Abstract
Background
Hybrid coronary revascularization (HCR) and off-pump coronary artery bypass grafting (OPCABG) are both feasible, less invasive techniques for coronary revascularization. Although both techniques utilize the left internal mammary artery to left anterior descending artery graft, HCR uses drug-eluting stents instead of saphenous vein bypass. It remains unclear whether HCR is equal to, better or worse than OPCABG.
Methods and results
A meta-analysis was carried out using a random-effects model. Seven observational studies were included. There was no significant difference either in in-hospital mortality [relative risk (RR) 0.57, 95% confidence interval (CI) 0.13–2.59, P=0.47] or in the MACCE rate (RR 0.63, 95% CI 0.24–1.64, P=0.34) between the HCR group and the OPCABG group. A significant difference was observed between the two groups in the length of hospitalization (RR 0.55, 95% CI 0.13–0.97, P=0.01), length of ICU stay (RR 0.45, 95% CI 0.10–0.80, P<0.05), intubation time (RR 0.48, 95% CI 0.13–0.84, P<0.01), need for red blood transfusion (RR 0.67, 95% CI 0.56–0.82, P<0.001), and total in-hospital costs (RR 0.90, 95% CI 0.39–1.42, P<0.01).
Conclusion
Compared with OPCABG, HCR did not improve early survival but decreased the length of hospitalization, length of ICU stay, intubation time, and need for red blood transfusion, and increased total in-hospitalcosts.
Keywords: coronary artery bypass grafting, myocardial revascularization, percutaneous coronary intervention, stents
Introduction
Coronary artery bypass grafting (CABG) is considered to be the ‘gold standard’ in patients with multivessel disease and/or left main coronary artery disease 1. However, whether the procedure should be performed with or without the use of cardiopulmonary bypass, referred to as off-pump and on-pump CABG, remains a matter of debate. Compared with on-pump CABG, off-pump CABG (OPCABG) has been suggested to lead to lower incidences of transient atrial fibrillation (AF), less requirements for red blood transfusion, shorter ventilation time 2, shorter length of ICU stay and hospitalization, and fewer perioperative complications, especially in elderly patients with severe comorbidities 3–5.
A meta-analysis 6 of almost 9000 patients from 59 randomized-controlled trials (RCTs) showed no significant difference between OPCABG and on-pump CABG in postoperative mortality and myocardial infarction (MI). Several studies have also reported comparable mid-term and long-term survival between these two patient populations 4,7–12. More recently, the largest (enrolling 4752 patients) RCT, known as the CORONARY trial (CABG Off or On Pump Revascularization Study) 13, also found no significant difference in the incidence of the composite adverse events (death, nonfatal stroke, nonfatal MI, or nonfatal new renal failure requiring dialysis) at 1 year between off-pump and on-pump CABG. However, in contrast to most previous RCTs, the CORONARY trial found no significant increase in the incidence of repeat revascularization for OPCABG at 1 year. The most likely explanation for the differences between the findings of the CORONARY trial and previous trials reporting inferior outcomes for OPCABG is that the CORONARY trial not only enrolled far greater number of patients, but importantly, also recruited surgeons with a far higher level of expertise in off-pump surgery.
Hybrid coronary revascularization (HCR) represents an alternative strategy through a minimally traumatic approach that combines the reliability and survival advantage of the left internal mammary artery to left anterior descending artery (LIMA–LAD) graft with a less invasive percutaneous coronary intervention (PCI) using drug-eluting stents (DESs) to treat non-LAD vessels. On the one hand, the 5-year patency rates of the LIMA–LAD were reported to be between 92 and 99%, whereas the 10-year patency rates approached 95–98% 14–16; on the other hand, a head-to-head comparison of a sirolimus-eluting stent with bare stent from RCTs showed freedom from target lesion revascularization using DES at 1, 3, and 5 years, with patency rates of 99, 93.8, and 89.7%, respectively 17. Essentially, stents are substituted for saphenous vein grafts for non-LAD lesions, allowing the LIMA–LAD bypass to be performed through a limited and less traumatic approach. Therefore, HCR potentially offers the ‘best of both worlds’.
Several controlled studies have compared the safety, feasibility, and efficacy of HCR with OPCABG 18–24. We pooled data from these studies and compared the clinical outcomes in patients treated with HCR versus those with OPCABG.
Methods
Study eligibility and search strategy
A systematic search of the PubMed, Embase, and CENTRAL databases was performed. The following keywords were used in various combinations: ‘coronary artery disease’, ‘angioplasty, balloon, coronary’, ‘multivessel coronary artery disease’, ‘minimally invasive coronary artery bypass’, ‘off-pump’, ‘coronary artery bypass grafting (CABG)’, ‘percutaneous coronary intervention (PCI)’, ‘hybrid coronary revascularization (HCR)’, and ‘clinical trial’, ‘randomized’. The search was limited to English-language articles published since 1996 (hybrid revascularization strategy was first introduced in 1996). We hand-searched references of retrieved articles and used PubMed’s related articles feature to identify studies not captured by our primary search strategy.
