Abstract
Objective
Released prisoners have high suicide rates compared with the general population, but little is known about risk factors and possible causal pathways. We conducted a population-based cohort study to investigate rates and risk factors for suicide in people previously imprisoned.
Methods
We identified individuals released from prison in Sweden between January 1, 2005 and December 31, 2009 through linkage of national population-based registers. Released prisoners were followed from the day of release until death, emigration, new incarceration, or December 31, 2009. Survival analyses were conducted to compare incidence rates and psychiatric morbidity with non-convicted population controls matched on gender and year of birth.
Results
We identified 38,995 releases among 26,953 prisoners (7.6% females) during 2005-2009. Overall, 127 suicides occurred, accounting for 14% of all deaths after release (n=920). The mean suicide rate was 204 per 100,000 person years yielding an incidence rate ratio of 18.2 (95% CI 13.9-23.8) compared with general population controls. Previous substance use disorder (Hazard Ratio [HR]=2.1, 1.4-3.2), suicide attempt (HR=2.5, 1.7-3.7), and being born in Sweden vs. abroad (HR=2.1, 1.2-3.6) were independent risk factors for suicide after release.
Conclusions
Released prisoners are at high suicide risk and with a slightly different pattern of psychiatric risk factors for suicide compared with the general population. Results suggest appropriate allocation of resources to facilitate transition to life outside prison and increased attention to prisoners with both a previous suicide attempt and substance use disorder.
Keywords: Suicide, Risk factors, Ex-prisoners
Introduction
Although 10 million people are currently held in prison worldwide [1], considerably larger numbers of ex-prisoners are living in society [2]. Since most prison sentences are short, the annual prevalence of people imprisoned is 2-3 times the total number of prisoners at any one time-point. Rates of suicide within prison are high [3], as are mortality rates from all causes after release [4]. Psychiatric disorders, especially affective, psychotic, and personality disorders, are well-known risk factors for suicide in the general population [5-7]. Further, psychosis and depression are consistently overrepresented among prisoners [8], and substance use disorders are highly prevalent upon arrival to prison [9]. A systematic review of suicide in prison [10] suggested that current psychiatric disorder or alcohol problems were associated with completed suicide; this was also shown in ex-prisoners [11, 12]. However, previous research on psychiatric risk factors has been limited by incomplete information on psychiatric morbidity, follow-up time no longer than one year, and has not investigated personality disorders.
A recent systematic review of suicide after release from prison [13] found that all existing studies reported standardized mortality ratios (SMRs) above 1, varying between 3 and 6 in England and Wales [14], the US [15], Australia [11] and the Netherlands [16]. Two of these studies demonstrated particularly high suicide rates during the first weeks after release, suggesting that this is a high-risk period [11, 17]. Hence, suicide in recently released prisoners has become a part of national suicide prevention strategies in many countries. For example, England’s 2012 National Suicide Prevention strategy targets high-risk groups, and specifically mentions recently released prisoners [3].
More than 10 000 persons (7 % women) started serving their prison sentences in Sweden each year during 2005-2009 [18]. The prison population rate in Sweden is 78 per 100 000 of the national population [1]. This is similar to other Scandinavian countries, but lower than both the world average (148) and that in Australia (133), Netherlands (94), England and Wales (153), and the US (743) where previous studies of suicides in released prisoners have been conducted [11, 14-16]. Previous studies show that a lifetime history of self-harm is prevalent among Swedish prisoners (reported by 17.9%, [19]) and that the suicide rates inside Swedish prisons are similar to other Scandinavian countries [3]. Further, suicide rates have been shown to be elevated among Swedish ex-prisoners with substance use problems [20]. However, no previous studies have investigated suicide rates and risk factors after release from prison on a population-based level in Sweden or in any other country with similar incarceration rates.
Based on current uncertainties in the literature, we addressed three main questions:
-
1)
Are the first 28 days after release the period of highest risk for suicide after release from prison?
-
2)
What psychiatric risk factors are linked to suicide after release from prison?
-
3)
Is there a difference in risk factors for suicide between released prisoners and general population individuals?
Methods
Study design
By linking longitudinal national registers, we conducted a cohort study including all releases from prison in Sweden between the January 1, 2005 and the December 31, 2009. People released from remand prisons (which house prisoners awaiting trial) without a subsequent conviction to imprisonment were excluded. The cohort was followed from the day of release until death, emigration, new incarceration or end of the study period (December 31, 2009). The focus in this design was on time after release, so that a unique person could reappear in the cohort (be released) several times during the study period.
To be able to compare prevalence of psychiatric morbidity and to calculate incidence rate ratios, we used a control group. Each released prisoner in the cohort was matched on gender and year of birth with ten general population controls, who had never been convicted to imprisonment, by the date of the corresponding cohort member’s release (labelled index date). If a control individual was convicted to a prison sentence during the study period, that person ceased to be a control, and - if released within the study period - reappeared as a member of the studied cohort.
Sources of data
Using personal identification numbers as key, we linked several nationwide population-based registries in Sweden. The studied outcome was suicide and the information about causes of death was obtained from the Cause of Death Register, held by the National Board of Health and Welfare. To avoid underestimation of suicide rates [21], and consistent with recent suicide research in prisoners and other contexts [22-25], we included both certain suicide and unnatural death with undetermined intent (ICD 8-9: E950-9, E980-9; ICD 10: X60-84, Y10-34) in our definition of suicide.
