Abstract
Medicare reimbursement policy encourages frequent provider visits for patients with ESRD undergoing hemodialysis. We hypothesize that patients seen more frequently by their nephrologist or advanced practitioner within the first 90 days of hemodialysis are more likely to undergo surgery to create an arteriovenous (AV) fistula or place an AV graft. We selected 35,959 patients aged ≥67 years starting hemodialysis in the United States from a national registry. We used multivariable regression to evaluate the associations between mean visit frequency and AV fistula creation or graft placement in the first 90 days of hemodialysis. We conducted an instrumental variable analysis to test the sensitivity of our findings to potential bias from unobserved characteristics. One additional visit per month in the first 90 days of hemodialysis was associated with a 21% increase in the odds of AV fistula creation or graft placement during that period (95% confidence interval, 19% to 24%), corresponding to an average 4.5% increase in absolute probability. An instrumental variable analysis demonstrated similar findings. Excluding visits in months when patients were hospitalized, one additional visit per month was associated with a 10% increase in odds of vascular access surgery (95% confidence interval, 8% to 13%). In conclusion, patients seen more frequently by care providers in the first 90 days of hemodialysis undergo earlier AV fistula creation or graft placement. Payment policies that encourage more frequent visits to patients at key clinical time points may yield more favorable health outcomes than policies that operate irrespective of patients’ health status.
Keywords: chronic hemodialysis, economic analysis, ESRD, outcomes, vascular access, epidemiology
More than 400,000 patients suffer with ESRD in the United States and the large majority receive in-center hemodialysis. Patients receiving hemodialysis suffer from high morbidity and mortality; the annual mortality rate for patients on hemodialysis was 20% per year in 2011.1 Patients can receive hemodialysis through a large-bore central venous catheter or an arteriovenous (AV) fistula or graft. Many studies demonstrate that hemodialysis through an AV fistula or graft is associated with prolonged survival and fewer hospitalizations compared with hemodialysis through a central venous catheter.2–7 Hemodialysis through an AV fistula or graft may also be associated with improved quality of life.8
Whether patients receive hemodialysis through a central venous catheter or an AV fistula or graft depends on patient health, the healthcare system, and access to care. Creation of an AV fistula or placement of an AV graft requires that a patient is healthy enough to undergo surgery and has vasculature that can support high blood flow rates through the fistula or graft. Health conditions such as cardiovascular disease, lower serum albumin, and older age have been associated with increased likelihood of hemodialysis with a catheter.9–12 At the same time, patients must have access to a healthcare provider who can refer them to a vascular surgeon (as well as access to a vascular surgeon). Seeing a nephrologist in advance of requiring dialysis is associated with increased likelihood of starting hemodialysis with a fistula or graft.12–16 Recognizing the role that healthcare providers have in promoting AV fistula and graft use, the US Centers for Medicare and Medicaid Services (CMS) has begun to report the proportion of patients at a dialysis facility receiving hemodialysis through a permanent vascular (noncatheter) access as a key measure of dialysis facility quality.17
In 2004, the CMS enacted a tiered fee-for-service reimbursement policy for nephrologist visits that promotes more frequent face-to-face visits to patients receiving hemodialysis.18 Despite a common financial incentive to see patients frequently, variation in visit frequency continues to exist among providers.19 In this study, we examine whether patients seen more frequently by their nephrologist or advanced practitioner in the first 90 days of hemodialysis were more likely to undergo surgery to create an AV fistula or place an AV graft during that period.
Results
Baseline Characteristics
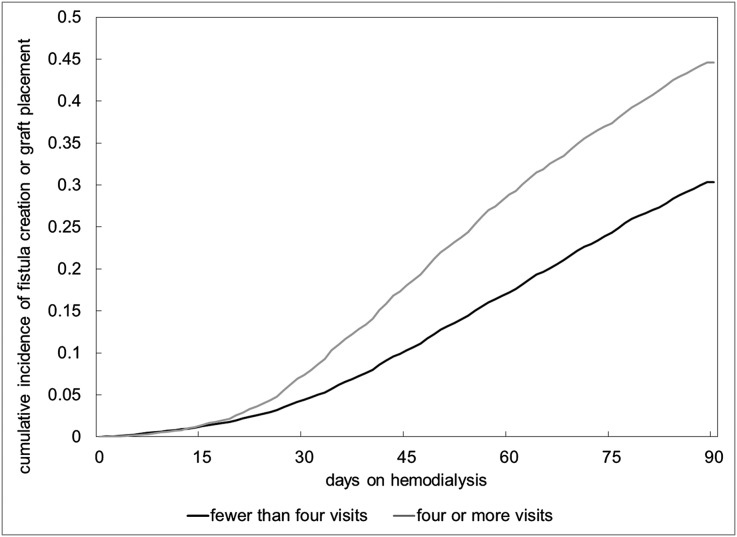
There were 35,959 patients included in this study (Supplemental Figure 1). In the first 90 days of hemodialysis, 36% of patients who started dialysis with a central venous tunneled catheter underwent surgery to create an AV fistula or place an AV graft. The average number of physician or advanced practitioner visits in the first 3 months of hemodialysis was 2.8 (SD 1.3). In total, 41% of patients received four visits per month in all months, 17% received an average of three to four visits per month, 21% received an average of two to three visits, 12% received an average of one to two visits, and 10% received an average of fewer than one visit per month. After censoring for death, the probability of fistula or graft placement among patients seen fewer than four times per month at 30, 60, and 90 days was 4.4%, 17.2%, and 30.3%, respectively. Among patients seen four or more times per month the probability of fistula or graft placement at 30, 60, and 90 days was 7.4%, 28.9%, and 44.6%, respectively (Figure 1).
