Abstract
The aim of the current study was to localize the epileptic focus and characterize its causal relation with other brain regions, to understand the cognitive deficits in children with benign childhood epilepsy with centrotemporal spikes (BECTS). Resting-state functional magnetic resonance imaging (fMRI) was performed in 37 children with BECTS and 25 children matched for age, sex and educational achievement. We identified the potential epileptogenic zone (EZ) by comparing the amplitude of low frequency fluctuation (ALFF) of spontaneous blood oxygenation level dependent fMRI signals between the groups. Granger causality analysis was applied to explore the causal effect between EZ and the whole brain. Compared with controls, children with BECTS had significantly increased ALFF in the right postcentral gyrus and bilateral calcarine, and decreased ALFF in the left anterior cingulate cortex, bilateral putaman/caudate, and left cerebellum. ALFF values in the putaman/caudate were positively correlated with verbal IQ scores in patients. The ALFF values in cerebellum and performance IQ scores were negatively correlated in patients. These results suggest that ALFF disturbances in the putaman/caudate and cerebellum play an important role in BECTS cognitive dysfunction. Compared with controls, the patients showed increased driving effect from the EZ to the right medial frontal cortex and posterior cingulate cortex and decreased causal effects from the EZ to left inferior frontal gyrus. The causal effect of the left inferior frontal gyrus negatively correlated with disease duration, which suggests a relation between the epileptiform activity and language impairment. All together, these findings provide additional insight into the neurophysiological mechanisms of epilepitogenisis and cognitive dysfunction associated with BECTS.
Introduction
Benign childhood epilepsy with centrotemporal spikes (BECTS) (also known as rolandic epilepsy) is the most common form of idiopathic focal epilepsy syndrome in childhood [1]. BECTS is not correlated with any brain lesion and may be genetically determined. Its onset is between the ages of 1 and 14 years, with a peak at 7–10 years, usually followed by recovery during adolescence [2]. Given these characteristics, BECTS is classically considered a benign condition. However, there is accumulating evidence that BECTS can present with a variety of cognitive comorbidities including: language dysfunction [3–6], attention deficit [7–9], and difficulty with spatial perception [10] and memory and phonological awareness [11]. These findings suggest that seizures also affect cognitive function during interictal periods in children with BECTS, but the underlying mechanism of this cognitive impairment remains to be elucidated.
Resting-state functional magnetic resonance imaging (fMRI) has been used extensively to study functional brain activity in various types of epilepsy free of specifically designed behavioral tasks [12–17]. Amplitude of low-frequency fluctuation (ALFF) is a useful tool for depicting local brain activity. ALFF measures the magnitude of spontaneous blood oxygenation level dependent (BOLD) activity of each voxel; reflects brain activity level during a given period of time; and may be similar to positron emission tomography measurement [18,19]. In temporal lobe epilepsy, it has been demonstrated that ALFF is useful for localizing epileptic focus in the mesial temporal lobe, and other cortical and subcortical structures associated with cognitive impairment [20,21]. Additionally, increased ALFF is positively correlated with the number of epileptic discharges [20], and reflects the BOLD activation induced by epileptic activity [2]. We hypothesized that ALFF can identify the increased activity of the epileptic focus of BECTS, which is mainly located in the inferior part of the rolandic area.
ALFF can provide information regarding regional spontaneous activity, and functional connectivity measures the synchronicity of neuronal activity signals among regions of the brain. They may complement each other and provide more information about the underlying processes resulting in changes in resting-state brain function. It has recently been demonstrated that functional connectivity is reduced between the sensorimotor and language networks in children with BECTS [22,23]. Concordant abnormalities in structural connectivity have also been found in this type of childhood epilepsy [24]. Functional connectivity estimated the functional integrate between brain regions. But it ignored an important point to understand epilepsy—the direction of information flow. The abnormal driving effect from epileptogenic zone (EZ) to other functional areas could be a major reason of multiple clinic syndromes in epilepsy patients. Granger causality analysis (GCA) is a prominent technique for inferring the direction of information flow in brain networks [25–27]. It enabled us to understand better how seizure activity initiates, propagates and terminates [28].
The aim of the current study was to reveal the underlying mechanism of epileptogenesis and the cognitive deficit associated with BECTS. We adopted ALFF to identify the possible EZ of BECTS, and utilized GCA to test directly the direction and magnitude of influence between the EZ and other brain regions. All the observed abnormality would be correlated with cognitive estimations in BECTS patients.
Materials and Methods
Participants
This study involved 37 children with BECTS aged 7.1–13.5 years and 25 healthy volunteers aged 7.6–12.4 years, who were all attending regular schools. The mean and standard deviation of the ages in these two groups of children were, 9.8 ± 1.5 years and 10.0 ± 1.5 years, respectively. None of the healthy controls had a history of dyslexia, learning disorders or psychiatric disorders. There were no significant differences between patients and healthy controls for age (P = 0.522) or sex distribution (BECTS, 46% male; healthy controls, 60% male; P = 0.570). The inclusion criteria for patients were as follows: (1) diagnosed with BECTS according to the current diagnostic criteria [29]; (2) no other neurological disease; (3) no abnormality in routine structural MRI examinations; (4) aged 7–14 years; and (5) full-scale IQ (FSIQ) >70. Thirty six patients were right-handed and one was left-handed; 23 healthy controls were right-handed and two left-handed. Thirty-three patients had not received any antiepileptic drugs, three had received one antiepileptic drug, and another three antiepileptic drugs. The mean duration of epilepsy from onset to time of scanning was 12.2 ± 13.3 months (range 0.1–56 months).
Ethics Statement
This study was approved by the Beijing Children’s Hospital Subcommittee on Human Studies. All study subjects and parents (or guardians) gave written informed consent prior to participation.