Inclusion criteria were (a) RCT, observational cohort studies, and prespecified subgroup analyses comparing HCR with OPCABG, (b) availability of complete clinical data, and (c) at least 10 study participants. Exclusion criteria were (a) duplicate reports failing to report additional or extended clinical outcomes and (b) ongoing studies or irretrievable data.
Data extraction and validity assessment
Two investigators (F.-B. Hu and L.-Q. Cui) independently performed the literature searches to identify the relevant studies. Information on study and patient characteristics and the prespecified clinical outcomes was systematically extracted. In the case of incomplete or unclear data, authors were contacted where possible.
The primary endpoint was in-hospital mortality and major adverse cardiac and cerebrovascular events (MACCE, defined as the occurrence of accidents: all-cause death, stroke, nonfatal MI, and repeat revascularization). The secondary endpoints included length of hospitalization, length of ICU stay, intubation time, need for red blood transfusion, the incidence of transient AF, and total in-hospital costs.
Statistical analysis
We carried out the analysis using Stata, version 11 (Stata Corp LP, College Station, Texas, USA). Relative risk (RR) with a 95% confidence interval (CI) was calculated for each study and pooled in random-effects models. Forest plots were then created for graphical presentations of clinical outcomes. Heterogeneity between trials, defined as variation among the results of individual trials beyond that expected from chance, was assessed by the I2 statistic applying the following interpretation for I2: less than 50%=low heterogeneity; 50–75%=moderate heterogeneity; and greater than 75%=high heterogeneity. In addition, publication bias was assessed using a funnel plot, Begg’s adjusted rank correlation test, and Egger’s regression asymmetry test. Two-sided P-values less than 0.05 were considered statistically significant.
Results
Baseline characteristics and clinical outcomes
Seven studies fulfilled our inclusion criteria and were included in this study (Fig. 1). A total of 5453 patients were included in this analysis; 422 patients received either staged HCR (62.8%) or simultaneous HCR (37.2%) and 5031 received OPCABG. Study characteristics are presented in Table 1. Early (in-hospital or 30-day) clinical outcomes are presented in Table 2.
Fig. 1.
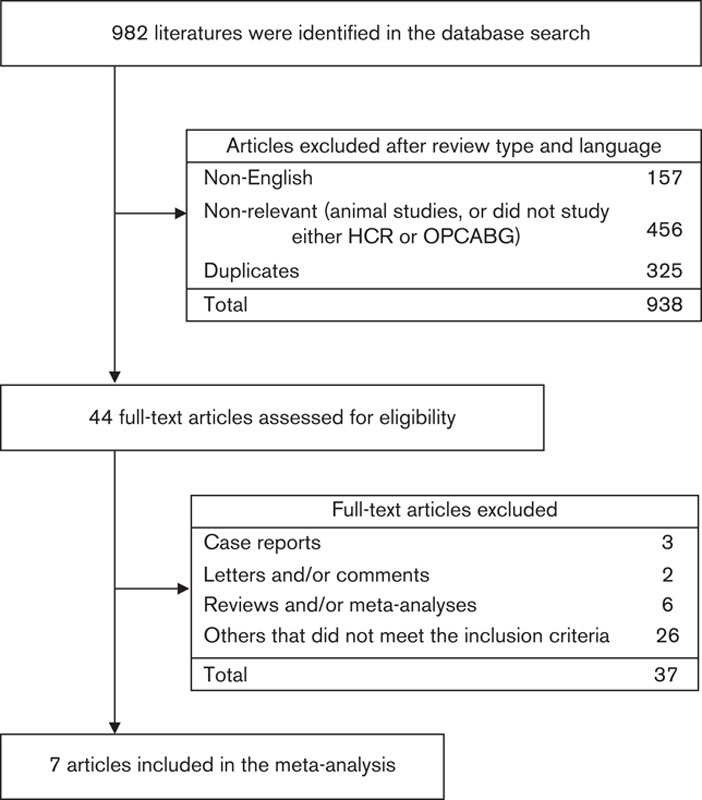
Flow chart of the study selection process. HCR, hybrid coronary revascularization; OPCABG, off-pump coronary artery bypass grafting.
Table 1.