Figure 1.
Cumulative incidence of fistula creation or graft placement stratified by visit frequency. Statistical analyses were based on the Kaplan–Meier method. The P value of the log-rank test for equality of survivor functions is <0.001.
When comparing patients seen four times each month with those seen fewer than four times in univariate analyses, there were no significant differences in demographic or socioeconomic characteristics. Patients seen fewer than four times per month, however, were more likely to be immobile, had a slightly lower serum albumin upon starting dialysis, and spent more days in the hospital before and in the first 90 days of hemodialysis. In addition, patients seen fewer than four times per month received less nephrologist care before hemodialysis and were more likely to dialyze at smaller facilities. Older patients and women were less likely to undergo vascular access surgery in the first 90 days of hemodialysis. Patients with heart failure, immobility, lower serum albumin, and more days spent in the hospital before and during the first 90 days of hemodialysis were also less likely to undergo vascular access surgery. Men, patients with more nephrologist care before hemodialysis, and those who received more nephrologist or advanced practitioner visits per month after hemodialysis initiation were more likely to have an AV fistula created or graft placed (Table 1).
Table 1.
Baseline characteristics
| Characteristic | Visits | Access Placed | ||||
|---|---|---|---|---|---|---|
| <4 (n=21,252) | 4 (n=14,484) | Standard Difference | No Access (n=23,043) | Permanent Access (n=12,693) | Standard Difference | |
| Demographic and socioeconomic | ||||||
| Age, yr | 77.4 | 77.6 | 1.9a | 77.9 | 76.8 | 16.2a |
| Men | 49.7 | 51.1 | 2.7a | 48.3 | 53.9 | 11.0a |
| American Indian | 0.9 | 0.7 | 2.5a | 0.8 | 0.7 | 1.2 |
| Black | 18.5 | 19.0 | 1.3 | 18.4 | 19.3 | 2.3a |
| White | 78.2 | 77.7 | 1.1 | 78.3 | 77.4 | 2.2a |
| Other race | 2.4 | 2.6 | 1.0 | 2.4 | 2.6 | 0.8 |
| Hispanic ethnicity | 7.0 | 7.1 | 0.2 | 6.9 | 7.3 | 1.5 |
| Medicaid coverage | 20.9 | 19.5 | 3.6a | 20.9 | 19.3 | 4.0a |
| Comorbidities | ||||||
| Diabetes | 48.9 | 49.2 | 0.6 | 47.8 | 51.2 | 6.7a |
| Coronary disease | 51.6 | 49.7 | 3.8a | 51.9 | 48.9 | 6.2a |
| Cancer | 23.6 | 22.9 | 1.8 | 24.1 | 21.9 | 5.3a |
| Heart failure | 78.0 | 75.1 | 7.1a | 78.5 | 73.9 | 11.3a |
| Pulmonary disease | 48.9 | 44.6 | 8.8a | 48.4 | 44.8 | 7.4a |
| Cerebrovascular disease | 28.7 | 26.4 | 5.1a | 28.9 | 25.6 | 7.4a |
| Peripheral vascular disease | 39.7 | 37.3 | 5.1a | 39.8 | 36.9 | 6.0a |
| Smoking history | 7.4 | 6.9 | 2.0 | 7.1 | 7.4 | 1.3 |
| Immobility | 14.7 | 10.2 | 14.0a | 15.3 | 8.4 | 21.8a |
| Hemoglobin, g/dl | 10.0 | 10.1 | 4.5a | 10.0 | 10.1 | 3.2a |
| Albumin, g/dl | 3.0 | 3.1 | 14.7a | 3.0 | 3.1 | 20.6a |
| Body mass index, kg/m2 | 27.4 | 27.3 | 0.3a | 27.1 | 27.8 | 8.8a |
| Drug or alcohol use | 0.8 | 0.7 | 0.8 | 0.8 | 0.6 | 2.1 |
| Prior nephrologist care, d | 1.9 | 2.4 | 15.5a | 1.9 | 2.5 | 19.9a |
| Hospital days in first 90 d of dialysis | 5.0 | 1.0 | 80.5a | 4.1 | 2.0 | 39.2a |
| Hospital days in 90 d before dialysis | 12.0 | 9.4 | 20.2a | 12.4 | 8.3 | 32.8a |
| Geographic and facility | ||||||
| Metropolitan | 76.1 | 78.5 | 5.7a | 77.8 | 75.6 | 5.4a |
| For-profit facility | 79.3 | 78.4 | 2.2a | 77.9 | 80.7 | 6.5a |
| Hospital-based facility | 13.0 | 14.5 | 4.3a | 14.4 | 12.1 | 6.7a |
| Facility size, no. of patients | 83.2 | 89.8 | 11.9a | 86.5 | 84.8 | 3.0a |
| Visits per month, n | 2.0 | 4.0 | 2.7 | 3.1 | 28.2a | |
Data are presented as percentages unless otherwise indicated.
P value <0.05, comparing groups.
Visit Frequency and Vascular Access Surgery
In a multivariable logistic regression analysis, one additional nephrologist or advanced practitioner visit per month in the first 90 days of hemodialysis was independently associated with a 21% increase in the odds of receiving an AV fistula or graft (95% confidence interval [95% CI], 19% to 24%) (Table 2). The mean predicted probability of vascular access surgery was 28%, 32%, 36%, and 40% if patients were seen an average of one, two, three, or four times per month, respectively, corresponding to an average difference in the absolute probability of undergoing vascular access surgery within the first 90 days of 4.5% per additional increase in average monthly visits.