Neuropsychological tests
Twenty-four children with epilepsy and 18 controls were administered the Wechsler Intelligence Scale for Children China-Revised (WISC-CR) test, which included FSIQ, verbal IQ (VIQ), and performance IQ (PIQ).
fMRI data acquisition
We performed functional and structural neuroimaging in children with BECTS and healthy controls using a Siemens Trio 3T scanner at Beijing 306 Hospital. We acquired resting-state functional images using a single-shot, gradient-recalled echo planar imaging sequence (2000 ms repetition time, 30 ms echo time, 90° flip angle, 210×210 mm2 field of view, 64×64 in-plane matrix, 4 mm slice thickness, 0.8 mm interslice gap, 3.3 × 3.3 × 4 mm3 voxel size, and 30 transverse slices aligned along the anterior–posterior commissure). We instructed subjects simply to rest, not to think of anything in particular, and not to fall asleep. Subsequently, we acquired high-resolution T1-weighted anatomical images in sagittal orientation using a magnetization-prepared rapid gradient-echo sequence (2300 ms repetition time, 2.98 ms echo time, 9° flip angle, 240 × 256 mm2 field of view, 256 × 256 in-plane matrix, 1 mm slice thickness, 0.5 mm interslice gap, 1 × 1 × 1 mm3 voxel size, and 176 slices).
fMRI data processing
Functional image preprocessing was carried out using the Data Processing Assistant for Resting-State fMRI (DPARSF; http://www.restfmri.net) [30], which synthesizes procedures in the Resting State fMRI Data Analysis Toolkit (REST; http://www.restfmri.net) [31] and Statistical Parametric Mapping (SPM8; www.fil.ion.ucl.ac.uk/spm). The first 10 images were excluded to ensure steady-state longitudinal magnetization, and the remaining images were then corrected for temporal differences and head motion. After subject selection, neither translation nor rotation parameters in any given data set exceeded ±3 mm or ±3°. We warped the functional images into a standard stereotaxic space at a resolution of 3 × 3 × 3 mm3, using the Montreal Neurological Institute (MNI) echo-planar imaging template, and then we spatially smoothed them with a 6-mm full-width half-maximum isotropic Gaussian kernel. Finally, we removed linear trends from the time courses, performed temporal band-pass filtering (0.01–0.08 Hz), and regressed out 9 nuisance signals (global mean, white matter, cerebrospinal fluid signals, and 6 head-motion parameters).
ALFF analysis
ALFF was defined as the averaged square root of activity in the low-frequency band (0.01–0.08 Hz) [18]. ALFF value of each voxel was standardized by dividing the full-brain mean ALFF values. Two-sample t tests were used to compare the differences in ALFF between the patients and controls. Using the REST AlphaSim program, a corrected significance level of P < 0.01 was obtained by clusters with a minimum volume of 1808 mm3 and individual voxel height threshold of P < 0.05.
GCA
A cluster showing abnormal ALFF was identified in rolandic area, the peak voxel (with a 3-mm radius) in this cluster was used as the seed region for the following GCA. The voxel-wise coefficient GCA [32] was performed in the whole brain using REST-GCA, a plug-in implemented in REST software [33]. We applied bivariate coefficient GCA to investigate the causal relation between the EZ and each voxel in the entire brain [21]. To explore the driving effect from the seed (EZ) to whole brain, one-sample t tests were performed for the causal effects within each group, with an uncorrected significance level of P < 0.05. The resulting maps of the two groups were combined and taken as a causal effect mask. Two-sample t tests were performed on the causal effects between groups within the causal effect mask with an AlphaSim-corrected significance level of P < 0.05 (height threshold, P < 0.01; extent threshold k = 432 mm3). The analysis for the driving effect from whole brain to seed (EZ) was performed in the same way as the seed (EZ) to whole brain.
To explore whether the neuroimaging measures correlate with the disease features in BECTS children, Pearson correlation was performed between causal effect/ALFF and disease duration/IQ scores at the peak voxel of clusters from the between-group analysis.
Results
Neuropsychological testing
Table 1 shows the demographic, clinical and neuropsychological characteristics of the patients with BECTS and healthy controls. FSIQ of the patients with BECTS was significantly lower than that of the control group (t = -2.39, P = 0.024). The PIQ scores did not differ significantly between the patients with BECTS and the healthy controls (t = -1.55, P = 0.13). The VIQ scores in the children with BECTS were significantly lower than those in the control group (t = -2.49, P = 0.021).
Table 1. Demographic, clinical, and neuropsychological characteristics of BECTS patients and healthy controls.
| Characteristic | Patients | Controls | t/χ2 | P value |
|---|---|---|---|---|
| Age (years) | 9.8±1.5 | 10.0±1.5 | -0.645 | 0.522 a |
| Sex (female/male) | 19/18 | 11/14 | 0.323 | 0.570 b |
| FSIQ | 90.50±9.22 | 100.56±15.94 | -2.39 | 0.024 a |
| VIQ | 91.75±8.24 | 103.44±18.64 | -2.49 | 0.021 a |
| PIQ | 91.17±11.37 | 96.94±12.77 | -1.55 | 0.130 a |
| Duration (months) | 12.2±13.3 | NA | – |
The intelligence quotient (IQ) scores in patients and controls were based on the results of 24 and 18 participants, respectively. FSIQ = full scale IQ; VIQ = verbal IQ; PIQ = performance IQ. NA, not available.
aTwo-sample t test.
bχ2 test.
Between-group analysis of ALFF
As compared with the healthy controls, the patients with BECTS showed significantly increased ALFF in the right postcentral gyrus and bilateral calcarine (P < 0.05 corrected) (Table 2 and Fig 1). Brain regions showing decreased ALFF included the left anterior cingulate cortex (ACC), bilateral putamen/caudate and left cerebellum (P < 0.05 corrected) (Table 2 and Fig 1).
