar a presença do ligamento anterolateral (LAL) do joelho em exames de ressonância magnética (RM).
Métodos
Foram avaliadas 33 RM de joelho de pacientes feitas por indicações não relacionadas a instabilidade ligamentar ou trauma. Foram obtidas imagens no plano sagital ponderadas em T1 e imagens nos planos axial, sagital e coronal ponderadas em T2 com saturação de gordura. As imagens foram avaliadas por dois radiologistas experientes em patologias musculoesqueléticas. Na avaliação da visualização, dividimos a análise do ligamento em três porções: origem femoral até o seu ponto de bifurcação, da bifurcação até a inserção meniscal e da bifurcação até a inserção tibial. Considerou-se com variável categórica dicotômica (sim ou não) a capacidade de visualizar o ligamento em cada uma das porções e no seu todo.
Resultados
O LAL foi visualizado com característica de sinal semelhante às demais estruturas ligamentares do joelho, com hipossinal em T2 com saturação de gordura. O principal plano em que o ligamento foi identificado foi o coronal. Alguma porção do ligamento foi visualizada com clareza em 27 (81,8%) joelhos. A porção meniscal ficou evidente em 25 (75,7%) dos joelhos, a porção femoral em 23 (69,6%) e a tibial em 13 (39,3%). As três porções foram visualizadas em conjunto em 11 (33,3%) joelhos.
Conclusão
O ligamento anterolateral do joelho é mais bem visualizado em sequências no plano coronal. O ligamento foi caracterizado por completo em 33,3% dos casos. A porção meniscal foi a mais facilmente identificada e a tibial a menos encontrada.
Palavras chave: Joelho, Instabilidade articular, Imagem por ressonância magnética, Anatomia
Introduction
The anterolateral ligament (ALL) of the knee was mentioned in the orthopedic literature for the first time by Segond in 1879 with Vincent et al.1 Although it was described more than 120 years ago, this ligament was named recently by Vieira et al.2 in a study on the iliotibial tract. Subsequently, starting in 2012, some anatomical studies came out, with the objective of defining parameters for the origin and insertion of the ALL, its path and other particular features.1, 3, 4, 5
Recent studies have demonstrated that the origin of the ALL is anterior and distal to the origin of the lateral collateral ligament (LCL). The ALL is located between the LCL and the tendon of the popliteal muscle, in the lateral femoral condyle. It has an oblique path toward the tibia, with two distinct insertions: one in the lateral meniscus and the other in the proximal tibia, between Gerdy's tubercle and the head of the fibula.5
Weber cited some aspects of the ALL in a study using magnetic resonance imaging (MRI) of the knee. This author reported that its length varied from 4.2 cm in flexion to 3.9 cm in extension, which suggests that it is under greater tension in flexion.6 Claes et al.7 evaluated 350 MRI scans on anterior cruciate ligament (ACL) injuries, searching for visualization of the ALL, and reported having viewed this structure in 95.7% of the cases.
Recently, greater importance has been placed on this ligament. There have been suggestions that this structure may present an association with ACL injuries and with the genesis of anterolateral knee instability.1, 3, 4, 5, 8 Thus, studies in which the ALL is identified by means of imaging examinations have become necessary.
The aim of the present study was to evaluate the presence of the ALL in knee MRI examinations. As a secondary objective, the aim was to assess what the best orientation for viewing the ALL would be.
Materials and methods
Thirty-three MRI scans on the knees of patients who underwent the examination due to clinical indications unrelated to knee ligament stability or trauma were evaluated with regard to lesions of the patellar cartilage. None of the patients presented any ligament lesions, meniscal lesions or chondral lesions in locations other than the patella. The patients’ mean age was 32.5 ± 8.1 years (ranging from 21 to 49). Seven patients were male and 26 were female.
The examinations were performed in a machine with a 1.5-Tesla magnetic field (Sigma HDxT, General Electric Medical Systems, Milwaukee, Wisconsin, USA), using an eight-channel knee coil (HD TR knee array). T1-weighted images were obtained in the sagittal plane (TR/TE, 400–700/9–16) and T2-weighted images with fat saturation in the axial, sagittal and coronal planes (TR/TE, 3200–4500/40–50), with slice thickness of 3 mm and spacing of 0.5 mm.