Table 2.
Logistic regression of the association between visit frequency and AV fistula creation or AV graft placement
| Characteristic | OR (95% CI) | P Value |
|---|---|---|
| One additional visit per month | 1.21 (1.19 to 1.24) | <0.001 |
| Demographic and socioeconomic | ||
| Male sex | 1.26 (1.21 to 1.32) | <0.001 |
| Age, 10 yr | 0.81 (0.78 to 0.84) | <0.001 |
| Race (white as referent) | 0.03a | |
| American Indian | 0.89 (0.69 to 1.15) | |
| Black | 1.09 (1.02 to 1.15) | |
| Other race including Asian | 1.11 (0.95 to 1.28) | |
| Ethnicity (non-Hispanic as referent) | ||
| Hispanic ethnicity | 1.07 (0.97 to 1.17) | 0.16 |
| Medicaid coverage | 0.94 (0.88 to 1.00) | 0.05 |
| Comorbidities | ||
| Diabetes | 1.10 (1.05 to 1.16) | <0.001 |
| Coronary disease | 0.96 (0.91 to 1.01) | 0.08 |
| Cancer | 0.89 (0.84 to 0.94) | <0.001 |
| Heart failure | 0.94 (0.88 to 0.99) | 0.03 |
| Pulmonary disease | 1.00 (0.95 to 1.05) | 0.95 |
| Cerebrovascular disease | 0.98 (0.93 to 1.03) | 0.45 |
| Peripheral vascular disease | 0.98 (0.93 to 1.03) | 0.44 |
| Smoking history | 1.03 (0.94 to 1.13) | 0.51 |
| Immobility | 0.64 (0.59 to 0.69) | <0.001 |
| Drug or alcohol use | 0.77 (0.59 to 1.01) | 0.06 |
| Predialysis care | ||
| Outpatient nephrology visits in 90 d before dialysis (0 visits is referent) | ||
| 1 | 1.28 (1.19 to 1.39) | <0.001 |
| 2–3 | 1.45 (1.36 to 1.54) | <0.001 |
| ≥4 | 1.52 (1.44 to 1.61) | <0.001 |
| Days in hospital in 90 d before dialysis (0 d is referent) | ||
| 1–4 | 0.88 (0.82 to 0.95) | <0.001 |
| 5–10 | 0.78 (0.72 to 0.84) | <0.001 |
| >10 | 0.59 (0.54 to 0.64 | <0.001 |
| Geographic and facility (metropolitan as referent) | ||
| Metropolitan | 0.91 (0.87 to 0.97) | <0.001 |
| For-profit facility | 1.08 (0.99 to 1.17) | 0.07 |
| Hospital-based facility | 0.92 (0.84 to 1.02) | 0.12 |
| Facility size (25 patients) | 0.98 (0.97 to 0.99) | <0.001 |
P value testing the joint significance of race variables (note, adjusted for calendar year).
The relation between visit frequency and vascular access surgery did not depend on patient age or days spent in the hospital before dialysis. In an analysis in which we divided visit frequency in months when patients were not hospitalized into discrete categories, the association between each incremental change in visit frequency and the odds of receiving an AV fistula or graft persisted as visits increased. Compared with patients seen fewer than two times per month, two to three visits per month was associated with a 21% increase in the odds of receiving an AV fistula or graft (odds ratio [OR], 1.21; 95% CI, 1.10 to 1.33); more than three visits per month was associated with a 32% increase in the odds of receiving an AV fistula or graft (95% CI, 21% to 44%).
In a sensitivity analysis in which we excluded visits in months when patients were in the hospital, the association between more visits and vascular access surgery was less pronounced but still substantial (OR, 1.10; 95% CI, 1.08 to 1.13). In an additional sensitivity analysis in which we estimated the odds of vascular access surgery in the second full month of hemodialysis as a function of visit frequency in the prior month (adjusting for hospital days in the prior month in addition to the covariates from Table 2), one additional visit was associated with a 6.4% increase in the odds of vascular access surgery in the subsequent month (95% CI, 3.5% to 9.3%).
Instrumental Variable Analyses
We used an instrumental variable analysis to assess the sensitivity of our findings to potential bias from unobserved confounding characteristics. The F-statistic testing the association between the instrumental variable (mean visit frequency per year among prevalent hemodialysis patients at a patient’s facility) and the exposure (visit frequency in the first 90 days of hemodialysis) was 226, demonstrating that this was a strong instrument. An examination of observable baseline characteristics stratified by within-facility quartiles of the instrumental variable demonstrates no significant differences in baseline characteristics between the first and fourth quartiles of the instrumental variable. These findings suggest that patients do not differ substantially across levels of the instrument (Table 3).
Table 3.