Main characteristics of the selected studies
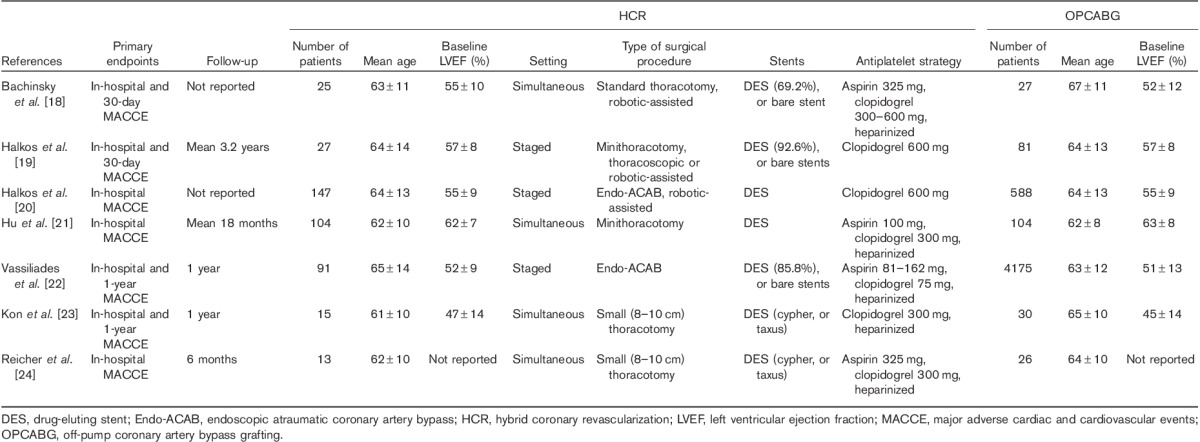
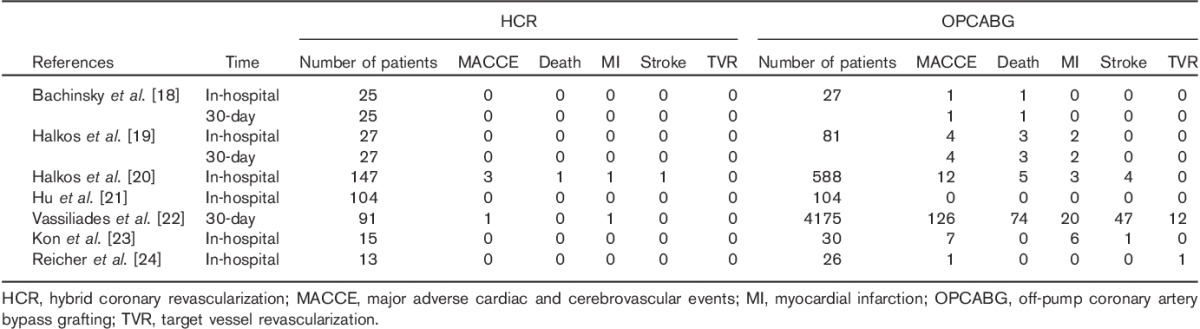
Table 2.
Early (in-hospital or 30-day) clinical outcomes of the selected studies
Primary endpoint
Figure 2 shows the comparison of in-hospital MACCE and mortality between the HCR group and the OPCABG group. Available data were reported in seven studies 18–24. No significant changes were observed in the cumulative analysis between the HCR group and the OPCABG group either in in-hospital mortality (RR 0.57, 95% CI 0.13–2.59, P=0.47, P for heterogeneity=0.90, I2=0%) or in the MACCE rate (RR 0.63, 95% CI 0.24–1.64, P=0.34, P for heterogeneity=0.77, I2=0%).
Fig. 2.
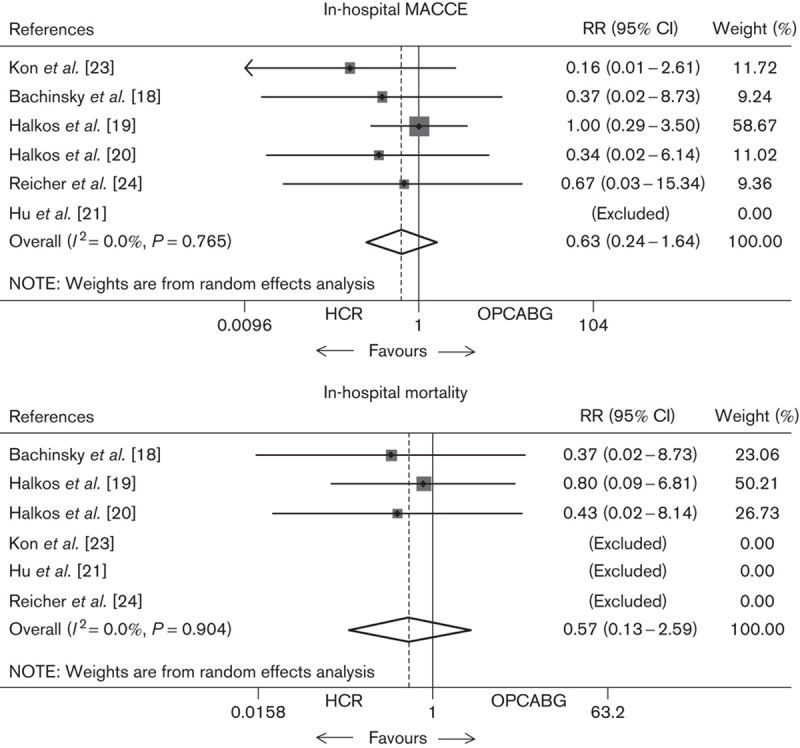
Meta-analysis showing the relative risk (RR) of overall in-hospital MACCE and mortality. Random-effects models were used for meta-analysis. CI, confidence interval; HCR, hybrid coronary revascularization; MACCE, major adverse cardiac and cerebrovascular event; OPCABG, off-pump coronary artery bypass grafting.
Subgroup analysis
Thirty-day mortality and MACCE data were available in three studies. Similarly, as shown in Fig. 3, meta-analysis also found that HCR was not associated with a significantly reduced RR of 30-day mortality (RR 0.36, 95% CI 0.07–1.95, P=0.24) or MACCE rate (RR 0.36, 95% CI 0.09–1.51, P=0.16) compared with OPCABG. We also observed no significant RR difference in early (in-hospital or 30-day) MACCE in the subgroup of simultaneous and staged HCR (Fig. 3; RR 0.57, 95% CI 0.24–1.34, P=0.20).
