Abstract
Background
To explore the feasibility and efficiency of community-based integrated traditional Chinese medicine (TCM) and Western medicine metabolic syndrome (MS) intervention in rural residents.
Material/Methods
The MS intervention was administered to 598 rural community residents aged 45 years and older in Zhoushi from 2011 to 2013. Subjects completed a health examination and health behavior questionnaire before and after the intervention. In the intervention, we designed a “healthy life self-help program” using TCM appropriate technologies for the subjects.
Results
After 2 years of intervention by means of integrated traditional Chinese and Western medicine, 57.0% (341 persons) of the subjects no longer suffered from MS. The recovery rate of BMI, blood pressure, FBG, TG, and HDL-C were 22.1%, 40.5%, 37.9%, 32.8%, and 62.4%, respectively. There were statistically significant differences in exercise, smoking, and alcohol drinking between baseline and 2 years later.
Conclusions
The integrated traditional Chinese and Western medicine MS intervention was effective in deceasing most of the parameters of MS, especially blood pressure, and helping people to do more exercise. The program would be useful to implement in other similar populations.
MeSH Keywords: Medicine, Chinese Traditional; Metabolic Syndrome X; Rural Population
Background
During recent decades, with improving living standards, changing lifestyles, and aging population, metabolic syndrome (MS) has become a major public health challenge worldwide [1]. The China Health and Nutrition Survey in 2009 showed that the overall age-standardized prevalence estimate of MS was 10.5% based on the Chinese Diabetes Society criteria [2]. Studies have shown that MS can cause cardiovascular disease, reduce quality of life, and increase mortality [3–5]. There is an urgent need to take measures to prevent and treat chronic diseases such as hypertension and metabolic syndrome.
Currently, lifestyle interventions focused on physical activity, diet, and other health behaviors are often adopted as the main method of MS intervention, using a web-based platform or cooperating with home-care providers or general practitioners [6–11]. These interventions can improve the patient’s lifestyle to some extent, but they are mostly offered to urban community residents. Few MS intervention studies have focus on rural community residents.
Kunshan is located inside the Yangtze River Delta economic area, one of the fastest growing regions in China. Kunshan is unique because of its high population density. The population density in Kunshan was 646 persons/km2 in 2002 [12]. With population and economic growth, a special rural community arose. Since the population of the rural community has grown so large, with a large transient population, it is more difficult technically and politically to carry out standardized MS interventions and management in rural communities in Kunshan.
Medical literature, clinical practice and basic research had proved that TCM can effectively lower blood pressure, blood lipids, blood glucose, and treat the complications of diabetes [13–17]. Since the cause and pathogenesis of MS varies and people with MS are at higher risk of diabetes, coronary heart disease, and other cardiovascular diseases, it is more effective to intervene in MS using TCM-appropriate technology on the basis of Western medicine, with emphasis on integrity, systemic, dialectic, and tian ren he yi (a theory that man is an integral part of nature).
Therefore, we put forward a novel community-based intervention, using integrated traditional Chinese and Western medicine on the basis of community health service, carrying out a study by the intervention and management of MS in rural residents.
Material and Methods
This study was conducted by the health care institutions of Zhoushi (a town in Kunshan) and our team. We did MS intervention from 2011 to 2013 for the rural community resident population aged 45 years and above in Zhoushi. There were 13 912 people who received a health examination. Among those people, 1964 persons were MS patients, and among them 630 agreed to participate in the intervention. In the end, 598 persons had the health examination and health behavior questionnaire before and after the intervention. This study was approved by the local ethics committee.
Participants
Inclusion criteria:
Participants with MS (based on the Chinese Diabetes Society 2004 criteria) [5];
Participants aged 45 years and above.
Exclusion criteria:
Inability to exercise;
Refused to attend.
