Abstract
Aims:
The aim of the present study was to evaluate the accuracy of Cone Beam Computed Tomography (CBCT) measurements of alveolar bone defects caused due to periodontal disease, by comparing it with actual surgical measurements which is the gold standard.
Materials and Methods:
Hundred periodontal bone defects in fifteen patients suffering from periodontitis and scheduled for flap surgery were included in the study. On the day of surgery prior to anesthesia, CBCT of the quadrant to be operated was taken. After reflection of the flap, clinical measurements of periodontal defect were made using a reamer and digital vernier caliper. The measurements taken during surgery were then compared to the measurements done with CBCT and subjected to statistical analysis using the Pearson's correlation test.
Results:
Overall there was a very high correlation of 0.988 between the surgical and CBCT measurements. In case of type of defects the correlation was higher in horizontal defects as compared to vertical defects.
Conclusions:
CBCT is highly accurate in measurement of periodontal defects and proves to be a very useful tool in periodontal diagnosis and treatment assessment.
Keywords: Bone defects, cone beam computed tomography, intra-oral radiograph, periodontal disease
INTRODUCTION
The importance of assessing the bone condition for the diagnosis, treatment planning and prognosis of periodontal disease is uncontested.
Traditionally intra-oral periapical (IOPA) radiograph are the mainstay to assess the periodontal bone loss, in addition to periodontal probing.[1] Periodontal probing has its own sets of limitation,[1] and so do the IOPA radiographs as they represent the two-dimensional (2D) image of three-dimensional (3D) structure.[2] The advent of digital imaging modality, digital subtraction radiography, and tuned aperture computed tomography (CT) have added considerable improvements to traditional IOPA radiographs, but have their own sets of limitation including that they too represent 2D image of 3D structure.[2]
The introduction of CT has overcome the drawbacks associated with 2D images, however the application of CT imaging for periodontal diagnosis have unfavorable cost-benefit ratio, furthermore CT imaging exposes patient to high radiation dose.[2]
Therefore surgical exposure was the only means to detect accurately the extent and type of bone loss as well as to evaluate bone gain after treatment, and thus surgical exposure was considered to be gold standard.[3] However, evaluation of the type and depth of the defect during surgery gives little time to the surgeon to plan out the type of procedure for periodontal regeneration. Recently cone beam CT (CBCT) has been introduced in dentistry and have proved useful in a wide range of application, especially related to implant site imaging.
The cited advantages of CBCT includes a rapid scan time comparable to panoramic radiograph, less radiation when compared to conventional CT and comparable to full mouth IOPA, image accuracy with resolution ranging from 0.4 mm to as low as 0.076 mm, less cost compared to conventional CT, allows multiplanar reformation and most important advantage of CBCT is that it provides unique 3D images demonstrating features that intraoral, panoramic, and cephalometric images cannot.[4]
Several in-vitro studies have been done to evaluate the accuracy of CBCT in measuring periodontal bone loss.[5,6,7,8] Overall the results of these in-vitro studies indicate that CBCT can accurately provide 3D morphology of periodontal defect and is significantly better than conventional intra-oral radiographs.
Several in-vivo studies have also been done to assess the role of CBCT in periodontics.
Grimard et al.[9] compared direct clinical, periapical radiograph, and CBCT measurement techniques for assessing bone level changes following regenerative periodontal therapy in 35 intrabony defects. Authors found that overall; CBCT was significantly more precise and accurate than periapical radiographs and concluded that CBCT may obviate surgical reentry as a technique for assessing regenerative therapy outcomes.
de Faria Vasconcelos et al.[10] compared periapical radiographs with CBCT imaging in detecting and localizing alveolar bone loss. The authors concluded that CBCT offers improved visualization of the morphology of the defect. The authors had used secondary image database for CBCT comparison and did not compare CBCT measurements with clinical gold standard.