The MRI scans were evaluated by two radiologists with experience of musculoskeletal pathological conditions, especially knee ligament injuries. Each evaluator made two evaluations with a minimum interval of 30 days between them. In the event of lack of agreement in the evaluations, two other evaluators viewed the MRI scans to determine whether the structure was present or not.
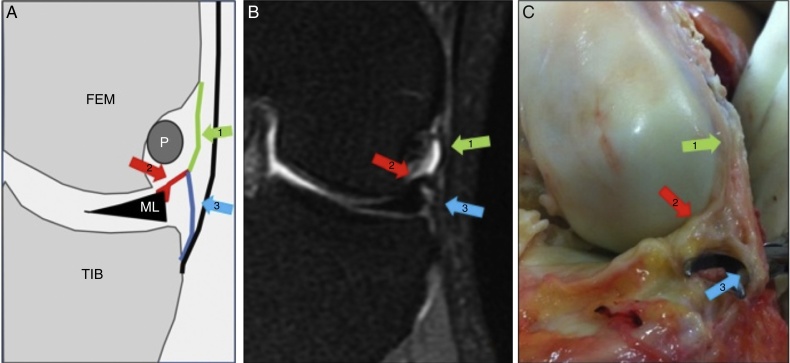
In evaluating the views of the ALL, we divided the analysis into three portions of the ligament:5 (1) from the femoral origin to the point of bifurcation; (2) from the bifurcation to the meniscal insertion; and (3) from the bifurcation to the tibial insertion (Fig. 1). For didactic purposes, these portions are called the femoral, meniscal and tibial portions here.
Fig. 1.
(A) Schematic drawing; (B) coronal MRI slice; (C) anatomical photo of the ALL of the knee. In these three images, arrow 1 (green) represents the femoral portion, arrow 2 (red) the meniscal portion and arrow 3 (blue) the tibial portion. P, tendon of the popliteal muscle; FEM, lateral femoral condyle; TIB, lateral tibial plateau. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of the article.)
The capacity to view the ligament in each of the portions and in its entirety was considered to be a dichotomous categorical variable (yes or no).
Results
The ALL was viewed on the knee MRI scans as a thin linear structure, with an outline that sometimes was regular and sometimes was undulating. It presented signal characteristics similar to those of the other ligament structures of the knee, with hyposignal seen on T2 images with fat saturation.
The main plane in which the ligament was identified was the coronal plane. The femoral portion was identified as a structure with its origin close to the anterior limit of the origin of the LCL, with an inferior path that was practically vertical and superficial to the popliteal tendon, with bifurcation less than 0.5 cm from the corpus of the lateral meniscus. The meniscal portion of the ligament presented an anteroinferior oblique path from the bifurcation toward the anterior corpus–cornu transition of the meniscus, viewed on subsequent coronal slices. The tibial portion was best characterized immediately after the bifurcation, with a lateral and practically vertical path. It maintained proximity to the iliotibial tract, with its insertion slightly posteriorly to Gerdy's tubercle (Fig. 2).
Fig. 2.
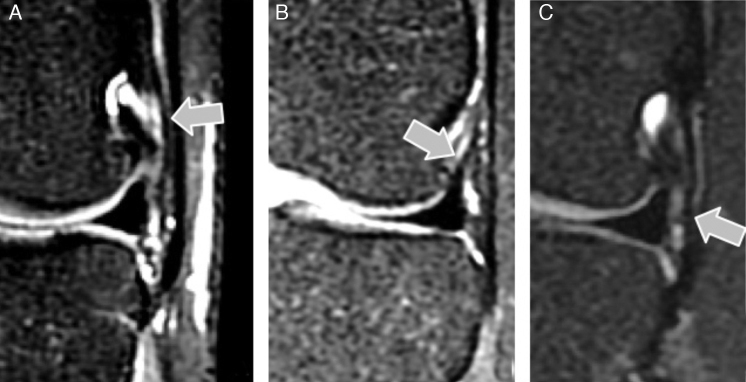
T2-weighted coronal MRI slice with fat saturation showing: (A) femoral portion; (B) meniscal portion; and (C) tibial portion of the ALL of the knee.
The characterization of the ligament in the sequences acquired in the axial and sagittal planes was limited. These sequences were used for confirming the location of the ALL, based on parameters from anatomical studies (Fig. 3).