Table 2. Regions showing abnormal amplitude of low-frequency fluctuation in patients.
| Brain region | MNI | BA | Cluster size (mm3) | Peak t value |
|---|---|---|---|---|
| Postcentral gyrus R. | 63, -9, 18 | 3 | 1323 | 4.23 |
| Calcarine L. | -18, -72, 9 | 17 | 3024 | 3.94 |
| Calcarine R. | 21, -72, 15 | 18 | 2268 | 4.07 |
| ACC L. | -6, 42, 3 | 32 | 2592 | -4.63 |
| Putaman/caudate L. | -21, 15, -9 | NA | 1728 | -3.87 |
| Putaman/caudate R. | 18, 18, -9 | NA | 3186 | -5.30 |
| Cerebellum L. | -6, -78, -48 | NA | 7992 | -4.56 |
ACC = anterior cingulate cortex; L = left side; MNI = Montreal Neurological Institute; R = right side;NA, not available.
Fig 1. Brain regions showing abnormal ALFF in patients with BECTS.
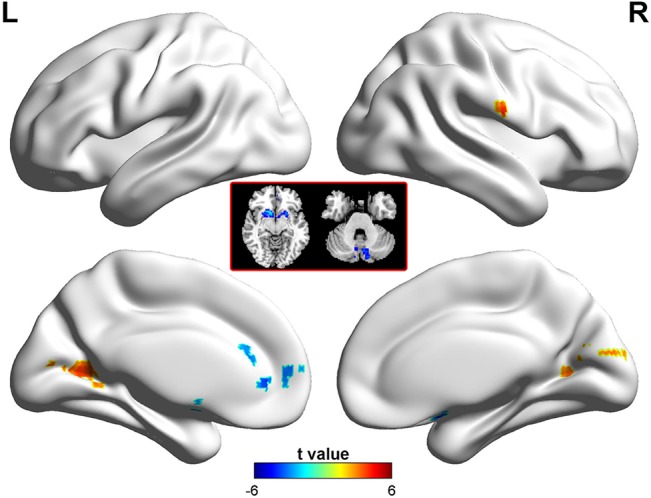
The warm (red) and cold (blue) colors represent higher and lower ALFF, respectively, in patients compared with controls (P<0.05, corrected). Color bar represents t values.
Voxel-wise GCA
Seed-to-whole-brain analysis
Widespread cortical and subcortical structures were driven by the seed region in patients with BECTS (Fig 2A). The pattern in the healthy controls (Fig 2B) was clearly distinct from that in the patients. Compared with healthy controls, the patients showed an increased driving effect from EZ to the right medial frontal cortex (BA8) and posterior cingulate cortex (PCC) (Fig 2C and Table 3), and a decreased causal effects from EZ to the left inferior frontal gyrus (BA9/44/45/46) (Fig 2C and Table 3).
Fig 2. Voxel-wise GCA.
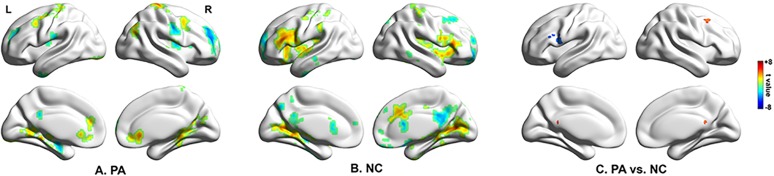
(A) Regions showing significant causal effect with the seed in patients. (B) Regions showing significant causal effect with the seed in controls. (C) Regions showing abnormal causal effect with the seed in patients compared with controls. Color bar represents t values. NC = normal control; PA = patient.
Table 3. Regions showing abnormal causal effect with epileptogenic zone in patients (seed-to-whole-brain).
| Brain region | MNI | BA | Volume (mm3) | Peak t value | BECTS | NC |
|---|---|---|---|---|---|---|
| MFG R | 45, 12, 51 | 8 | 1620 | 4.02 | 3.53* | -2.27* |
| PCC | 0, -48, 18 | 23 | 459 | 3.75 | 1.22 | -3.83* |
| IFG L | -57, 6, 18 | 44/9 | 2133 | -4.45 | -3.79* | 2.62* |
| IFG L | -39, 21, 21 | 45/46 | 1053 | -3.67 | -0.15 | 4.43* |
| WM | -42, -3, 18 | NA | 1188 | -3.98 | -3.49* | 2.32 |
The last two columns show the t value of the corresponding peak voxel within the patient and control group, respectively. Values with an asterisk show that the mean causal effect of the corresponding cluster is significantly different from zero. BA = Brodmann’s area; IFG = inferior frontal gyrus; L = left side; PCC = posterior cingulate cortex, R = right side; MNI = Montreal Neurological Institute coordinate; NC = normal control; WM = white matter;NA, not available.
Whole-brain-to-seed analysis
Whole-brain-to-seed analysis showed that there was no abnormal positive or negative driving effect from whole brain to seed in the patients with BECTS.
Correlation analysis
A positive correlation was identified for ALFF values in the putamen/caudate and VIQ scores (r = 0.521, P = 0.009) (Fig 3A). In contrast, the cerebellum and PIQ scores showed a negative correlation (r = −0.441, P = 0.031) (Fig 3B). The causal effect from EZ to the left inferior frontal gyrus (r = −0.393, P = 0.02) was negatively correlated with disease duration (Fig 3C). These associations were absent in the healthy controls.
Fig 3. Correlation between fMRI measures and cognitive estimation or disease duration.
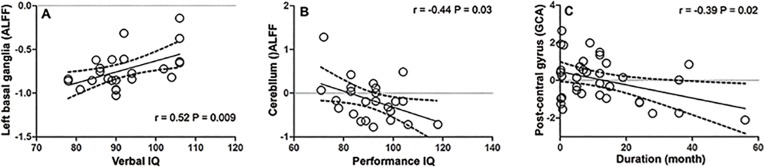
(A) A positive correlation was identified for ALFF values in the putamen/caudate and VIQ scores. There were four children had same scores of verbal IQ(90), 4 points overlapping together, so there were only 22 points in the this figure. (B) The cerebellum and PIQ scores showed a negative correlation. (C) The causal effect from EZ to the left inferior frontal gyrus was negatively correlated with disease duration.