The Prison Register (PR, held by the Prison and Probation Services), provided data on exact dates of release from prison between January 1, 2005 and December 31, 2009. To avoid selection bias, the inclusion period was limited to five years since Swedish law requires that individual data should be removed from the PR if no new criminal convictions involving prison and probation have occurred within this period.
Through the National Crime Register (1973-, held by the National Council of Crime Prevention), we obtained information about previous prison sentences. Information about psychiatric (including abuse or dependence) disorders was obtained from the National Patient Register (National Board of Health and Welfare), including all psychiatric hospitalizations since 1973, and outpatient, non-GP physician specialist diagnoses since 2001. The diagnostic categories used were psychotic disorder (ICD 8: 295, 297, 298.2-9, 299; ICD 9: 295, 297, 298.2-9; ICD 10: F20-29), affective disorder (ICD 8: 296.0-3, 296.8-9, 298.0-1, 300.4, 301.1; ICD 9: 296.0-9, 298.0-1, 300.4, 311; ICD 10: F30-33), personality disorder (ICD 8: 301.1-9; ICD 9: 301.0, 301.2-9; ICD 10: F60-61), substance use disorder (ICD 8: 291, 303, 304; ICD 9: 291, 292, 303, 304, 305.0-9; ICD 10: F10-19), any psychiatric disorder (ICD 8: 290-315; ICD 9: 290-319; ICD 10: F00-F99) and any psychiatric disorder excluding substance disorder (as defined above). At least one main diagnosis was required for inclusion in psychotic disorder or affective disorder categories, whereas for personality and substance use disorders a secondary diagnosis sufficed for inclusion. Further, for the category any psychiatric diagnosis, at least one main or secondary diagnosis was required for inclusion. Information about previous suicide attempts was also obtained from the National Patient Register and was defined as a definite or an uncertain suicide attempt (ICD-8-9: E950-9 and E980-9, ICD-10: X60-84 and Y10-34), as registered in outpatient or inpatient services.
We used a definition of violent crime previously used in epidemiological research. It includes homicide, assault, robbery, threats and violence against an officer, gross violation of a person’s integrity, unlawful coercion, unlawful threats, kidnapping, illegal confinement, arson and intimidation [26]. Attempted and aggravated versions of these offences were included. Sexual crimes were not included in our definition of violent crime.
Statistical analyses
Absolute suicide rates and incidence rate ratios were calculated using data from released prisoners and matched controls. Prevalence of psychiatric morbidity among released prisoners was obtained and prevalence ratios were calculated for comparisons with controls. We used Fisher’s exact tests and Cox proportional hazards regression modelling to compare psychiatric morbidity among released prisoners who committed suicide and non-prisoner suicide controls. Relative risks were expressed as hazard ratios (HRs) with 95% confidence intervals (CI). Statistical analyses were undertaken with SPSS 20.
Results
We observed 38,995 releases among 26,985 prisoners (7.6% females) during the study period. At the date of release, the mean age was 37.8 ± 12.1 years (range 18-84). In total 27.8% of the released prisoners were born outside of Sweden (Table 1). The number of releases per prisoner varied from 1 to 9 during the study period, with a mean of 1.5 releases per prisoner (median=1). The median follow-up time per release was 451 days.
Table 1.
Descriptive data for all individuals released from prison* in Sweden 2005-2009 (n=38,955).
| Released prisoners, % (N) | |||
|---|---|---|---|
| Male | Female | All | |
| Age 17-24 years | 19.1 (6896) | 9.6 (274) | 18.4 (7170) |
| Age 25-44 years | 52.0 (18780) | 55.2 (1574) | 52.2 (2035) |
| Age 45-64 years | 27.5 (9935) | 34.4 (981) | 28.0 (10,916) |
| Age 65+ years | 1.5 (535) | 0.7 (20) | 1.4 (555) |
| Born in Sweden | 71.7 (25,920) | 78.8 (2244) | 72.2 (28,164) |
| Released once | 49.8 (18,003) | 54.5 (1552) | 50.1 (19,555) |
| Released twice | 22.6 (8174) | 22.6 (644) | 22.6 (8818) |
| Released 3+ times | 27.6 (9969) | 22.9 (653) | 27.2 (1062) |
| Prior violent conviction | 72.9 (26,334) | 40.3 (1147) | 70.5 (27,481) |
| Total | 100 (36,146) | 100 (2849) | 100 (38,995) |
Notes:
The number of released individuals is lower (N=26,985) since an individual could be released more than once during the study period.