Fig. 3.
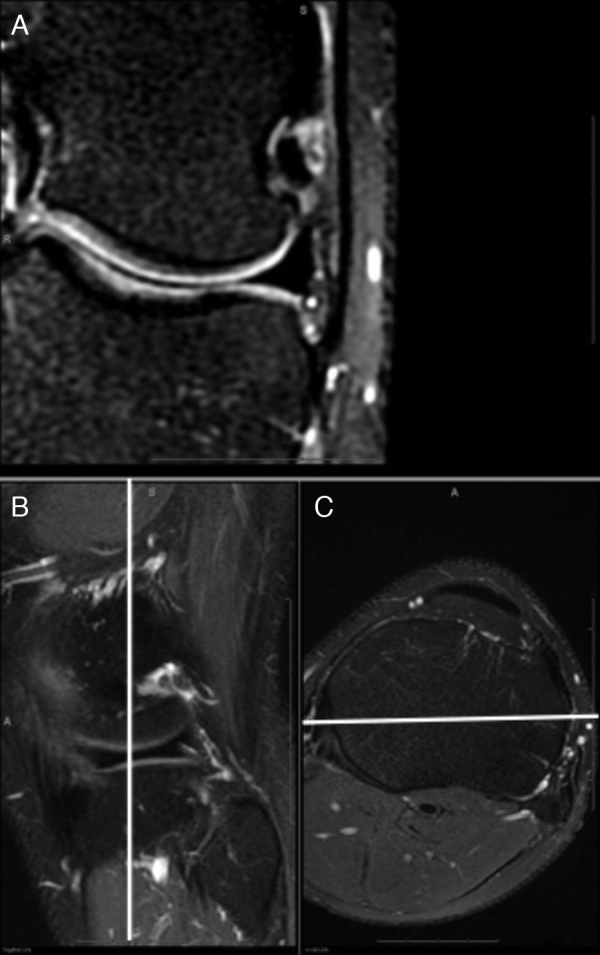
T2-weighted MRI slices with fat saturation: (A) coronal slice showing ALL of the knee; (B) sagittal slice and (C) axial slice showing the topographic location of the ligament based on anatomical parameters.
From analyzing the MRI examinations, it was seen that some portion of the ligament could be clearly viewed in 27 knees (81.8%). In these, the meniscal portion of the ligament was the one most frequently viewed, observed in 25 knees (75.7%). The femoral portion was observed in 23 knees (69.6%) and the tibial portion in 13 (39.3%). The three portions together were viewed in 11 knees (33.3%) (Table 1).
Table 1.
Number of views and percentage viewing of each portion of the ALL of the knee separately and of all of the portions together, in 33 MRI examinations.
| Number of views | Percentage (%) | |
|---|---|---|
| Femoral portion | 23 | 69.6% |
| Meniscal portion | 25 | 75.7% |
| Tibial portion | 13 | 39.3% |
| Any portion of the ligament | 27 | 81.8% |
| Entire ligament | 11 | 33.3% |
In four cases, there was disagreement between the evaluators regarding the presence of the ALL structure: two regarding the femoral portion and two regarding the meniscal portion. In these cases, two auxiliary evaluators made complementary assessments and confirmed its presence.
Discussion
The ALL of the knee has recently been better characterized in anatomical studies.1, 3, 4, 5 Although Vieira et al.2 named this structure, they did not describe any detailed anatomical parameters for it. Its origin in the lateral condyle and its two insertions have been clearly identified in the knees of cadavers.1, 4, 5 Its bifurcation point and meniscal insertion were most clearly demonstrated in the studies by Helito et al.3 and Claes et al.5
This structure may have importance in the genesis of anterolateral instability of the knee. The importance of this joint capsule region in rotational instability has been shown in biomechanical studies, although these did not focus specifically on the ALL.8
Even though these studies suggested that injury to this ligament would increase the anterolateral instability and consequently the grade in the pivot-shift test (which is considered to be the main predictor of functional results following ACL reconstruction), there are still not many studies demonstrating the possibility of viewing this structure through the MRI protocols generally used, i.e. in T2-weighted sequences with fat saturation and T1-weighted sequencers, in the sagittal, coronal and axial planes.6, 9
Our study showed that it was not possible to view the ALL in all the knees when MRI was performed with the abovementioned sequences, especially with regard to viewing all its portions.
