Abstract
Hereditary gingival fibromatosis (HGF) is a rare hereditary condition characterized by slow, progressive, nonhemorrhagic, fibrous enlargement of gingiva due to increase in sub-mucosal connective tissue component. This paper presents a case report of an 18-year-old female suffering from HGF with positive family history. Her 42-year-old mother also have enlargement of the gums. After through clinical examination of both the patients, routine blood investigation was advised. All the investigations were within normal physiological limits of both the patients. Surgical excision of enlarged gingival tissue was planned after meticulous scaling and root planing. Patients were recalled 1 week after surgery. Postoperative healing were good and desired crown lengthening was achieved with significant improvement in speech and masticatory problems in both the patients. There was no recurrence of the disease even after 2 years follow-up.
Keywords: Crown lengthening, gingival hyperplasia, internal bevel gingivectomy
INTRODUCTION
Gingival hyperplasia (synonymous as gingival overgrowth, gingival fibromatosis) may occur as a side effect to systemic medications, including phenytoin, cyclosporine, and nifedipine[1] and some time it may be due to genetic origin, known as hereditary gingival fibromatosis (HGF), which is an uncommon condition characterized by diffuse gingival enlargement, sometimes covered major parts of the gingiva or involved the total gingiva.[2] HGF first reported by Goddard and Gross in 1856,[3] the mode of inheritance is believed to be autosomal dominant[4] although some cases of a recessive mode of inheritance have been also reported.[5]
Gingival fibromatosis also associated with syndrome chromosomal anomalies occurred 2p13-16, 4q, 8, 14q, 19p, 19q and Xq.[6] The primary etiological factors of gingival fibromatosis which are not associated with syndrome are Son-of-Sevenless homolog 1 has been identified recently, which are guanine nucleotide-exchange factor which play important role in transduction of signals that controls cell growth and differentiation.[7]
Hereditary gingival fibromatosis presents firm, dense, resilient, insensitive fibrous tissue that covers the alveolar ridges and extend over the teeth, resulting in extensive pseudo pockets. The color may be normal or erythematous if inflamed.
Histological features of HGF is characterized by densely arranged collagen bundles, numerous fibroblasts, and connective tissue that is avascular along with well-structured epithelium with elongated and thin papillae inserted in fibrous connective tissue.[8]
CASE REPORT
In this case, a 18-year-old female reported with her mother and complain of swollen gums and progressive gingival enlargement since last 7 years [Figures 1 and 2]. The enlargement had led to poor esthetics and masticatory problems. Intra oral examination revealed generalized fibrotic enlargement of gingiva in the upper arch. Generalized pseudo pocket were observed with no bleeding on probing. The patient had not given any positive drug history. His current health condition and mental state were considered normal. During the evaluation of his family history, the patient mother aged 42 years also reported the similar intra oral lesions in the form of generalized gingival enlargement, affected the lower arch since last 10–15 years with extensive mobility of teeth. Generalized periodontal pocket were observed with no bleeding on probing. She has not given any positive drugs history and current health condition and mental state was normal. Biopsy samples from both the patients were taken and send for histopathological examination. Based on the histopathological findings [Figure 3] and positive family history, the diagnosis of “HGF” was made.
Figure 1.

Preoperative photograph of daughter
Figure 2.

Preoperative photograph of mother
Figure 3.
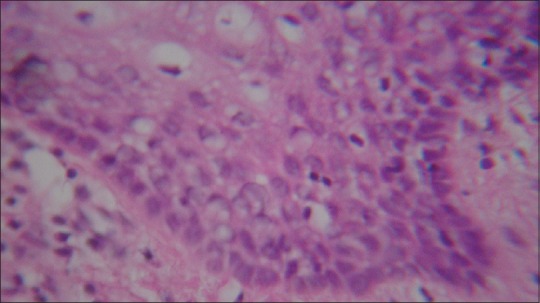
Histopathological photographs of daughter and mother showed densely arranged collagen bundles, numerous fibroblasts, and connective tissue
Considering the severity of the enlargement, a quadrant-by-quadrant internal bevel gingivectomy in daughter and internal bevel gingivectomy plus full thickness mucoperiosteal flap surgery in her mother were performed.
Postoperative healing was satisfactory and desired crown lengthening was achieved. Patient's esthetic and masticatory problems were completely resolved with gain of adequate functional ability. Esthetics was significantly improved in terms of gingival appearance after surgical excision of enlarged gingival tissue. Patient was put in the follow-up program at 1, 3, 6 months interval followed by [Figures 4 and 5] after 1 and 2 years. After 2 years follow-up, oral examination showed that patient's oral hygiene were good with minimal plaque, normal probing pocket depth and no recurrence of the lesion. These conditions were achieved by a combination of monthly examination with professional cleaning and follow the given oral hygiene instructions [Figures 6 and 7].
Figure 4.

One year postoperative follow-up of daughter right side
Figure 5.

One year postoperative follow-up of daughter left side
Figure 6.

Two years postoperative follow-up of daughter
Figure 7.