Intervention
Building “healthy life self-help program”
“Healthy life self-help program” was run by the community health services center. The program serves subjects by forming self-management groups and conducting monthly activities. Since the main working methods are health education, health guidance, and health intervention, people in the program can take part in activities like regularly self-help health examination, health knowledge lecture, prevention measure guide, and early disease screening, which can help residents adopt a healthy lifestyle, make early health interventions, lead people to self-involvement and self-management, and improve the quality of life. Details were as follows:
Diagnostic equipment such as a food quantitative model, automatic arm tube type blood pressure monitor, automatic height and weight measurement instrument, blood glucose meter, body fat meter, and rehabilitation activities equipment are furnished in the program for the subjects. With the food quantitative model, patients could make diet choices more intuitively, feeling the weight, size, and thickness of food by looking and touching. With other equipment we measured height, weight, blood pressure, blood glucose, and body fat for the subjects. All the measures above are free so we can constantly monitor different factors of the subjects, and we can also help the subjects strengthen the sense of self-management.
Lectures and on-site consultation were held for the subjects, during which physicians and nurses would give lectures about basic knowledge of diabetes, diet therapy, exercise therapy, medication, and so on.
Other activities aimed to develop self-management skills and establish confidence in improving health for the subjects, such as training on blood glucose monitoring and insulin injection.
The application of TCM appropriate technologies
We identified the TCM constitution of the subjects using the software named TCM constitution evaluation system. On the basis of the evaluation results, we used acupuncture, massage, daoyin, tai chi, and meridian flap to mobilize the residents’ body’s natural balance fully. At the same time, we used diet and medication to complement the vigor of the residents, which can improve the body’s resistance to disease inside and outside. Details were as follows:
Give different dietary suggestions to different subjects according to their TCM constitution so as to keep the balance of Yin and Yang. Eat less but often was advocated. Details are as follows: Do not eat any sugar products such as candy. Eat less starch products like Chinese yam, less oily foods like peanuts, less high-cholesterol foods like yolk. Eat more whole grains such as oatmeal, bean products, and vegetables.
One of the characteristics of TCM is dialectical treatment. Most of the MS patients have disorders on the balance of Yin and Yang. So we took TCM treatments respectively depending on the subjects’ TCM constitution, which can improve the body’s internal environment. At the same time, we took treatments of tonifying to avoid the liver and kidney damage because of the long-term use of Western medicine, took traditional massage and medicinal food diet to delay the complications of MS.
Training in tai chi was held for the subjects every week. According to the theory of Yin and Yang, 5 elements and viscera meridian of TCM, teaching the MS patients special exercises such as Baduanjin qigong, to help them establish the coordination of body and mind. We used methods like tai chi, health qigong, massage, acupoint pressure, and meridian flap to dredge the meridian and adjust the qixue of the MS patients. Warm-up before exercise and cool-down after exercise are also essential to keep the balance of Yin and Yang.
Study design
This was a 2-year before-after study, conducting health physically examination at baseline and 2 years later, including the measurement of height, weight, systolic blood pressure (SBP), diastolic blood pressure (DBP), fasting blood glucose (FBG), triglycerides (TG), and high-density lipoprotein cholesterol (HDL-C). In addition, we researched the health behaviors (including exercise, smoking, and alcohol drinking) of the intervention subjects using the self-response questionnaire at the beginning and the end of the project. We had a total of 598 subjects after pretreatment.
Evaluation
Evaluation indexes were the changes of MS and its components (body weight, blood pressure, blood glucose, blood lipids) and the stage of change in health behaviors.
Statistical analysis
We used Excel for database integration and graphics and SPSS for the statistical analyses.
All analyses were performed on persons who completed the MS intervention and had the health examination and health behavior test at baseline and 2 years. Mean and standard deviation (SD), frequency, and ratio were used to describe the basic situation of the indicators. Paired t-test, McNemar test, and Wilcoxon paired rank-sum test were used to analyze the change of biological parameters and health behaviors. Statistical significance was defined as a P value <0.05.