We consider that it is important to completely characterize the ALL, i.e. its entire structure in a single examination, so as to make an imaging evaluation of this structure in cases of suspected injury. Furthermore, understanding the limitations on viewing the entire ligament in MRI examinations makes it possible to better determine the predictive value of this test for identifying injuries. Failure to view the ligament can be attributed to injury or simply the limitations of MRI evaluations.
In our study, we were able to view all the portions of the structure in only 33.3% of the cases. At least one portion of the structure was viewed in 81.8% of the examinations. The portion that was viewed most often was the meniscal portion (75.7%), while the tibial portion was viewed least often (39.3%).
The study by Claes et al.7 did not mention the parameters used in MRI or the differentiation between the ligament portions that were evaluated. However, we believe that because of joint tensioning due to hemarthrosis of the ACL injury, its viewing may have been greater.
In a study using three-dimensional MRI, Carpenter showed that knees that had undergone ACL reconstruction presented greater internal rotation in going from extension to flexion than did knees with a native ACL. This situation showed that this reconstruction alone did not fully restore the kinematics of the knee. The greater internal rotation in flexion may have been due to an undiagnosed and untreated ALL injury.10, 11
Because the epicondylar region is the point of origin of the ALL and LCL and the point of insertion of the tendon of the popliteal muscle, it is not always feasible to clearly differentiate the three structures using 1.5-Tesla MRI machines. This makes it difficult to interpret possible injuries in this region. The same is seen in relation to the tibial insertion, at which there may be superposition of the joint capsule or the iliotibial tract. At the site of the meniscal insertion, this superposition does not occur and therefore viewing the insertion of the ALL in this region is easier.
Characterization of this structure is important for future studies, given that ALL injury may be responsible for the portion of the cases that do not evolve satisfactorily after ACL reconstruction.12, 13, 14 Although reconstruction failure in situations without technical errors of tunnel positioning and with grafts of appropriate size are credited as graft failures, we believe that the ALL may have a significant role in these patients.
One limitation of the present study is the fact that the MRI was performed on patients without acute knee trauma and therefore with small volumes of joint fluid. Since larger quantities of fluid inside the joint puts tension on the capsule and makes it easier to view the ALL, better viewing of the ALL might be achieved in examinations on post-trauma cases. For future studies, we suggest that MRI examinations on knees should be performed after injecting fluid in order to put tension on the capsule, or that patients with acute knee trauma should be evaluated. Another limitation to be considered is the 1.5-Tesla MRI machine, which might not be sufficient for clear evaluation of the structure and for enabling differentiation in relation to adjacent structures. Nevertheless, since this machine is the one most used in routine clinical practice in our setting, we consider that it was adequate for use in the present study.
Given that we only had to request evaluations from two complementary evaluators in four cases, we believe that the evaluation bias was very low and did not change the nature of the findings. Because evaluations on this ligament by means of MRI examinations are at an early stage, it is possible that these disagreements in the evaluations might not occur in future studies, because of the greater experience of the evaluators.
Because of the low viewing rate found for the three portions of the ligament in the three acquisition planes, with the weightings generally used in MRI, we believe that it is difficult to establish diagnostic protocols with this type of examination. Further studies need to be conducted using thinner slices, different sequences and machines with bigger magnetic fields (3 T), in an attempt to view this structure with greater clarity. Studies using oblique slices, thinner slices and different weightings are already underway in our clinic, in order to characterize the ligament more definitively and completely.
Conclusion
The ALL of the knee was best viewed in MRI examinations through sequences acquired in the coronal plane. The ligament was completely characterized only in 33.3% of the cases. The meniscal portion was most easily identified and the tibial was found least often in our sample.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Work developed in the Medical Investigation Laboratory for the Musculoskeletal System (LIM41), Department of Orthopedics and Traumatology, School of Medicine, Universidade de São Paulo, São Paulo, SP, Brazil.
