Abstract
The transition of AKI to CKD has major clinical significance. As reviewed here, recent studies show that a subpopulation of dedifferentiated, proliferating tubules recovering from AKI undergo pathologic growth arrest, fail to redifferentiate, and become atrophic. These abnormal tubules exhibit persistent, unregulated, and progressively increasing profibrotic signaling along multiple pathways. Paracrine products derived therefrom perturb normal interactions between peritubular capillary endothelium and pericyte-like fibroblasts, leading to myofibroblast transformation, proliferation, and fibrosis as well as capillary disintegration and rarefaction. Although signals from injured endothelium and inflammatory/immune cells also contribute, tubule injury alone is sufficient to produce the interstitial pathology required for fibrosis. Localized hypoxia produced by microvascular pathology may also prevent tubule recovery. However, fibrosis is not intrinsically progressive, and microvascular pathology develops strictly around damaged tubules; thus, additional deterioration of kidney structure after the transition of AKI to CKD requires new acute injury or other mechanisms of progression. Indeed, experiments using an acute-on-chronic injury model suggest that additional loss of parenchyma caused by failed repair of AKI in kidneys with prior renal mass reduction triggers hemodynamically mediated processes that damage glomeruli to cause progression. Continued investigation of these pathologic mechanisms should reveal options for preventing renal disease progression after AKI.
Keywords: acute renal failure, fibrosis, CKD, hypoxia, hypertension, tubular epithelium
Incomplete recovery from AKI can lead to long-term functional deficits that are severe and progressive in subpopulations of patients with preexisting CKD.1–6 Kidneys from patients recovering from AKI exhibit chronic dysfunction, tubule atrophy, and interstitial fibrosis (Figure 1, E and F).7–20 Incomplete recovery from AKI in patients with CKD not only adds to preexisting pathology and dysfunction but also, may synergize with hemodynamic mechanisms of progression. Severe loss of kidney mass by CKD has long-term adverse consequences attributable to impaired blood flow autoregulation, glomerular hypertension, glomerulosclerosis, and tubulointerstitial fibrosis.21–25 Additional nephron loss by AKI in patients with CKD could tip the balance of functional reserve through hemodynamic effects.4 Thus, failed recovery from AKI may have far-reaching significance. Recent research has provided insights into the pathologic basis for this failed recovery from AKI (i.e., tubule atrophy and renal fibrosis [tubulointerstitial fibrosis]).
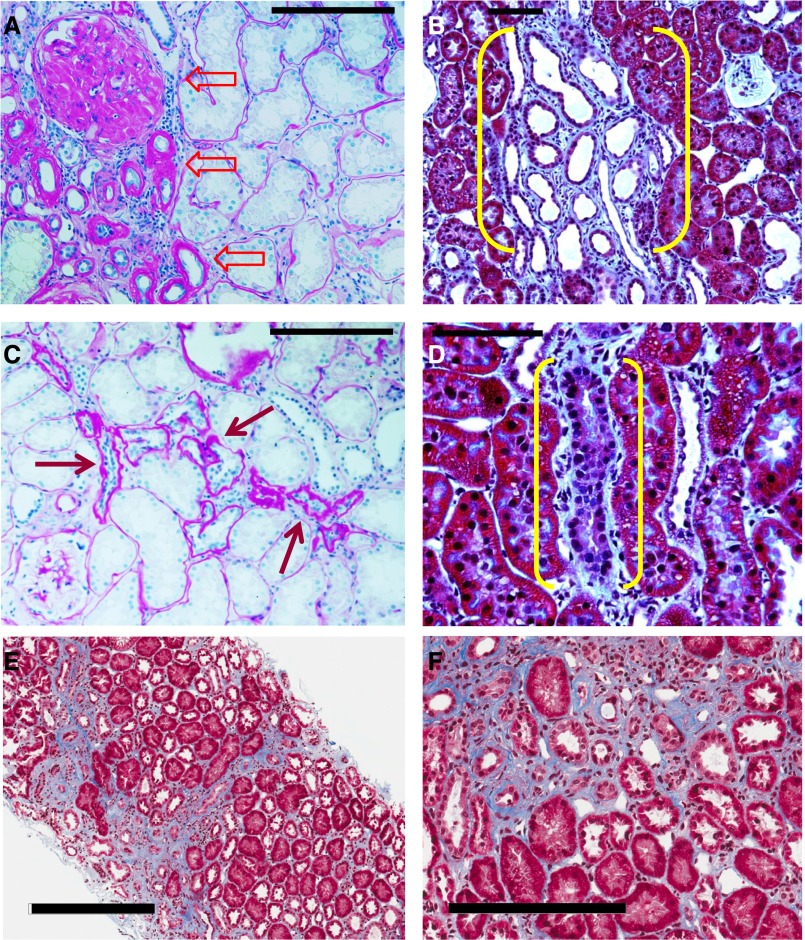
Figure 1.
Injured kidney tissue heals by fibrosis that does not extend to involve previously nondiseased parenchyma. (A and C) Periodic acid–Schiff staining of the kidney from an autopsy of a patient with human FSGS. (A) Advanced scar containing sclerotic glomerulus, atrophic tubules with greatly thickened basement membranes, and interstitial fibrosis is sharply demarcated from completely normal parenchyma (block arrows with red outlines). There is no indication of fibrosis spreading from the scar into the adjacent interstitium. (C) Small scar from the same kidney showing a few atrophic tubules with thick basement membranes and expanded interstitium adjacent to the atrophic tubules (red arrows) near a glomerulus with mild mesangial expansion. The histopathology is one of resolved injury to tubules with development of a shrunken scar in relationship to an atrophic nephron with no suggestion that the lesion is invasive or expansive in its nature. (B and D) Kidney of rat 14 days after AKI was induced by proximal tubule selective toxin maleic acid stained with Masson’s Trichrome. (B) Low-power micrograph showing a localized lesion containing undifferentiated atrophic tubules surrounded by a florid early fibrotic response (yellow brackets). The lesion is sharply demarcated from the adjacent well differentiated proximal tubules that had either recovered normally after AKI or had not been injured by the poison. (D) High-power micrograph showing a single profile of an atrophic tubule with surrounding fibroblastic response (yellow brackets). Adjacent proximal tubules are well differentiated. The interstitium between them is either normal or minimally expanded. Interstitial fibroblastic responses that occur after AKI resolve and regress as tubules recover and redifferentiate or persist and undergo scarring if tubules fail to redifferentiate and become atrophic. (E and F) Kidney biopsy from a patient 10 months after post-transplant AKI with delayed graft function stained with Masson’s Trichrome (provided by Robert B. Colvin, Massachusetts General Hospital and Harvard Medical School, Boston, MA). (E) Low-power micrograph showing shrunken mature scars separated by healthy parenchyma with minimal or no increase of interstitial connective tissue. (F) High-power micrograph with sharply demarcated boundary between scar and healthy tubules. One healthy well differentiated proximal tubule remains within the scar, suggesting that it had not been injured during the AKI episode 10 months earlier or had recovered normal structure during regeneration and repair after injury. Scale bars, 100 µm in A–D; 300 µm in E; 200 µm in F.
Regardless of the diverse origins of CKD in blood vessels, glomeruli, or tubules, tubulointerstitial fibrosis is the major pathway of progression to ESRD.26 In CKD caused by hypertension or GN, fibrosis develops around tubules made atrophic by ischemia, misdirected glomerular filtration, and disuse.27,28 After primary tubule injury by AKI, glomeruli remain structurally normal over the short term, even as tubules atrophy and fibrosis develops. However, over the long term, glomeruli in nephrons that emerge unscathed from AKI can suffer hypertensive damage and foster progression if AKI had occurred in kidneys with reduced renal reserve.29
Why some tubules damaged by AKI become atrophic and then give rise to subsequent long-term adverse effects, whereas others recover completely is a fundamentally important unanswered question. Particularly noteworthy in the AKI-CKD transition and subsequent progression are epithelial pathologies that prevent tubule recovery, the cellular biology of fibrosis, and the significance of renal mass reduction (RMR) by prior CKD. Here, we review the pathology and pathophysiology of the AKI-CKD transition and its potential over the long term to degrade nephrons that had not been severely injured by the initial AKI insult.
By Itself, Renal Fibrosis Is Not Progressive; Progression Requires Additional Injury
Although fibrosis in response to injury is often perceived to be a pathologic and destructive event, it is essentially a self-limiting repair process that restricts injury. After tissue damage, fibroblasts use signaling and genetic/epigenetic programs to proliferate and make connective tissue but then, regress as scar tissue matures and contracts. Therefore, such fibrosis is not autonomous and does not expand or invade normal tissue. Rather, it shrinks. Damage to tubules is associated with fibrosis around them. Endothelial injury and capillary loss around damaged tubules may produce hypoxia that likely prevents recovery of the affected segments and ensures tubule atrophy.30–38 However, such interactions are confined to diseased tubulointerstitial microenvironments. Therefore, as in any other scar, fibrotic tissue that is formed around damaged tubules shrinks over time as activated fibroblasts regress and collagens mature. That is, fibrosis develops only around atrophic tubules, and the surrounding tubulointerstitium remains normal. Pathologic observations bear this out—kidney surfaces in benign nephrosclerosis display shrunken scars alternating with areas of hypertrophic cortex. Biopsies of patients with chronic glomerular disease show clusters of atrophic tubules surrounded by fibrosis that is confined to regions containing diseased glomeruli28 (Figure 1, A and C). Similarly, during repair of experimental AKI, tubules that fail to recover normal structure become atrophic, and fibrosis develops around them in microenvironments sharply demarcated from tubules that had recovered normally or had not been injured (Figure 1, B and D) (AKI induced by maleate and tissue from the work by Lan et al.39). Much later, such lesions would shrink further and become less perceptible (i.e., they do not progress). Fibrotic scars that develop after ischemia-reperfusion injury (IRI) show similarly sharp demarcations from normal kidney tissue (figure 2 in the work by Goldfarb et al.,40 figure 4g in the work by Yang et al.,41 and figures 10 and 11 in the work by Lan et al.39). Indeed, small islands of pristine kidney remain within areas of extensive scarring after IRI (figures 10 and 11 in the work by Lan et al.39); fibrosis had not involved these preserved tubules because they either had not been injured or had recovered normally after injury. Pathologic features of healed human post-transplant AKI with delayed graft function bear this out: 10 months after AKI, there is patchy fibrosis containing atrophic tubules, but the fibrotic scars are clearly separated by sharply demarcated healthy parenchyma, with only minimal focal increase of interstitial connective tissue (Figure 1, E and F).