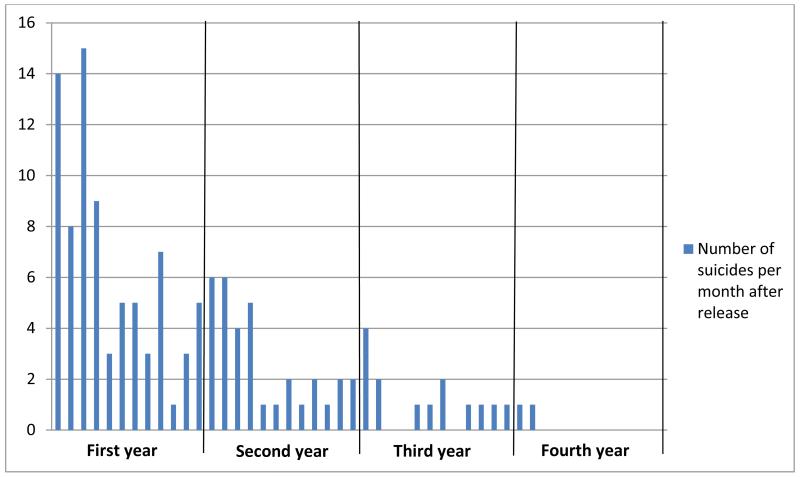
Most suicides were identified during the first year after release (Figure 1). Naturally, the numbers of person years at risk were also falling for each year of the study period. Nevertheless, with 12 observed suicides, the incidence rate for suicide was highest during the first 28 days (408 per 100,000 person years, 95% CI 211-712), and the suicide incidence rate ratio was 58 (13-534) compared to controls. The incidence rate for suicide during the whole study period was 204 (170-243), yielding an incidence rate ratio of 18 (14-24).
Figure 1.
Number of suicides (total N=127) among released prisoners in Sweden 2005-2009 by month of release. The fifth year is not shown since no suicide occurred.
Prevalence of psychiatric history in prisoners and general population controls
More than half of all released prisoners (53.6%) had been diagnosed with a psychiatric disorder at some point, with substance use disorder as the predominant category (47.0%). Altogether, 17.6% had made a previous suicide attempt that became known to health care. Compared with controls, a previous psychiatric diagnosis was more common among released prisoners. This was seen across all diagnostic categories, with the highest prevalence ratios in substance use disorder and personality disorder. Except for psychotic disorder, the prevalence was significantly higher for released female prisoners compared with released males across all diagnostic categories (Table 2).
Table 2.
Prior inpatient and outpatient* psychiatric diagnoses among released prisoners: Absolute prevalence and prevalence ratios compared with matched population controls.
| Absolute prevalence in released prisoners | Prevalence ratio (prevalence in released prisoners/controls) |
|||||
|---|---|---|---|---|---|---|
| Male (95% CI) | Female (95% CI) | All (95% CI) | Male (95% CI) | Female (95% CI) | All (95% CI) | |
| Psychotic disorder | 8.2% (7.9-8.5) | 8.4% (7.4-9.4) | 8.2% (7.9-8.5) | 10.2 (10.0-10.5) | 9.4 (8.6-10.2) | 10.2 (9.9-10.5) |
| Affective disorder | 3.4% (3.2-3,6) | 5.8% (4.9-6.7) | 3.6% (3.4-3.8) | 5.2 (4.8-5.6) | 4.8 (3.5-6.0) | 5.1 (4.6-5.5) |
| Substance use disorder | 46.1% (45.6-46.6) | 59.2% (57.4-61.0) | 47.0% (46.5-47.5) | 27.3 (26.5-28.1) | 43.3 (37.4-49.2) | 28.2 (27.3-29.1) |
| Personality disorder | 7.3% (7.0-7.6) | 11.8% (10.6-13.0) | 7.6% (7.6-7.9) | 28.6 (25.8-31.7) | 18.3 (14.4-23.6) | 26.8 (24.4-29.5) |
| Any psychiatric diagnosis (including substance use disorder) | 52.5% (52.0-53.0) | 67.3% (65.5-69.0) | 53.6% (53.1-54.1) | 11.4 (11.2-11.7) | 11.3 (10.5-12.2) | 11.4 (11.1-11.7) |
| Any psychiatric diagnosis (excluding substance use disorder) | 6.5% (6.3-6.8) | 8.1% (7.1-9.1) | 6.6% (6.4-6.9) | 2.2 (2.1-2.4) | 1.8 (1.5-2.1) | 2.2 (2.1-2.3) |
| Previous suicide attempt | 16.8% (16.4-17.2) | 27.5% (25.9-29.2) | 17.6% (17.2-18.0) | 18.6 (17.5-19.7) | 13.4 (11. 6-15.4) | 17.7 (16.8-18.7) |
Notes:
Outpatient data includes non-GP physician specialist diagnoses since 2001.
Risk factors for suicide after release from prison
A univariate Cox regression analysis of risk factors for suicide (Table 3) among released prisoners found significantly increased risk in prisoners with any previous psychiatric history (HR=3.5, 95% CI 2.3-5.3). However, when substance use disorder was excluded from this category, the increase disappeared (HR=1.1, 0.5-2.1). Other factors related to increased suicide risk were previous suicide attempt (HR=3.6, 2.5-5.1), being released twice during the study period (HR=1.6, 1.0-2.4) and being born in Sweden compared with abroad (HR=2.7, 1.6-4.6). Specific diagnostic categories associated with increased suicide risk were psychotic disorder (HR=2.4, 1.5-3.8) and substance use disorder (HR=3.1, 2.1-4.6). We found no significant increase of risk by gender, age band, or in those with a history of violent crime. In the multivariate Cox regression model, including non-overlapping predictors, the findings remained significant for substance use disorder (HR=2.1, 1.4-3.2), previous suicide attempt (HR=2.5, 1.7-3.7) and being born in Sweden (HR=2.1, 1.2-3.6) (Table 3).