References
- 1.Vincent J.P., Magnussen R.A., Gezmez F., Uguen A., Jacobi M., Weppe F. The anterolateral ligament of the human knee: an anatomic and histologic study. Knee Surg Sports Traumatol Arthrosc. 2012;20(1):147–152. doi: 10.1007/s00167-011-1580-3. [DOI] [PubMed] [Google Scholar]
- 2.Vieira E.L., Vieira E.A., da Silva R.T., Berlfein P.A., Abdalla R.J., Cohen M. An anatomic study of the iliotibial tract. Arthroscopy. 2007;23(3):269–274. doi: 10.1016/j.arthro.2006.11.019. [DOI] [PubMed] [Google Scholar]
- 3.Helito C.P., Miyahara H.S., Bonadio M.B., Tirico E.L., Gobbi R.G., Demange M.K. Estudo anatômico do ligamento anterolateral do joelho. Rev Bras Ortop. 2013;48(4):368–373. doi: 10.1016/j.rboe.2013.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Claes S., Vereecke E., Maes M., Victor J., Verdonk P., Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013;223(4):321–328. doi: 10.1111/joa.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Helito C.P., Demange M.K., Bonadio M.B., Tírico L.E., Gobbi R.G., Pécora J.R. Anatomy and histology of the knee anterolateral ligament. Orthop J Sports Med. 2013;1(7):1–5. doi: 10.1177/2325967113513546. Available from: http://ojs.sagepub.com/content/1/7/2325967113513546.abstract?patientinform-links=yes&legid=spojs;1/7/2325967113513546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weber M.A. New aspects on the macroanatomy of anterolateral ligament structures of the knee and the implications for Segond fractures. Radiologe. 2013;53(12):1072–1074. doi: 10.1007/s00117-013-2595-1. [DOI] [PubMed] [Google Scholar]
- 7.Claes S.A., Bartholomeeusen S., Vereecke E.E., Victor M., Verdonk P., Bellemans J. AAOS annual meeting. 2013. The anterolateral ligament of the knee: anatomy, radiology, biomechanics, and clinical implication. Available from: www.abstractonline.com. [Google Scholar]
- 8.Monaco E., Ferretti A., Labianca L., Maestri B., Speranza A., Kelly M.J. Navigated knee kinematics after cutting of the ACL and its secondary restraint. Knee Surg Sports Traumatol Arthrosc. 2012;20(5):870–877. doi: 10.1007/s00167-011-1640-8. [DOI] [PubMed] [Google Scholar]
- 9.Ayeni O.R., Chahal M., Tran M.N., Sprague S. Pivot shift as an outcome measure for ACL reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2012;20(4):767–777. doi: 10.1007/s00167-011-1860-y. [DOI] [PubMed] [Google Scholar]
- 10.Carpenter R.D., Majumdar S., Ma C.B. Magnetic resonance imaging of 3-dimensional in vivo tibiofemoral kinematics in anterior cruciate ligament-reconstructed knees. Arthroscopy. 2009;25(7):760–766. doi: 10.1016/j.arthro.2009.01.014. [DOI] [PubMed] [Google Scholar]
- 11.Logan M., Dunstan E., Robinson J., Williams A., Gedroyc W., Freeman M. Tibiofemoral kinematics of the anterior cruciate ligament (ACL)-deficient weightbearing, living knee employing vertical access open “interventional” multiple resonance imaging. Am J Sports Med. 2004;32(3):720–726. doi: 10.1177/0095399703258771. [DOI] [PubMed] [Google Scholar]
- 12.Hussein M., van Eck C.F., Cretnik A., Dinevski D., Fu F.H. Prospective randomized clinical evaluation of conventional single-bundle, anatomic single-bundle, and anatomic double-bundle anterior cruciate ligament reconstruction: 281 cases with 3- to 5-year follow-up. Am J Sports Med. 2012;40(3):512–520. doi: 10.1177/0363546511426416. [DOI] [PubMed] [Google Scholar]
- 13.Piefer J.W., Pflugner T.R., Hwang M.D., Lubowitz J.H. Anterior cruciate ligament femoral footprint anatomy: systematic review of the 21st century literature. Arthroscopy. 2012;28(6):872–881. doi: 10.1016/j.arthro.2011.11.026. [DOI] [PubMed] [Google Scholar]
- 14.Scheffel P.T., Henninger H.B., Burks R.T. Relationship of the intercondylar roof and the tibial footprint of the ACL: implications for ACL reconstruction. Am J Sports Med. 2013;41(2):396–401. doi: 10.1177/0363546512467955. [DOI] [PubMed] [Google Scholar]