Baseline characteristics stratified by visit frequency and level of the instrumental variable
| Characteristic | Quartile of Actual Visits | Rank of Mean Facility Visits | |||||||
|---|---|---|---|---|---|---|---|---|---|
| First | Second | Third and Fourth | Standard Difference | Lowest | Second | Third | Highest | Standard Difference | |
| Demographic | |||||||||
| Men | 50.0 | 49.5 | 51.1 | 2.2 | 50.1 | 51.0 | 49.2 | 50.2 | 0.2 |
| Age, yr | 77.4 | 77.4 | 77.6 | 1.8 | 77.5 | 77.4 | 77.4 | 77.5 | 0.0 |
| Native American | 1.0 | 0.7 | 0.7 | 4.1 | 0.9 | 1.0 | 1.1 | 0.9 | 0.0 |
| Black | 18.3 | 18.8 | 19.0 | 2.0 | 18.9 | 19.0 | 19.1 | 18.9 | 0.0 |
| White | 78.2 | 78.1 | 77.7 | 1.2 | 77.4 | 77.6 | 78.6 | 78.2 | 1.8 |
| Other race | 2.5 | 2.4 | 2.6 | 0.6 | 2.7 | 2.7 | 1.6 | 2.3 | 2.7 |
| Hispanic ethnicity | 7.5 | 6.6 | 7.1 | 1.7 | 7.7 | 7.4 | 7.8 | 8.0 | 1.1 |
| Socioeconomic and comorbidities | |||||||||
| Drug or alcohol use | 0.8 | 0.8 | 0.7 | 1.2 | 0.8 | 0.7 | 0.8 | 0.6 | 2.1 |
| Smoker | 7.1 | 7.7 | 6.9 | 0.6 | 7.2 | 7.4 | 7.5 | 7.4 | 0.6 |
| Cerebrovascular disease | 29.5 | 27.9 | 26.4 | 6.8 | 27.4 | 27.6 | 28.8 | 28.5 | 2.3 |
| Coronary artery disease | 52.2 | 51.1 | 49.7 | 4.8 | 49.4 | 50.5 | 50.5 | 52.8 | 6.8 |
| Heart failure | 79.1 | 77.2 | 75.1 | 9.4 | 75.6 | 76.6 | 77.0 | 78.2 | 6.2 |
| Pulmonary disease | 50.0 | 47.9 | 44.6 | 10.9 | 46.0 | 47.2 | 46.1 | 49.3 | 6.6 |
| Albumin, g/dl | 3.0 | 3.0 | 3.1 | 20.1 | 3.1 | 3.1 | 3.0 | 3.1 | 1.2 |
| Cancer | 23.2 | 24.0 | 22.8 | 1.0 | 23.2 | 23.4 | 22.9 | 23.3 | 0.4 |
| Hemoglobin | 10.0 | 10.0 | 10.1 | 5.9 | 10.0 | 10.1 | 10.1 | 10.1 | 8.7 |
| Diabetes | 49.8 | 48.1 | 49.2 | 1.4 | 48.5 | 49.3 | 49.7 | 49.2 | 1.4 |
| Body mass index, kg/m2 | 27.4 | 27.3 | 27.3 | 0.9 | 27.4 | 27.5 | 27.3 | 27.2 | 3.9 |
| Immobile | 16.8 | 13.0 | 10.2 | 19.5 | 13.5 | 13.7 | 13.1 | 13.3 | 0.6 |
| Peripheral vascular disease | 41.3 | 38.4 | 37.3 | 8.3 | 37.8 | 39.0 | 37.8 | 38.3 | 1.0 |
| Days of prior nephrologist care | 1.7 | 2.1 | 2.4 | 22.3 | 2.1 | 2.1 | 2.1 | 2.1 | 1.5 |
| Hospital days in first 90 d of dialysis | 7.2 | 3.1 | 1.0 | 101.8 | 3.3 | 3.5 | 3.4 | 3.3 | 0.4 |
| Hospital days in 90 d before dialysis | 13.5 | 10.8 | 9.4 | 29.2 | 11.0 | 11.0 | 10.8 | 11.5 | 3.6 |
| Provider, geographic, and facility | |||||||||
| Facility size (no. of patients) | 80.6 | 85.5 | 89.7 | 16.6 | 79.3 | 78.3 | 78.1 | 77.8 | 2.8 |
Data are expressed as percentages unless otherwise indicated. The third quartile ranges from three and one-half visits to four visits, whereas the fourth quartile is entirely composed of four visits per month. Because both include patients with four visits per month, these quartiles were pooled. Summary statistics by quartile of the instrumental variable (mean facility visits) reflect average differences within facilities from comparing each year with the year with the lowest mean facility visits. For more detail, see the Supplemental Appendix.
In the instrumental variable analysis, one additional provider visit per month was associated with a 5.8% increase in the probability of undergoing vascular access surgery (95% CI, 0.7% to 10.9%) (Supplemental Appendix, Supplemental Table 1). These findings are comparable in magnitude to findings from the main logistic regression analysis.
Discussion
We found that patients seen more frequently by their nephrologist or advanced practitioner in the first 90 days of hemodialysis were more likely to undergo surgery to create an AV fistula or place an AV graft. On average, one additional nephrologist or advanced practitioner visit per month increased the probability of vascular access surgery by nearly 5%. A companion instrumental variable analysis corroborated this finding. In a sensitivity analysis in which we only considered physician (and advanced practitioner) visits in months when patients were not hospitalized, the association between one additional visit and vascular access surgery was smaller in magnitude.
Evidence suggests that having seen a nephrologist in the months before the development of ESRD increases the likelihood of initiating hemodialysis with an AV fistula or graft.12–16 Our findings suggest that the purported benefits from specialist provider contact persist after starting hemodialysis. The association between one additional nephrologist visit per month after initiation of hemodialysis and vascular access surgery was only slightly smaller in magnitude to the benefit observed from seeing a nephrologist before starting hemodialysis. The larger magnitude of observed benefit from pre-ESRD visits may be due, in part, to unobserved health differences in patients who have access to nephrologist care before ESRD compared with patients who do not.