Table 3.
Cox regression modelling with risk factors for suicide among al individuals releases from prison in S weden 2005-2009 (n=38,955).
| Unadjusted Hazard ratio (95% CI) |
Adjusted Hazard ratio (95% CI) |
|
|---|---|---|
| Female gender | 1.24 (0.68-2.24) | 1.05 (0.57-1.94) |
| Age 17-24§ | 0.97 (0.61-1.54) | reference |
| Age 25-44§ | 1.11 (0.78-1.57) | 0.86 (0.53-1.40) |
| Age 45-64§ | 0.86 (0.58-1.28) | 0.67 (0.39-1.16) |
| Age 65-§ | 1.54 (0.58-4.83) | 1.53 (0.46-5.14) |
| Born in Sweden vs. abroad | 2.70*** (1.60-4.56) | 2.09** (1.23-3.56) |
| Psychotic disorder | 2.35*** (1.47-3.76) | 1.59 (0.97-2.61) |
| Affective disorder | 1.53 (0.71-3.28) | 1.00 (0.46-2.18) |
| Substance use disorder | 3.12*** (2.12-4.59) | 2.13** (1.39-3.26) |
| Personality disorder | 1.38 (0.76-2.51) | 0.66 (0.35-1.24) |
|
Any psychiatric disorder (including substance use disorder) |
3.49*** (2.28-5.34) | not used due to predictor collinearity |
|
Any psychiatric disorder (excluding substance use disorder) |
1.06 (0.54-2.08) | not used due to predictor collinearity |
| Any previous suicide attempt | 3.58*** (2.51-5.09) | 2.58*** (1.76-3.78) |
| Any violent crime | 1.50 (0.99-2.26) | 1.20 (0.79-1.88) |
| Released once# | 0.68 (0.47-1.00) | reference |
| Released twice# | 1.54* (1.01-2.34) | 1.33 (0.86-2.04) |
| Released more than twice# | 1.12 (0.60-2.09) | 0.94 (0.49-1.78) |
Notes:
p<0.05,
p<0.01,
p<0.001.
Used as a dichotomous variable in the unadjusted analysis, and together with the three other age strata as a categorical variable for the adjusted, multivariate analysis.
Used as a dichotomous variable in the unadjusted analysis, and together with the two other “Released…” variables as a categorical variable for the adjusted, multivariate analysis.
Comparisons of psychiatric; morbidity among all suicide victims (Table 4) suggested higher prevalence of substance use disorder and prior suicide attempts among male prisoner suicide completers compared to male non-prisoner suicides. In contrast, a history of affective disorders was less common among released male prisoners who committed suicide than among male suicide victims in the control group of non-prisoners.
Table 4.
Characteristics of released prisoners that were also suicide deaths (N=127) and non-prisoner suicide controls matched on birth year and gender (N=102).
| Released prisoner suicide | Non-prisoner suicide | |||||
|---|---|---|---|---|---|---|
| Male % | Female % | All % | Male % | Female % | All % | |
| Age 17-24 | 17.4 (20) | 13.3 (2) | 17.3 (22) | 16.2 (16) | 0.0 (0) | 15.9 (16) |
| Age 25-44 | 52.2 (60) | 75.0 (9) | 54.3 (69) | 52.5 (52) | 66.7 (2) | 52.9 (54) |
| Age 45-64 | 27.8 (32) | 8.3 (1) | 26.0 (33) | 29.3 (29) | 33.3 (1) | 30.3 (30) |
| Age 65- | 2.6 (3) | 0.0 (0) | 2.4 (3) | 2.0 (2) | 0.0 (0) | 2.0 (2) |
| Born in Sweden | 87.8 (101) | 83.3 (10) | 87.4 (111) | 86.9 (86) | 100.0 (3) | 87.3 (89) |
| Psychotic disorder | 16.5 (19) | 16.7 (2) | 16.5¤ (21) | 8.1 (8) | 0.0 (0) | 7.8 (8) |
| Affective disorder | 6.1# (7) | 0.0 (0) | 5.5# (7) | 15.2 (15) | 33.3 (1) | 15.7 (16) |
| Substance use disorder | 70.4¤ (81) | 83.3 (10) | 71.7¤ (91) | 24.2 (24) | 33.3 (1) | 24.5 (25) |
| Personality disorder | 7.8 (9) | 25.0 (3) | 9.5 (12) | 6.1 (6) | 66.7 (2) | 7.8 (8) |
| Any psychiatric disorder | 76.5¤ (88) | 100.0 (12) | 78.7¤ (100) | 41.4 (41) | 66.7 (2) | 42.2 (43) |
| Any psychiatric disorder | 6.1# (7) | 16.7 (2) | 7.1# (9) | 17.2 (17) | 33.3 (1) | 17.6 (18) |
| Prior suicide attempt | 40.9¤ (47) | 50.0 (6) | 41.7¤ (53) | 23.2 (23) | 66.7 (2) | 24.5 (25) |
| All suicides | 100 (115) | 100 (12) | 100 (127) | 100 (99) | 100 (3) | 100 (102) |
Notes:
Significantly higher than among the respective controls; male, female or all (Fischer’s exact test, 2-sided p<0.05).