Two years postoperative follow-up of mother
DISCUSSION
Syndromes that have been occasionally associated with HGF are Zimmerman–Laband syndrome (defects of bone, ear, nail and nose, accompanied by hepatosplenomegaly), Murray–Puretic–Drescher syndrome (multiple dental hyaline tumors), Rutherfurd syndrome (corneal dystrophy), Cowden syndrome (multiple hamartomas) and Cross syndrome (hypopigmentation with athetosis).[9] In this case, a thorough evaluation of the patient, revealed no association with any of the clinical features associated with the above syndromes.
The present case reported as HGF. HGF is transmitted as either autosomal dominant or recessive. This case is diagnosed as gingival fibromatosis due to hereditary and autosomal dominant with occurrence of enlargement in successive generation from mother to daughter and support with other evidence by the same characteristic histopathological findings in both mother and daughter.
Various types of treatment modalities have been employed for the excision of the enlarged gingival tissues, including of conventional surgery, electro surgery, an apically positioned flap and lasers.[10]
In present case, surgery was performed quadrant-by-quadrant internal bevel gingivectomy in daughter because only marginal bone loss present in this patient and her mother internal bevel gingivectomy plus full thickness mucoperiosteal flap was performed due presence of a thick bulk of gingival tissue along with alveolar bone loss.
A periodontal flap procedure also can prefer for the treatment of gingival enlargement if there are large areas of gingival overgrowth or attachment loss and osseous defects.
After surgery, they improve the physiologic contour of marginal gingiva that play an important role in the maintenance of good oral hygiene and prevent the recurrence.[11] Reports about recurrence rates are contradictory[12] so the postoperative long-term benefit of periodontal surgery cannot be predicted. Normally recurrence is minimal or delayed if good oral hygiene is achieved by a combination of monthly examinations or delayed if good oral hygiene is achieved by a combination of monthly examination with professional cleaning and oral hygiene instructions.[11]
Some reports in severe cases of HGF, full-mouth tooth clearance has been advocated, and they suggest that the condition does not recur if the teeth have been extracted.[12]
Because in the dentulous areas of the mouth as patient failed to maintain good oral hygiene.[12] In our case report, there was no recurrence of the disease even after 2 years follow-up.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Coletta RD, Graner E. Hereditary gingival fibromatosis: A systematic review. J Periodontol. 2006;77:753–64. doi: 10.1902/jop.2006.050379. [DOI] [PubMed] [Google Scholar]
- 2.Babu KB, Kumar KP, Anuradha BR, Arora N. Hereditary gingival fibromatosis – A case report and management using a novel surgical technique. RSBO. 2011;8:453–8. [Google Scholar]
- 3.Goddard WH, Gross SD. Case of hypertrophy of the gums. Dent Regist West. 1856;9:276–82. [PMC free article] [PubMed] [Google Scholar]
- 4.Bozzo L, de Almedia OP, Scully C, Aldred MJ. Hereditary gingival fibromatosis. Report of an extensive four-generation pedigree. Oral Surg Oral Med Oral Pathol. 1994;78:452–4. doi: 10.1016/0030-4220(94)90037-x. [DOI] [PubMed] [Google Scholar]
- 5.Jorgenson RJ, Cocker EM. Variation in the inheritance and expression of gingival fibromatosis. J Periodontol. 1974;45:472–7. doi: 10.1902/jop.1974.45.7.472. [DOI] [PubMed] [Google Scholar]
- 6.Hart TC, Zhang Y, Gorry MC, Hart PS, Cooper M, Marazita ML, et al. A mutation in the SOS1 gene causes hereditary gingival fibromatosis type 1. Am J Hum Genet. 2002;70:943–54. doi: 10.1086/339689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee EJ, Jang SI, Pallos D, Kather J, Hart TC. Characterization of fibroblasts with Son of Sevenless-1 mutation. J Dent Res. 2006;85:1050–5. doi: 10.1177/154405910608501115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Collan Y, Ranta H, Vartio T, Perheentupa J, Raeste AM. Histochemical and biochemical study of hereditary fibrous hyperplasia of the gingiva. Scand J Dent Res. 1982;90:20–8. doi: 10.1111/j.1600-0722.1982.tb01520.x. [DOI] [PubMed] [Google Scholar]
- 9.Gorlin RJ, Pinborg JJ, Cohen MM., Jr . 2nd ed. New York: McGraw-Hill; 1976. Syndromes of the Head and Neck; pp. 329–36. [Google Scholar]
- 10.Danesh-Meyer MJ, Holborow DW. Familial gingival fibromatosis: A report of two patients. N Z Dent J. 1993;89:119–22. [PubMed] [Google Scholar]
- 11.Nagarale GP, Ravindra S, Thakur S, Setty S. Long term follow up of idiopathic gingival enlargement associated with chronic periodontitis: A case report and review. J Indian Soc Periodontol. 2013;17:242–7. doi: 10.4103/0972-124X.113088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kharbanda P, Sidhu SS, Panda SK, Deshmukh R. Gingival fibromatosis: Study of three generations with consanguinity. Quintessence Int. 1993;24:161–4. [PubMed] [Google Scholar]