Discussion
In the current study, we localized the possible EZ of BECTS, and characterized the causal effect between EZ and the whole brain. We found that the possible EZ of BECTS not only showed abnormal increased local activity but also had abnormal driving effects to other brain areas.Findings of correlation analysis suggested that these disrupted brain activities were related to the abnormal cognitive functions.
This study identified that ALFF pattern in children with BECTS was altered compared to that in healthy controls.We found increased ALFF in the right postcentral gyrus, a presumed location of the generator of the epileptic discharges as supported by the findings of previous electroencephalography–fMRI studies [34–37]. We propose that the occipital activations (bilateral calcarine cortex) detected in our study might reflect some internally evoked secondary response of the brain to the initial spike event.
We consider decreased ALFF in the ACC, putamen/caudate and cerebellum to be responsible for functional impairments in cognitive processes in children with BECTS.
The ACC is involved in attention and concentration [38]. fMRI demonstrates ACC activation in executive control of attention [39], and conflict monitoring in the engagement of cognitive control [40]. One recent fMRI study of sustained attention demonstrated bilateral ACC activation, and a correlation between worse performance and lower BOLD signal in the ACC [41]. Moreover, a novel conflict monitoring task has been used to assess the effects on cognitive control of excitotoxic lesions in the ACC in rats. The animals with ACC lesions had difficulty in adjusting cognitive control [42]. Children with BECTS have sustained attention difficulties [7,43–45]. We infer that this decreased ALFF in the ACC may explain the attention deficit that is a common symptom in BECTS.
A particularly interesting finding in the current study was decreased ALFF in the putamen/caudate in children with BECTS, and a positive correlation was seen between ALFF values in the putamen/caudate VIQ score. The involvement of the basal ganglia has been demonstrated in focal and generalized epilepsy [46–48]. The basal ganglia were previously thought to be primarily involved in motor control, however, more recent evidence from neuropsychological and neuroimaging studies suggests that the basal ganglia also support language processing [49]. The striatal dopaminergic system plays an essential role in grammatical processes that form the core of human language [50]. The putamen plays a special role in reading but this is likely to vary with individual reading preferences and strategies [51]. Dysfunction particularly related to language has been reported in BECTS [3–6,52–54]. In the current study, we found that children with BECTS had a significantly lower VIQ score, which agrees with previous studies [55,56]. In the current study, there were decreased ALFF values in the putamen/caudate in children with BECTS, along with a correlation between these decreased ALFF values and VIQ scores. These results suggest that abnormal spontaneous neural activity in the basal ganglia may play a role in BECTS-related language dysfunction. One recent study found children with BECTS demonstrated significant putamen hypertrophy [57]. This finding, with combined our results, suggests that a structural abnormality underlies the functional abnormality in basal ganglia in BECTS. Additionally, the altered structural features in basal ganglia was also reported in children with absence seizures[58] As both absence epilepsy and BECTS are childhood onset and most patients of them become seizure free after adulthood, we speculate the basal ganglia may be a common target for epileptic patients with abnormal neurodevelopment.
Like basal ganglia, decreased ALFF values were also found in the cerebellum in children with BECTS. The involvement of the cerebellum in a wide range of cognitive functions has been found in many studies [59–61]. In addition, decreased ALFF values in the cerebellum were found to be negatively correlated with PIQ scores in children with BECTS. Whether these decreased cerebellar ALFF values were part of a compensatory mechanism limited progression of cognitive decline in BECTS remains to be determined in longitudinal studies.
After we identified the EZ (postcentral gyrus) by ALFF, we utilized coefficient-based GCA to obtain information about the flow directions and magnitude between the EZ (postcentral gyrus) and the whole brain. Unlike the residual-based GCA, this novel GCA method can characterize not only the positive causality but also negative causality. These two kinds of causalities may represent inhibitory and excitatory effect in physiology and have shed new light on the pathophysiology of several disorders [21,62,63]. Here, the predominant finding was that the abnormal causal effect in BECTS is unidirectional (seed to whole brain), without abnormal feedback (whole brain to seed). Compared with controls, patients demonstrated a decreased driving effect from the EZ to the inferior frontal gyrus (BA44/9, BA 45/46). Furthermore, we found that the abnormal driving effect from the EZ to the inferior frontal gyrus (BA 45/46) in patients was negatively correlated with disease duration. The traditional Broca’s area usually refers to the pars triangularis (BA 45) and pars opercularis (BA 44) of the inferior frontal gyrus. Broca’s area is one of the essential nodes in the language network. Evidence shows that BA 45 is implicated in semantic processing, while BA 44 is involved in phonological and syntactic processing [64]. Recent studies have demonstrated reduced functional connectivity between the sensorimotor network and the inferior frontal gyrus (Broca’s area) in children with BECTS [22,23], although the directions of information flow have been overlooked. For the first time, we identified a decreased driving effect from the EZ to Broca’s area in children with BECTS, and this agrees with the decreased VIQ. Our results provide new evidence that epileptiform activity in BECTS may cause language impairment.
In the current study, the ipsilateral medial frontal cortex (BA8) and PCC showed an increased causal effect driven by the right postcentral gyrus. The medial frontal cortex has previously been implicated in action selection/outcome monitoring, behavioral adjustments and learning [65–67]; all of which are important in complex cognitive tasks such as language. The PCC is the main hub within the default network whose activation is greater at rest than during tasks [68]. Several studies have found decreased resting-state connectivity within the default network in patients with epilepsy [69–72]. Oser and coworkers [73] have provided evidence of abnormal functional integration of the default network in BECTS. We speculate that the increased causal effects driven by the EZ to the medial frontal cortex and PCC are compensatory reallocations for the neural system to compensate for cognitive deficits in BECTS. Future studies are needed to confirm this speculation.