Results
General conditions
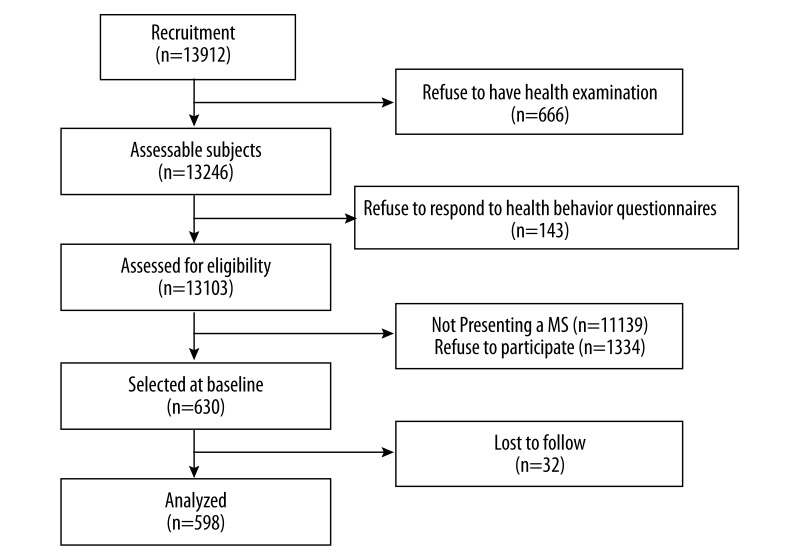
Figure 1 is the flow chart of the study population. There were 13 912 people who participated in our research at baseline and 1334 of them were MS patients. Among the patients, 598 people accepted the intervention and had health examination and health behavior questionnaire after intervention – 56.5% of the 598 people were women; 52.8% were 60 years old and above; 60.9% of them were postgraduate; 0.3% of them were unmarried; 77.3% of them had joined the basic medical insurance for urban workers, and 21.4% of them had participated in the basic medical insurance for urban residents.
Figure 1.
Flow chart of the study population.
Health status change
After 2 years of intervention, 57.0% (341 persons) of the subjects no longer had MS. There were 3.8% (23 persons) of the subjects with zero components of MS, 16.2% (97 persons) of the subjects were had 1, and 37.0% (221 persons) of the subjects had 2 components.
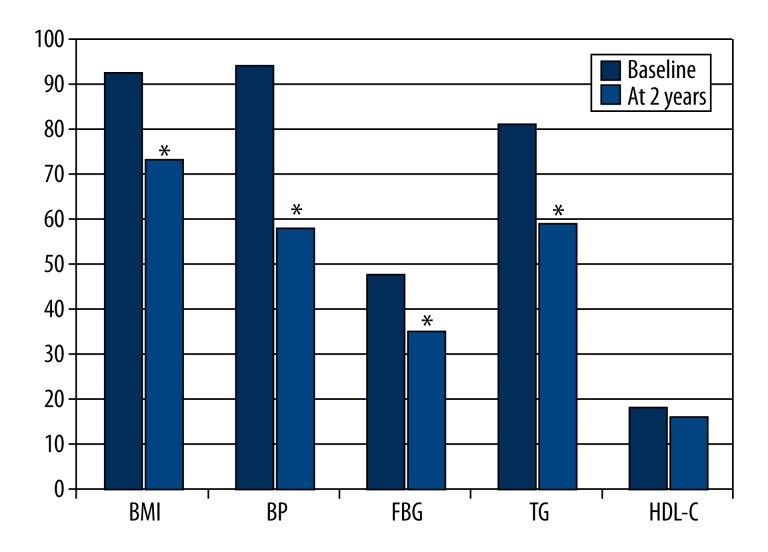
Figure 2 shows the change of the abnormal rate in MS components between baseline and 2 years later. There were statistically significant reductions in the abnormal rate in BMI (χ2=100.744, P<0.001), blood pressure (χ2 =192.604, P<0.001), FBG (χ2=38.837, P<0.001), and TG (χ2=92.263, P<0.001). There was a reduction in HDL-C, but the reduction was not statistically significant.
Figure 2.
Change of the metabolic syndrome components between baseline and 2 years later. * P<0.05 between baseline and 2 years.
Table 1 presents the changes of the biological parameters of the intervention subjects. There were reductions in BMI, SBP, DBP, FBG, and TG and the reductions were statistically significant (P<0.05).
Table 1.