Figure 2.
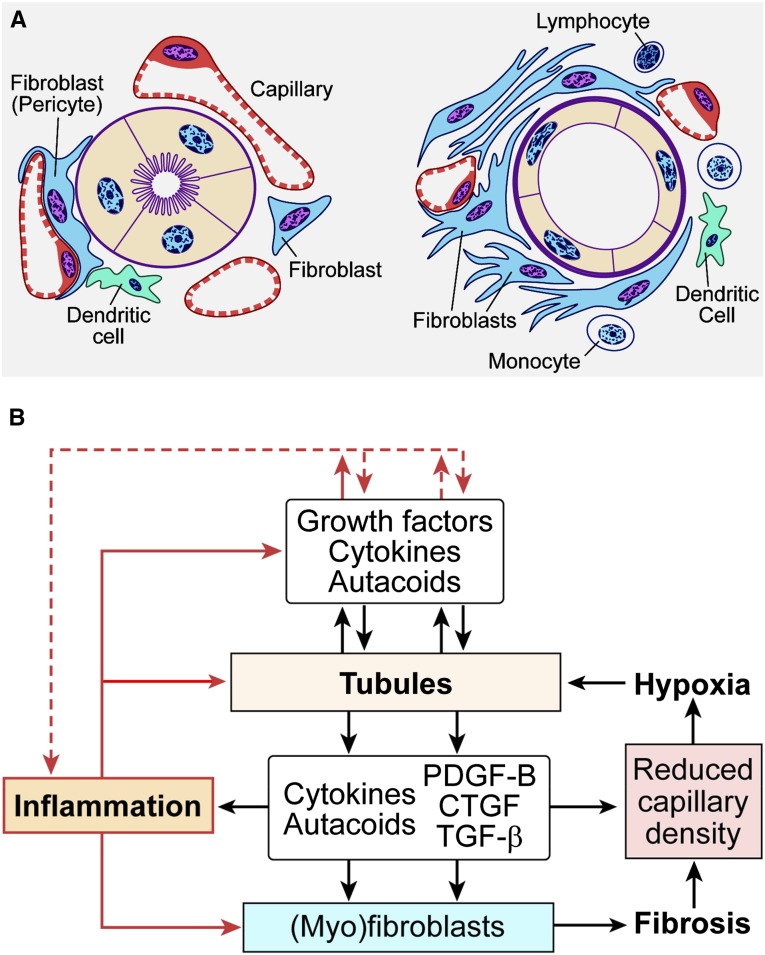
Pathologic events in tubules and interstitium interact to produce tubulointerstitial fibrosis. (A) Schematic diagram of (left panel) normal tubule-interstitium and (right panel) early tubulointerstitial fibrosis. Resident fibroblasts in the interstitium may or may not have intimate relationships to peritubular capillaries and basement membranes of tubules. The former type has also been termed pericyte. After injury, this type of fibroblast/pericyte detaches from capillaries, initiating pathologic events that cause capillary disintegration and rarefaction as well as myofibroblasts transformation and proliferation. This process is aided and abetted by inflammatory cells, chiefly monocytes, and resident immune cells, including dendritic cells. (B) Schematic diagram illustrating vicious cycle feedback interactions between tubule pathology and interstitial pathology that potentiate tubule atrophy. Modified from reference 4, with permission.
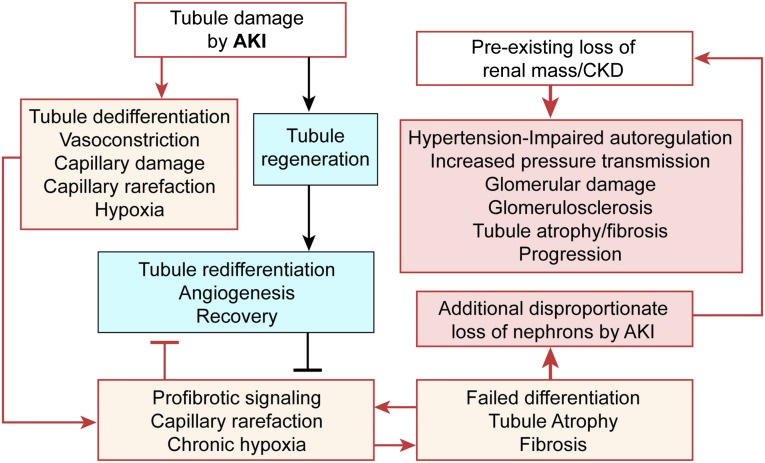
Figure 4.
Failed tubule differentiation and RMR after AKI lead to hemodynamic abnormalities that cause progression. Schematic diagram illustrating the effects of AKI that lead to tubulointerstitial fibrosis, the RMR that retards recovery of tubules regenerating after AKI, and the resulting disproportionate further reduction of renal mass that triggers hemodynamic mechanisms of renal disease progression.
Thus, insights from studies of kidney pathology inform us that progressive renal fibrosis requires additional, repetitive, and/or severe damage of previously normal nephrons unless primary interstitial disease is itself the instigating factor for fibrosis. One possibility is that one or more episodes of acute injury subsequent to initial AKI cause progression. Repeated but not single episodes of myohemoglobinuric AKI caused fibrotic CKD.42 Alternatively, single episodes of massive AKI could produce severe tubulointerstitial fibrosis and consequent RMR, triggering adverse hemodynamic events that foster progression, particularly in settings where functional renal mass had been reduced by prior CKD (see below). These principles apply to all forms of primary glomerular and tubulointerstitial disease: progression requires serial recruitment of nephrons to the injury process—be it slow and indolent or rapid and severe. Fibrosis progresses incrementally, closely following each nephron or clusters of nephrons damaged by nascent injury.
Cellular Origin of Interstitial Fibrosis after AKI
After AKI, humoral factors from regenerating tubules as well as inflammatory cells, including monocytes, lymphocytes, and dendritic cells, activate interstitial precursor cells that become (myo)fibroblasts, which proliferate and make connective tissue. The majority of resident precursors—termed pericytes43,44 or fibroblasts28,45,46—are cells with branching processes that contact capillaries and tubules.28,43,47,48 They express pericyte markers 5′-ectonucleotidase (CD73) and type I collagen and make contacts with dendritic cells.28,43,47,48 By lineage analysis, precursors termed pericytes are derived from FoxD1–expressing embryonic progenitors.44 Ephrin B signaling between pericytes and capillary endothelium maintains pericyte quiescence and endothelial integrity.49 Maintenance of endothelial integrity also involves vascular endothelial growth factor (VEGF) produced by pericytes and proximal tubules.37,50 Activating signals from several sources disrupt these interactions, inducing intercellular proteolysis that is followed by dissociation from each other. Two important effects ensue: (1) PDGFRβ-mediated migration and transformation of fibroblasts/pericytes to α-smooth muscle actin (α-SMA) –expressing (myo)fibroblasts and (2) dysangiogenic VEGF signaling, causing loss of endothelial integrity37 attributable to loss of the nursing function of pericytes that stabilize capillaries.51 With continued activation, the interstitium becomes widened by proliferating myofibroblasts and connective tissue, and the injured endothelium regresses, causing capillary rarefaction (Figure 2A).51
Pathologic events at the endothelial–pericyte/fibroblast interface that disrupt capillaries and cause the detachment, transformation, migration, and proliferation of fibroblasts include perturbations of the activities of disintegrin ADAMTS-1 and protease inhibitor TIMP3, bidirectional Ephrin B2 signaling, and VEGFR2.37,43,48,52–54 These events are reinforced by signaling through wnt, TGF-β, PDGF-B, connective tissue growth factor (CTGF), and sonic hedgehog pathways in myofibroblasts, with contributions from microRNA21, PPARα, and NOX4.37,52,54–63 Although triggered by tubule damage and loss of endothelial–pericyte/fibroblast interactions, the subsequent proliferation of (myo)fibroblasts, fibrosis, and capillary rarefaction may depend also on cytokines and growth factors from monocytes that infiltrate injured kidneys (Figure 2).64,65
Although pericytes seem to be the major source of fibroblasts driving fibrosis, other sources exist. Classic fibroblasts without special relationship to capillaries are present between tubules and around arterioles, and they contribute to fibrosis.47,66 Bone marrow–derived precursors were reported to infiltrate kidneys after injury and become myofibroblasts.67,68 However, these invading cells did not express collagen or proliferate after TGF-β stimulation,67,68 unlike fibroblasts that do.69–71 Moreover, hematopoietic stem cells (cells reported to become myofibroblasts in injured kidneys) can fuse with tissue recipients and produce tetraploid cells, thereby generating spurious signals of transdifferentiation72–74; also, rare bone marrow monocytes/macrophages can express α-SMA.75,76 Moreover, other investigators could not identify transplantable bone marrow precursors of α-SMA–expressing cells in normal or injured kidneys.76,77 Bone marrow derivation of kidney myofibroblasts remains confounded by lineage issues and technical artifacts. There also are difficulties in distinguishing markers in bone marrow–derived precursor cells and myeloid cells in injured kidneys from those of fibroblasts/pericytes and myofibroblasts on account of complex branching processes in the latter. High-resolution microscopy is required to distinguish fibroblasts/pericytes and their transformants from the large numbers of myeloid cells that do infiltrate injured kidneys.78 Moreover, the concept that fibrocytes of myeloid lineage79 become myofibroblasts in the kidney80 is doubtful owing to uncertainties of collagen expression versus collagen internalization by these cells.78 Endothelial-mesenchymal transition—a putative mechanism for myofibroblast derivation from endothelium68,81—is also controversial owing to possible lineage artifacts caused by nonspecificity of endothelial markers,78 whereas several publications have convincingly refuted a role for epithelial-mesenchymal transitions in kidney fibrosis.46,66
Vasoconstriction, Endothelial Injury, Capillary Compression, and Rarefaction: A Role for Poor Blood Flow and Hypoxia after AKI
Blood flow is persistently decreased after IRI in deep cortex and outer medulla—the regions most injured by ischemia. The decrease is brought about by vasoconstriction, tissue edema, endothelial swelling, and capillary disintegration, leading to microvascular rarefaction.31,36,82–95 Reduced blood flow during the extension phase of IRI could cause hypoxia in microenvironments of injured tubules and promote tubulointerstitial fibrosis.31,34,36,82–86,95,96 Microvascular defects and tubulointerstitial fibrosis after AKI occur in close conjunction with tubule hypoxia shown by pimonidazole adduct formation.34,40,96 VEGF-A expression in proximal tubules is lost early after AKI followed by decreased peritubular capillary density, perfusion defects, and tubule hypoxia,30,31,33,34,36,96,97 consistent with a role for tubule VEGF-A for peritubular capillary development50 and proliferation.98 Failure of endothelial cells to regenerate after kidney injury may explain capillary rarefaction.35 Interventions that avert tissue hypoxia by increasing blood flow or maintaining endothelial integrity mitigate tubulointerstitial fibrosis after kidney injury.34,37,99 These findings dovetail findings that tubule VEGF-A in tubules decreases after injury, and VEGF-A expression in pericytes/fibroblasts and macrophages shifts from predominantly VEGF164 isoform to dysangiogenic isoforms (VEGF120 and -188).37 Concurrently with these alterations, PDGF-B increases in tubules, endothelium, and macrophages. Crucially, blockade of PDGFRβ or VEGFR2 signaling by soluble ectodomains of their receptors prevents myofibroblast transformation and capillary damage and rarefaction, maintains normal capillary–pericyte/fibroblast interactions, and ameliorates fibrosis.37 These studies emphasize that physiologic signaling between endothelial cells and FoxD1+ pericytes/fibroblasts maintains their quiescent and differentiated states and keeps in abeyance disruptive VEGF and PDGF-B signaling that causes capillary rarefaction and myofibroblast transformation.