Significantly lower than among the respective controls; male, female or all (Fischer’s exact test, 2-sided p<0.05).
Discussion
In this study of almost 40,000 releases of nearly 27,000 prisoners over five years, we identified 920 deaths, of which 127 (14 %) were from suicide. There were three main findings. First, the overall suicide risk among released prisoners was 18 times higher compared to the non-convicted general population. The risk increase was even more pronounced during the first months after release, suggesting that this is a particularly vulnerable period. Second, the strongest independent risk factors for suicide among released prisoners were substance use disorder, previous suicide attempt, and being born in Sweden. Third, the prevalence of risk factors for completed suicide differed between released prisoners and general population controls.
Suicide rates after release from prison
The high overall suicide rate supported the idea that transition to life outside prison is a period with substantially increased risk for premature death. Previous research has also suggested increased risks for relapse in alcohol- and drug misuse, unemployment, and homelessness [27]. Programs designed to facilitate the transition from prison to the general community differ between countries; this could partly explain differences between studies in suicide rates immediately after release. Different ways of pathologists’ labelling of cases of drug overdoses with unknown intent might also explain some differences [28].
The generalizability of previous research on suicide rates and risk factors in ex-prisoners has been uncertain because prison systems differ across countries. Previous research has been conducted in nations with large prison populations. However, despite this important difference, suicide rates in this study were similar to (or slightly higher) than in prior research [3]. Interestingly, the study with the most similar suicide rates to the current investigation was from England and Wales [14], where the prison population rate is almost twice that in Sweden.
The particularly high suicide rate ratios in this study should be interpreted with caution due to the large confidence intervals. The use of non-convicted general population controls enabled us to show the difference in suicide risk between ex-prisoners and individuals who have never been sentenced. Our choice of controls can partly explain the prominent figures in this study. In some earlier work in the field, researchers have tried to adjust for social class and others have used suicide rates in drug-addicted persons[29], with lower suicide rate ratios subsequently reported.
Risk factors for suicide after release from prison
We identified several risk factors for suicide among prisoners following release. Substance use disorder and psychotic disorder were strong risk factors in unadjusted analyses. However, when combined in a multivariate Cox regression model, psychotic disorder was of borderline significance. This is probably a type II error, but could also suggest that psychosis often co-exists with substance use disorder in offender populations. The latter interpretation is supported by the fact that the combination of these disorders has a strong association with criminal behavior [30, 31]. Importantly, a previous suicide attempt, an established risk factor for suicide among psychiatric patients [6] and incarcerated prisoners [10] remained a moderately strong independent risk factor in the multivariate model. Previous research in this field has not been able to compare the impact of psychiatric morbidity, including personality disorder, with the same detail as in the present study. Our novel findings underline the relevance of identifying substance use disorder and prior suicidal behavior when assessing suicide risk in released prisoners.
Previous studies [12, 32, 33] suggested that violent crime predicts subsequent suicide among released prisoners. However, our results agree with another recent population study of suicide risk among criminal offenders in Denmark [34]; these authors reported that the suicide risk seen among violent offenders was substantially lowered when psychiatric and social risk factors were accounted for.
We found that being born in Sweden was associated with higher suicide risk among the released prisoners. This is in line with a recent Swedish cohort study where being born in Sweden was compared with being born in a non-Nordic country [35]. In general, the suicide rates among first-generation immigrants reflect the suicide rates in the countries of birth [36]. A National Swedish report from 2005 showed that more than 60% of the immigrants who were suspected of crime between 1997 and 2001 were from outside the European Union [37]. However, since we lack more detailed data on specific country, further analysis on this is beyond the scope of our present study.
Psychiatric history among prisoners and general population controls
As expected, lifetime psychiatric morbidity was common among released prisoners, especially substance use, psychotic and personality disorders. Substance use disorder strongly correlates with criminal behavior [38, 39] and the high prevalence seen in our study is in line with previous work based on screening at incarceration [9]. Psychotic disorder is a heterogeneous diagnostic category including schizophrenia but also, for instance, acute and psychotic states that may be induced by substance abuse. Since substance abuse is common among prisoners, prevalence patterns of psychotic disorder could differ between prisoners and the general population. In addition, since people suffering from a severe psychotic disorder (excluding alcohol-induced psychoses) while committing a crime is normally diverted away from prison sentences in Sweden, this group was not included in our study. The prevalence of personality disorder in this cohort of released prisoners is likely underestimated, since personality disorders are seldom primary reason for inpatient psychiatric care. Hence, several studies based on structured interviews have shown much higher figures among prisoners [40].
Interestingly, a history of substance use disorder was more common among released male prisoners who committed suicide than among matched population, non-prisoner suicides. This suggests that substance use disorder may play a more important role in suicides among released prisoners. Further, released prisoners who committed suicide more often had previous suicide attempts compared to general population suicide victims. The relatively low prevalence of affective disorder and personality disorder among released prisoners who committed suicide is somewhat surprising.