Feijo et al.[11] did an in-vivo study to evaluate the accuracy of CBCT in the detection of horizontal periodontal bone defects. They measured 72 defects in maxillary molar region in patients with periodontitis using CBCT and direct clinical measurement performed during surgical intervention. The authors found that CBCT accurately reproduced the clinical measurement of horizontal periodontal bone defects. However, this study did not evaluate the accuracy of CBCT in vertical defects measurement.
Thus, data from these in-vivo studies have validated the accuracy of CBCT measurements. However, these studies had several inadequacies such as limited sample size, and use of different techniques to do direct clinical measurements. And, therefore, the clinical data on the accuracy of CBCT as periodontal diagnostic aid is still inadequate.
Thus the present study was undertaken to evaluate the accuracy of CBCT for measurement of periodontal defects by comparing linear measurements from CBCT data to actual clinical measurements made during surgical therapy, by using a still larger sample size and standardizing the techniques for direct surgical measurement.
MATERIALS AND METHODS
The present study was approved by the ethical committee board of Government Dental College and Hospital, Mumbai, Maharashtra, India.
The patient selection criteria were as under:
Patient should be above 18 years of age
Patient diagnosed with advanced periodontitis (localized/generalized)
Patient scheduled for flap surgery in at least one quadrant
Patient with known medical conditions, smokers, pregnancy/lactation and those who refused consent were excluded from the study.
After completion of initial nonsurgical periodontal therapy, a written consent was taken from the patients prior to participation in the study. On the scheduled day of periodontal flap surgery prior to anesthesia a high definition CBCT of the quadrant to be operated was taken.
Following aseptic technique, after securing local anesthesia, a full thickness mucoperiosteal flap was raised. Complete scaling and root planning, degranulation was done, and hemostasis was then achieved. Clinical measurements were then made. The surgical site was then irrigated with normal saline and flaps were sutured back. Periodontal pack was given to protect the wound site. Written postoperative instructions were provided to the patient along with antibiotic and analgesics. Sutures were removed 7th postoperative day.
Clinical measurements
Once hemostasis was achieved, the type of defect was first identified. In the case of horizontal defects, the defect depth was measured as distance between the cement enamel junction (CEJ) and the alveolar crest [Figure 1].[5] In the case of vertical defects, the defect depth was measured as distance between the CEJ and the base of the defect [Figure 2].[5,9]
Figure 1.

Measurement of the horizontal bone defect during surgery
Figure 2.

Measurement of the vertical bone defect during surgery
Measurements of the depth of the bone defect were taken for each tooth in the surgical site on the facial aspect. An endodontic reamer was used for measurements. The depth of the defect was measured by holding the reamer parallel to the root surface, the tip of the reamer was placed at the base of the defect and the lower border of the rubber stopper was adjusted to correspond to the CEJ. This distance was then measured using a digital Vernier caliper [Figures 3 and 4] to the accuracy of nearest 0.2 mm. In order to eliminate inter-examiner discrepancies the same investigator performed all measurements in all patients.
Figure 3.
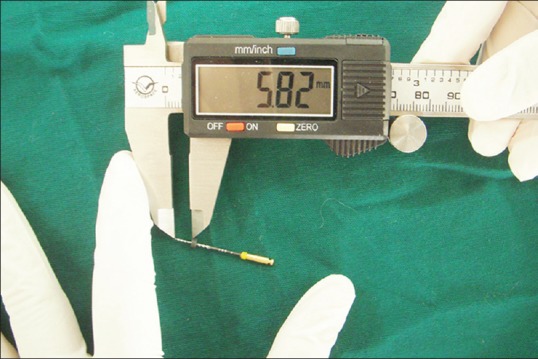
Digital Vernier caliper measurement of horizontal defect with accuracy of 0.2 mm
Figure 4.