Fig. 3.
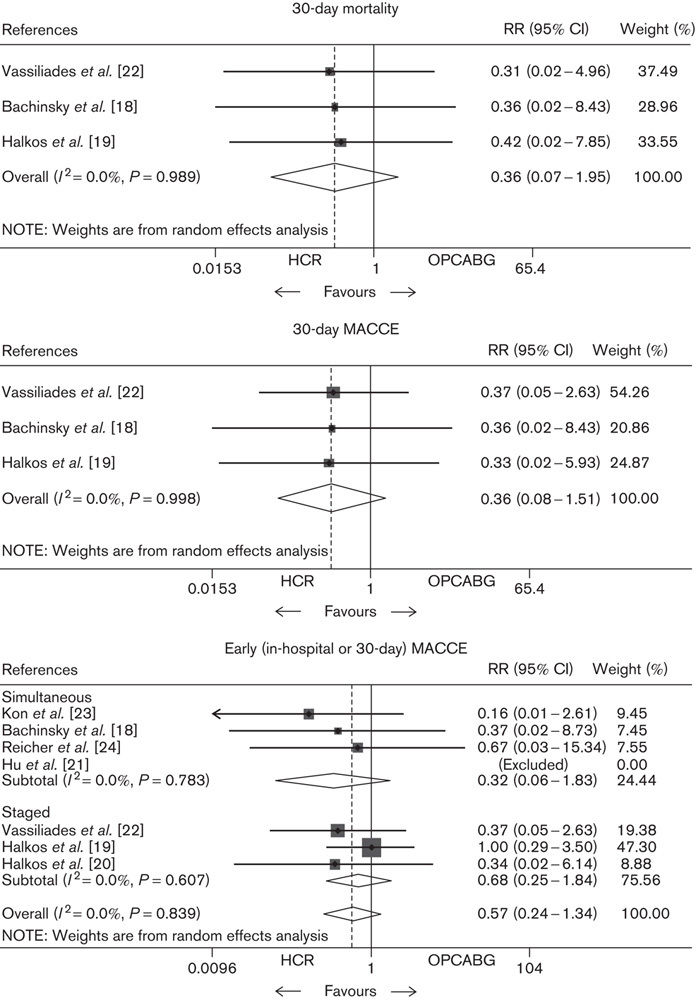
Meta-analysis showing the RR of 30-day mortality, MACCE, and early (in-hospital or 30-day) MACCE in the subgroup of simultaneous and staged HCR. Random-effects models were used for meta-analysis. CI, confidence interval; HCR, hybrid coronary revascularization; MACCE, major adverse cardiac and cerebrovascular event; OPCABG, off-pump coronary artery bypass grafting; RR, relative risk.
Secondary endpoints
As shown in Fig. 4, a significant difference was observed between the two groups in the length of hospitalization (RR 0.55, 95% CI 0.13–0.97, P=0.01), length of ICU stay (RR 0.45, 95% CI 0.10–0.80, P<0.05), intubation time (RR 0.48, 95% CI 0.13–0.84, P<0.01), need for red blood transfusion (RR 0.67, 95% CI 0.56–0.82, P<0.001), and total in-hospital costs (RR 0.90, 95% CI 0.39–1.42, P<0.01). However, no significant difference was observed in the incidence of transient AF (RR 1.03, 95% CI 0.76–1.41, P=0.84).
Fig. 4.
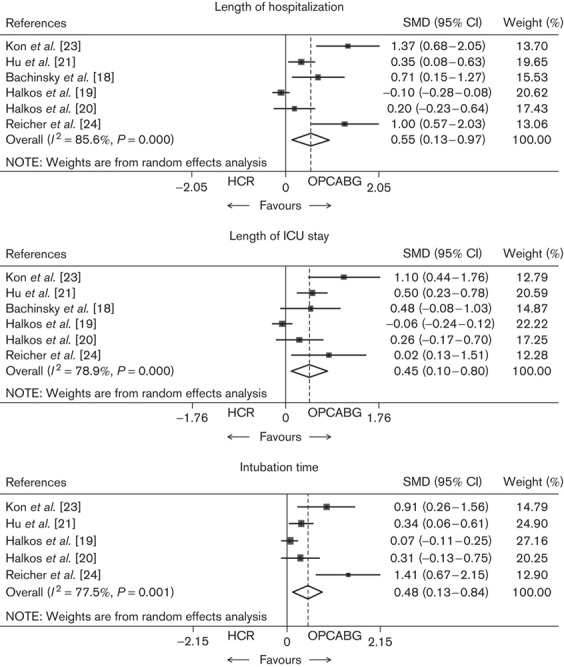
Meta-analysis showing the RR of length of hospitalization, length of ICU stay, intubation time, need for red blood transfusion, the incidence of transient atrial fibrillation (AF), and total in-hospital costs. Random-effects models were used for meta-analysis. CI, confidence interval; HCR, hybrid coronary revascularization; OPCABG, off-pump coronary artery bypass grafting; RR, relative risk; SMD, standardized mean difference.