Biological parameter of the subjects.
| Variables | Baseline | Change at 2 years | t | P value |
|---|---|---|---|---|
| BMI | 27.31±2.32 | −0.77 | 11.858 | 0.000 |
| SBP | 152.20±17.84 | −9.49 | 12.496 | 0.000 |
| DBP | 93.49±9.88 | −8.41 | 17.975 | 0.000 |
| FBG | 6.40±1.97 | −0.25 | 3.959 | 0.000 |
| TG | 2.73±1.96 | −0.26 | 3.368 | 0.001 |
Data are expressed as mean ±SD.
Table 2 presents the 598 intervention subjects’ improvement results of the health status. After 2 years of comprehensive intervention, among those 553 persons who were overweight or obese, 122 of them recovered to normal weight, and the recovery rate was 22.1% (122/553). The recovery rate of blood pressure, FBG, TG, and HDL-C were 40.5%, 37.9%, 32.8%, and 62.4%, respectively.
Table 2.
Health status improvement of the intervention subjects.
| Variables | Abnormal | Up to standard | |
|---|---|---|---|
| n | % | ||
| BMI | 553 | 122 | 22.1 |
| Blood pressure | 563 | 228 | 40.5 |
| FBG | 285 | 108 | 37.9 |
| TG | 485 | 159 | 32.8 |
| HDL-C | 109 | 68 | 62.4 |
Health behavior change
Table 3 shows the 598 subjects’ change in health behaviors at baseline and 2 years later. Wilcoxon paired rank-sum test showed that there was a statistically significant of change in exercise (p<0.001) between baseline and 2 years later – 72.9% (422 persons) of the 579 persons who didn’t do any exercise at baseline began to participate in physical exercise 2 years later and 15.8% (3 persons) of the 19 persons who did exercise at baseline didn’t carry on 2 years later. The difference of rate in smoking was statistically significant (p<0.001) – 34.8% (55 persons) of the 158 smokers at baseline had quitted smoking 2 years later and 15.5% (68 persons) of the 440 non-smokers began to smoke. The difference of rate in alcohol drinking was statistically significant (p<0.05) – 34.5% (50 persons) of the 145 persons who drink alcohol quitted drinking 2 years later and 19.4% (88 persons) of the 453 persons who didn’t drink alcohol became drinkers.
Table 3.
Change in health behaviors at baseline and 2 years later.
| Variables | Baseline | 2 years | Z | p value | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Exercise | −17.880 | 0.000 | ||||
| Every day | 5 | 0.8 | 123 | 20.6 | ||
| More than once a week | 3 | 0.5 | 128 | 21.4 | ||
| Occasionally | 11 | 1.8 | 187 | 31.3 | ||
| Never | 579 | 96.8 | 160 | 26.8 | ||
| Smoking | −5.929 | 0.000 | ||||
| Never | 430 | 71.9 | 362 | 60.5 | ||
| Formerly | 10 | 1.7 | 65 | 10.9 | ||
| Currently | 158 | 26.4 | 171 | 28.6 | ||
| Alcohol drinking | −2.055 | 0.040 | ||||
| Never | 453 | 75.8 | 415 | 69.4 | ||
| Occasionally | 40 | 6.7 | 107 | 17.9 | ||
| Often | 16 | 2.7 | 44 | 7.4 | ||
| Every day | 89 | 14.9 | 32 | 5.4 | ||
Discussion
After 2 years of the intervention, 57.0% (341 persons) of the subjects no longer suffered from MS. There were statistically significant reductions in the abnormal rate and value of BMI, Blood pressure, FBG and TG. Compared with the results of the network platform health behavior intervention in South Korea in 2014, our intervention seems to be more effective and consistent in reducing SBG (from 132.03±15.27 to 129.21±17.80) and DBG (from 84.79±13.07 to 86.96±8.91) [6]. In addition, there were different degrees of improvement in MS components (recovery rate of BMI, blood pressure, FBG, TG and HDL-C were 22.1%, 40.5%, 37.9%, 32.8%, and 62.4%, respectively), which is similar with the results of the 2012 health behavior intervention project in South Korean (recovery rate of blood pressure, FBG, TG, HDL-C were 46.4%, 29.8%, 51.2%, and 59.4%, respectively) [8].