Previous studies have shown that risk factors for suicide appear to be different for suicide in custody (e.g. marital status [10]) and for those with any psychiatric diagnosis (e.g. marital status and socioeconomic status [41]) when compared with the general population. The findings in our present study support the hypothesis that suicide among released prisoners is less related to affective disorder than suicide in the general population, and that other markers of psychopathology are more prominent. One explanation could be higher prevalence of impulsive and/or aggressive personality traits that predispose to both criminal and suicidal behavior among criminal offenders, as well as the development of substance use disorders [42]. It is also possible that the observed difference indicates specific health care seeking behaviors among prisoners, or tendencies in the health care system to underdiagnose affective disorders when they co-exist with substance use disorders. Our results also suggest that more research is needed to further investigate specific; risk factors for suicide and all-cause mortality in recently released prisoners. This could include the effect of imprisonment, psychosocial factors, and the role of treatment after release.
Strengths and limitations
To date, this is the largest study on suicide following release from prison. Further, compared to previous studies, we were able to delineate the psychiatric morbidity that affects suicide risk and how the suicide risk factor pattern differs from that in the general population. Complete coverage of the studied population is another strength. Although our data collection was prospective and preceded the suicide death, register-based studies rely on collection of data from many different clinics and hospitals and the validity of the diagnoses may thus vary. Still, previous studies of the Swedish Patient Register indicate good to excellent validity for schizophrenia and bipolar disorder diagnoses [43, 44]. The particularly high suicide rate ratios in this study should be interpreted with some caution due to the large confidence intervals. Further, the use of non-convicted general population controls without adjusting for possible social risk factors could partly explain the prominent elevation of suicide risk.
However, a limitation of our study was that we could only include psychiatric morbidity and suicide attempts that led to an episode of inpatient care if it occurred before 2001, and inpatient or outpatient care after 2001. People with psychiatric problems who never sought help and who never were referred to psychiatric care were therefore not included. Further, due to lack of statistical power, we did not study the contribution of length of sentence, physical illness, family history of suicide, and work status, to name a few potentially important factors, that could be considered in future research.
Conclusion
In summary, we found that suicide among released prisoners was 18 times more common than in the general population with particularly high risks during the first four weeks. A previous suicide attempt, previous psychiatric disorder, particularly substance abuse, and being born in Sweden were important, independent risk factors. We found a different pattern of psychiatric risk factors for suicide among released prisoners compared with suicide in the general population.
Our findings are consistent with those from other high-income countries with different prison systems than Sweden, such as the US, England and Australia, suggesting some generalizability of previous results in this field. Further, our study advance knowledge on suicide risk factors among ex-prisoners, which should inform suicide risk assessment following release from prison. Future research in this field is needed, for example, to investigate the role of risk assessment, psychiatric treatment and efforts aimed to facilitate transition to life outside prison.
The elevated suicide rates in this study underline the need for selective preventive efforts for this high-risk group. Hence, prison and probation services, mental healthcare, and social services may need to collaborate to develop evidence-based prevention strategies for this population. Other implications arising from our findings include allocating appropriate resources to facilitate transition to life outside prison, as well as increased clinical monitoring during the first four weeks post-release for ex-prisoners with a history of both previous suicide attempts and substance abuse. In addition, consideration should be given to involving community mental health services before release from prison in those at higher risk. Finally, the risk of suicide after release from prison should be highlighted. National suicide prevention strategies should include recently released prisoners as a high-risk group.
Clinical points.
-
-
The suicide risk among released prisoners is high, particularly during the first months after release
-
-
Previous psychiatric disorder, substance abuse and suicide attempts are strong risk factors
-
-
Factors facilitating transition to life outside prison and clinical monitoring during the first months after release may be indicated to prevent suicide
Acknowledgements
Axel Haglund received financial support for this research project from the Swedish Prison and Probation Administration
Jussi Jokinen is supported by The Swedish Research Council
Niklas Långström is supported by the Swedish National Prison and Probation Administration. He received one speaker honorarium from Lundbeck in the past year.
Seena Fazel is supported by the Wellcome Trust
Bo Runeson received honoraria from Astra Zeneca AB, Lundbeck Foundation and Lilly in the past year.
Footnotes
Ethical approval was obtained from the Stockholm’s Regional Ethics Committee (Protocol 2010/5:7)
Preliminary data from this study were presented in an oral presentation at The International Association for Suicide Prevention’s (IASP) World Congress, September 27, 2013, in Oslo, Norway
Declaration of interest: None.