Fig. 4.
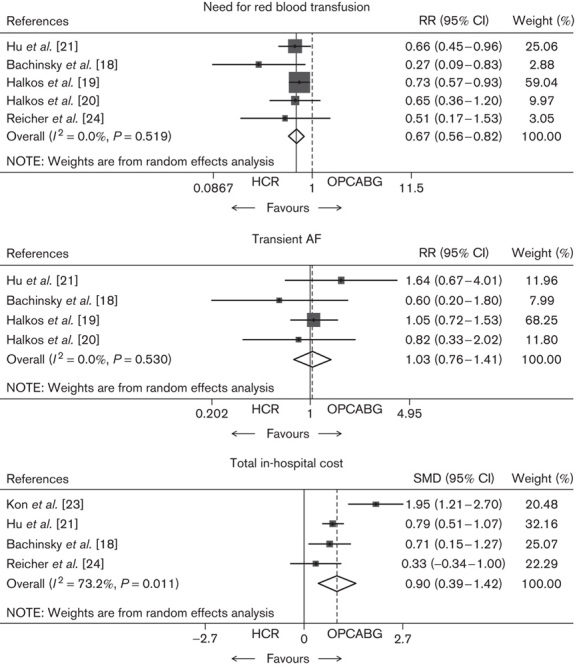
(Continued)
Heterogeneity
In terms of in-hospital MACCE or mortality, there was no evidence of heterogeneity in the treatment effect between the studies.
Publication bias assessment
In the funnel plot of data on RR of in-hospital MACCE, both Begg’s test and Egger’s test suggest the absence of bias (Fig. 5).
Fig. 5.
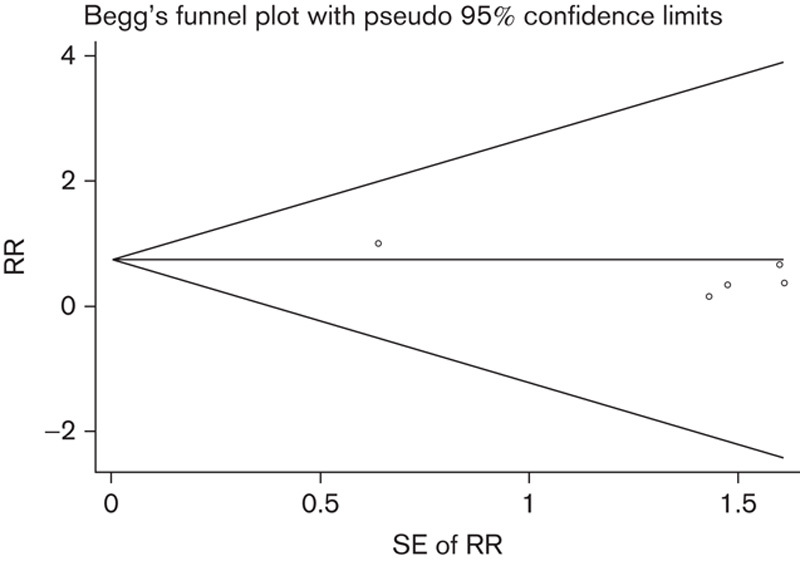
Funnel plot. RR, relative risk.
Discussion
The aim of a hybrid technique is to reduce the invasiveness, mortality, and morbidity of each single procedure and combine the optimal results and the best practice of both procedures. LIMA–LAD bypass grafting through a minimally traumatic approach offers the best evidence-based management in terms of graft patency and survival benefits 25,26. In contrast, saphenous vein graft (SVG) conduits are found to be unreliable in terms of short-term patency and long-term durability 27. Several studies have reported a SVG failure rate between 1.6 and 30% at 1 year, with an average of 20% 28–31, and approaching 30% within 12–18 months 28. Moreover, 40–50% of the SVG graft would have failed at follow-up of 10–15 years 14. The restenosis rate with DES within 12–18 months seems to be superior to SVG 32–36. Therefore, the hybrid technique might be a novel alternative and more practical solution to avoid the well-known limitations of SVG conduits than all-arterial grafting. Currently, the American College of Cardiology Foundation and the American Heart Association have recommended HCR for selected patients on level of evidence B for limitation to traditional CABG, lack of available graft conduits, or unfavorable LAD artery disease for PCI 37.
However, the best protocol of a hybrid approach remains a matter of debate. Currently, there are three HCR strategies available: (a) performing PCI first, followed by staged LIMA to LAD bypass grafting, or (b) vice versa; (c) combining LIMA–LAD bypass grafting with PCI in the same setting in a hybrid operative unit. More recently, a simultaneous HCR procedure has been applied much more frequently than a staged procedure. A simultaneous HCR procedure not only has the advantage of avoiding the potential problems related to two separate procedures and hands-off, but is also convenient for doctors to resolve any complications arising from either procedure in one setting. Importantly, LIMA–LAD bypass graft patency can be confirmed immediately. Furthermore, the same setting strategy improves the efficiency and cost-effectiveness of HCR and ultimately provides a more attractive alternative for the patient. Patients are more likely to accept HCR if complete revascularization can be finished in one procedure.