Kidneys are physiologically hypoxic in vulnerable medullary regions, where pO2 is normally as low as 4–5 mmHg.86,100–102 In view of tenuous oxygen tensions in mitochondria of parenchymal cells103 caused by steep oxygen gradients from capillaries across interstitial spaces and cytoplasm,104 oxygen available for respiration could fall further to precipitously low concentrations when interstitial spaces are widened by edema and inflammation and capillaries regress during fibrosis. Indeed, pathologic hypoxia shown by pimonidazole technique in deep cortex—outer medullary regions during early reperfusion after IRI105—persists as fibrosis develops.34,40 Consequent to hypoxia, tubule recovery after AKI could be impaired by oxidant stress, protein synthesis inhibition, and growth arrest—the known adverse effects of hypoxia.106–109 However, such hypoxic effects should remain confined to the injured tubule-interstitial microenvironments. In such locations but not beyond, hypoxia could prevent epithelial recovery through feedback effects that ensure tubule atrophy (Figure 2). Apropos the effects of hypoxia on tubule recovery, the actions of TGF-β antagonism to promote tubule differentiation during recovery from IRI110 could be ascribed to not only direct effects of TGF-β antagonism on regenerating tubules110 but also, conceivably, effects that preserve the renal microvasculature, thereby mitigating hypoxia and averting tubule atrophy and fibrosis.110,111 It is worth noting, however, that hypoxic effects that lead to tubule atrophy and fibrosis may involve other mechanisms as well, including HIF-1–dependent and –independent processes.101,112
Roles of Cortical Versus Medullary Pathology in the AKI-CKD Transition
As outlined above, falling oxygen tensions in the renal medulla could injure tubules after AKI; however, transition from acute injury to chronic medullary disease is only partially understood. Being most prone to injury after AKI, S3 proximal tubule segments in medullary rays of the inner cortex and the outer stripe of outer medulla (OSOM) have received most attention. In part, S3 segments are most injured because of cell-specific susceptibility of S3 cells.113 However, complexity of outer medullary microcirculation, disproportionately poor blood reflow to medulla after ischemia, and tubule hypoxia caused by oxygen gradients attributable to countercurrent vascular systems also contribute substantially.86,87,114–116 Most of our understanding of the AKI-CKD transition is, in fact, derived from research on the progression of tubulointerstitial fibrosis in the OSOM. We note, however, that such medullary pathology in the OSOM and conceivably, the inner stripe of outer medulla (see below), if extensive, could give rise to secondary damage in the cortex as a consequence of hemodynamic injury mechanisms triggered by significantly reduced renal mass (discussed below).
However, we have little knowledge regarding the development of chronic pathology after AKI in the inner stripe of outer medulla—a region crucial for several critical kidney functions and the site of a dense grouping of collecting ducts in the interbundle region most distant from the vascular bundles and thus, most vulnerable to hypoxia.117 This microanatomic feature suggests that pathology of the inner stripe will affect the integrity of large areas of the cortical hinterland in proportion to the number of collecting ducts that are involved.
Cortical damage caused by medullary pathology would be particularly severe if medullary tubules undergo atresia as the result of tubulointerstitial fibrosis and therefore, become obstructed. It is surprising that this aspect of post-AKI pathophysiology receives little attention. The cortical consequences of tubule obstruction in the medulla are exemplified by clinical experience; human papillary necrosis, such as that caused by acetaminophen toxicity, causes damage to the papilla, but this is followed by cortical atrophy. Studies have emphasized acute damage in ascending thick limbs of Henle caused by reduced blood flow and hypoxia attributable to adverse oxygen gradients,40,86,114,115,117 but there has been little focus on chronic pathology. In this connection, we have consistently noticed significant fibrosis with reduced tubule numbers in the inner stripe chronically after IRI (unpublished observations), but we, also, have not studied this pathology in detail. In-depth investigation of this aspect of medullary pathology after AKI is clearly in order.
Failed Differentiation of Regenerating Epithelium Leads to Profibrotic Signaling That Persists in Tubules Undergoing Atrophy after AKI
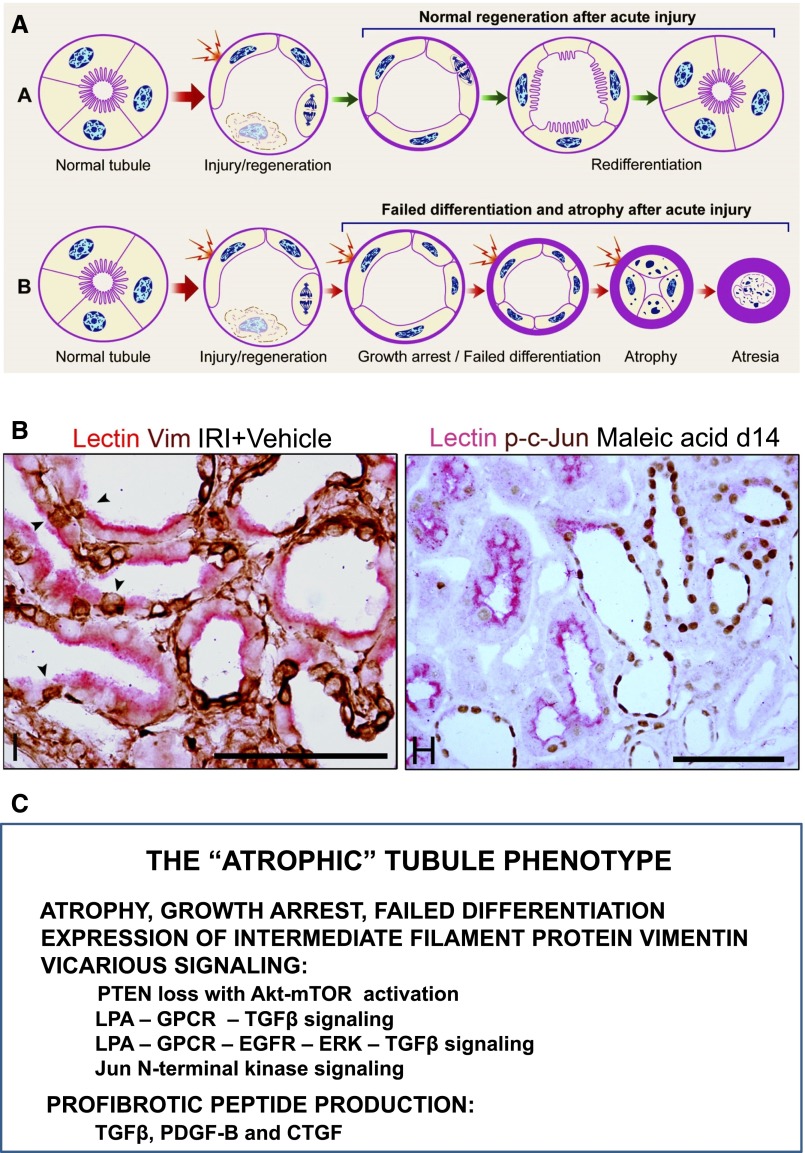
Some proximal tubule cells that dedifferentiate during regeneration after IRI fail to redifferentiate and regain normal structure during recovery.39,110,118 Such abnormally undifferentiated but growth-arrested epithelium occurred along entire tubule segments, in small cell clusters, or as single undifferentiated cells surrounded by differentiated proximal tubule cells late during recovery after IRI.39 Remarkably, the abnormal epithelium displayed intense signaling activity and expressed profibrotic peptides, despite being growth arrested and atrophic by morphologic criteria.39 These findings were similar to earlier observations on proximal tubules undergoing atrophy in a microembolic ischemia model.119 On the basis of these observations,39,119 we postulated that tubules undergoing pathologic growth arrest during regeneration after AKI fail to differentiate, signal vicariously through multiple profibrotic pathways, and secrete fibrogenic peptides into the interstitium, instigating fibrosis (Figure 3).4 Underlying this hypothesis is the activation after AKI of signaling pathways required for dedifferentiation, migration, and proliferation. For this purpose, the surviving epithelium produces and secretes growth factors, cytokines, and autacoids.82,120–122 These signaling and secretory events are required for normal regeneration, but they should cease when tubules recover. Therefore, persistence of proliferative signaling in growth–arrested undifferentiated epithelium undergoing atrophy is inherently abnormal. We showed that such atrophic tubules are engaged in pathologically increased signaling through PI3K-Akt-mTOR (mammalian target of rapamycin), ERK-MAPK, JNK-MAPK, and TGF-β pathways, with markedly increased expression of profibrotic peptides PDGF-B, CTGF, and TGF-β.39,110,118,123
Figure 3.