Digital Vernier caliper measurement of vertical defect with accuracy of 0.2 mm
Cone beam computed tomography measurements
Cone beam CT data was collected prior to surgery on Planmeca Promax 3D machine. The data was acquired with an image size of 400 × 400 × 400, voltage of 90 kv, voxel size-400 μm, current-10 mA, and exposure time-13 s. The examiner underwent training for performing the measurements. The examiner was unaware of the name of the patient or the clinical measurements made during surgery, to avoid any bias. The CBCT measurements followed the same pattern as clinical measurements. First the type of defect was identified. Then in case of horizontal defects, distance between CEJ to alveolar crest was measured [Figure 5] and in case of vertical defects the distance between CEJ and the base of the defect was measured [Figure 6]. The measurements were done with the help of Planmeca Romexis (Planmeca USA, Inc.,) viewer software to the accuracy of 0.2 mm.
Figure 5.
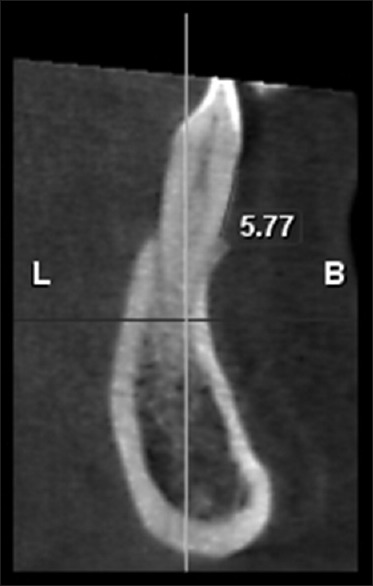
Measurement of the horizontal bone defect on cone beam computed tomography
Figure 6.

Measurement of the vertical bone defect on cone beam computed tomography
A total of 100 periodontal bone defects in 15 patients planned for surgical open flap debridement were thus measured clinically during surgery and by CBCT. Figures 1, 3 and 5 show measurement of horizontal bone defect and Figures 2, 4 and 6 show measurement of vertical bone defect.
The data collected were subjected to statistical analysis. The Pearson's correlation test was used to correlate the measurements done clinically and by CBCT.
RESULTS
The overall mean clinical and CBCT measurements were 3.8052 mm and 3.8139 mm respectively with a standard deviation of 1.66 [Table 1]. The comparison between the two measurements showed a very high correlation of 0.988, which was significant at the 0.01 level (two-tailed) [Table 2].
Table 1.
Mean and SD values for horizontal defect, vertical defect and horizontal and vertical defects combined
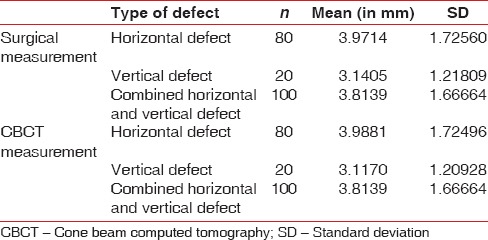
Table 2.
Correlation between surgical measurement and CBCT measurements in horizontal defect, vertical defects and horizontal and vertical defects combined
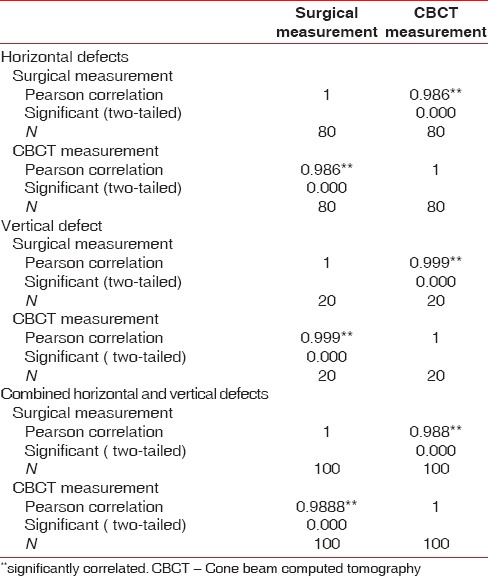
Of the 100 defects, 80 were horizontal defects and 20 vertical defects and CBCT was 100% accurate in identifying the type of defect in all the patients. The mean clinical and CBCT measurements in case of horizontal defects were 3.9714 mm and 3.9881 mm, respectively [Table 1]. In the case of vertical defects the mean clinical and CBCT measurements were 3.1405 mm and 3.1170 mm, respectively [Table 1]. The correlation between the measurements for horizontal defects was 0.986, which was significant at the 0.01 level (two-tailed) [Table 2]. Similarly, the measurements in vertical defects showed a high correlation of 0.999, which was significant at the 0.01 level (two-tailed) [Table 2].