After the intervention, the health behaviors of the intervention subjects had improved, too. There were statistically significant differences in exercise, smoking, and alcohol drinking between baseline and 2 years later – 72.9% of the 579 persons who didn’t do any exercise began to participate in physical exercise 2 years later, and the participation rate of physical activity had increased from 3.2% at baseline to 73.2% 2 years later. Compared with the Geneva (Switzerland) research result that behavioral intervention increased the participation rate of physical activity by 3.4% (P<0.05) [10], this intervention seemed to have a better effect in that it could motivate more MS patients to do exercise. This may be because the subjects in our intervention were all rural residents who had little health knowledge and lack of health consciousness before the intervention. The MS interventions conduct an intense training of tai chi for the patients with MS in the community every week. After a period of study, it activated subjects’ body and soul, and it increased the enthusiasm of the subjects to participate in the exercise. Tai chi also exerted a positive effect on patients with MS.
TCM has a long history. TCM is characterized by differential treatment. It provides symptomatic treatment to patients with hypertension, hyperglycemia, or hyperlipidemia according to their physical characteristics, so as to improve the environment of the body and relieve symptoms effectively. It can also protect those patients from liver and kidney damage under the condition that they take medicine through tonifying adjustment. In addition, with traditional massage, medicated diet, and other therapies, it can relieve the complications caused by diabetes or hypertension. For different people, TCM will adopt different therapies to help patients keep fit, strengthen vital qi to eliminate pathogenic factors, and consequently improve living quality. Using integrated traditional Chinese and Western medicine technology on the basis of community health service, carrying out the intervention, and management of MS to rural residents can both take advantage of traditional Chinese medicine and adapt to the specific characteristics of rural communities so that it can be popularized and used in similar regions.
Furthermore, the intervention subjects’ health behaviors also have a negative side – 15.8% of the 19 persons who did exercise at baseline didn’t carry on 2 years later and 15.5% of the 440 non-smokers began to smoke at 2 years, and 19.4% of the 453 persons who didn’t drink alcohol became drinkers at 2 years. The reason is that subjects with bad health behaviors could get more attention. The intervention implementers tended to pay more attention to those with bad health behaviors so that these people would have more motivation to reduce bad behavior. In contrast, those subjects without bad health behaviors had less health awareness and were reluctant to participate in the intervention. This phenomenon reminds us that during the process of behavior intervention, it’s not enough to only aim at the high risk group, it’s more important to aim at the general population.
The main limitation of this study is the lack of a parallel control group. This means that we cannot conclude that the improvement in MS was due to our intervention alone. There may be other factors such as participation, which may promote MS patients to pay more attention to their health, which could also affect the attitude to health and the health behaviors of the MS patients. Another limitation is the selection of the subjects of study. In the process of the intervention, every year there were many people participating in the intervention project. And many people left the project. Only studying people who insisted on the intervention and health examination could overlook the characteristics of the group that quit midway. Moreover, information bias could have partly influenced our results because the staff and instrument used in the 2 health examinations were different. Therefore, it is necessary to design randomized controlled trials to better evaluate the effect of the integrated traditional Chinese medicine and Western medicine MS intervention.
The main advantage of this study is the application and practice of the integrated traditional Chinese and Western medicine MS intervention in rural communities. It provides ideas and technology for future MS intervention and behavior modification practice.
Conclusions
Our integrated traditional Chinese and Western medicine MS intervention was effective in deceasing most of the parameters of the syndrome, especially blood pressure, and it helped people to do more exercise. This program can be useful in similar populations. Further studies of MS interventions in rural communities should focus on how to solve the problem of compliance to improve the effect of the intervention.