Failed differentiation of proximal tubules regenerating after AKI leads to development of the atrophic abnormally signaling profibrotic tubule phenotype. (A) Schematic diagram illustrating (upper panel) the normal pathway of proximal tubule cell dedifferentiation and proliferation followed by redifferentiation and recovery of normal structure after AKI and (lower panel) the abnormal pathway of failure to redifferentiate after early dedifferentiation that leads to tubule atrophy after AKI. (B, left panel) Immunohistochemistry and PHA lectin affinity cytochemistry of atrophic and normal proximal tubule cells 14 days after IRI in rats. Mosaic tubules showing well differentiated proximal tubule cells with brush border–bound PHA (lectin) staining pink in close juxtaposition with atrophic epithelium without brush border that stains brown for the expression of vimentin, an intermediate filament protein that is not present in differentiated proximal tubule cells but is rapidly expressed after dedifferentiation during regeneration and retained after atrophy occurs. (B, right panel) Immunohistochemistry and lectin cytochemistry of proximal tubules 14 days after AKI induced by proximal tubule selective toxin maleic acid. Well differentiated proximal tubule profiles and well differentiated proximal tubule cells in a mosaic tubule (center) exhibit pink staining for brush border–bound PHA lectin but no nuclear staining for phospho-c-Jun, whereas atrophic tubule profiles and atrophic cells in mosaic tubule (center) show nuclear staining for phospho-c-Jun, indicating the activation of the JNK-MAPK signaling pathway. (C) The diverse abnormalities exhibited by atrophic tubules are listed. These several alterations take place in vimentin–expressing atrophic tubules illustrated in B, left panel. Scale bars, 100 µm. A is modified from reference 4, with permission. B is modified from reference 39, with permission. GPCR, G-protein coupled receptor; JNK-MAPK, Jun N-terminal kinase-mitogen activated protein kinase; LPA, lysophosphatidic acid; PHA, phytohemagglutinin; PTEN, phosphatase and tensin homolog.
Experiments performed in tissue culture and in vivo showed that increased profibrotic TGF-β signaling in tubules recovering from AKI is, in part, attributable to autocrine signaling by lysophosphatidic acid. Lysophosphatidic acid signaling through separate G protein–coupled receptors triggers αvβ6 integrin–dependent activation of latent TGF-β as well as transactivation of EGFR and ERK-MAPK. Although divergent when initiated, the two pathways cooperatively converge to increase TGF-β signaling and thereby, increase the production and secretion of PDGF-B and CTGF.110,118,123 Furthermore, signaling intensities as well as signaling protein and growth factor expression in these abnormal tubules increased progressively with time to strikingly high levels—far higher than during the earlier stages of physiologic regeneration.39,110,118,123 Interestingly, after microembolic kidney ischemia,119 fibrosis developed within interstitial spaces abutting PDGF-B–expressing undifferentiated atrophic tubule epithelial cells but not differentiated cells without PDGF-B. In such fibrotic microenvironments, myofibroblasts expressed PDGFRβ, the cognate receptor for PDGF-B, suggesting that PDGF-B from atrophic epithelium had given rise to fibrosis through paracrine effects.
We have reported that atrophic tubules also exhibit near-total depletion of phosphatase and tensin homolog (PTEN), the lipid phosphatase that inhibits PI3K signaling.39 PTEN is normally low in proliferating proximal tubule cells but highly expressed in quiescent differentiated epithelium, and PTEN decreases were shown to be driven, at least in part, by upstream TGF-β signaling.39 However, the most proximal causes of unregulated signaling in the growth–arrested atrophic proximal tubules that develop after IRI are unknown, including those for TGF-β and the related PTEN abnormality. Recent studies have emphasized the role of premature growth arrest in giving rise to the profibrotic tubule phenotype.41 We also have observed that pathologically dedifferentiated profibrotic atrophic tubules with signaling disorders are growth arrested, which was inferred by lack of expression of Ki67, a marker for cycling cells.39 Whether tubule growth arrest during regeneration after AKI is a uniquely controlled pathologic event that causes profibrotic signaling or part of a spectrum of pathology controlled by a common upstream abnormality that also disrupts differentiation programs, causes ongoing cell injury, and instigates profibrotic signaling remains to be determined.
Tubule Selective Injury Is Sufficient to Drive Fibrosis, Inflammation, and Capillary Rarefaction
Paracrine triggers that compromise capillary integrity and activate myofibroblast precursors during AKI may derive from inflammatory/immune cells and stressed tubule epithelium. Because tubules and capillaries can be simultaneously injured during AKI produced by ischemia, it is difficult in these contexts to distinguish the most proximal activating factors that drive endothelial–pericyte/fibroblast dissociation, capillary rarefaction, and myofibroblast proliferation. Interventions, such as TGF-β antagonism, that protect against fibrosis development after IRI110,111 cannot distinguish between benefits conferred by restored microvascular integrity and those that promote tubule recovery. Nevertheless, tubule damage, by itself, can be sufficient to produce the full spectrum of interstitial pathology. Infiltrates of myofibroblasts and monocytes/macrophages developed exclusively around proximal tubules selectively damaged by uranyl ions, and images of 3H-thymidine autoradiography in sections stained for α-SMA showed clear relationships of regenerating epithelium to myofibroblasts in surrounding interstitium.124 Fibrosis developed around tubules selectively injured by folic acid, and affected tubules in hypoxic environments (indicated by pimonidazole adducts) showed loss of VEGF-A corresponding to fibrosis and capillary loss in adjoining interstitium.96 We investigated tubulointerstitial fibrosis in rats after injections of maleic acid,39 a proximal tubule–selective poison.125 Two weeks after maleic acid, patchy fibrosis with mononuclear cell infiltrates developed around atrophic tubules39 together with capillary rarefaction and myofibroblast increase in the interstitium (unpublished observations). Furthermore, selective proximal tubule injury produced by diphtheria toxin treatment and Kidney Injury Molecule-1 or Notch1 overexpression leads to interstitial inflammation, fibrosis, and CKD126–128; recent studies suggest that tubule–derived wnt and sonic hedgehog ligands, tubule-specific activity of ADAM17 protease, and other pathologies strictly localized to tubules are sufficient to drive interstitial fibrosis 41,58,62,129–133 We note here that such cross-talk between injured tubules, peritubular capillaries, and interstitial cells through locally activated mechanisms has the advantage of circumscribing the fibrotic response and minimizing dissociation of nephron function and vascular perfusion.
The CKD-AKI-CKD Connection: AKI on CKD Can Trigger Hemodynamic Mechanisms of CKD Progression
Hospital-based AKI in patients with prior CKD adversely affects their long-term outcomes (Figure 4); there is incomplete recovery, increased mortality, and predilection for progression to ESRD among survivors.1–6 We modeled this clinical paradigm experimentally by inducing IRI in rats with prior RMR.29 Rats with implanted BP transducers were subjected to IRI 2 weeks after sham surgery, unilateral nephrectomy (moderate RMR), or unilateral nephrectomy with surgical removal of 50% renal mass from the other kidney (severe RMR). BPs recorded by radiotelemetry in conscious rats were normal before IRI in all groups, although slightly higher in rats with severe RMR. Rats in all groups showed equivalently severe azotemia and tubule necrosis 3 days after IRI and similar fractional masses of dedifferentiated regenerating proximal tubules 7 days after IRI. However, 4 weeks after IRI, disproportionately greater fractions of regenerating tubules in the severe RMR group failed to differentiate and became atrophic. Correspondingly, tubules with failed differentiation were surrounded by fibrosis. We surmised that stresses associated with renal hypertrophy after RMR had compromised the ability of regenerating tubules to enter differentiation programs required to regain normal structure. Although the nature of the epithelial defect that prevented redifferentiation remained unknown, it was clear that failed differentiation had given rise to greater atrophic tubule mass and proportionately severe fibrosis. Functional effect of the tubule defect was reflected by incomplete abatement of azotemia 4 weeks after IRI.29
Failed tubule recovery after AKI in rats with severe RMR was attended by hypertension.29 Severe RMR impairs renal blood flow autoregulation.134,135 Severe RMR, impaired blood flow autoregulation, hypertension, and glomerulosclerosis are closely related.134,136 Therefore, we surmised that high systemic arterial pressures in RMR rats recovering poorly from AKI would be transmitted through less responsive arterioles and damage glomeruli. Rats with IRI after severe RMR not only became hypertensive but also proteinuric; in the most hypertensive animals, proteinuria was severe, and glomeruli showed focal/segmental hyalinosis, necrosis, and sclerosis.29 These findings showed that, in a normotensive setting with impaired blood flow autoregulation (caused by RMR), poor recovery from superimposed AKI was sufficient in itself to cause hypertension.29 Rats with severe RMR were not hypertensive before IRI. Without IRI, control rats with severe RMR remained normotensive for 6 weeks.29 Furthermore, the majority of such rats with 75% RMR produced by surgical excision without IRI are known to remain normotensive up to 6 months,137,138 unlike rats with 75% RMR produced by unilateral nephrectomy and partial renal infarction that develop hypertension, vascular damage, and progressively increasing glomerulosclerosis, tubule atrophy, and fibrosis by 16 weeks.135 Even lesser degrees of RMR may predispose for such pathologies in the aftermath of AKI. Uninephrectomized rats (50% RMR) but not rats with intact kidneys (0% RMR) developed hypertension, proteinuria, and glomerulosclerosis over several months after IRI.34,139–141 It is unclear how incomplete tubule healing and fibrosis after AKI in rats with RMR give rise to hypertension. Prior observations suggest that hypertension after AKI may be volume dependent. Kidneys develop microvascular defects after AKI,30,31,33–36,96 a pathology that is particularly severe in kidneys with RMR and superimposed IRI.29 Microvascular injury with reduction of peritubular capillary capacitance after AKI or other tubulointerstitial disease may predispose to impaired pressure natriuresis, reduced capacity of tubules to excrete salt, and volume-dependent hypertension.30,34,36,99,142–146 Notably, even without RMR, rats remain normotensive after IRI, but they become hypertensive after salt loading—unlike normal rats, which remain normotensive despite high salt loads.144 Although additional work is necessary to delineate the pathophysiology of hypertension development after AKI in rats with RMR, there can be no doubt that increased BP bodes poorly for kidneys in such contexts. Patients with CKD with compromised kidney reserve who also undergo AKI are likely to be at risk for long-term deterioration of kidney structure and function through hemodynamic mechanisms if they are also hypertensive. Indeed, it is the most plausible mechanism for progression to ESRD in patients with CKD who experience superimposed AKI. The relationships of preexisting hypertension in cohorts of patients with CKD with additional AKI as well as hypertension development after AKI in such cohorts need investigation.