To assess the clinical significance of our findings, we reviewed published literature on mortality by vascular access type. Compared with a tunneled catheter, patients receiving hemodialysis through an AV fistula experience a 29%–64% reduction in the rate of mortality, whereas patients receiving dialysis through an AV graft experience an 8%–50% reduction in the rate of mortality.3–5,10 We combined these rate reductions with findings from our analysis. We estimate that one additional physician (or advanced practitioner) visit per month in the first 90 days of hemodialysis could reduce the absolute probability of death in the first year of hemodialysis by 0.3%–0.8%, to the extent that the association we observe between visit frequency and vascular access surgery represents a causal connection (Supplemental Appendix).
Early transition to dialysis through an AV fistula or graft could also lead to significant cost savings,20 and may decrease the likelihood that patients will remain on dialysis through a tunneled catheter indefinitely. Evidence suggests that the longer that patients receive dialysis through a catheter, the less likely it is that they will transition to an AV fistula or graft.21 Patients receiving dialysis through a catheter often develop central venous stenosis, which can prevent permanent vascular access placement.22 In addition, patients receiving dialysis with catheters frequently refuse placement of AV fistulas and grafts.23
There are several possible explanations for why more frequent visits might be associated with the creation of AV fistulas and placement of AV grafts. More face-to-face encounters could help providers to stabilize sick patients. Improved management of hypertension, volume overload, electrolyte abnormalities, malnutrition, and anemia may improve patients’ health, and these patients are then either more likely to be referred or more likely to be deemed acceptable surgical candidates once evaluated. Patients may be more willing to undergo surgery once recommended—particularly knowing that after vascular access surgery, hemodialysis will be conducted with regular needle sticks—if they gain trust in their dialysis care providers. The proverb “out of sight, out of mind” may be a simple explanation of these findings. Providers who do not see patients as often may be less likely to refer them for vascular access surgery—it may require face-to-face contact with a patient receiving catheter-based hemodialysis to prompt referral.
In 2004, the CMS transformed physician reimbursement for outpatient hemodialysis from a capitated system to a tiered fee-for-service system that encourages more frequent visits. Several studies since then have demonstrated that more frequent visits did not lead to substantial improvements in health outcomes for the majority of patients. For instance, one analysis of the reimbursement policy nationwide found no associated improvements in survival or listing for kidney transplantation in the United States24. A regional survey of 12 dialysis facilities found that although physician visit frequency increased briskly in response to the reimbursement policy, health outcomes did not improve.25 Another study examining the association between visit frequency and health outcomes at a national level in the period after reimbursement reform found no association between more frequent visits and mortality, and only a slight reduction in hospitalization among patients seen more frequently.26
Although more frequent visits do not appear to improve health outcomes in the majority of patients on hemodialysis,24–26 there may be specific groups of patients who benefit from closer monitoring. We previously demonstrated that patients recently discharged from the hospital benefit from more frequent visits through fewer rehospitalizations and reduced healthcare costs.27 This study suggests that the first 90 days of hemodialysis may be another period during which nephrologist or advanced practitioner visits can be particularly beneficial.
Under the current reimbursement system, the acuity of patient illness, including the time since starting dialysis and recent hospitalizations, plays only a minor role in determining how often providers see their patients. Instead, local provider practice patterns and economic incentives faced by individual providers explain a higher fraction of the variation in visit frequency.19 Current reimbursement encourages visits to all patients, irrespective of their health needs. Policies that encourage more frequent visits to patients who actually benefit from additional visits, such as patients who recently started dialysis or who were recently discharged from the hospital, could lead to improvements in health outcomes.
This study has several limitations. Because it is based on observational data, our analysis remains subject to selection bias. For example, if patients who are sicker in unobservable ways are less likely to be seen by their nephrologist and are also less likely to undergo vascular access surgery, this could bias our results. We attempt to address this potential bias by controlling for many observed characteristics and using an instrumental variable analysis. In addition, we were limited to studying patients aged ≥67 years upon initiation of dialysis. Although this comprises a significant fraction of the hemodialysis population, results may not be generalizable to younger patients starting hemodialysis or to patients with established ESRD. Finally, the claims data did not allow us to differentiate between visits from physicians and visits from advanced practitioners. It is possible that one of these providers is more effective or cost-effective in promoting vascular access surgery.
In summary, we found that patients seen more frequently in the first 90 days of hemodialysis are more likely to undergo early creation of an AV fistula or placement of an AV graft. Payment policies that encourage more frequent care provider visits to patients at key clinical time points may yield more favorable health outcomes than policies that operate irrespective of patients’ health status.
Concise Methods
Data and Patient Selection
We selected patients starting in-center hemodialysis in the United States through a central venous tunneled catheter between January 1, 2006, and September 31, 2009. We included patients who were aged ≥67 years at the time of dialysis initiation and who had Medicare Parts A and B coverage for at least 12 months before starting hemodialysis, owing to the availability of Medicare claims in the 2 years before hemodialysis initiation in this population. We obtained data on patients and dialysis facilities from the US Renal Data System, a registry of virtually all patients with treated ESRD in the United States.