When the correlation between the horizontal and vertical defects was compared the horizontal defect correlation was higher than the vertical defects. However, this difference was very small.
DISCUSSION
The introduction of CBCT in dentistry has opened a new vista in maxillofacial imaging. CBCT has facilitated the transition of dental diagnosis from 2D to 3D images and has potential to expand the role of dental imaging from mere diagnosis to image guidance of operative and surgical procedures.[4]
Several studies have been done to evaluate the accuracy of CBCT imaging, and the recent review of these studies has positively affirmed that CBCT is superior to conventional dental imaging modalities.[12] The reviewers also noted that this data are based on limited in-vitro and in-vivo research and stressed the need for more clinical studies.[12]
This study was undertaken to evaluate the accuracy of CBCT for measurement of periodontal defects by comparing linear measurements from CBCT data to actual gold standard clinical measurements made during surgical therapy.
A total of 100 defects were evaluated in 15 patients. The results from our study indicate that CBCT is highly accurate for diagnosing both horizontal and vertical bone defect. Furthermore, there is a high degree of correlation between clinical and CBCT measurements of bone defects.
These results are consistent with the results of all the previous in-vivo studies Grimard et al.,[9] de Faria Vasconcelos et al.,[10] and Feijo et al.[11] This study is one of the few studies that have evaluated and compared CBCT measurements of periodontal defects with actual surgical measurements in vivo.[9,11]
In comparing the individual types of defect, there was high correlation between clinical and CBCT measurements of both horizontal and vertical bone defects, which is again consistent with previous such study by Grimard et al.[9]
The correlation in the case of horizontal defects was higher as compared to vertical defects although this difference was not significant. This could be explained by the fact that the in case of horizontal defect the distance was measured from CEJ to alveolar crest and the crest is corticated bone, which gave a more demarcated line on the CBCT, whereas in case of vertical defects the base of the defect is cancellous thus decreasing the sensitivity of demarcation on the CBCT.
One of the highlights of this study was that the actual clinical measurements were done using an endodontic reamer to record the distance between the CEJ and alveolar crest/base of defect and this recording was then measured with a digital Vernier caliper with an accuracy of up to 0.2 mm which is comparable to the accuracy of CBCT measurement. To the best knowledge of the authors, this was the first of its kind novel method used to accurately obtain clinical measurements, unlike the previous in vivo studies that used a periodontal probe with 1 mm markings for measurement of the defects clinically.[9,11]
However, few areas need to be addressed. In this study, the defects were recorded only on the facial aspect as it was difficult to keep the reamer parallel to the root surface in the mesial and distal side unless there is was a diastema between teeth. This problem can be overcome by the use of advanced probing systems.
Clinical relevance
Given the high accuracy of CBCT in detection of periodontal bone defects as found in the present study along with its various advantages such as low radiation, rapidity of scan time, and relatively low cost of CBCT, its use is highly desirable in periodontal practice especially for advanced periodontal disease to more accurately diagnose periodontal disease and its aspects such as amount of bone loss, involvement of furcation, type of defects and their dimension, determine accurately the prognosis of each tooth by allowing 3D analysis of bone around them, and plan for the type of periodontal intervention procedure especially related to regeneration. Also, CBCT may alleviate the need for surgical re-entry to assess bone formation. All these aspect will eventually contribute to significantly improve the quality of periodontal care and thus to improved outcome. Therefore, it may not be farfetched to speculate that in near future CBCT may replace the traditional panoramic radiographs and full mouth IOPA for periodontal diagnosis and treatment planning.