References
- 1.Walmsley R. World Prison population List. 9th edition. Kings College London International Centre for Prison Studies; London: 2012. http://www.scribd.com/doc/77097293/World-Prison-Population-List-9th-edition. [Google Scholar]
- 2.Schmitt J, Warner K. Ex-offenders and the Labor Market. Center for Economic and Policy Research. 2010 http://www.cepr.net/documents/publications/ex-offenders-2010-11.pdf. [Google Scholar]
- 3.Fazel S, Grann M, Kling B, et al. Prison suicide in 12 countries: an ecological study of 861 suicides during 2003-2007. Soc Psychiatry Psychiatr Epidemiol. 2011;46(3):191–5. doi: 10.1007/s00127-010-0184-4. [DOI] [PubMed] [Google Scholar]
- 4.Fazel S, Baillargeon J. The health of prisoners. Lancet. 2011;377(9769):956–65. doi: 10.1016/S0140-6736(10)61053-7. [DOI] [PubMed] [Google Scholar]
- 5.Harris EC, Barraclough B. Suicide as an outcome for mental disorders. A meta-analysis. Br J Psychiatry. 1997;170:205–28. doi: 10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- 6.Tidemalm D, Langstrom N, Lichtenstein P, et al. Risk of suicide after suicide attempt according to coexisting psychiatric disorder: Swedish cohort study with long term follow-up. BMJ. 2008;337:a2205. doi: 10.1136/bmj.a2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hawton K, van Heeringen K. Suicide. Lancet. 2009;373(9672):1372–81. doi: 10.1016/S0140-6736(09)60372-X. [DOI] [PubMed] [Google Scholar]
- 8.Fazel S, Seewald K. Severe mental illness in 33,588 prisoners worldwide: systematic review and meta-regression analysis. Br J Psychiatry. 2012;200(5):364–73. doi: 10.1192/bjp.bp.111.096370. [DOI] [PubMed] [Google Scholar]
- 9.Fazel S, Bains P, Doll H. Substance abuse and dependence in prisoners: a systematic review. Addiction. 2006;101(2):181–91. doi: 10.1111/j.1360-0443.2006.01316.x. [DOI] [PubMed] [Google Scholar]
- 10.Fazel S, Cartwright J, Norman-Nott A, et al. Suicide in prisoners: a systematic review of risk factors. J Clin Psychiatry. 2008;69(11):1721–31. [PubMed] [Google Scholar]
- 11.Kariminia A, Law MG, Butler TG, et al. Suicide risk among recently released prisoners in New South Wales, Australia. Med J Aust. 2007;187(7):387–90. doi: 10.5694/j.1326-5377.2007.tb01307.x. [DOI] [PubMed] [Google Scholar]
- 12.Pratt D, Appleby L, Piper M, et al. Suicide in recently released prisoners: a case-control study. Psychol Med. 2009:1–9. doi: 10.1017/S0033291709991048. [DOI] [PubMed] [Google Scholar]
- 13.Zlodre J, Fazel S. All-cause and external mortality in released prisoners: systematic review and meta-analysis. Am J Public Health. 2012;102(12):e67–75. doi: 10.2105/AJPH.2012.300764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pratt D, Piper M, Appleby L, et al. Suicide in recently released prisoners: a population-based cohort study. Lancet. 2006;368(9530):119–23. doi: 10.1016/S0140-6736(06)69002-8. [DOI] [PubMed] [Google Scholar]
- 15.Binswanger IA, Stern MF, Deyo RA, et al. Release from prison--a high risk of death for former inmates. N Engl J Med. 2007;356(2):157–65. doi: 10.1056/NEJMsa064115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dirkzwager A, Nieuwbeerta P, Blokland A. Effects of First-Time Imprisonment on Postprison Mortality: A 25-Year Follow-Up Study with a Matched Control Group. Journal of Research in Crime and Delinquency. 2012;49(3):383–419. [Google Scholar]
- 17.Binswanger IA, Blatchford PJ, Lindsay RG, et al. Risk factors for all-cause, overdose and early deaths after release from prison in Washington state. Drug Alcohol Depend. 2011;117(1):1–6. doi: 10.1016/j.drugalcdep.2010.11.029. [DOI] [PubMed] [Google Scholar]
- 18.Swedish Prison and Probation Services Official Statistics. 2012 http://www.kriminalvarden.se/sv/Statistik/
- 19.Carli V, Mandelli L, Postuvan V, et al. Self-Harm in Prisoners. CNS Spectr. 2011;16(3):75–81. doi: 10.1017/S1092852912000211. [DOI] [PubMed] [Google Scholar]
- 20.Hakansson A, Berglund M. All-cause mortality in criminal justice clients with substance use problems-A prospective follow-up study. Drug Alcohol Depend. 2013 doi: 10.1016/j.drugalcdep.2013.03.014. doi: 10.1016/j.drugalcdep.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 21.Neeleman J, Wessely S. Changes in classification of suicide in England and Wales: time trends and associations with coroners’ professional backgrounds. Psychol Med. 1997;27(2):467–72. doi: 10.1017/s0033291796004631. [DOI] [PubMed] [Google Scholar]
- 22.Runeson B, Tidemalm D, Dahlin M, et al. Method of attempted suicide as predictor of subsequent successful suicide: national long term cohort study. BMJ. 2010;341:c3222. doi: 10.1136/bmj.c3222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Webb RT, Kontopantelis E, Doran T, et al. Suicide risk in primary care patients with major physical diseases: a case-control study. Arch Gen Psychiatry. 2012;69(3):256–64. doi: 10.1001/archgenpsychiatry.2011.1561. [DOI] [PubMed] [Google Scholar]