Summary
In summary, recent studies have provided crucial connections between AKI and CKD in terms of understanding how AKI contributes to the progression of renal disease. AKI by itself is a self-healing process, but if severe, it leaves behind tubule atrophy, interstitial fibrosis, and long-term dysfunction. However, these pathologies cannot and do not progress without additional AKI episodes. However, if AKI is massive or superimposed on CKD with compromised renal reserve, injured tubules heal poorly and cause disproportionately severe scarring with loss of peritubular capillaries, setting in motion a pathophysiology that produces volume–dependent salt–sensitive hypertension. Because hypertension occurs in the setting of impaired renal blood flow autoregulation, increased transmission of arterial pressure damages glomeruli. Serial glomerular damage and consequent tubule atrophy cause progression. On the basis of these considerations, rigorous control of BP and calorie restriction—an approach that also decreases BP—still remain staple strategies to delay CKD progression. However, it is unclear why tubules regenerating after AKI sometimes fail to differentiate, a pathology that instigates fibrosis. Therefore, investigation of the conundrum of failed tubule differentiation after acute injury has the potential to uncover strategies that prevent AKI-CKD transitions, preserve renal mass, and thereby, delay hemodynamically mediated progression.
Disclosures
None.
Acknowledgments
We thank Dr. Robert B. Colvin for providing renal biopsy illustrations of healed post-transplant AKI. Illustrations from experimental models of AKI-CKD transition are from the work by Lan et al.39
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
References
- 1.Hsu CY: Yes, AKI truly leads to CKD. J Am Soc Nephrol 23: 967–969, 2012 [DOI] [PubMed] [Google Scholar]
- 2.Okusa MD, Chertow GM, Portilla D, Acute Kidney Injury Advisory Group of the American Society of Nephrology : The nexus of acute kidney injury, chronic kidney disease, and World Kidney Day 2009. Clin J Am Soc Nephrol 4: 520–522, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chawla LS, Eggers PW, Star RA, Kimmel PL: Acute kidney injury and chronic kidney disease as interconnected syndromes. N Engl J Med 371: 58–66, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Venkatachalam MA, Griffin KA, Lan R, Geng H, Saikumar P, Bidani AK: Acute kidney injury: A springboard for progression in chronic kidney disease. Am J Physiol Renal Physiol 298: F1078–F1094, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bydash JR, Ishani A: Acute kidney injury and chronic kidney disease: A work in progress. Clin J Am Soc Nephrol 6: 2555–2557, 2011 [DOI] [PubMed] [Google Scholar]
- 6.Waikar SS, Winkelmayer WC: Chronic on acute renal failure: Long-term implications of severe acute kidney injury. JAMA 302: 1227–1229, 2009 [DOI] [PubMed] [Google Scholar]
- 7.Finn WF: Recovery from Acute Renal Failure, edited by Lazarus JMBBM, New York, Churchill Livingstone, 1993, pp 553–596 [Google Scholar]
- 8.Price JD, Palmer RA: A functional and morphological follow-up study of acute renal failure. Arch Intern Med 105: 90–98, 1960 [DOI] [PubMed] [Google Scholar]
- 9.Muehrcke RC, Pirani CL: Arsine-induced anuria. A correlative clinicopathological study with electron microscopic observations. Ann Intern Med 68: 853–866, 1968 [DOI] [PubMed] [Google Scholar]
- 10.Lewers DT, Mathew TH, Maher JF, Schreiner GE: Long-term follow-up of renal function and histology after acute tubular necrosis. Ann Intern Med 73: 523–529, 1970 [DOI] [PubMed] [Google Scholar]
- 11.Pasternack A, Tallqvist G, Kuhlbäck B: Occurrence of interstitial nephritis in acute renal failure. Acta Med Scand 187: 27–31, 1970 [DOI] [PubMed] [Google Scholar]
- 12.Levin ML, Simon NM, Herdson PB, del Greco F: Acute renal failure followed by protracted, slowly resolving chronic uremia. J Chronic Dis 25: 645–651, 1972 [DOI] [PubMed] [Google Scholar]
- 13.Wise WJ, Bakir AA, Dunea G: Recovery from acute renal failure after 11 months of hemodialysis. Arch Intern Med 142: 1568–1569, 1982 [PubMed] [Google Scholar]
- 14.Muehrcke RC, Rosen S, Pirani CL, Kark RM: Renal lesions in patients recovering from acute renal failure [Abstract]. J Lab Clin Med 64: 888, 1964 [Google Scholar]
- 15.Gueler F, Gwinner W, Schwarz A, Haller H: Long-term effects of acute ischemia and reperfusion injury. Kidney Int 66: 523–527, 2004 [DOI] [PubMed] [Google Scholar]
- 16.Forbes JM, Hewitson TD, Becker GJ, Jones CL: Ischemic acute renal failure: Long-term histology of cell and matrix changes in the rat. Kidney Int 57: 2375–2385, 2000 [DOI] [PubMed] [Google Scholar]
- 17.Abdulkader RC, Libório AB, Malheiros DM: Histological features of acute tubular necrosis in native kidneys and long-term renal function. Ren Fail 30: 667–673, 2008 [DOI] [PubMed] [Google Scholar]
- 18.Hsu CY: Linking the population epidemiology of acute renal failure, chronic kidney disease and end-stage renal disease. Curr Opin Nephrol Hypertens 16: 221–226, 2007 [DOI] [PubMed] [Google Scholar]
- 19.Ponte B, Felipe C, Muriel A, Tenorio MT, Liaño F: Long-term functional evolution after an acute kidney injury: A 10-year study. Nephrol Dial Transplant 23: 3859–3866, 2008 [DOI] [PubMed] [Google Scholar]
- 20.Snoeijs MG, van Heurn LE, Buurman WA: Biological modulation of renal ischemia-reperfusion injury. Curr Opin Organ Transplant 15: 190–199, 2010 [DOI] [PubMed] [Google Scholar]
- 21.Hostetter TH, Olson JL, Rennke HG, Venkatachalam MA, Brenner BM: Hyperfiltration in remnant nephrons: A potentially adverse response to renal ablation. Am J Physiol 241: F85–F93, 1981 [DOI] [PubMed] [Google Scholar]
- 22.Olson JL, Hostetter TH, Rennke HG, Brenner BM, Venkatachalam MA: Altered glomerular permselectivity and progressive sclerosis following extreme ablation of renal mass. Kidney Int 22: 112–126, 1982 [DOI] [PubMed] [Google Scholar]
- 23.Brenner BM, Meyer TW, Hostetter TH: Dietary protein intake and the progressive nature of kidney disease: The role of hemodynamically mediated glomerular injury in the pathogenesis of progressive glomerular sclerosis in aging, renal ablation, and intrinsic renal disease. N Engl J Med 307: 652–659, 1982 [DOI] [PubMed] [Google Scholar]
- 24.Tapp DC, Wortham WG, Addison JF, Hammonds DN, Barnes JL, Venkatachalam MA: Food restriction retards body growth and prevents end-stage renal pathology in remnant kidneys of rats regardless of protein intake. Lab Invest 60: 184–195, 1989 [PubMed] [Google Scholar]
- 25.Griffin KA, Picken MM, Churchill M, Churchill P, Bidani AK: Functional and structural correlates of glomerulosclerosis after renal mass reduction in the rat. J Am Soc Nephrol 11: 497–506, 2000 [DOI] [PubMed] [Google Scholar]
- 26.Nath KA: Tubulointerstitial changes as a major determinant in the progression of renal damage. Am J Kidney Dis 20: 1–17, 1992 [DOI] [PubMed] [Google Scholar]
- 27.Kriz W, LeHir M: Pathways to nephron loss starting from glomerular diseases-insights from animal models. Kidney Int 67: 404–419, 2005 [DOI] [PubMed] [Google Scholar]
- 28.Kaissling B, Lehir M, Kriz W: Renal epithelial injury and fibrosis. Biochim Biophys Acta 1832: 931–939, 2013 [DOI] [PubMed] [Google Scholar]
- 29.Polichnowski AJ, Lan R, Geng H, Griffin KA, Venkatachalam MA, Bidani AK: Severe renal mass reduction impairs recovery and promotes fibrosis after AKI. J Am Soc Nephrol 25: 1496–1507, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Basile DP: Rarefaction of peritubular capillaries following ischemic acute renal failure: A potential factor predisposing to progressive nephropathy. Curr Opin Nephrol Hypertens 13: 1–7, 2004 [DOI] [PubMed] [Google Scholar]
- 31.Basile DP: The endothelial cell in ischemic acute kidney injury: Implications for acute and chronic function. Kidney Int 72: 151–156, 2007 [DOI] [PubMed] [Google Scholar]
- 32.Basile DP, Leonard EC, Beal AG, Schleuter D, Friedrich J: Persistent oxidative stress following renal ischemia-reperfusion injury increases ANG II hemodynamic and fibrotic activity. Am J Physiol Renal Physiol 302: F1494–F1502, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Basile DP, Donohoe D, Roethe K, Osborn JL: Renal ischemic injury results in permanent damage to peritubular capillaries and influences long-term function. Am J Physiol Renal Physiol 281: F887–F899, 2001 [DOI] [PubMed] [Google Scholar]
- 34.Basile DP, Donohoe DL, Roethe K, Mattson DL: Chronic renal hypoxia after acute ischemic injury: Effects of L-arginine on hypoxia and secondary damage. Am J Physiol Renal Physiol 284: F338–F348, 2003 [DOI] [PubMed] [Google Scholar]