The current study had several limitations. First, it was not a longitudinal survey, therefore, it is unknown if the ALFF values and causal effect alterations will normalize with seizure remission in BECTS. Second, although only 4 children received antiepileptic drugs, the effects of medications cannot be fully excluded. Ideally, these results need validation in drug-naïve patients. Third, we did not simultaneously perform electroencephalography during fMRI, thus we did not know to what extent the functional alteration was caused by interictal discharges. Fourth, clinically, the identification of a real EZ should be based on a comprehensive evaluation, including video-EEG, clinical characteristics or even surgery. Although previous studies found ALFF significantly correlated with epileptic activity, the ‘potential’ EZ found here through ALFF still need further validation. Fifth, the maintaining of normal brain function may be largely dependent on the interaction between multiple networks. To estimate the effect of epileptic network on brain function, a network based analytic strategy may be adopted as previous epilepsy studies [74].
In conclusion, we characterized the abnormal local activity and causal connectivity in patients with BECTS using resting-state fMRI data. The findings from ALFF suggested that the inferior part of postcentral gyrus may be the EZ of BECTS, and the putamen/caudate and cerebellum play an important role in the cognitive dysfunction of BECTS. GCA indicated a decreased driving effect from the EZ to Broca’s area in children with BECTS, which was negatively correlated with disease duration, giving new evidence that epileptiform activity in BECTS may cause language impairment. Our findings provide neuroimaging evidence of the neuropathophysiological mechanisms underlying the cognitive impairments in BECTS.
Acknowledgments
The authors would like to thank the help of Drs Xiaotun Ren, Junlan Lv,Changhong Ding, Chunhong Chen,Tongli Han and Weihua Zhang; the staff of the Department of Neurology,Beijing Children’s Hospital Affiliated to Capital Medical University; and the patients and volunteers for participating in this study.
Data Availability
All relevant data are within the paper.
Funding Statement
This work was supported by the Natural Science Foundation of China (Grant no. 81341041) to YW, National Key Basic Research Program of China (973 Program) 2012CB720704 to ZJ, Natural Science Foundation of China (Grant nos. 81401400 to GJ and 81471653 to WL), and the ‘Qian Jiang Distinguished Professor’ program to YZ. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Berg AT, Levy SR, Testa FM, Shinnar S. Classification of childhood epilepsy syndromes in newly diagnosed epilepsy: interrater agreement and reasons for disagreement. Epilepsia.1999; 40: 439–444. [DOI] [PubMed] [Google Scholar]
- 2. Panayiotopoulos CP, Michael M, Sanders S, Valeta T, Koutroumanidis M. Benign childhood focal epilepsies: assessment of established and newly recognized syndromes. Brain.2008; 131: 2264–2286. 10.1093/brain/awn162 [DOI] [PubMed] [Google Scholar]
- 3. Staden U, Isaacs E, Boyd SG, Brandl U, Neville BG. Language dysfunction in children with Rolandic epilepsy. Neuropediatrics.1998; 29: 242–248. [DOI] [PubMed] [Google Scholar]
- 4. Riva D, Vago C, Franceschetti S, Pantaleoni C, D'Arrigo S, Granata T, et al. Intellectual and language findings and their relationship to EEG characteristics in benign childhood epilepsy with centrotemporal spikes. Epilepsy Behav.2007; 10: 278–285. [DOI] [PubMed] [Google Scholar]
- 5. Monjauze C, Broadbent H, Boyd SG, Neville BG, Baldeweg T. Language deficits and altered hemispheric lateralization in young people in remission from BECTS. Epilepsia.2011; 52: e79–83. 10.1111/j.1528-1167.2011.03105.x [DOI] [PubMed] [Google Scholar]
- 6. Overvliet GM, Aldenkamp AP, Klinkenberg S, Vles JS, Hendriksen J. Impaired language performance as a precursor or consequence of Rolandic epilepsy? J Neurol Sci.2011; 304: 71–74. 10.1016/j.jns.2011.02.009 [DOI] [PubMed] [Google Scholar]
- 7. Cerminara C, D'Agati E, Lange KW, Kaunzinger I, Tucha O, Parisi P,et al. Benign childhood epilepsy with centrotemporal spikes and the multicomponent model of attention: a matched control study. Epilepsy Behav.2010; 19: 69–77. 10.1016/j.yebeh.2010.07.008 [DOI] [PubMed] [Google Scholar]
- 8. Bennett-Back O, Keren A, Zelnik N. Attention-deficit hyperactivity disorder in children with benign epilepsy and their siblings. Pediatr Neurol.2011; 44:187–192. 10.1016/j.pediatrneurol.2010.10.003 [DOI] [PubMed] [Google Scholar]
- 9. Bedoin N, Ciumas C, Lopez C, Redsand G, Herbillon V, Laurent A, et al. Disengagement and inhibition of visual-spatial attention are differently impaired in children with rolandic epilepsy and Panayiotopoulos syndrome. Epilepsy Behav.2012; 25: 81–91. 10.1016/j.yebeh.2012.05.025 [DOI] [PubMed] [Google Scholar]
- 10. Volkl-Kernstock S, Willinger U, Feucht M. Spacial perception and spatial memory in children with benign childhood epilepsy with centro-temporal spikes (BCECTS). Epilepsy Res.2006; 72: 39–48. [DOI] [PubMed] [Google Scholar]