We used procedure codes from Medicare claims in the 12 months before starting hemodialysis to identify patients who had a tunneled dialysis catheter in place at the start of hemodialysis and who did not also have an AV fistula or graft (Supplemental Appendix, Supplemental Table 2). We excluded 1152 cases in which we identified patients as starting hemodialysis with a tunneled catheter while the CMS Medical Evidence Report (CMS 2728), which is filled out by providers at the initiation of ESRD, documented that they began hemodialysis with a fistula or graft, and 4121 cases in which the CMS Medical Evidence Report documented that they had a maturing fistula or graft. We examined the sensitivity of our results to this exclusion (Supplemental Appendix). We used Medicare claims to identify patients who had an AV fistula created or graft placed within 90 days of starting dialysis.
Study Outcomes, Exposures, and Other Variables
We captured data on each patient from the start of hemodialysis for 90 days. The primary study outcome was whether patients had surgery to create an AV fistula or place an AV graft in the first 90 days of hemodialysis. The primary study exposure was the average number of monthly outpatient nephrologist (or advanced practitioner) visits to patients in the first 90 days of hemodialysis, obtained from Medicare claims (Supplemental Appendix, Supplemental Table 2). Because codes from claims captured zero, one, two to three, or four or more outpatient visits, we assigned claims for two to three visits a value of two and one-half visits, and claims for four or more visits a value of four visits. We varied these assumptions in sensitivity analyses (Supplemental Appendix). When calculating mean visit frequency for each patient, we excluded months that did not completely overlap with the first 90 days of dialysis and months after vascular access surgery.
We determined the presence or absence of comorbid conditions based on 12 prior months of Medicare claims and the Medical Evidence Report, and assumed that a comorbid condition was present if it appeared in either source. Because of a large number of missing values for Quetelet’s body mass index, hemoglobin, and albumin, we used multiple imputation to estimate these values.28 We included days hospitalized before ESRD and number of outpatient nephrologist visits before ESRD based from claims as categorical variables due to nonlinear associations between these variables and the study outcome. We obtained dialysis facility characteristics from the annual dialysis facility survey in the year of each patient’s ESRD onset, whereas information on population density came from census-based rural-urban commuting area codes.29 Because of the large population size, we used a 10% standardized difference as a marker of heterogeneity when comparing differences in characteristics between groups.30 We used cumulative incidence estimates to plot the probability of vascular access surgery among patients seen at different visit frequencies.
Statistical Analyses
We used multivariable logistic regression to evaluate the association between visit frequency and the odds of undergoing surgery to create an AV fistula or place an AV graft in the first 90 days of hemodialysis. We tested whether age or hospital days before starting hemodialysis modified the association between visit frequency and vascular access surgery using multiplicative interaction terms in regression models. In all regression analyses, we adjusted for calendar year along with patient, dialysis facility, and geographic characteristics listed in Table 2.
More frequent physician (and advanced practitioner) visits are associated with fewer hospitalizations and rehospitalizations.26,27 By reducing patients’ probability of being hospitalized, more frequent visits could increase the likelihood of undergoing vascular access surgery by making patients more available to be seen by a vascular surgeon. Alternatively, hospital days may confound the association between visit frequency and vascular access surgery. This might occur if, due to greater acuity of illness, patients who are hospitalized more often are both less likely to undergo vascular access surgery and less available to be seen in the outpatient hemodialysis setting.
We examined the sensitivity of our model to the relation between visit frequency, hospitalizations, and vascular access surgery by excluding months when patients were hospitalized from our calculation of visit frequency. We used this measure of visit frequency to assess for a nonlinear association between visit frequency and vascular access surgery after categorizing visit frequency into three groups.
To examine sensitivity to the temporal association between visit frequency and vascular access surgery, we modeled the likelihood of AV fistula creation or graft placement in the second full month of hemodialysis as a function of visit frequency in the prior month. In this analysis, we included hospital days in the prior month and days since starting dialysis as additional covariates (Supplemental Appendix).
Instrumental Variable Analyses
The results of our main analysis could be biased if unobserved patient and provider characteristics were associated with both the likelihood of a patient being seen by his or her nephrologist (or advanced practitioner) and of having vascular access surgery. To determine the sensitivity of our findings to this potential form of bias, we conducted a companion instrumental variable analysis. Instrumental variable analysis is a quasiexperimental approach that has been used to reduce bias in observational studies.31–33 The instrumental variable we used was the mean frequency of nephrologist or advanced practitioner visits to all prevalent Medicare patients dialyzed at a patient’s facility in each calendar year. We excluded visits to patients in the first 3 months of dialysis as well as patients included in our analytic cohort from the instrumental variable calculation. We used this facility-level instrumental variable to predict how often patients in our cohort were seen in the first 90 days of hemodialysis. The theoretical basis for our choice of instrument comes from previous findings that provider visit frequency in hemodialysis is determined to a greater degree by dialysis facility location than individual patient characteristics, in addition to similarities among physician networks and observations that providers working in close proximity to one another share practice patterns.19,34–37
Using a two-stage least-squares linear probability model, we measured the association between predicted visits in the first 90 days of dialysis and each outcome of interest. We controlled for patient demographic, socioeconomic, and comorbidity characteristics listed in Table 2. To account for potential unobserved differences in patient and provider characteristics among facilities with different levels of visit frequency, we controlled for fixed dialysis facility effects. Consequently, sample variation in all model parameters (including the instrumental variable) came from within-facility variation over time. Because of large numbers of missing data for body mass index, hemoglobin, and albumin, we excluded these covariates from the instrumental variable analysis, while demonstrating that these parameters did not vary considerably across levels of the instrument.