- 35.Basile DP, Friedrich JL, Spahic J, Knipe N, Mang H, Leonard EC, Changizi-Ashtiyani S, Bacallao RL, Molitoris BA, Sutton TA: Impaired endothelial proliferation and mesenchymal transition contribute to vascular rarefaction following acute kidney injury. Am J Physiol Renal Physiol 300: F721–F733, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Basile DP, Anderson MD, Sutton TA: Pathophysiology of acute kidney injury. Compr Physiol 2: 1303–1353, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lin SL, Chang FC, Schrimpf C, Chen YT, Wu CF, Wu VC, Chiang WC, Kuhnert F, Kuo CJ, Chen YM, Wu KD, Tsai TJ, Duffield JS: Targeting endothelium-pericyte cross talk by inhibiting VEGF receptor signaling attenuates kidney microvascular rarefaction and fibrosis. Am J Pathol 178: 911–923, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kramann R, Tanaka M, Humphreys BD: Fluorescence microangiography for quantitative assessment of peritubular capillary changes after AKI in mice. J Am Soc Nephrol 25: 1924–1931, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lan R, Geng H, Polichnowski AJ, Singha PK, Saikumar P, McEwen DG, Griffin KA, Koesters R, Weinberg JM, Bidani AK, Kriz W, Venkatachalam MA: PTEN loss defines a TGF-β-induced tubule phenotype of failed differentiation and JNK signaling during renal fibrosis. Am J Physiol Renal Physiol 302: F1210–F1223, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Goldfarb M, Rosenberger C, Abassi Z, Shina A, Zilbersat F, Eckardt KU, Rosen S, Heyman SN: Acute-on-chronic renal failure in the rat: Functional compensation and hypoxia tolerance. Am J Nephrol 26: 22–33, 2006 [DOI] [PubMed] [Google Scholar]
- 41.Yang L, Besschetnova TY, Brooks CR, Shah JV, Bonventre JV: Epithelial cell cycle arrest in G2/M mediates kidney fibrosis after injury. Nat Med 16: 535–543, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nath KA, Croatt AJ, Haggard JJ, Grande JP: Renal response to repetitive exposure to heme proteins: Chronic injury induced by an acute insult. Kidney Int 57: 2423–2433, 2000 [DOI] [PubMed] [Google Scholar]
- 43.Duffield JS: Cellular and molecular mechanisms in kidney fibrosis. J Clin Invest 124: 2299–2306, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Humphreys BD, Lin SL, Kobayashi A, Hudson TE, Nowlin BT, Bonventre JV, Valerius MT, McMahon AP, Duffield JS: Fate tracing reveals the pericyte and not epithelial origin of myofibroblasts in kidney fibrosis. Am J Pathol 176: 85–97, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Picard N, Baum O, Vogetseder A, Kaissling B, Le Hir M: Origin of renal myofibroblasts in the model of unilateral ureter obstruction in the rat. Histochem Cell Biol 130: 141–155, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kriz W, Kaissling B, Le Hir M: Epithelial-mesenchymal transition (EMT) in kidney fibrosis: Fact or fantasy? J Clin Invest 121: 468–474, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kaissling B, Le Hir M: The renal cortical interstitium: Morphological and functional aspects. Histochem Cell Biol 130: 247–262, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Campanholle G, Ligresti G, Gharib SA, Duffield JS: Cellular mechanisms of tissue fibrosis. 3. Novel mechanisms of kidney fibrosis. Am J Physiol Cell Physiol 304: C591–C603, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kida Y, Ieronimakis N, Schrimpf C, Reyes M, Duffield JS: EphrinB2 reverse signaling protects against capillary rarefaction and fibrosis after kidney injury. J Am Soc Nephrol 24: 559–572, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dimke H, Sparks MA, Thomson BR, Frische S, Coffman TM, Quaggin SE: Tubulovascular cross-talk by vascular endothelial growth factor A maintains peritubular microvasculature in kidney [published online ahead of print November 10, 2014]. J Am Soc Nephrol doi:ASN.2014010060 [DOI] [PMC free article] [PubMed]
- 51.Fligny C, Duffield JS: Activation of pericytes: Recent insights into kidney fibrosis and microvascular rarefaction. Curr Opin Rheumatol 25: 78–86, 2013 [DOI] [PubMed] [Google Scholar]
- 52.Chen YT, Chang FC, Wu CF, Chou YH, Hsu HL, Chiang WC, Shen J, Chen YM, Wu KD, Tsai TJ, Duffield JS, Lin SL: Platelet-derived growth factor receptor signaling activates pericyte-myofibroblast transition in obstructive and post-ischemic kidney fibrosis. Kidney Int 80: 1170–1181, 2011 [DOI] [PubMed] [Google Scholar]
- 53.Schrimpf C, Xin C, Campanholle G, Gill SE, Stallcup W, Lin SL, Davis GE, Gharib SA, Humphreys BD, Duffield JS: Pericyte TIMP3 and ADAMTS1 modulate vascular stability after kidney injury. J Am Soc Nephrol 23: 868–883, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wu CF, Chiang WC, Lai CF, Chang FC, Chen YT, Chou YH, Wu TH, Linn GR, Ling H, Wu KD, Tsai TJ, Chen YM, Duffield JS, Lin SL: Transforming growth factor β-1 stimulates profibrotic epithelial signaling to activate pericyte-myofibroblast transition in obstructive kidney fibrosis. Am J Pathol 182: 118–131, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ren S, Johnson BG, Kida Y, Ip C, Davidson KC, Lin SL, Kobayashi A, Lang RA, Hadjantonakis AK, Moon RT, Duffield JS: LRP-6 is a coreceptor for multiple fibrogenic signaling pathways in pericytes and myofibroblasts that are inhibited by DKK-1. Proc Natl Acad Sci U S A 110: 1440–1445, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chau BN, Xin C, Hartner J, Ren S, Castano AP, Linn G, Li J, Tran PT, Kaimal V, Huang X, Chang AN, Li S, Kalra A, Grafals M, Portilla D, MacKenna DA, Orkin SH, Duffield JS: MicroRNA-21 promotes fibrosis of the kidney by silencing metabolic pathways. Sci Transl Med 4: 121ra18, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Li S, Mariappan N, Megyesi J, Shank B, Kannan K, Theus S, Price PM, Duffield JS, Portilla D: Proximal tubule PPARα attenuates renal fibrosis and inflammation caused by unilateral ureteral obstruction. Am J Physiol Renal Physiol 305: F618–F627, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Maarouf OH, Ikeda Y, Humphreys BD: Wnt signaling in kidney tubulointerstitium during disease. Histol Histopathol 30: 163–171, 2015 [DOI] [PubMed] [Google Scholar]
- 59.Kramann R, Humphreys BD: Kidney pericytes: Roles in regeneration and fibrosis. Semin Nephrol 34: 374–383, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.DiRocco DP, Kobayashi A, Taketo MM, McMahon AP, Humphreys BD: Wnt4/β-catenin signaling in medullary kidney myofibroblasts. J Am Soc Nephrol 24: 1399–1412, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fabian SL, Penchev RR, St-Jacques B, Rao AN, Sipilä P, West KA, McMahon AP, Humphreys BD: Hedgehog-Gli pathway activation during kidney fibrosis. Am J Pathol 180: 1441–1453, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhou D, Li Y, Zhou L, Tan RJ, Xiao L, Liang M, Hou FF, Liu Y: Sonic hedgehog is a novel tubule-derived growth factor for interstitial fibroblasts after kidney injury. J Am Soc Nephrol 25: 2187–2200, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Barnes JL, Gorin Y: Myofibroblast differentiation during fibrosis: Role of NAD(P)H oxidases. Kidney Int 79: 944–956, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Castaño AP, Lin S-L, Surowy T, Nowlin BT, Turlapati SA, Patel T, Singh A, Li S, Lupher ML, Duffield JS: Serum amyloid P inhibits fibrosis through FcgR-dependent monocyte-macrophage regulation in vivo, science translational medicine. Sci Transl Med 1: 5ra13, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Huen SC, Cantley LG: Macrophage-mediated injury and repair after ischemic kidney injury. Pediatr Nephrol 30: 199–209, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Barnes JL, Glass WF, 2nd: Renal interstitial fibrosis: A critical evaluation of the origin of myofibroblasts. Contrib Nephrol 169: 73–93, 2011 [DOI] [PubMed] [Google Scholar]
- 67.Broekema M, Harmsen MC, van Luyn MJ, Koerts JA, Petersen AH, van Kooten TG, van Goor H, Navis G, Popa ER: Bone marrow-derived myofibroblasts contribute to the renal interstitial myofibroblast population and produce procollagen I after ischemia/reperfusion in rats. J Am Soc Nephrol 18: 165–175, 2007 [DOI] [PubMed] [Google Scholar]
- 68.LeBleu VS, Taduri G, O’Connell J, Teng Y, Cooke VG, Woda C, Sugimoto H, Kalluri R: Origin and function of myofibroblasts in kidney fibrosis. Nat Med 19: 1047–1053, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Grotendorst GR: Connective tissue growth factor: A mediator of TGF-beta action on fibroblasts. Cytokine Growth Factor Rev 8: 171–179, 1997 [DOI] [PubMed] [Google Scholar]
- 70.Battegay EJ, Raines EW, Seifert RA, Bowen-Pope DF, Ross R: TGF-beta induces bimodal proliferation of connective tissue cells via complex control of an autocrine PDGF loop. Cell 63: 515–524, 1990 [DOI] [PubMed] [Google Scholar]