- 11. Northcott E, Connolly AM, Berroya A, McIntyre J, Christie J, Taylor A, et al. Memory and phonological awareness in children with Benign Rolandic Epilepsy compared to a matched control group. Epilepsy Res.2007; 75: 57–62. [DOI] [PubMed] [Google Scholar]
- 12. Woodward KE, Gaxiola-Valdez I, Goodyear BG, Federico P. Frontal lobe epilepsy alters functional connections within the brain's motor network: a resting-state fMRI study. Brain Connect.2014; 4: 91–99. 10.1089/brain.2013.0178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Vaessen MJ, Jansen JF, Braakman HM, Hofman PA, De Louw A, Aldenkamp AP,et al. Functional and structural network impairment in childhood frontal lobe epilepsy. PLoS One.2014; 9: e90068 10.1371/journal.pone.0090068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lv ZX, Huang DH, Ye W, Chen ZR, Huang WL, Zheng JO. Alteration of functional connectivity within visuospatial working memory-related brain network in patients with right temporal lobe epilepsy: a resting-state fMRI study. Epilepsy Behav.2014; 35: 64–71. 10.1016/j.yebeh.2014.04.001 [DOI] [PubMed] [Google Scholar]
- 15. Haneef Z, Lenartowicz A, Yeh HJ, Levin HS, Engel J Jr, Stern JM. Functional connectivity of hippocampal networks in temporal lobe epilepsy. Epilepsia.2014; 55: 137–145. 10.1111/epi.12476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kay BP, DiFrancesco MW, Privitera MD, Gotman J, Holland SK, Szaflarski JP. Reduced default mode network connectivity in treatment-resistant idiopathic generalized epilepsy. Epilepsia.2013; 54: 461–470. 10.1111/epi.12057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yang T, Luo C, Li Q, Guo Z, Liu L, Gong Q, et al. Altered resting-state connectivity during interictal generalized spike-wave discharges in drug-naive childhood absence epilepsy. Hum Brain Mapp.2013; 34: 1761–1767. 10.1002/hbm.22025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zang YF, He Y, Zhu CZ, Cao QJ, Sui MQ, Liang M, et al. Altered baseline brain activity in children with ADHD revealed by resting-state functional MRI. Brain Dev.2007; 29: 83–91. [DOI] [PubMed] [Google Scholar]
- 19. Zuo XN, Di Martino A, Kelly C, Shehzad ZE, Gee DG, Klein DF, et al. The oscillating brain: complex and reliable. Neuroimage.2010; 49: 1432–1445. 10.1016/j.neuroimage.2009.09.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zhang Z, Lu G, Zhong Y, Tan Q, Chen H, Liao W, et al. fMRI study of mesial temporal lobe epilepsy using amplitude of low-frequency fluctuation analysis. Hum Brain Mapp.2010; 31: 1851–1861. 10.1002/hbm.20982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ji GJ, Zhang Z, Zhang H, Wang J, Liu DQ, Zang YF, et al. Disrupted causal connectivity in mesial temporal lobe epilepsy. PLoS One.2013; 8: e63183 10.1371/journal.pone.0063183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Besseling RM, Jansen JF, Overvliet GM, van der Kruijs SJ, Vles JS, Ebus SC, et al. Reduced functional integration of the sensorimotor and language network in rolandic epilepsy. Neuroimage Clin.2013; 2: 239–246. 10.1016/j.nicl.2013.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Besseling RM, Overvliet GM, Jansen JF, van der Kruijs SJ, Vles JS, Ebus SC, et al. Aberrant functional connectivity between motor and language networks in rolandic epilepsy. Epilepsy Res.2013; 107: 253–262. 10.1016/j.eplepsyres.2013.10.008 [DOI] [PubMed] [Google Scholar]
- 24. Besseling RM, Jansen JF, Overvliet GM, van der Kruijs SJ, Ebus SC, de Louw A, et al. Reduced structural connectivity between sensorimotor and language areas in rolandic epilepsy. PLoS One.2013; 8: e83568 10.1371/journal.pone.0083568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. David O, Guillemain I, Saillet S, Reyt S, Deransart C, Segebarth C, et al. Identifying neural drivers with functional MRI: an electrophysiological validation. PLoS Biol.2008; 6: 2683–2697. 10.1371/journal.pbio.0060315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Jenison RL. Directional Influence between the Human Amygdala and Orbitofrontal Cortex at the Time of Decision-Making. PLoS One.2014; 9: e109689 10.1371/journal.pone.0109689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Deshpande G, Hu X. Investigating effective brain connectivity from fMRI data: past findings and current issues with reference to Granger causality analysis. Brain Connect.2012; 2: 235–245. 10.1089/brain.2012.0091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cadotte AJ, Mareci TH, DeMarse TB, Parekh MB, Rajagovindan R, Ditto WL, et al. Temporal lobe epilepsy: anatomical and effective connectivity. IEEE Trans Neural Syst Rehabil Eng.2009; 17: 214–223. 10.1109/TNSRE.2008.2006220 [DOI] [PubMed] [Google Scholar]
- 29. ILAE.Proposal for revised classification of epilepsies and epileptic syndromes. Commission on Classification and Terminology of the International League Against Epilepsy. Epilepsia.1989; 30: 389–399. [DOI] [PubMed] [Google Scholar]