The feasibility and efficacy of the simultaneous hybrid procedure has been reported with high 6-month angiographic vessel patency and minimal adverse cardiac events, comparable to OPCABG patients 18,21,23,24,38. Especially, the rates of acute/subacute stent thrombosis in the simultaneous HCR approach seem similar to those with complex PCI procedures 39. This is the first meta-analysis of controlled trials comparing HCR with OPCABG thus far; our data showed that there was no significant between-group difference either in early (in-hospital or 30-day) mortality or in the MACCE rate. However, the total in-hospital costs were significantly higher in the HCR group than in the OPCAB group, mainly because of the use of radiographic instruments and stent implantation. Similarly, we also found no significant RR difference in early (in-hospital or 30-day) MACCE in the subgroup of simultaneous and staged HCR.
More rapid recovery from HCR procedure indicates that factors other than pain may play important roles in the recovery process. Less need for red blood transfusion, shorter intubation time and ICU stay, as well as reduced systemic inflammation, may contribute significantly toward the improved morbidity after HCR. Interestingly, this is similar to the comparison between minimally invasive off-pump and conventional on-pump CABG in terms of less trauma–rapid recovery pattern. In addition, the degree of cardiac manipulation varies markedly between the HCR and the OPCABG procedure. Actually, the heart is left in its natural position during the HCR procedure, whereas it requires frequent rotation during the OPCABG procedure, which may compromise hemodynamic status. Furthermore, coronary occlusion for the HCR procedure is limited to that required for the placement of a single LIMA–LAD graft and less than 30 s intervals for each stent implantation. In contrast, OPCABG requires 8–12 min intervals of coronary occlusion during each of three to four distal anastomoses, resulting in a total ischemic time approaching 25–40 min. Better myocardial protection, reflected by a reduction in regional myoglobin and systemic troponin I release, might be another important mechanism for quicker recovery from the HCR procedure 40.
Nevertheless, in the current era of evidence-based medicine, the best strategy for countering doubt and validating the safety, feasibility, and efficacy of a therapeutic approach such as HCR is convincing data from RCTs. Thus, large, multicenter RCTs are needed to compare HCR with OPCABG to clarify patient populations that would benefit most from HCR. Moreover, different HCR strategies (staged vs. simultaneous) should be compared to identify which strategy would serve which patients best. Finally, both the advantages and the disadvantages of a same-setting HCR operative unit need to be explored further.
Study limitations
At first, all of the studies included were observational in nature and thus might have been affected by confounding with indication and/or selection bias. Second, the study enrolled a relatively small number of patients undergoing HCR procedures and some controlled groups were propensity adjusted with a retrospective design. Third, the mean length of follow-up was generally short, in particular, because of the lack of mid-term and long-term systematic and routine angiographic follow-up of graft and stent patency in the majority of studies included in the present study, which made it difficult to evaluate mid-term and long-term clinical outcomes. Finally, different kinds of DES were used in the studies included, and in two studies, although the majority of patients received DES, bare stents were also implanted.
Conclusion
HCR did not improve early survival compared with OPCABG, but decreased the length of hospitalization, length of ICU stay, intubation time, and need for red blood transfusion, and increased total in-hospital costs.
Acknowledgements
Conflicts of interest
There are no conflicts of interest.
References
- 1.Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, et al. SYNTAX Investigators. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 2009; 360:961–972. [DOI] [PubMed] [Google Scholar]
- 2.Hu S, Zheng Z, Yuan X, Wang W, Song Y, Sun H, et al. Increasing long-term major vascular events and resource consumption in patients receiving off-pump coronary artery surgery: a single-center prospective observational study. Circulation 2010; 121:1800–1808. [DOI] [PubMed] [Google Scholar]
- 3.Palmer G, Herbert MA, Prince SL, Williams JL, Magee MJ, Brown P, et al. Coronary artery revascularization (CARE) registry: an observational study of on-pump and off-pump coronary artery revascularization. Ann Thorac Surg 2007; 83:986–991. [DOI] [PubMed] [Google Scholar]