- 71.Moses HL, Coffey RJ, Jr., Leof EB, Lyons RM, Keski-Oja J: Transforming growth factor beta regulation of cell proliferation. J Cell Physiol Suppl 5: 1–7, 1987 [DOI] [PubMed] [Google Scholar]
- 72.Wang X, Willenbring H, Akkari Y, Torimaru Y, Foster M, Al-Dhalimy M, Lagasse E, Finegold M, Olson S, Grompe M: Cell fusion is the principal source of bone-marrow-derived hepatocytes. Nature 422: 897–901, 2003 [DOI] [PubMed] [Google Scholar]
- 73.Vassilopoulos G, Wang PR, Russell DW: Transplanted bone marrow regenerates liver by cell fusion. Nature 422: 901–904, 2003 [DOI] [PubMed] [Google Scholar]
- 74.Medvinsky A, Smith A: Stem cells: Fusion brings down barriers. Nature 422: 823–825, 2003 [DOI] [PubMed] [Google Scholar]
- 75.Ludin A, Itkin T, Gur-Cohen S, Mildner A, Shezen E, Golan K, Kollet O, Kalinkovich A, Porat Z, D’Uva G, Schajnovitz A, Voronov E, Brenner DA, Apte RN, Jung S, Lapidot T: Monocytes-macrophages that express α-smooth muscle actin preserve primitive hematopoietic cells in the bone marrow. Nat Immunol 13: 1072–1082, 2012 [DOI] [PubMed] [Google Scholar]
- 76.Yokota T, Kawakami Y, Nagai Y, Ma JX, Tsai JY, Kincade PW, Sato S: Bone marrow lacks a transplantable progenitor for smooth muscle type alpha-actin-expressing cells. Stem Cells 24: 13–22, 2006 [DOI] [PubMed] [Google Scholar]
- 77.Duffield JS, Park KM, Hsiao LL, Kelley VR, Scadden DT, Ichimura T, Bonventre JV: Restoration of tubular epithelial cells during repair of the postischemic kidney occurs independently of bone marrow-derived stem cells. J Clin Invest 115: 1743–1755, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gomez IG, Duffield JS: The FOXD1 lineage of kidney perivascular cells and myofibroblasts: Functions and responses to injury. Kidney Int Suppl 4: 26–33, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bucala R, Spiegel LA, Chesney J, Hogan M, Cerami A: Circulating fibrocytes define a new leukocyte subpopulation that mediates tissue repair. Mol Med 1: 71–81, 1994 [PMC free article] [PubMed] [Google Scholar]
- 80.Reich B, Schmidbauer K, Rodriguez Gomez M, Johannes Hermann F, Göbel N, Brühl H, Ketelsen I, Talke Y, Mack M: Fibrocytes develop outside the kidney but contribute to renal fibrosis in a mouse model. Kidney Int 84: 78–89, 2013 [DOI] [PubMed] [Google Scholar]
- 81.Zeisberg EM, Potenta SE, Sugimoto H, Zeisberg M, Kalluri R: Fibroblasts in kidney fibrosis emerge via endothelial-to-mesenchymal transition. J Am Soc Nephrol 19: 2282–2287, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bonventre JV, Yang L: Cellular pathophysiology of ischemic acute kidney injury. J Clin Invest 121: 4210–4221, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kwon O, Hong SM, Sutton TA, Temm CJ: Preservation of peritubular capillary endothelial integrity and increasing pericytes may be critical to recovery from postischemic acute kidney injury. Am J Physiol Renal Physiol 295: F351–F359, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Schrier RW, Wang W: Acute renal failure and sepsis. N Engl J Med 351: 159–169, 2004 [DOI] [PubMed] [Google Scholar]
- 85.Sutton TA, Fisher CJ, Molitoris BA: Microvascular endothelial injury and dysfunction during ischemic acute renal failure. Kidney Int 62: 1539–1549, 2002 [DOI] [PubMed] [Google Scholar]
- 86.Brezis M, Rosen S: Hypoxia of the renal medulla—its implications for disease. N Engl J Med 332: 647–655, 1995 [DOI] [PubMed] [Google Scholar]
- 87.Mason J, Torhorst J, Welsch J: Role of the medullary perfusion defect in the pathogenesis of ischemic renal failure. Kidney Int 26: 283–293, 1984 [DOI] [PubMed] [Google Scholar]
- 88.Conger J: Hemodynamic factors in acute renal failure. Adv Ren Replace Ther 4[Suppl 1]: 25–37, 1997 [PubMed] [Google Scholar]
- 89.Yamamoto K, Wilson DR, Baumal R: Outer medullary circulatory defect in ischemic acute renal failure. Am J Pathol 116: 253–261, 1984 [PMC free article] [PubMed] [Google Scholar]
- 90.Flores J, DiBona DR, Beck CH, Leaf A: The role of cell swelling in ischemic renal damage and the protective effect of hypertonic solute. J Clin Invest 51: 118–126, 1972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Laubach VE, French BA, Okusa MD: Targeting of adenosine receptors in ischemia-reperfusion injury. Expert Opin Ther Targets 15: 103–118, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Timsit MO, García-Cardeña G: Flow-dependent endothelial function and kidney dysfunction. Semin Nephrol 32: 185–191, 2012 [DOI] [PubMed] [Google Scholar]
- 93.Franklin WA, Ganote CE, Jennings RB: Blood reflow after renal ischemia. Effects of hypertonic mannitol on reflow and tubular necrosis after transient ischemia in the rat. Arch Pathol 98: 106–111, 1974 [PubMed] [Google Scholar]
- 94.Summers WK, Jamison RL: The no reflow phenomenon in renal ischemia. Lab Invest 25: 635–643, 1971 [PubMed] [Google Scholar]
- 95.Molitoris BA, Sutton TA: Endothelial injury and dysfunction: Role in the extension phase of acute renal failure. Kidney Int 66: 496–499, 2004 [DOI] [PubMed] [Google Scholar]
- 96.Yuan HT, Li XZ, Pitera JE, Long DA, Woolf AS: Peritubular capillary loss after mouse acute nephrotoxicity correlates with down-regulation of vascular endothelial growth factor-A and hypoxia-inducible factor-1 alpha. Am J Pathol 163: 2289–2301, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Basile DP, Fredrich K, Chelladurai B, Leonard EC, Parrish AR: Renal ischemia reperfusion inhibits VEGF expression and induces ADAMTS-1, a novel VEGF inhibitor. Am J Physiol Renal Physiol 294: F928–F936, 2008 [DOI] [PubMed] [Google Scholar]
- 98.Hakroush S, Moeller MJ, Theilig F, Kaissling B, Sijmonsma TP, Jugold M, Akeson AL, Traykova-Brauch M, Hosser H, Hähnel B, Gröne HJ, Koesters R, Kriz W: Effects of increased renal tubular vascular endothelial growth factor (VEGF) on fibrosis, cyst formation, and glomerular disease. Am J Pathol 175: 1883–1895, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Leonard EC, Friedrich JL, Basile DP: VEGF-121 preserves renal microvessel structure and ameliorates secondary renal disease following acute kidney injury. Am J Physiol Renal Physiol 295: F1648–F1657, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Haase VH: Mechanisms of hypoxia responses in renal tissue. J Am Soc Nephrol 24: 537–541, 2013 [DOI] [PubMed] [Google Scholar]
- 101.Tanaka S, Tanaka T, Nangaku M: Hypoxia as a key player in the AKI-to-CKD transition. Am J Physiol Renal Physiol 307: F1187–F1195, 2014 [DOI] [PubMed] [Google Scholar]
- 102.Whitehouse T, Stotz M, Taylor V, Stidwill R, Singer M: Tissue oxygen and hemodynamics in renal medulla, cortex, and corticomedullary junction during hemorrhage-reperfusion. Am J Physiol Renal Physiol 291: F647–F653, 2006 [DOI] [PubMed] [Google Scholar]
- 103.Gnaiger E, Lassnig B, Kuznetsov A, Rieger G, Margreiter R: Mitochondrial oxygen affinity, respiratory flux control and excess capacity of cytochrome c oxidase. J Exp Biol 201: 1129–1139, 1998 [DOI] [PubMed] [Google Scholar]
- 104.Gnaiger E, Steinlechner-Maran R, Méndez G, Eberl T, Margreiter R: Control of mitochondrial and cellular respiration by oxygen. J Bioenerg Biomembr 27: 583–596, 1995 [DOI] [PubMed] [Google Scholar]
- 105.Abdelkader A, Ho J, Ow CP, Eppel GA, Rajapakse NW, Schlaich MP, Evans RG: Renal oxygenation in acute renal ischemia-reperfusion injury. Am J Physiol Renal Physiol 306: F1026–F1038, 2014 [DOI] [PubMed] [Google Scholar]
- 106.Koritzinsky M, Magagnin MG, van den Beucken T, Seigneuric R, Savelkouls K, Dostie J, Pyronnet S, Kaufman RJ, Weppler SA, Voncken JW, Lambin P, Koumenis C, Sonenberg N, Wouters BG: Gene expression during acute and prolonged hypoxia is regulated by distinct mechanisms of translational control. EMBO J 25: 1114–1125, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.van den Beucken T, Koritzinsky M, Wouters BG: Translational control of gene expression during hypoxia. Cancer Biol Ther 5: 749–755, 2006 [DOI] [PubMed] [Google Scholar]
- 108.Hammond EM, Kaufmann MR, Giaccia AJ: Oxygen sensing and the DNA-damage response. Curr Opin Cell Biol 19: 680–684, 2007 [DOI] [PubMed] [Google Scholar]
- 109.Hamanaka RB, Chandel NS: Mitochondrial reactive oxygen species regulate hypoxic signaling. Curr Opin Cell Biol 21: 894–899, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Geng H, Lan R, Wang G, Siddiqi AR, Naski MC, Brooks AI, Barnes JL, Saikumar P, Weinberg JM, Venkatachalam MA: Inhibition of autoregulated TGFbeta signaling simultaneously enhances proliferation and differentiation of kidney epithelium and promotes repair following renal ischemia. Am J Pathol 174: 1291–1308, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Spurgeon KR, Donohoe DL, Basile DP: Transforming growth factor-beta in acute renal failure: Receptor expression, effects on proliferation, cellularity, and vascularization after recovery from injury. Am J Physiol Renal Physiol 288: F568–F577, 2005 [DOI] [PubMed] [Google Scholar]