For an instrumental variable to be valid, it must be correlated with the exposure of interest and not be correlated with the outcome other than through the exposure. We assessed the correlation between our instrument and visit frequency using the F-statistic from a first-stage regression model of visit frequency on the instrument.38 For the second criterion, we suggest that providers visiting other patients in a dialysis facility should not affect a given patient’s chances of vascular access surgery other than through more frequent visits with the given patient. The degree to which the second criterion may be violated due to differences in the type of patient dialyzed in years when facilities experienced higher and lower values of the instrumental variable was explored by comparing observed characteristics among different levels of the instrument.39
This project was approved by an institutional review board of Stanford University School of Medicine.
Disclosures
None.
Supplementary Material
Acknowledgments
This research was supported by grants from the Agency for Healthcare Research and Quality (F32 HS019178 to K.F.E.) and the National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) (DK085446 to G.M.C.). Jay Bhattacharya would like to thank the National Institute on Aging for support for his work on this paper (R37 150127-5054662-0002).
This work was conducted under a data use agreement between W.C.W. and the NIDDK. An NIDDK officer reviewed the manuscript and approved it for submission. The data reported here have been supplied by the US Renal Data System. The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy or interpretation of the US Government.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2014050464/-/DCSupplemental.
References
- 1.US Renal Data System : 2013 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States, Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2013 [Google Scholar]
- 2.Dixon BS, Novak L, Fangman J: Hemodialysis vascular access survival: Upper-arm native arteriovenous fistula. Am J Kidney Dis 39: 92–101, 2002 [DOI] [PubMed] [Google Scholar]
- 3.Astor BC, Eustace JA, Powe NR, Klag MJ, Fink NE, Coresh J, CHOICE Study : Type of vascular access and survival among incident hemodialysis patients: The Choices for Healthy Outcomes in Caring for ESRD (CHOICE) Study. J Am Soc Nephrol 16: 1449–1455, 2005 [DOI] [PubMed] [Google Scholar]
- 4.Dhingra RK, Young EW, Hulbert-Shearon TE, Leavey SF, Port FK: Type of vascular access and mortality in U.S. hemodialysis patients. Kidney Int 60: 1443–1451, 2001 [DOI] [PubMed] [Google Scholar]
- 5.Pastan S, Soucie JM, McClellan WM: Vascular access and increased risk of death among hemodialysis patients. Kidney Int 62: 620–626, 2002 [DOI] [PubMed] [Google Scholar]
- 6.Pisoni RL, Arrington CJ, Albert JM, Ethier J, Kimata N, Krishnan M, Rayner HC, Saito A, Sands JJ, Saran R, Gillespie B, Wolfe RA, Port FK: Facility hemodialysis vascular access use and mortality in countries participating in DOPPS: An instrumental variable analysis. Am J Kidney Dis 53: 475–491, 2009 [DOI] [PubMed] [Google Scholar]
- 7.Polkinghorne KR, McDonald SP, Atkins RC, Kerr PG: Vascular access and all-cause mortality: A propensity score analysis. J Am Soc Nephrol 15: 477–486, 2004 [DOI] [PubMed] [Google Scholar]
- 8.Wasse H, Kutner N, Zhang R, Huang Y: Association of initial hemodialysis vascular access with patient-reported health status and quality of life. Clin J Am Soc Nephrol 2: 708–714, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wasse H, Speckman RA, Frankenfield DL, Rocco MV, McClellan WM: Predictors of central venous catheter use at the initiation of hemodialysis. Semin Dial 21: 346–351, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xue JL, Dahl D, Ebben JP, Collins AJ: The association of initial hemodialysis access type with mortality outcomes in elderly Medicare ESRD patients. Am J Kidney Dis 42: 1013–1019, 2003 [DOI] [PubMed] [Google Scholar]
- 11.Stehman-Breen CO, Sherrard DJ, Gillen D, Caps M: Determinants of type and timing of initial permanent hemodialysis vascular access. Kidney Int 57: 639–645, 2000 [DOI] [PubMed] [Google Scholar]
- 12.Avorn J, Winkelmayer WC, Bohn RL, Levin R, Glynn RJ, Levy E, Owen W, Jr: Delayed nephrologist referral and inadequate vascular access in patients with advanced chronic kidney failure. J Clin Epidemiol 55: 711–716, 2002 [DOI] [PubMed] [Google Scholar]
- 13.Jungers P, Zingraff J, Albouze G, Chauveau P, Page B, Hannedouche T, Man NK: Late referral to maintenance dialysis: detrimental consequences. Nephrol Dial Transplant 8: 1089–1093, 1993 [PubMed] [Google Scholar]
- 14.Ratcliffe PJ, Phillips RE, Oliver DO: Late referral for maintenance dialysis. Br Med J (Clin Res Ed) 288: 441–443, 1984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arora P, Obrador GT, Ruthazer R, Kausz AT, Meyer KB, Jenuleson CS, Pereira BJ: Prevalence, predictors, and consequences of late nephrology referral at a tertiary care center. J Am Soc Nephrol 10: 1281–1286, 1999 [DOI] [PubMed] [Google Scholar]
- 16.Astor BC, Eustace JA, Powe NR, Klag MJ, Sadler JH, Fink NE, Coresh J: Timing of nephrologist referral and arteriovenous access use: the CHOICE Study. Am J Kidney Dis 38: 494–501, 2001 [DOI] [PubMed] [Google Scholar]