- 4.Hannan EL, Wu C, Smith CR, Higgins RS, Carlson RE, Culliford AT, et al. Off-pump versus on-pump coronary artery bypass graft surgery: differences in short-term outcomes and in long-term mortality and need for subsequent revascularization. Circulation 2007; 116:1145–1152. [DOI] [PubMed] [Google Scholar]
- 5.Stamou SC, Jablonski KA, Hill PC, Bafi AS, Boyce SW, Corso PJ. Coronary revascularization without cardiopulmonary bypass versus the conventional approach in high-risk patients. Ann Thorac Surg 2005; 79:552–557. [DOI] [PubMed] [Google Scholar]
- 6.Afilalo J, Rasti M, Ohayon SM, Shimony A, Eisenberg MJ. Off-pump vs. on-pump coronary artery bypass surgery: an updated meta-analysis and metaregression of randomized trials. Eur Heart J 2012; 33:1257–1267. [DOI] [PubMed] [Google Scholar]
- 7.Khan NE, De Souza A, Mister R, Flather M, Clague J, Davies S, et al. A randomized comparison of off-pump and on-pump multivessel coronary-artery bypass surgery. N Engl J Med 2004; 350:21–28. [DOI] [PubMed] [Google Scholar]
- 8.Williams ML, Muhlbaier LH, Schroder JN, Hata JA, Peterson ED, Smith PK, et al. Risk-adjusted short- and long-term outcomes for on pump versus off-pump coronary artery bypass surgery. Circulation 2005; 112:I366–I370. [DOI] [PubMed] [Google Scholar]
- 9.Angelini GD, Culliford L, Smith DK, Hamilton MC, Murphy GJ, Ascione R, et al. Effects of on- and off-pump coronary artery surgery on graft patency, survival, and health-related quality of life: long term follow-up of 2 randomized controlled trials. J Thorac Cardiovasc Surg 2009; 137:295–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karolak W, Hirsch G, Buth K, Legare JF. Medium-term outcomes of coronary artery bypass graft surgery on pump versus off pump: results from a randomized controlled trial. Am Heart J 2007; 153:689–695. [DOI] [PubMed] [Google Scholar]
- 11.Motallebzadeh R, Bland JM, Markus HS, Kaski JC, Jahangiri M. Health-related quality of life outcome after on-pump versus off-pump coronary artery bypass graft surgery: a prospective randomized study. Ann Thorac Surg 2006; 82:615–619. [DOI] [PubMed] [Google Scholar]
- 12.Puskas JD, Kilgo PD, Lattouf OM, Thourani VH, Cooper WA, Vassiliades TA, et al. Off-pump coronary bypass provides reduced mortality and morbidity and equivalent 10-year survival. Ann Thorac Surg 2008; 86:1139–1146. [DOI] [PubMed] [Google Scholar]
- 13.Lamy A, Devereaux PJ, Prabhakaran D, Taggart DP, Hu S, Paolasso E, et al. CORONARY Investigators. Effects of off-pump and on-pump coronary artery bypass grafting at 1 year. N Engl J Med 2013; 368:1179–1188. [DOI] [PubMed] [Google Scholar]
- 14.Tatoulis J, Buxton BF, Fuller JA. Patencies of 2127 arterial to coronary conduits over 15 years. Ann Thorac Surg 2004; 77:93–101. [DOI] [PubMed] [Google Scholar]
- 15.Kim KB, Cho KR, Jeong DS. Midterm angiographic follow-up after off-pump coronary artery bypass: serial comparison using early, 1-year, and 5-year postoperative angiograms. J Thorac Cardiovasc Surg 2008; 135:300–307. [DOI] [PubMed] [Google Scholar]
- 16.Hayward PA, Buxton BF. Contemporary coronary graft patency: 5-year observational data from a randomized trial of conduits. Ann Thorac Surg 2007; 84:795–799. [DOI] [PubMed] [Google Scholar]
- 17.Narasimhan S, Srinivas VS, DeRose JJ., Jr Hybrid coronary revascularization: a review. Cardiol Rev 2011; 19:101–107. [DOI] [PubMed] [Google Scholar]
- 18.Bachinsky WB, Abdelsalam M, Boga G, Kiljanek L, Mumtaz M, McCarty C. Comparative study of same sitting hybrid coronary artery revascularization versus off-pump coronary artery bypass in multivessel coronary artery disease. J Interv Cardiol 2012; 25:460–468. [DOI] [PubMed] [Google Scholar]
- 19.Halkos ME, Rab ST, Vassiliades TA, Morris DC, Douglas JS, Kilgo PD, et al. Hybrid coronary revascularization versus off-pump coronary artery bypass for the treatment of left main coronary stenosis. Ann Thorac Surg 2011; 92:2155–2160. [DOI] [PubMed] [Google Scholar]
- 20.Halkos ME, Vassiliades TA, Douglas JS, Morris DC, Rab ST, Liberman HA, et al. Hybrid coronary revascularization versus off-pump coronary artery bypass grafting for the treatment of multivessel coronary artery disease. Ann Thorac Surg 2011; 92:1695–1701. [DOI] [PubMed] [Google Scholar]
- 21.Hu S, Li Q, Gao P, Xiong H, Zheng Z, Li L, et al. Simultaneous hybrid revascularization versus off-pump coronary artery bypass for multivessel coronary artery disease. Ann Thorac Surg 2011; 91:432–438. [DOI] [PubMed] [Google Scholar]
- 22.Vassiliades TA, Kilgo PD, Douglas JS, Babaliaros VC, Block PC, Samady H, et al. Clinical outcomes after hybrid coronary revascularization versus off pump coronary artery bypass. Innovations 2009; 4:299–306. [DOI] [PubMed] [Google Scholar]