CONCLUSION
This study shows that CBCT is highly accurate in identifying and quantifying periodontal bone loss for both horizontal and vertical defect and thus can be an excellent diagnostic aid for periodontal treatment planning as well as re-evaluation.
Footnotes
Source of Support: Government Dental College and Hospital, Mumbai, Maharashtra, India
Conflict of Interest: None declared.
REFERENCES
- 1.Zybutz M, Rapoport D, Laurell L, Persson GR. Comparisons of clinical and radiographic measurements of inter-proximal vertical defects before and 1 year after surgical treatments. J Clin Periodontol. 2000;27:179–86. doi: 10.1034/j.1600-051x.2000.027003179.x. [DOI] [PubMed] [Google Scholar]
- 2.Mol A. Imaging methods in periodontology. Periodontol 2000. 2004;34:34–48. doi: 10.1046/j.0906-6713.2003.003423.x. [DOI] [PubMed] [Google Scholar]
- 3.Ito K, Yoshinuma N, Goke E, Arai Y, Shinoda K. Clinical application of a new compact computed tomography system for evaluating the outcome of regenerative therapy: A case report. J Periodontol. 2001;72:696–702. doi: 10.1902/jop.2001.72.5.696. [DOI] [PubMed] [Google Scholar]
- 4.Scarfe WC, Farman AG. What is cone-beam CT and how does it work? Dent Clin North Am. 2008;52:707–30. doi: 10.1016/j.cden.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 5.Misch KA, Yi ES, Sarment DP. Accuracy of cone beam computed tomography for periodontal defect measurements. J Periodontol. 2006;77:1261–6. doi: 10.1902/jop.2006.050367. [DOI] [PubMed] [Google Scholar]
- 6.Vandenberghe B, Jacobs R, Yang J. Detection of periodontal bone loss using digital intraoral and cone beam computed tomography images: An in vitro assessment of bony and/or infrabony defects. Dentomaxillofac Radiol. 2008;37:252–60. doi: 10.1259/dmfr/57711133. [DOI] [PubMed] [Google Scholar]
- 7.Mol A, Balasundaram A. In vitro cone beam computed tomography imaging of periodontal bone. Dentomaxillofac Radiol. 2008;37:319–24. doi: 10.1259/dmfr/26475758. [DOI] [PubMed] [Google Scholar]
- 8.Noujeim M, Prihoda T, Langlais R, Nummikoski P. Evaluation of high-resolution cone beam computed tomography in the detection of simulated interradicular bone lesions. Dentomaxillofac Radiol. 2009;38:156–62. doi: 10.1259/dmfr/61676894. [DOI] [PubMed] [Google Scholar]
- 9.Grimard BA, Hoidal MJ, Mills MP, Mellonig JT, Nummikoski PV, Mealey BL. Comparison of clinical, periapical radiograph, and cone-beam volume tomography measurement techniques for assessing bone level changes following regenerative periodontal therapy. J Periodontol. 2009;80:48–55. doi: 10.1902/jop.2009.080289. [DOI] [PubMed] [Google Scholar]
- 10.de Faria Vasconcelos K, Evangelista KM, Rodrigues CD, Estrela C, de Sousa TO, Silva MA. Detection of periodontal bone loss using cone beam CT and intraoral radiography. Dentomaxillofac Radiol. 2012;41:64–9. doi: 10.1259/dmfr/13676777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Feijo CV, Lucena JG, Kurita LM, Pereira SL. Evaluation of cone beam computed tomography in the detection of horizontal periodontal bone defects: An in vivo study. Int J Periodontics Restorative Dent. 2012;32:e162–8. [PubMed] [Google Scholar]
- 12.Tyndall DA, Rathore S. Cone-beam CT diagnostic applications: Caries, periodontal bone assessment, and endodontic applications. Dent Clin North Am. 2008;52:825–41. doi: 10.1016/j.cden.2008.05.002. vii. [DOI] [PubMed] [Google Scholar]