- 30. Chao-Gan Y, Yu-Feng Z. DPARSF: A MATLAB Toolbox for "Pipeline" Data Analysis of Resting-State fMRI. Front Syst Neurosci.2010: 4: 13 10.3389/fnsys.2010.00013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Song XW, Dong ZY, Long XY, Li SF, Zuo XN, Zhu CZ, et al. REST: a toolkit for resting-state functional magnetic resonance imaging data processing. PLoS One.2011; 6: e25031 10.1371/journal.pone.0025031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Chen G, Hamilton JP, Thomason ME, Gotlib IH, Saad ZS, Cox RW. Granger causality via vector auto-regression tuned for fMRI data analysis. Proc Intl Soc Mag Reson Med.2009; 17. [Google Scholar]
- 33. Zang ZX, Yan CG, Dong ZY, Huang J, Zang YF. Granger causality analysis implementation on MATLAB: a graphic user interface toolkit for fMRI data processing. J Neurosci Methods.2012; 203: 418–426. 10.1016/j.jneumeth.2011.10.006 [DOI] [PubMed] [Google Scholar]
- 34. Masterton RA, Harvey AS, Archer JS, Lillywhite LM, Abbott DF, Scheffer IE, et al. Focal epileptiform spikes do not show a canonical BOLD response in patients with benign rolandic epilepsy (BECTS). Neuroimage.2010; 51: 9. [DOI] [PubMed] [Google Scholar]
- 35. Archer JS, Briellman RS, Abbott DF, Syngeniotis A, Wellard RM, Jackson GD. Benign epilepsy with centro-temporal spikes: spike triggered fMRI shows somato-sensory cortex activity. Epilepsia.2003; 44: 200–204. [DOI] [PubMed] [Google Scholar]
- 36. Boor R, Jacobs J, Hinzmann A, Bauermann T, Scherg M, Boor S, et al. Combined spike-related functional MRI and multiple source analysis in the non-invasive spike localization of benign rolandic epilepsy. Clin Neurophysiol.2007; 118: 901–909. [DOI] [PubMed] [Google Scholar]
- 37. Lengler U, Kafadar I, Neubauer BA, Krakow K.fMRI correlates of interictal epileptic activity in patients with idiopathic benign focal epilepsy of childhood. A simultaneous EEG-functional MRI study. Epilepsy Res.2007; 75: 29–38. [DOI] [PubMed] [Google Scholar]
- 38. Bush G, Luu P, Posner MI.Cognitive and emotional influences in anterior cingulate cortex. Trends Cogn Sci.2000; 4: 215–222. [DOI] [PubMed] [Google Scholar]
- 39. Fan J, McCandliss BD, Fossella J, Flombaum JI, Posner MI. The activation of attentional networks. Neuroimage.2005; 26: 471–479. [DOI] [PubMed] [Google Scholar]
- 40. Kerns JG, Cohen JD, MacDonald AW 3rd, Cho RY, Stenger VA, Carter CS. Anterior cingulate conflict monitoring and adjustments in control. Science.2004; 303: 1023–1026. [DOI] [PubMed] [Google Scholar]
- 41. Tana MG, Montin E, Cerutti S, Bianchi AM. Exploring cortical attentional system by using fMRI during a Continuous Perfomance Test. Comput Intell Neurosci. 2010:329213 10.1155/2010/329213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Newman LA, Creer DJ, McGaughy JA. Cognitive control and the anterior cingulate cortex: How conflicting stimuli affect attentional control in the rat. J Physiol Paris. 2014. July 19 pii: S0928-4257(14)00027-8. 10.1016/j.jphysparis.2014.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Deltour L, Quaglino V, Barathon M, De Broca A, Berquin P. Clinical evaluation of attentional processes in children with benign childhood epilepsy with centrotemporal spikes (BCECTS). Epileptic Disord.2007; 9: 424–431. [DOI] [PubMed] [Google Scholar]
- 44. Kim EH, Yum MS, Kim HW, Ko TS. Attention-deficit/hyperactivity disorder and attention impairment in children with benign childhood epilepsy with centrotemporal spikes. Epilepsy Behav.2014; 37: 54–58. 10.1016/j.yebeh.2014.05.030 [DOI] [PubMed] [Google Scholar]
- 45. Sanchez-Carpintero R, Neville BG.Attentional ability in children with epilepsy. Epilepsia.2003; 44: 1340–1349. [DOI] [PubMed] [Google Scholar]
- 46. Rektor I, Kuba R, Brazdil M, Chrastina J. Do the basal ganglia inhibit seizure activity in temporal lobe epilepsy? Epilepsy Behav.2012; 25: 56–59. 10.1016/j.yebeh.2012.04.125 [DOI] [PubMed] [Google Scholar]
- 47. Rektor I, Tomčík J, Mikl M, Mareček R, Brázdil M, Rektorová I. Association between the basal ganglia and large-scale brain networks in epilepsy. Brain Topogr.2013; 26: 355–362. 10.1007/s10548-012-0272-8 [DOI] [PubMed] [Google Scholar]
- 48. Moeller F, Siebner HR, Wolff S, Muhle H, Boor R, Granert O. Changes in activity of striato-thalamo-cortical network precede generalized spike wave discharges. Neuroimage.2008; 39: 1839–1849. [DOI] [PubMed] [Google Scholar]
- 49. Chan SH, Ryan L, Bever TG.Role of the striatum in language: Syntactic and conceptual sequencing. Brain Lang.2013; 125: 283–294. 10.1016/j.bandl.2011.11.005 [DOI] [PubMed] [Google Scholar]
- 50. Tettamanti M, Moro A, Messa C, Moresco RM, Rizzo G, Carpinelli A, et al. Basal ganglia and language: phonology modulates dopaminergic release. Neuroreport.2005; 16: 397–401. [DOI] [PubMed] [Google Scholar]
- 51. Seghier ML, Price CJ.Reading aloud boosts connectivity through the putamen. Cereb Cortex.2010; 20: 570–582. 10.1093/cercor/bhp123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Pinton F, Ducot B, Motte J, Arbues AS, Barondiot C, Barthez MA, et al. Cognitive functions in children with benign childhood epilepsy with centrotemporal spikes (BECTS). Epileptic Disord.2006; 8: 11–23. [PubMed] [Google Scholar]