- 17.Centers for Medicare & Medicaid Services (CMS), HHS: Dialysis facility compare. Quality measures: Best treatment practices, 2014. Available at: http://www.medicare.gov/DialysisFacilityCompare/Data/Best-Treatment-Practices.html?AspxAutoDetectCookieSupport=1. Accessed January, 20 2014
- 18.Centers for Medicare & Medicaid Services (CMS), HHS : Medicare program; revisions to payment policies under the physician fee schedule for calendar year 2004. Final rule with comment period. Fed Regist 68: 63195–63395, 2003 [PubMed] [Google Scholar]
- 19.Erickson KF, Tan KB, Winkelmayer WC, Chertow GM, Bhattacharya J: Variation in nephrologist visits to patients on hemodialysis across dialysis facilities and geographic locations. Clin J Am Soc Nephrol 8: 987–994, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Manns B, Tonelli M, Yilmaz S, Lee H, Laupland K, Klarenbach S, Radkevich V, Murphy B: Establishment and maintenance of vascular access in incident hemodialysis patients: A prospective cost analysis. J Am Soc Nephrol 16: 201–209, 2005 [DOI] [PubMed] [Google Scholar]
- 21.Lee T, Barker J, Allon M: Tunneled catheters in hemodialysis patients: Reasons and subsequent outcomes. Am J Kidney Dis 46: 501–508, 2005 [DOI] [PubMed] [Google Scholar]
- 22.MacRae JM, Ahmed A, Johnson N, Levin A, Kiaii M: Central vein stenosis: A common problem in patients on hemodialysis. ASAIO J 51: 77–81, 2005 [DOI] [PubMed] [Google Scholar]
- 23.Asif A, Cherla G, Merrill D, Cipleu CD, Briones P, Pennell P: Conversion of tunneled hemodialysis catheter-consigned patients to arteriovenous fistula. Kidney Int 67: 2399–2406, 2005 [DOI] [PubMed] [Google Scholar]
- 24.Erickson KF, Winkelmayer WC, Chertow GM, Bhattacharya J: Medicare reimbursement reform for provider visits and health outcomes in patients on hemodialysis. Forum Health Econ Policy 17: 53–77, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mentari EK, DeOreo PB, O’Connor AS, Love TE, Ricanati ES, Sehgal AR: Changes in Medicare reimbursement and patient-nephrologist visits, quality of care, and health-related quality of life. Am J Kidney Dis 46: 621–627, 2005 [DOI] [PubMed] [Google Scholar]
- 26.Slinin Y, Guo H, Li S, Liu J, Ensrud K, Gilbertson DT, Collins AJ, Ishani A: Association of provider-patient visit frequency and patient outcomes on hemodialysis. J Am Soc Nephrol 23: 1560–1567, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Erickson KF, Winkelmayer WC, Chertow GM, Bhattacharya J: Physician visits and 30-day hospital readmissions in patients receiving hemodialysis. J Am Soc Nephrol 25: 2079–2087, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Montez-Rath ME, Winkelmayer WC, Desai M: Addressing missing data in clinical studies of kidney diseases. Clin J Am Soc Nephrol 9: 1328–1335, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.WWAMI Rural Health Research Center: Rural-Urban Commuting Area Codes (RUCA), Seattle, WA, WWAMI Rural Health Research Center, 2005 [Google Scholar]
- 30.Austin PC: Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 28: 3083–3107, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dennis MS, Burn JP, Sandercock PA, Bamford JM, Wade DT, Warlow CP: Long-term survival after first-ever stroke: The Oxfordshire Community Stroke Project. Stroke 24: 796–800, 1993 [DOI] [PubMed] [Google Scholar]
- 32.Wang PS, Schneeweiss S, Avorn J, Fischer MA, Mogun H, Solomon DH, Brookhart MA: Risk of death in elderly users of conventional vs. atypical antipsychotic medications. N Engl J Med 353: 2335–2341, 2005 [DOI] [PubMed] [Google Scholar]
- 33.McClellan M, McNeil BJ, Newhouse JP: Does more intensive treatment of acute myocardial infarction in the elderly reduce mortality? Analysis using instrumental variables. JAMA 272: 859–866, 1994 [PubMed] [Google Scholar]
- 34.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL: The implications of regional variations in Medicare spending. Part 1: The content, quality, and accessibility of care. Ann Intern Med 138: 273–287, 2003 [DOI] [PubMed] [Google Scholar]
- 35.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL: The implications of regional variations in Medicare spending. Part 2: Health outcomes and satisfaction with care. Ann Intern Med 138: 288–298, 2003 [DOI] [PubMed] [Google Scholar]
- 36.Soumerai SB, McLaughlin TJ, Gurwitz JH, Guadagnoli E, Hauptman PJ, Borbas C, Morris N, McLaughlin B, Gao X, Willison DJ, Asinger R, Gobel F: Effect of local medical opinion leaders on quality of care for acute myocardial infarction: A randomized controlled trial. JAMA 279: 1358–1363, 1998 [DOI] [PubMed] [Google Scholar]
- 37.Landon BE, Keating NL, Barnett ML, Onnela J-P, Paul S, O’Malley AJ, Keegan T, Christakis NA: Variation in patient-sharing networks of physicians across the United States. JAMA 308: 265–273, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Staiger D, Stock JH: Instrumental variables regression with weak instruments. Econometrica 65: 29, 1997 [Google Scholar]
- 39.Altonji JG, Elder TE, Taber CR: Selection on observed and unobserved variables: Assessing the effectiveness of Catholic schools. J Polit Econ 113: 151–184, 2005 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.