- 23.Kon ZN, Brown EN, Tran R, Joshi A, Reicher B, Grant MC, et al. Simultaneous hybrid coronary revascularization reduces postoperative morbidity compared with results from conventional off-pump coronary artery bypass. J Thorac Cardiovasc Surg 2008; 135:367–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reicher B, Poston RS, Mehra MR, Joshi A, Odonkor P, Kon Z, et al. Simultaneous ‘hybrid’ percutaneous coronary intervention and minimally invasive surgical bypass grafting: feasibility, safety, and clinical outcomes. Am Heart J 2008; 155:661–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Loop FD, Lytle BW, Cosgrowe DM, Stewart RW, Goormastic M, Williams GW, et al. Influence of the internal mammary artery graft on 10-year survival and other cardiac events. N Engl J Med 1986; 314:1–6. [DOI] [PubMed] [Google Scholar]
- 26.Diegler A, Thiele H, Falk V, Hambrect R, Spyrantis N, Sick P, et al. Comparison of stenting with minimally invasive bypass surgery for stenosis of the left anterior descending coronary artery. N Engl J Med 2002; 347:561–566. [DOI] [PubMed] [Google Scholar]
- 27.Guyton RA. Coronary artery bypass is superior to drug-eluting stents in multivessel coronary artery disease. Ann Thorac Surg 2006; 81:1949–1957. [DOI] [PubMed] [Google Scholar]
- 28.Alexander JH, Hafley G, Harrington RA, Peterson ED, Ferguson TB, Jr, Lorenz TJ, et al. PREVENT IV Investigators. Efficacy and safety of edifoligide, an E2F transcription factor decoy, for prevention of vein graft failure following coronary artery bypass graft surgery: PREVENT IV: a randomized controlled trial. JAMA 2005; 294:2446–2454. [DOI] [PubMed] [Google Scholar]
- 29.Puskas JD, Williams WH, Mahoney EM, Huber PR, Block PC, Duke PG, et al. Off-pump vs conventional coronary artery bypass grafting: early and 1-year graft patency, cost, and quality-of-life outcomes: a randomized trial. JAMA 2004; 291:1841–1849. [DOI] [PubMed] [Google Scholar]
- 30.Balacumaraswami L, Taggart DP. Intraoperative imaging techniques to assess coronary artery bypass graft patency. Ann Thorac Surg 2007; 83:2251–2257. [DOI] [PubMed] [Google Scholar]
- 31.Magee MJ, Alexander JH, Hafley G, Ferguson TB, Jr, Gibson CM, Harrington RA, et al. PREVENT IV Investigators. Coronary artery bypass graft failure after on-pump and off-pump coronary artery bypass: findings from PREVENT IV. Ann Thorac Surg 2008; 85:494–500. [DOI] [PubMed] [Google Scholar]
- 32.Park SJ, Shim WH, Ho DS, Raizner AE, Park SW, Hong MK, et al. A paclitaxel-eluting stent for the prevention of coronary restenosis. N Engl J Med 2003; 348:1537–1545. [DOI] [PubMed] [Google Scholar]
- 33.Moses JW, Leon MB, Popma JJ, Fitzgerald PJ, Holmes DR, O’Shaughnessy C, et al. SIRIUS Investigators. Sirolimus-eluting stents versus standard stents in patients with stenosis in a native coronary artery. N Engl J Med 2003; 349:1315–1323. [DOI] [PubMed] [Google Scholar]
- 34.Grube E, Silber S, Hauptmann KE, Mueller R, Buellesfeld L, Gerckens U, et al. TAXUS I: six- and twelve-month results from a randomized, double-blind trial on a slow-release paclitaxel-eluting stent for de novo coronary lesions. Circulation 2003; 107:38–42. [DOI] [PubMed] [Google Scholar]
- 35.Murphy GJ, Bryan AJ, Angelini GD. Hybrid coronary revascularization in the era of drug-eluting stents. Ann Thorac Surg 2004; 78:1861–1867. [DOI] [PubMed] [Google Scholar]
- 36.Schampaert E, Moses JW, Schofer J, Schlüter M, Gershlick AH, Cohen EA, et al. SIRIUS, E- and C-SIRIUS Investigators. Sirolimus-eluting stents at two years: a pooled analysis of SIRIUS, E-SIRIUS, and C-SIRIUS with emphasis on late revascularizations and stent thromboses. Am J Cardiol 2006; 98:36–41. [DOI] [PubMed] [Google Scholar]
- 37.Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, Byrne JG, et al. 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the American Association for Thoracic Surgery, Society of Cardiovascular Anesthesiologists, and Society of Thoracic Surgeons. J Am Coll Cardiol 2011; 58:e123–e210. [DOI] [PubMed] [Google Scholar]
- 38.Vassiliades TA, Jr, Douglas JS, Morris DC, Block PC, Ghazzal Z, Rab ST, et al. Integrated coronary revascularization with drug-eluting stents: immediate and seven-month outcome. J Thorac Cardiovasc Surg 2006; 131:956–962. [DOI] [PubMed] [Google Scholar]
- 39.King SB, 3rd, Smith SC, Jr, Hirshfeld JW, Jr, Jacobs AK, Morrison DA, Williams DO, et al. 2007 focused update of the ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2008; 117:261–295. [DOI] [PubMed] [Google Scholar]
- 40.Harskamp RE, Abdelsalam M, Lopes RD, Boga G, Hirji S, Krishnan M, et al. Cardiac troponin release following hybrid coronary revascularization versus off-pump coronary artery bypass surgery. Interact Cardiovasc Thorac Surg 2014; 19:1008–1012. [DOI] [PubMed] [Google Scholar]