- 24.Hawton K, Bergen H, Simkin S, et al. Long term effect of reduced pack sizes of paracetamol on poisoning deaths and liver transplant activity in England and Wales: interrupted time series analyses. BMJ. 2013;346:f403. doi: 10.1136/bmj.f403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bjorkenstam E, Bjorkenstam C, Vinnerljung B, et al. Juvenile delinquency, social background and suicide--a Swedish national cohort study of 992,881 young adults. Int J Epidemiol. 2011;40(6):1585–92. doi: 10.1093/ije/dyr127. [DOI] [PubMed] [Google Scholar]
- 26.Frisell T, Lichtenstein P, Langstrom N. Violent crime runs in families: a total population study of 12.5 million individuals. Psychol Med. 2010:1–9. doi: 10.1017/S0033291710000462. [DOI] [PubMed] [Google Scholar]
- 27.Binswanger IA, Nowels C, Corsi KF, et al. Return to drug use and overdose after release from prison: a qualitative study of risk and protective factors. Addict Sci Clin Pract. 2012;7(1):3. doi: 10.1186/1940-0640-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bohnert AS, Ilgen MA, Ignacio RV, et al. Risk of death from accidental overdose associated with psychiatric and substance use disorders. Am J Psychiatry. 2012;169(1):64–70. doi: 10.1176/appi.ajp.2011.10101476. [DOI] [PubMed] [Google Scholar]
- 29.Fazel S, Benning R. Suicides in female prisoners in England and Wales, 1978-2004. Br J Psychiatry. 2009;194(2):183–4. doi: 10.1192/bjp.bp.107.046490. [DOI] [PubMed] [Google Scholar]
- 30.Fazel S, Langstrom N, Hjern A, et al. Schizophrenia, substance abuse, and violent crime. JAMA. 2009;301(19):2016–23. doi: 10.1001/jama.2009.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Van Dorn R, Volavka J, Johnson N. Mental disorder and violence: is there a relationship beyond substance use? Soc Psychiatry Psychiatr Epidemiol. 2012;47(3):487–503. doi: 10.1007/s00127-011-0356-x. [DOI] [PubMed] [Google Scholar]
- 32.Stenbacka M, Moberg T, Romelsjo A, et al. Mortality and causes of death among violent offenders and victims--a Swedish population based longitudinal study. BMC Public Health. 2012;12:38. doi: 10.1186/1471-2458-12-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Joukamaa M. The mortality of released Finnish prisoners; a 7 year follow-up study of the WATTU project. Forensic Sci Int. 1998;96(1):11–9. doi: 10.1016/s0379-0738(98)00098-x. [DOI] [PubMed] [Google Scholar]
- 34.Webb RT, Qin P, Stevens H, et al. National Study of Suicide in All People With a Criminal Justice History. Arch Gen Psychiatry. 2011;68(6):591–9. doi: 10.1001/archgenpsychiatry.2011.7. [DOI] [PubMed] [Google Scholar]
- 35.Crump C, Sundquist K, Sundquist J, et al. Sociodemographic, psychiatric and somatic risk factors for suicide: a Swedish national cohort study. Psychol Med. 2013:1–11. doi: 10.1017/S0033291713000810. [DOI] [PubMed] [Google Scholar]
- 36.Ferrada-Noli M. A cross-cultural breakdown of Swedish suicide. Acta Psychiatr Scand. 1997;96(2):108–16. doi: 10.1111/j.1600-0447.1997.tb09914.x. [DOI] [PubMed] [Google Scholar]
- 37.Martens P, Holmberg S. Crime among persons born in Sweden and other countries. National Council for Crime Prevention; 2005. [Google Scholar]
- 38.Grann M, Danesh J, Fazel S. The association between psychiatric diagnosis and violent re-offending in adult offenders in the community. BMC Psychiatry. 2008;8:92. doi: 10.1186/1471-244X-8-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lundholm L, Haggard U, Moller J, et al. The triggering effect of alcohol and illicit drugs on violent crime in a remand prison population: a case crossover study. Drug Alcohol Depend. 2013;129(1-2):110–5. doi: 10.1016/j.drugalcdep.2012.09.019. [DOI] [PubMed] [Google Scholar]
- 40.Fazel S, Danesh J. Serious mental disorder in 23000 prisoners: a systematic review of 62 surveys. Lancet. 2002;359(9306):545–50. doi: 10.1016/S0140-6736(02)07740-1. [DOI] [PubMed] [Google Scholar]
- 41.Agerbo E. High income, employment, postgraduate education, and marriage: a suicidal cocktail among psychiatric patients. Arch Gen Psychiatry. 2007;64(12):1377–84. doi: 10.1001/archpsyc.64.12.1377. [DOI] [PubMed] [Google Scholar]
- 42.Gvion Y, Apter A. Aggression, impulsivity, and suicide behavior: a review of the literature. Arch Suicide Res. 2011;15(2):93–112. doi: 10.1080/13811118.2011.565265. [DOI] [PubMed] [Google Scholar]
- 43.Dalman C, Broms J, Cullberg J, et al. Young cases of schizophrenia identified in a national inpatient register--are the diagnoses valid? Soc Psychiatry Psychiatr Epidemiol. 2002;37(11):527–31. doi: 10.1007/s00127-002-0582-3. [DOI] [PubMed] [Google Scholar]
- 44.Sellgren C, Landen M, Lichtenstein P, et al. Validity of bipolar disorder hospital discharge diagnoses: file review and multiple register linkage in Sweden. Acta Psychiatr Scand. 2011;124(6):447–53. doi: 10.1111/j.1600-0447.2011.01747.x. [DOI] [PubMed] [Google Scholar]