- 53. Clarke T, Strug LJ, Murphy PL, Bali B, Carvalho J, et al. High risk of reading disability and speech sound disorder in rolandic epilepsy families: case-control study. Epilepsia.2007; 48: 2258–2265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Bedoin N, Ferragne E, Lopez C, Herbillon V, De Bellescize J, Foster S, et al. Atypical hemispheric asymmetries for the processing of phonological features in children with rolandic epilepsy. Epilepsy Behav.2011; 21: 42–51. 10.1016/j.yebeh.2011.02.026 [DOI] [PubMed] [Google Scholar]
- 55. Liu X, Zhang X, Han Q, Guo J, Wang C.Cognition in Chinese children with benign childhood epilepsy with centrotemporal spikes (BCECTS). Neurosci Lett.2012; 507: 1–4. 10.1016/j.neulet.2011.10.016 [DOI] [PubMed] [Google Scholar]
- 56. Tang YL, Ji GJ, Yu Y, Wang J, Wang ZJ, Zang YF, et al. Altered regional homogeneity in rolandic epilepsy: a resting-state FMRI study. Biomed Res Int. 2014;2014:960395 10.1155/2014/960395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Lin JJ, Riley JD, Hsu DA, Stafstrom CE, Dabbs K, Becker T, et al. Striatal hypertrophy and its cognitive effects in new-onset benign epilepsy with centrotemporal spikes. Epilepsia.2012; 53: 677–685. 10.1111/j.1528-1167.2012.03422.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Luo C, Xia Y, Li Q, Xue K, Lai Y, Gong Q, et al. Diffusion and volumetry abnormalities in subcortical nuclei of patients with absence seizures. Epilepsia. 2011; 52(6):1092–1099 10.1111/j.1528-1167.2011.03045.x [DOI] [PubMed] [Google Scholar]
- 59. Tedesco AM, Chiricozzi FR, Clausi S, Lupo M, Molinari M, Leggio MG. The cerebellar cognitive profile. Brain.2011;134: 3672–3686. 10.1093/brain/awr266 [DOI] [PubMed] [Google Scholar]
- 60. Stoodley CJ, Valera EM, Schmahmann JD. Functional topography of the cerebellum for motor and cognitive tasks: an fMRI study. Neuroimage.2012; 59: 1560–1570. 10.1016/j.neuroimage.2011.08.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Koziol LF, Budding D, Andreasen N, D'Arrigo S, Bulgheroni S, Imamizu H, et al. Consensus paper: the cerebellum's role in movement and cognition. Cerebellum.2014; 13: 151–177. 10.1007/s12311-013-0511-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Hamilton JP, Chen G, Thomason ME, Schwartz ME, Gotlib IH. Investigating neural primacy in Major Depressive Disorder: multivariate Granger causality analysis of resting-state fMRI time-series data. Mol Psychiatry.2011; 16: 763–772. 10.1038/mp.2010.46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Palaniyappan L, Simmonite M, White TP, Liddle EB, Liddle PF. Neural primacy of the salience processing system in schizophrenia. Neuron.2013; 79: 814–828. 10.1016/j.neuron.2013.06.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Amunts K, Weiss PH, Mohlberg H, Pieperhoff P, Eickhoff S, Gurd JM, et al. Analysis of neural mechanisms underlying verbal fluency in cytoarchitectonically defined stereotaxic space—the roles of Brodmann areas 44 and 45. Neuroimage.2004; 22: 42–56. [DOI] [PubMed] [Google Scholar]
- 65. Ridderinkhof KR, Ullsperger M, Crone EA, Nieuwenhuis S. The role of the medial frontal cortex in cognitive control. Science.2004; 306: 443–447. [DOI] [PubMed] [Google Scholar]
- 66. Rushworth MF, Walton ME, Kennerley SW, Bannerman DM.Action sets and decisions in the medial frontal cortex. Trends Cogn Sci.2004; 8: 410–417. [DOI] [PubMed] [Google Scholar]
- 67. Rushworth MF, Buckley MJ, Behrens TE, Walton ME, Bannerman DM. Functional organization of the medial frontal cortex. Curr Opin Neurobiol.2007; 17: 220–227. [DOI] [PubMed] [Google Scholar]
- 68. Buckner RL, Andrews-Hanna JR, Schacter DL. The brain's default network: anatomy, function, and relevance to disease. Ann N Y Acad Sci.2008; 1124: 1–38. 10.1196/annals.1440.011 [DOI] [PubMed] [Google Scholar]
- 69. McGill ML, Devinsky O, Kelly C, Milham M, Castellanos FX, Quinn BT, et al. Default mode network abnormalities in idiopathic generalized epilepsy. Epilepsy Behav.2012; 23: 353–359. 10.1016/j.yebeh.2012.01.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Song M, Du H, Wu N, Hou B, Wu G, Wang J, et al. Impaired resting-state functional integrations within default mode network of generalized tonic-clonic seizures epilepsy. PLoS One.2011; 6: e17294 10.1371/journal.pone.0017294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Luo C, Li Q, Lai Y, Xia Y, Qin Y, Liao W, et al. Altered functional connectivity in default mode network in absence epilepsy: a resting-state fMRI study. Hum Brain Mapp.2011; 32: 438–449. 10.1002/hbm.21034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Haneef Z, Lenartowicz A, Yeh HJ, Engel J Jr, Stern JM. Effect of lateralized temporal lobe epilepsy on the default mode network. Epilepsy Behav.2012; 25: 350–357. 10.1016/j.yebeh.2012.07.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Oser N, Hubacher M, Specht K, Datta AN, Weber P, Penner IK (2014) Default mode network alterations during language task performance in children with benign epilepsy with centrotemporal spikes (BECTS). Epilepsy Behav.2014; 33: 12–17. 10.1016/j.yebeh.2014.01.008 [DOI] [PubMed] [Google Scholar]
- 74. Luo C, Qiu C, Guo Z, Fang J, Li Q, Lei X, et al. Disrupted functional brain connectivity in partial epilepsy: a resting-state fMRI study. PLoS One.2011; 7: e28196 10.1371/journal.pone.0028196 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.