- 112.Haase VH: Pathophysiological Consequences of HIF Activation: HIF as a modulator of fibrosis. Ann N Y Acad Sci 1177: 57–65, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Venkatachalam MA, Bernard DB, Donohoe JF, Levinsky NG: Ischemic damage and repair in the rat proximal tubule: Differences among the S1, S2, and S3 segments. Kidney Int 14: 31–49, 1978 [DOI] [PubMed] [Google Scholar]
- 114.Heyman SN, Khamaisi M, Rosen S, Rosenberger C: Renal parenchymal hypoxia, hypoxia response and the progression of chronic kidney disease. Am J Nephrol 28: 998–1006, 2008 [DOI] [PubMed] [Google Scholar]
- 115.Heyman SN, Rosenberger C, Rosen S: Experimental ischemia-reperfusion: Biases and myths-the proximal vs. distal hypoxic tubular injury debate revisited. Kidney Int 77: 9–16, 2010 [DOI] [PubMed] [Google Scholar]
- 116.Mason J, Welsch J, Torhorst J: The contribution of vascular obstruction to the functional defect that follows renal ischemia. Kidney Int 31: 65–71, 1987 [DOI] [PubMed] [Google Scholar]
- 117.Schurek HJ, Kriz W: Morphologic and functional evidence for oxygen deficiency in the isolated perfused rat kidney. Lab Invest 53: 145–155, 1985 [PubMed] [Google Scholar]
- 118.Geng H, Lan R, Singha PK, Gilchrist A, Weinreb PH, Violette SM, Weinberg JM, Saikumar P, Venkatachalam MA: Lysophosphatidic acid increases proximal tubule cell secretion of profibrotic cytokines PDGF-B and CTGF through LPA2- and Gαq-mediated Rho and αvβ6 integrin-dependent activation of TGF-β. Am J Pathol 181: 1236–1249, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Suzuki T, Kimura M, Asano M, Fujigaki Y, Hishida A: Role of atrophic tubules in development of interstitial fibrosis in microembolism-induced renal failure in rat. Am J Pathol 158: 75–85, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Bonventre JV: Dedifferentiation and proliferation of surviving epithelial cells in acute renal failure. J Am Soc Nephrol 14[Suppl 1]: S55–S61, 2003 [DOI] [PubMed] [Google Scholar]
- 121.Bonventre JV: Pathophysiology of AKI: Injury and normal and abnormal repair. Contrib Nephrol 165: 9–17, 2010 [DOI] [PubMed] [Google Scholar]
- 122.Bonventre JV, Zuk A: Ischemic acute renal failure: An inflammatory disease? Kidney Int 66: 480–485, 2004 [DOI] [PubMed] [Google Scholar]
- 123.Geng H, Lan R, Singha PK, Saikumar P, Weinberg JM, Venkatachalam MA: Lysophosphatidic acid (LPA) transactivates epidermal growth factor receptors (EGFR) via LPAR1/Gαi/o signaling to potentiate LPAR2/Gαq/αvβ6 integrin dependent TGFβ signaling and increase the production of PDGF-B and CTGF by proximal tubule (PT) cells [Abstract]. J Am Soc Nephrol 24: 15A, 2013 [Google Scholar]
- 124.Fujigaki Y, Muranaka Y, Sun D, Goto T, Zhou H, Sakakima M, Fukasawa H, Yonemura K, Yamamoto T, Hishida A: Transient myofibroblast differentiation of interstitial fibroblastic cells relevant to tubular dilatation in uranyl acetate-induced acute renal failure in rats. Virchows Arch 446: 164–176, 2005 [DOI] [PubMed] [Google Scholar]
- 125.Zager RA, Johnson AC, Naito M, Bomsztyk K: Maleate nephrotoxicity: Mechanisms of injury and correlates with ischemic/hypoxic tubular cell death. Am J Physiol Renal Physiol 294: F187–F197, 2008 [DOI] [PubMed] [Google Scholar]
- 126.Grgic I, Campanholle G, Bijol V, Wang C, Sabbisetti VS, Ichimura T, Humphreys BD, Bonventre JV: Targeted proximal tubule injury triggers interstitial fibrosis and glomerulosclerosis. Kidney Int 82: 172–183, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Humphreys BD, Xu F, Sabbisetti V, Grgic I, Naini SM, Wang N, Chen G, Xiao S, Patel D, Henderson JM, Ichimura T, Mou S, Soeung S, McMahon AP, Kuchroo VK, Bonventre JV: Chronic epithelial kidney injury molecule-1 expression causes murine kidney fibrosis. J Clin Invest 123: 4023–4035, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Bielesz B, Sirin Y, Si H, Niranjan T, Gruenwald A, Ahn S, Kato H, Pullman J, Gessler M, Haase VH, Susztak K: Epithelial Notch signaling regulates interstitial fibrosis development in the kidneys of mice and humans. J Clin Invest 120: 4040–4054, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Maarouf OH, Rangarajan D, Welborn J, Humphreys BD: Epithelial-derived Wnt ligand drives interstitial fibrosis through paracrine signaling [Abstract]. J Am Soc Nephrol 25: 76A, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Kefalogianni E, Kaeppler JR, Muthu ML, Humphreys BD, Bonventre JV, Herrlich A: ADAM17 promotes kidney fibrosis after severe ischemia-reperfusion injury [Abstract]. J Am Soc Nephrol 25: 6A-7A, 2014 [Google Scholar]
- 131.Zhou D, Tan RJ, Fu H, Xiao L, Liu Y: Tubule-derived Wnts are indispensable for fibroblast activation and kidney fibrosis [Abstract]. J Am Soc Nephrol 25: 76A, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kang HM, Ahn SH, Choi P, Ko YA, Han SH, Chinga F, Park AS, Tao J, Sharma K, Pullman J, Bottinger EP, Goldberg IJ, Susztak K: Defective fatty acid oxidation in renal tubular epithelial cells has a key role in kidney fibrosis development. Nat Med 21: 37–46, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Matsui K, Kamijo-Ikemorif A, Sugaya T, Yasuda T, Kimura K: Renal liver-type fatty acid binding protein (L-FABP) attenuates acute kidney injury in aristolochic acid nephrotoxicity. Am J Pathol 178: 1021–1032, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Bidani AK, Griffin KA: Long-term renal consequences of hypertension for normal and diseased kidneys. Curr Opin Nephrol Hypertens 11: 73–80, 2002 [DOI] [PubMed] [Google Scholar]
- 135.Griffin KA, Picken M, Bidani AK: Method of renal mass reduction is a critical modulator of subsequent hypertension and glomerular injury. J Am Soc Nephrol 4: 2023–2031, 1994 [DOI] [PubMed] [Google Scholar]
- 136.Griffin KA, Bidani AK: Hypertensive renal damage: Insights from animal models and clinical relevance. Curr Hypertens Rep 6: 145–153, 2004 [DOI] [PubMed] [Google Scholar]
- 137.Griffin KA, Picken MM, Bidani AK: Blood pressure lability and glomerulosclerosis after normotensive 5/6 renal mass reduction in the rat. Kidney Int 65: 209–218, 2004 [DOI] [PubMed] [Google Scholar]
- 138.Griffin KA, Polichnowski A, Licea-vargas H, Picken MM, Lan R, Venkatachalam MA, Bidani AK, Rosenberger C: Progression of renal injury after normotensive renal mass reductin (RMR): Relationship to BP parameters over 6 months [Abstract]. J Am Soc Nephrol 23: 469A, 2012 [Google Scholar]
- 139.Pagtalunan ME, Olson JL, Tilney NL, Meyer TW: Late consequences of acute ischemic injury to a solitary kidney. J Am Soc Nephrol 10: 366–373, 1999 [DOI] [PubMed] [Google Scholar]
- 140.Pagtalunan ME, Olson JL, Meyer TW: Contribution of angiotensin II to late renal injury after acute ischemia. J Am Soc Nephrol 11: 1278–1286, 2000 [DOI] [PubMed] [Google Scholar]
- 141.Cruzado JM, Torras J, Riera M, Herrero I, Hueso M, Espinosa L, Condom E, Lloberas N, Bover J, Alsina J, Grinyó JM: Influence of nephron mass in development of chronic renal failure after prolonged warm renal ischemia. Am J Physiol Renal Physiol 279: F259–F269, 2000 [DOI] [PubMed] [Google Scholar]
- 142.Johnson RJ, Schreiner GF: Hypothesis: The role of acquired tubulointerstitial disease in the pathogenesis of salt-dependent hypertension. Kidney Int 52: 1169–1179, 1997 [DOI] [PubMed] [Google Scholar]
- 143.Johnson RJ, Herrera-Acosta J, Schreiner GF, Rodriguez-Iturbe B: Subtle acquired renal injury as a mechanism of salt-sensitive hypertension. N Engl J Med 346: 913–923, 2002 [DOI] [PubMed] [Google Scholar]
- 144.Pechman KR, Basile DP, Lund H, Mattson DL: Immune suppression blocks sodium-sensitive hypertension following recovery from ischemic acute renal failure. Am J Physiol Regul Integr Comp Physiol 294: R1234–R1239, 2008 [DOI] [PubMed] [Google Scholar]
- 145.Spurgeon-Pechman KR, Donohoe DL, Mattson DL, Lund H, James L, Basile DP: Recovery from acute renal failure predisposes hypertension and secondary renal disease in response to elevated sodium. Am J Physiol Renal Physiol 293: F269–F278, 2007 [DOI] [PubMed] [Google Scholar]
- 146.Pechman KR, De Miguel C, Lund H, Leonard EC, Basile DP, Mattson DL: Recovery from renal ischemia-reperfusion injury is associated with altered renal hemodynamics, blunted pressure natriuresis, and sodium-sensitive hypertension. Am J Physiol Regul Integr Comp Physiol 297: R1358–R1363, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]