Footnotes
Source of support: This study was funded by cooperative agreement number 70973018 from the National Natural Science Foundation of China
References
- 1.Alberti KG, Zimmet P, Shaw J. The metabolic syndrome – a new worldwide definition. Lancet. 2005;366(9491):1059–62. doi: 10.1016/S0140-6736(05)67402-8. [DOI] [PubMed] [Google Scholar]
- 2.Xi B, He D, Hu Y, Zhou D. Prevalence of metabolic syndrome and its influencing factors among the Chinese adults: The China Health and Nutrition Survey in 2009. Prev Med. 2013;57(6):867–71. doi: 10.1016/j.ypmed.2013.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roglic G, Unwin N, Bennett PH, et al. The burden of mortality attributable to diabetes: realistic estimates for the year 2000. Diabetes Care. 2005;28(9):2130–35. doi: 10.2337/diacare.28.9.2130. [DOI] [PubMed] [Google Scholar]
- 4.He J, Gu D, Chen J, et al. Premature deaths attributable to blood pressure in China: a prospective cohort study. Lancet. 2009;374(9703):1765–72. doi: 10.1016/S0140-6736(09)61199-5. [DOI] [PubMed] [Google Scholar]
- 5.Kang WM, Zhang JS, Wang MS, et al. Prevalence of metabolic syndrome and its associations with other metabolic disorders and cardiovascular changes in health examination population in Beijing. Chin Med Sci J. 2009;24(4):227–30. doi: 10.1016/s1001-9294(10)60006-5. [DOI] [PubMed] [Google Scholar]
- 6.Kang JS, Kang HS, Jeong Y. A Web-based health promotion program for patients with metabolic syndrome. Asian Nurs Res (Korean Soc Nurs Sci) 2014;8(1):82–89. doi: 10.1016/j.anr.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 7.Chen YC, Tsao LI, Huang CH, et al. An Internet-based health management platform may effectively reduce the risk factors of metabolic syndrome among career women. Taiwan J Obstet Gynecol. 2013;52(2):215–21. doi: 10.1016/j.tjog.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 8.Yoo S, Kim H, Cho H-I. Improvements in the metabolic syndrome and stages of change for lifestyle behaviors in Korean older adults. Osong Public Health Res Perspect. 2012;3(2):85–93. doi: 10.1016/j.phrp.2012.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.den Boer AT, Herraets IJ, Stegen J, et al. Prevention of the metabolic syndrome in IGT subjects in a lifestyle intervention: Results from the SLIM study. Nutr Metab Cardiovasc Dis. 2013;23(11):1147–53. doi: 10.1016/j.numecd.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 10.Gerstel E, Pataky Z, Busnel C, et al. Impact of lifestyle intervention on body weight and the metabolic syndrome in home-care providers. Diabetes Metab. 2013;39(1):78–84. doi: 10.1016/j.diabet.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 11.Bihan H, Takbou K, Cohen R, et al. Impact of short-duration lifestyle intervention in collaboration with general practitioners in patients with the metabolic syndrome. Diabetes Metab. 2009;35(3):185–91. doi: 10.1016/j.diabet.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 12.Long H, Tang G, Li X, Heilig GK. Socio-economic driving forces of land-use change in Kunshan, the Yangtze River Delta economic area of China. J Environ Manage. 2007;83(3):351–64. doi: 10.1016/j.jenvman.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 13.Abuaisha BB, Costanzi JB, Boulton AJ. Acupuncture for the treatment of chronic painful peripheral diabetic neuropathy: a long-term study. Diabetes Res Clin Pract. 1998;39(2):115–21. doi: 10.1016/s0168-8227(97)00123-x. [DOI] [PubMed] [Google Scholar]
- 14.Li WL, Zheng HC, Bukuru J, De Kimpe N. Natural medicines used in the traditional Chinese medical system for therapy of diabetes mellitus. J Ethnopharmacol. 2004;92(1):1–21. doi: 10.1016/j.jep.2003.12.031. [DOI] [PubMed] [Google Scholar]
- 15.Wang J, Xiong X, Liu W. Acupuncture for essential hypertension. Int J Cardiol. 2013;169(5):317–26. doi: 10.1016/j.ijcard.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 16.Xie W, Zhao Y, Du L. Emerging approaches of traditional Chinese medicine formulas for the treatment of hyperlipidemia. J Ethnopharmacol. 2012;140(2):345–67. doi: 10.1016/j.jep.2012.01.027. [DOI] [PubMed] [Google Scholar]
- 17.Zhang H, Tan C, Wang H, et al. Study on the history of Traditional Chinese Medicine to treat diabetes. European Journal of Integrative Medicine. 2010;2(1):41–46. [Google Scholar]